Pregnancy letters from doctors
Free Pregnancy Verification Form - Word
Home » Verification » Pregnancy
Updated August 03, 2022
A pregnancy verification form is a letter that is used to show proof of a positive pregnancy test confirming that a woman is indeed pregnant. The form details the date when the individual visited the clinic/hospital, the estimated date of delivery, and any additional notes or comments related to the test. This information is important as it helps to keep a record of the child’s development and can assist doctors in treating the individual for future visits.
How to
Verify a Pregnancy (3 steps)Use the following instructions to inform an employer, educational entity, or partner of a positive pregnancy. The form is also useful during instances of traveling and is recommended to have on hand. Moreover, it’s often used for filing for maternity leave and claiming health insurance. If pregnancy is verified, a partner may be able to dispute claims until the baby is born.
If someone has missed their period, this is usually the first (1st) sign that something could be changing in a woman’s body. In this case, it’s best to go to the local pharmacy and procure a pregnancy test.
Most Popular Testing Kits
- First Response
- ClearBlue
Both testing kits are over 99% accurate and may be used up to five (5) days before a woman’s expected period. Although, it’s more accurate on the day of or after the expected period. Depending on where you purchase the test, it may cost anywhere from $6 to $20.
Most Popular In-Home Tests
- Place Urine in a Cup – Let it sit overnight, and if a thin white film covers the top of the surface, then there is a chance the woman is pregnant. If the urine stays the same, she may not be pregnant.

- Sugar Test – Urinate in a cup and add 2-3 teaspoons of white granulated sugar (common sugar used for coffee). Wait 5-10 minutes, and if the sugar clumps into small balls, there is a chance she is pregnant. If the sugar dissolves evenly, the woman is may not be pregnant.
It should be noted that the in-home tests are anecdotal and should always be followed with a more accurate testing approach, such as a store-bought testing kit. The longer a woman waits after her missed period, the more likely for an accurate result, as hCG hormones will elevate.
Step 2 – Schedule an AppointmentAfter a positive result, it’s best to schedule an appointment with your primary care physician or local OB/GYN. At the office, they will conduct their own internal tests which may be a combination of blood and urine.
Step 3 – Get VerifiedDuring the appointment, if you test positive, the medical office will issue a pregnancy verification form (Download) that can be used to prove to a partner, employers, schools, or other third (3rd) parties that the pregnancy is positive.
Video
Step 1 – Start by downloading the form in the format you prefer (Adobe PDF, Microsoft Word (.docx), Open Document Text (.odt)).
Step 2 – At the top of the form, use the empty spaces to enter the date of the pregnancy test (day, month, year) followed by the patient’s name.
Step 3 – Next, specify the estimated date of delivery (day, month, year).
Step 4 – Additional notes or comments may be entered in this section of the verification form.
Step 5 – In the remaining empty spaces, provide your signature, title, printed name, and phone number.
By using the website, you agree to our use of cookies to analyze website traffic and improve your experience on our website.
pregnancy verification form: Fill out & sign online
pregnancy verification form: Fill out & sign online | DocHub- Home
- Proof of pregnancy letter from doctor pdf
4.5 out of 5
35 votes
DocHub Reviews
44 reviews
DocHub Reviews
23 ratings
15,005
10,000,000+
303
100,000+ users
Here's how it works
01. Edit your pregnancy verification form pdf online
Type text, add images, blackout confidential details, add comments, highlights and more.
02. Sign it in a few clicks
Draw your signature, type it, upload its image, or use your mobile device as a signature pad.
03. Share your form with others
Send pregnancy verification via email, link, or fax. You can also download it, export it or print it out.
How to edit proof of pregnancy letter from doctor pdf online
9.5Ease of Setup
DocHub User Ratings on G2
9.0Ease of Use
DocHub User Ratings on G2
With DocHub, making changes to your paperwork requires only some simple clicks. Make these quick steps to edit the PDF proof of pregnancy letter from doctor pdf online for free:
- Register and log in to your account. Sign in to the editor with your credentials or click on Create free account to test the tool’s functionality.
- Add the proof of pregnancy letter from doctor pdf for redacting. Click the New Document button above, then drag and drop the file to the upload area, import it from the cloud, or using a link.
