Pregnancy and psychosis
Postpartum psychosis | Pregnancy Birth and Baby
Postpartum psychosis | Pregnancy Birth and Baby beginning of content6-minute read
Listen
If you or someone close to you is having thoughts of self-harm or you are worried for your baby’s safety, go to the nearest hospital emergency department or call triple zero (000) and ask for an ambulance.
Key facts
- Postpartum psychosis is a mental illness that can affect you in the first few weeks after giving birth.
- Your symptoms can appear suddenly, where you lose your ‘sense of reality’ including hallucinations, delusions, mood swings and behaviour changes.
- Postpartum psychosis is different from the more common condition called postnatal depression.
- You need to be diagnosed by a psychiatrist and usually you’ll need treatment in hospital with medicines.
- After getting appropriate treatment, you’re likely to make a full recovery.
What is postpartum psychosis?
Postpartum psychosis is a rare but serious mental illness that can develop soon after you give birth, and can cause major changes in your mood and behaviour. If you think you (or someone you know) could have postpartum psychosis, it’s important to see a doctor without delay.
Postpartum psychosis (also called postnatal psychosis or puerperal psychosis) is a mental illness that can affect anyone who gives birth. You’re at greatest risk if you have bipolar disorder or if you have experienced postpartum psychosis before. But you can also develop postpartum psychosis even if you don’t have any history of mental illness. The condition can come on very suddenly — sometimes within hours after you give birth, although they may take a couple of months to appear.
The word ‘psychosis’ refers to a loss of sense of reality. If you have postpartum psychosis, you may see or hear things that are not there (hallucinations), feel everyone is against you (paranoia) and experience powerful delusions (beliefs that don’t match with reality).
If you have postpartum psychosis you will need specialised psychiatric treatment to get better.
Postpartum psychosis is not the same as postnatal depression. While postnatal depression affects more than 1 in 7 new mothers each year in Australia, postpartum psychosis is rare, affecting only about 1 