- Modify your template. Make any changes required: insert text and images to your proof of pregnancy letter from doctor pdf, highlight information that matters, erase parts of content and substitute them with new ones, and add icons, checkmarks, and areas for filling out.
- Complete redacting the template. Save the updated document on your device, export it to the cloud, print it right from the editor, or share it with all the people involved.
Our editor is very intuitive and effective. Give it a try now!
be ready to get more
Complete this form in 5 minutes or less
Get form
Got questions?
We have answers to the most popular questions from our customers. If you can't find an answer to your question, please contact us.
Contact us
How do I report a birth to Medicaid in Texas?
Call 800-925-9126.
What is the law on maternity leave UK?
Statutory Maternity Leave Eligible employees can take up to 52 weeks' maternity leave. The first 26 weeks is known as 'Ordinary Maternity Leave', the last 26 weeks as 'Additional Maternity Leave'. The earliest that leave can be taken is 11 weeks before the expected week of childbirth, unless the baby is born early.
The first 26 weeks is known as 'Ordinary Maternity Leave', the last 26 weeks as 'Additional Maternity Leave'. The earliest that leave can be taken is 11 weeks before the expected week of childbirth, unless the baby is born early.
Can a phantom pregnancy cause a positive test?
A "Phantom hCG" causes a positive blood pregnancy test without being pregnant. Patients with a phantom hCG will have a persistently yet not significantly rising positive blood pregnancy test while the urine test is negative.
How do I get my child's Medicaid number in Texas?
Phone. Call toll-free at 800-252-8263, 2-1-1 or 877-541-7905.
What benefits can I claim when pregnant UK?
Benefits available during pregnancy \u2013 background information Statutory Maternity Pay and Maternity Allowance. Employment and Support Allowance. Sure Start Maternity Grant.
Employment and Support Allowance. Sure Start Maternity Grant.
confirmation of pregnancy form pdf
proof of pregnancy form from doctor proof of pregnancy form planned parenthood proof of pregnancy from doctor proof of pregnancy for snap
Related forms
be ready to get more
Complete this form in 5 minutes or less
Get form
People also ask
How do doctors verify pregnancy?
Urine tests Doctors can perform urine pregnancy tests (UPT) in their office and is usually the first step in diagnosing a pregnancy. After the urine testing, the doctor can perform even more pregnancy tests such as a blood test and sonogram.
Are pregnancy verification letters real?
A pregnancy verification form is a letter that is used to show proof of a positive pregnancy test confirming that a woman is indeed pregnant. The form details the date when the individual visited the clinic/hospital, the estimated date of delivery, and any additional notes or comments related to the test.
The form details the date when the individual visited the clinic/hospital, the estimated date of delivery, and any additional notes or comments related to the test.
How Long Does Medicaid cover baby after birth in Texas?
Medicaid provides health coverage to low-income pregnant women during pregnancy and up to two months after the birth of the baby. CHIP Perinatal provides similar coverage for women who can't get Medicaid and don't have health insurance. To get Medicaid for Pregnant Women or CHIP Perinatal, you must be a Texas resident.
How do I contact Medicaid in Texas?
If you don't have a health plan and need help, call the Medicaid Helpline 800-335-8957.
What does confirmation of pregnancy mean?
A confirmation of pregnancy simply proves that a medical provider ran a pregnancy test on the patient, and it was positive. A positive, medical grade pregnancy test is more reliable than having a positive home test.
A positive, medical grade pregnancy test is more reliable than having a positive home test.
ina neman forms da naffito yanzu
Form h4037, Report of Pregnancy
Instructions Updated: 4/2003 Purpose To document pregnancy, the sixth to ninth months, delivery date, multiple births, and other disabling conditions ...
Learn more
Forms & Letters | People & Culture - UC Berkeley HR
Hiring Forms (expand) · Employment Eligibility Verification Form (PDF file)(link is external) (PDF) · Online Instructions for Completing the I-9(link is external) ...
Learn more
Abortion in India - Wikipedia
Abortion in India has been legal under various circumstances for the last 50 years with the introduction of Medical Termination of Pregnancy (MTP) Act in 1971. ... paid leave of up to one month on submission of relevant medical proofs.
... paid leave of up to one month on submission of relevant medical proofs.
Learn more
Try more PDF tools
© 2022 by DocHub LLC
Letter from mother about perinatal care
June 18, 2018
We received a very important letter about perinatal palliative care at the hospice, with the permission of the author, we share it with you:
“Good afternoon! I saw your article about opening a perinatal palliative care program at the Children's Hospice and decided to write to you. You write that the program has been running for 2 months, but no one has asked for help. Perhaps those in need of this type of assistance simply do not know about your program, no one talks about it in antenatal clinics, for them the main thing is that a woman gives birth to a healthy child, and a child with a developmental defect, all the more incompatible with life, is a problem for 9months and corrupted statistics. But there are women who need such help, you can be sure. I once in 2014 - 2015. I was one of them and I know firsthand what you have to go through in order to defend your position and the right of a child with a lethal prognosis to be born at all costs.
But there are women who need such help, you can be sure. I once in 2014 - 2015. I was one of them and I know firsthand what you have to go through in order to defend your position and the right of a child with a lethal prognosis to be born at all costs.
I'll tell my story, maybe it will be useful to someone. She became pregnant in 2014 after the first missed pregnancy. The pregnancy was planned, I passed the tests in advance, everything was normal. The first screening is normal, at the second at 23 weeks my husband and I go for a 3D ultrasound to burn it on a disc. And we are told that the child has a brain defect incompatible with life, and we need to terminate the pregnancy as soon as possible. And they wonder how they did not see such a gross malformation at the first screening? They said: "You are still young, you will become pregnant in 6 months and give birth to a healthy one." We went to a good specialist to confirm the diagnosis, she took pity on us and also recommended terminating the pregnancy as soon as possible.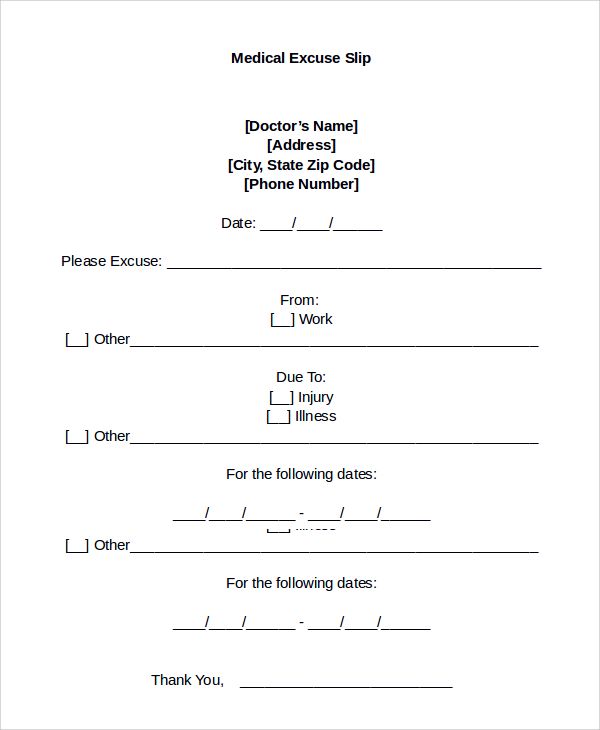
What was going on in my head is hard to describe, because my long-awaited child was already moving, we had already made plans for the future life, and then everything collapses in an instant. There were weekends ahead, after which it was necessary to go to the LCD for a referral for interruption. I could not sleep, said goodbye to the child, could not imagine how I would kill him. I decided the next day to go to church to talk with the priest, my heart was out of place. The priest's answer was not long in coming - this is murder, you must give birth to him and have time to baptize him. It was a shock. I told the words of the priest to my husband, and he says - so we will give birth. The decision was made, and somehow abruptly everything fell into place, this is our child, and we will decide whether he lives or not, and all responsibility lies with us, not with the doctors.
In a short time the world has turned upside down, thinking has changed, we have revised many things in our lives. The doctor in the housing complex was shocked by my decision to carry and give birth to a terminally ill child, she sent me to the head. She only asked, what would I do if I found out about the defect at the first screening - would I also leave the child? I said I don't know, maybe not, but it doesn't matter now. The only doctor who supported me was a geneticist who said that if this happened to her daughter, she would do the same.
The doctor in the housing complex was shocked by my decision to carry and give birth to a terminally ill child, she sent me to the head. She only asked, what would I do if I found out about the defect at the first screening - would I also leave the child? I said I don't know, maybe not, but it doesn't matter now. The only doctor who supported me was a geneticist who said that if this happened to her daughter, she would do the same.
The pregnancy was uneventful, although I was scared that the baby would hardly live to see the birth, and if it did, it would die during the birth. We gave ourselves the installation that each of us has our own time period on this earth, which means that our boy has been given such a short period, and we must go this path together, rejoicing every day, because this could never have happened at all. We talked with the baby, he answered us with jerks, although the doctors said that he would practically not move ... For us, this time was a whole life, the life of our baby.
The attitude of the doctors at the maternity hospital was tough from the first minutes: “Why couldn't you terminate a pregnancy before? You know how it all ends." I didn’t see the point in looking for a paid maternity hospital, who would take us with our diagnosis, and how much they would charge for it. Nevertheless, the birth went well, the son was born alive, obstetricians and doctors constantly looked at each other in bewilderment that he was still alive. I christened him myself by prior arrangement with the priest. The resuscitator came and took him away with a displeased face, saying that he was breathing on his own.
The next day was my first visit to the intensive care unit. They let you in for 2 hours a day. The head of resuscitation approached me and spoke to me in a very harsh manner, saying: “What couldn’t you endure, he is suffering because of you and who knows how long he will die painfully.” Coming out of there, I even thought for a while that there was no God, and I actually did everything wrong and was to blame for everything.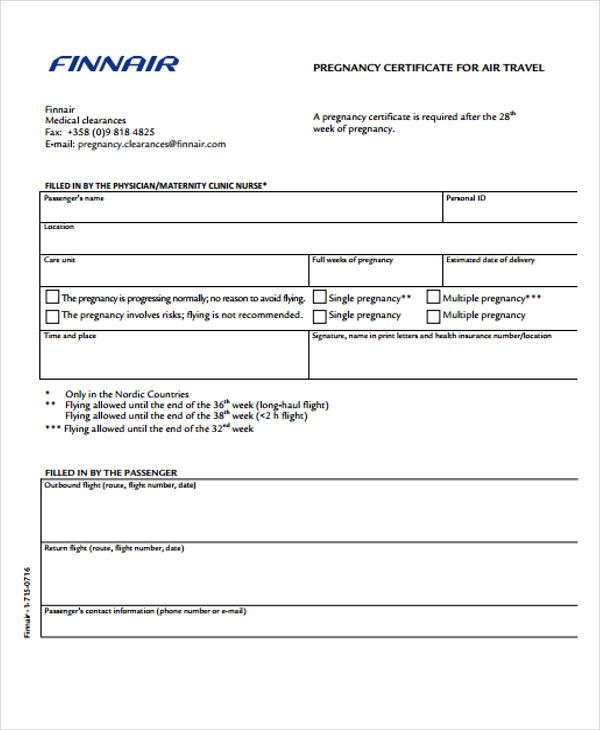 But then she took matters into her own hands. Each of my trips to the intensive care unit was accompanied by unpleasant statements addressed to me, but I endured and did not answer them with rudeness, I don’t know where my strength came from. The next day, the priest came to the intensive care unit to baptize another child, and I was offered to baptize my son in accordance with all the rules. Batiushka said that he was well done for waiting for the baptism. The next day my son went to the world of Angels.
But then she took matters into her own hands. Each of my trips to the intensive care unit was accompanied by unpleasant statements addressed to me, but I endured and did not answer them with rudeness, I don’t know where my strength came from. The next day, the priest came to the intensive care unit to baptize another child, and I was offered to baptize my son in accordance with all the rules. Batiushka said that he was well done for waiting for the baptism. The next day my son went to the world of Angels.
It was very difficult to go through all this, meeting only obstacles and obstacles along the way, although compassion and support were needed. But we did not regret for a second that we chose this path. We did everything that depended on us, and now our soul is calm. It is a pity that there was no palliative care program before, and that our system is so rigid in deciding who is destined to be born and who does not belong here. I hope that there will be those women who will need your help and give them strength and support in a difficult life test.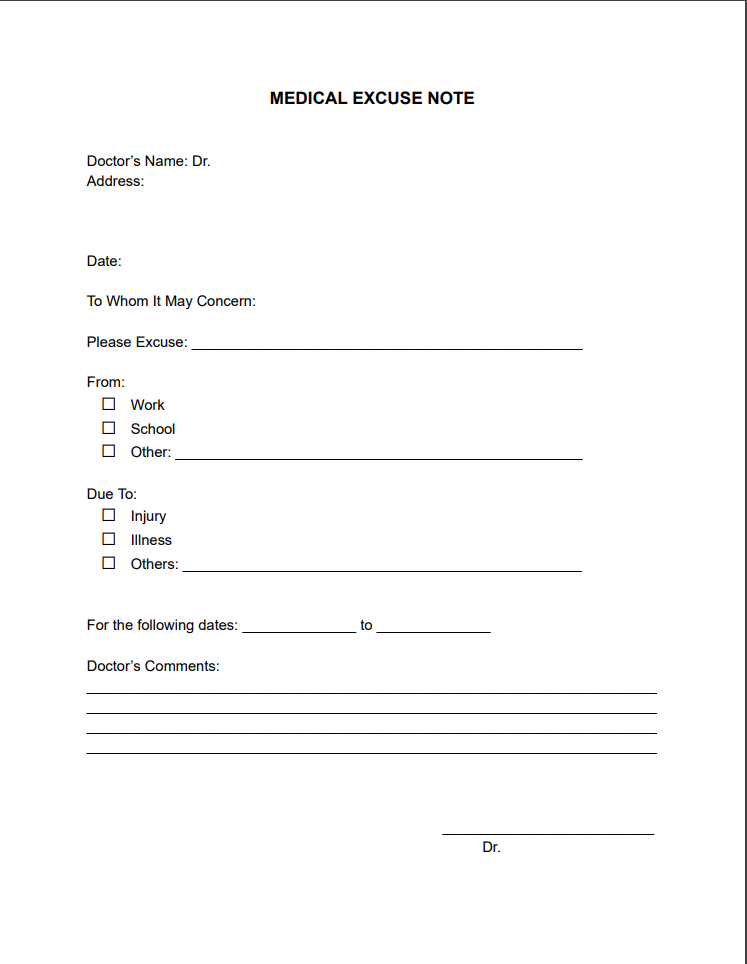 Good luck in your very important and good undertaking!!!”.
Good luck in your very important and good undertaking!!!”.
Information letter of the Russian Society of Obstetricians and Gynecologists
For a doctor, planning and managing pregnancy is a special responsibility. The most important task is to help give birth to a healthy child and maintain the health of the mother.
Taking complexes containing iron, folic acid and trace elements reduces the risk of fetal death by 9%.
Dear colleagues!
This information letter is devoted to the nutritional support of a woman as an important factor in preventing the development of fetal defects and pregnancy complications. The threat of developmental anomalies in our complex age is indeed growing, and ignoring risk management means showing unjustified carelessness. Every woman planning a pregnancy should understand the measure of her own responsibility for her health. At the same time, during pregnancy, this responsibility increases and extends not only to yourself and your unborn child, but also to subsequent generations. The concept of "fragile fruit", which was put forward in 1992 European scientist H. Bern (N. Bern) [1]. The essence of the concept is that the reproductive cells of the unborn child are formed during his stay in the womb, and it is they who determine what the descendants of this unborn baby will be like. The more aggressive factors affect the body of a pregnant woman (hypovitaminosis, smoking, stress, etc.), the higher the risk of various anomalies in subsequent generations. It is obvious that doctors must necessarily instill in each of their patients the idea that her lifestyle during pregnancy can affect the health of not only her children, but also her grandchildren.
The concept of "fragile fruit", which was put forward in 1992 European scientist H. Bern (N. Bern) [1]. The essence of the concept is that the reproductive cells of the unborn child are formed during his stay in the womb, and it is they who determine what the descendants of this unborn baby will be like. The more aggressive factors affect the body of a pregnant woman (hypovitaminosis, smoking, stress, etc.), the higher the risk of various anomalies in subsequent generations. It is obvious that doctors must necessarily instill in each of their patients the idea that her lifestyle during pregnancy can affect the health of not only her children, but also her grandchildren.
An analysis of the actual nutrition of pregnant women showed that the intake of vitamins A, C, B1, B2, folic acid and most minerals does not reach the recommended intake norms (RDA). The diet of a modern woman, even the most varied and made up of natural products, is not able to provide the body with the necessary amount of vitamins and minerals, especially during pregnancy. This is due to a decrease in energy consumption by almost two times compared with the energy consumption of previous generations [2, 3].
This is due to a decrease in energy consumption by almost two times compared with the energy consumption of previous generations [2, 3].
Insufficient provision of micronutrients to women before conception and during pregnancy leads to the development of a number of congenital malformations of the fetus. According to Rosstat, there is currently a steady increase in congenital malformations (CMDs). Over the past 14 years in Russia, the number of children with congenital anomalies has increased significantly: from 172.4 thousand in 2000 to 277.9 thousand in 2014 or, if counted per 100 thousand children, from 659.5 to 1154 ,8 respectively [4].
It was found that some fetal CMs are preventable, in particular, taking various vitamins in the preconception period and in early pregnancy can reduce the risk of malformations. Thus, taking vitamins during preparation and in early pregnancy is a method of primary prevention of congenital malformations. The most convincing evidence is in favor of the preventive effect of folic acid. Failure to prescribe folic acid at the stage of preparation for pregnancy, prescribed by the procedures for providing medical care and clinical recommendations developed and approved in accordance with Part 2 of Article 76 of the Federal Law of November 21, 2011 No. 323-FZ "On the Fundamentals of Protecting the Health of Citizens in the Russian Federation", is a defect medical care [5].
Failure to prescribe folic acid at the stage of preparation for pregnancy, prescribed by the procedures for providing medical care and clinical recommendations developed and approved in accordance with Part 2 of Article 76 of the Federal Law of November 21, 2011 No. 323-FZ "On the Fundamentals of Protecting the Health of Citizens in the Russian Federation", is a defect medical care [5].
An obstetrician-gynecologist must remember that by regulating the diet, providing a woman with the necessary vitamins and minerals, it is possible to reduce the risk of developing congenital anomalies.
The role of folic acid and iron in the IUD at the planning stages and in the first trimester of pregnancy
Reception at the planning stages and in the first trimester of IUDs containing trace elements, iron and folic acid can significantly improve the prospects for the birth of a healthy child and the course of pregnancy. These are the results of a review published in 2015 by Cochrane, a global independent body of researchers and health experts. The review included 17 randomized controlled trials involving 137 791 women. According to the expert advisory group of the review authors, the use of complexes containing iron and folic acid (for example, Elevit® Pronatal) demonstrates a 12% reduction in the risk of having a child with a deficiency of weight, by 10% in the risk of neonatal malnutrition, as well as 9% risk of stillbirth compared with iron-only preparations with or without folic acid [6]. It was also noted that taking complexes containing folic acid and iron at an early stage of pregnancy further reduces the likelihood of preterm birth. Based on the results of the meta-analysis, the expert advisory group developed recommendations for the inclusion of complexes containing iron and folic acid in national programs for adolescent health and reproductive health.
The review included 17 randomized controlled trials involving 137 791 women. According to the expert advisory group of the review authors, the use of complexes containing iron and folic acid (for example, Elevit® Pronatal) demonstrates a 12% reduction in the risk of having a child with a deficiency of weight, by 10% in the risk of neonatal malnutrition, as well as 9% risk of stillbirth compared with iron-only preparations with or without folic acid [6]. It was also noted that taking complexes containing folic acid and iron at an early stage of pregnancy further reduces the likelihood of preterm birth. Based on the results of the meta-analysis, the expert advisory group developed recommendations for the inclusion of complexes containing iron and folic acid in national programs for adolescent health and reproductive health.
Folic acid deficiency during pregnancy is one of the most well-known and preventable causes of congenital malformations caused by neural tube defects, other congenital malformations: the cardiovascular system, urinary tract, limbs, etc. , as well as malnutrition and prematurity. It is important to understand that the neural tube of the embryo is formed in the earliest stages of pregnancy and is completely closed by the 28th day of intrauterine development. In this regard, it is extremely important to saturate the body of the expectant mother with folates even before pregnancy [5]. Folic acid intake should begin at least 3 months before. before conception and continue throughout pregnancy and lactation. It should be emphasized that a dose of 800 mcg/day of folic acid is optimal for most women, because unreasonably high doses - more than 1 mg/day increase the risk of adverse effects, and low doses - 200-400 mcg/day not in all cases provide adequate protection against folate-dependent defects. Thus, heterozygous carriers of defective alleles of the MTHFR (methylenetetrahydrofolate reductase) gene need more folate, so the standard dose of 400 µg of folic acid (or 200 µg of folic acid + 200 µg of methylfolate) is insufficient for them, while the dose of 800 µg covers the needs of most women [7 ].
, as well as malnutrition and prematurity. It is important to understand that the neural tube of the embryo is formed in the earliest stages of pregnancy and is completely closed by the 28th day of intrauterine development. In this regard, it is extremely important to saturate the body of the expectant mother with folates even before pregnancy [5]. Folic acid intake should begin at least 3 months before. before conception and continue throughout pregnancy and lactation. It should be emphasized that a dose of 800 mcg/day of folic acid is optimal for most women, because unreasonably high doses - more than 1 mg/day increase the risk of adverse effects, and low doses - 200-400 mcg/day not in all cases provide adequate protection against folate-dependent defects. Thus, heterozygous carriers of defective alleles of the MTHFR (methylenetetrahydrofolate reductase) gene need more folate, so the standard dose of 400 µg of folic acid (or 200 µg of folic acid + 200 µg of methylfolate) is insufficient for them, while the dose of 800 µg covers the needs of most women [7 ]. It should be recognized that, as a rule, women apply for the first time to the doctor already at the beginning of the first trimester without going through the pregnancy planning stage and without having previously received a sufficient amount of folate. As a result, low folate concentrations and, as a result, high concentrations of homocysteine in early pregnancy may increase the risk of congenital malformations and adversely affect the formation and attachment of the placenta, and hence the outcome of pregnancy [8]. In such a situation, the obstetrician-gynecologist should provide the woman with the optimal level of folate as soon as possible. It has been proven that the effective dose for the rapid accumulation of folate in the body is dose of 800 mcg/day as part of VMK (Fig. 1). In this case, the optimal level of folate in erythrocytes - 906 nmol / l is achieved in 4 weeks. [9].
It should be recognized that, as a rule, women apply for the first time to the doctor already at the beginning of the first trimester without going through the pregnancy planning stage and without having previously received a sufficient amount of folate. As a result, low folate concentrations and, as a result, high concentrations of homocysteine in early pregnancy may increase the risk of congenital malformations and adversely affect the formation and attachment of the placenta, and hence the outcome of pregnancy [8]. In such a situation, the obstetrician-gynecologist should provide the woman with the optimal level of folate as soon as possible. It has been proven that the effective dose for the rapid accumulation of folate in the body is dose of 800 mcg/day as part of VMK (Fig. 1). In this case, the optimal level of folate in erythrocytes - 906 nmol / l is achieved in 4 weeks. [9].
Recent scientific reviews focus on the role of vitamin D in maintaining a healthy pregnancy . Observational and interventional studies have shown that vitamin D supplementation improves immune function, providing the maternal immunological adaptation necessary to maintain a normal pregnancy [10]. Sufficient intake of vitamin D during pregnancy is of fundamental importance for the development of the fetal skeleton, the formation of tooth enamel, as well as the overall growth and development of the fetus. A Cochrane review confirmed that vitamin D supplementation in pregnant women increased blood levels of 25-hydroxyvitamin D and reduced the risk of preeclampsia, low birth weight, and preterm birth [11].
Observational and interventional studies have shown that vitamin D supplementation improves immune function, providing the maternal immunological adaptation necessary to maintain a normal pregnancy [10]. Sufficient intake of vitamin D during pregnancy is of fundamental importance for the development of the fetal skeleton, the formation of tooth enamel, as well as the overall growth and development of the fetus. A Cochrane review confirmed that vitamin D supplementation in pregnant women increased blood levels of 25-hydroxyvitamin D and reduced the risk of preeclampsia, low birth weight, and preterm birth [11].
Taking folic acid at a dose of 800 mcg in combination with the vital vitamins, minerals and trace elements contained in the Elevit® Pronatal preparation is one of the ways to meet the needs of pregnant women. Elevit® Pronatal has been proven to reduce the risk of congenital malformations of the fetus, improve the course of pregnancy. Elevit® Pronatal is recommended to be taken at the planning stage, during pregnancy and until the end of breastfeeding.
Unlike other IUDs, Elevit® Pronatal is the only placebo-controlled study that has proven its pronounced preventive efficacy against many malformations [12].
The observation was carried out for 6 years with the participation of 4753 pregnant women under the guidance of Professor E.I. Zeitzel (Hungary), one of the founders of the system of primary prevention of malformations and the founder of the International Monitoring System and the Register of Congenital Malformations. During the study, the participants were divided into two groups. One group took Elevit® Pronatal during the planning period and in the first trimester of pregnancy, the second, the control group, took placebo (Fig. 2). Clinical trials have shown that the IUD is 92% reduces the risk of developing neural tube defects, 81% reduces the risk of developing malformations of the extremities, 79% reduces the risk of developing malformations of the genitourinary system, and 58% reduces the risk of developing heart defects [12, 13].
In addition, an additional positive result was obtained: women who took Elevit® Pronatal were much less likely to complain of nausea and vomiting during pregnancy [14].
Subsequently, the complex underwent multiple clinical trials, including in our country.
2nd and 3rd trimester nutritional support
Deficiency of vitamins and minerals during pregnancy damages the health of mother and child, increases the risk of perinatal pathology, increases infant mortality, is one of the causes of prematurity, disorders of physical and mental development of children. Of particular importance for the growth and development of the fetus are iron, copper, zinc and magnesium, vitamins D, A, C, E and B2. Their deficiency further manifests itself in the form of a delay in the processes of hemoglobin formation, delayed sexual development, changes in bone tissue, and impaired immune adaptation.
Low iron (Fe) intake is the main cause of anemia. Russia, according to WHO data, is a country with a high level of anemia (Fig. 3) [15]. The need for iron during pregnancy increases by 100% [16]. In the second half of pregnancy, anemia is diagnosed 40 times more often than in the first weeks, while anemia in pregnant women in 90% of cases is of an iron deficiency nature. Anemia in a pregnant woman is an independent risk factor for the need for caesarean section, blood transfusion after childbirth, preterm birth, macrosomia, and hospitalization of the child in the neonatal intensive care unit [17].
Russia, according to WHO data, is a country with a high level of anemia (Fig. 3) [15]. The need for iron during pregnancy increases by 100% [16]. In the second half of pregnancy, anemia is diagnosed 40 times more often than in the first weeks, while anemia in pregnant women in 90% of cases is of an iron deficiency nature. Anemia in a pregnant woman is an independent risk factor for the need for caesarean section, blood transfusion after childbirth, preterm birth, macrosomia, and hospitalization of the child in the neonatal intensive care unit [17].
WHO experts have developed recommendations according to which a pregnant woman must take 60 mg of iron per day in combination with folic acid to prevent anemia and other iron deficiency conditions. (WHO recommendations for pregnant women, 2012) [18].
Pregnancy in the II-III trimesters is characterized by the rapid development of the organs and systems of the fetus. Taking the so-called "visual" vitamins (A, C, E and B2) will also have a beneficial effect on the development of the organ of vision. In general, the listed vitamins (A, C and E) are protectors of photochemical damage to the retina. Vitamin B2 (riboflavin) is involved in carbohydrate, protein and fat metabolism, and, in particular, in the cornea and lens. It promotes the conversion of carbohydrates into energy needed by the muscles of the eyes and oxygen metabolism, playing an important role in maintaining normal vision.
In general, the listed vitamins (A, C and E) are protectors of photochemical damage to the retina. Vitamin B2 (riboflavin) is involved in carbohydrate, protein and fat metabolism, and, in particular, in the cornea and lens. It promotes the conversion of carbohydrates into energy needed by the muscles of the eyes and oxygen metabolism, playing an important role in maintaining normal vision.
Elevit® Pronatal is a balanced preparation containing 60 mg of iron, essential microelements copper, zinc and magnesium, "visual" vitamins that contribute to the development of the fetus and the maintenance of pregnancy. In conclusion, we can say that the use of adequate IUDs, such as Elevit® Pronatal, allows us to provide nutritional programming for the health of a child, an adult, and even his descendants. It is important to understand that the most optimal is the use of IUDs from preconception to the end of lactation.
Prevention of vitamin deficiency in pregnant women is aimed at ensuring full compliance between vitamin requirements and their dietary intake.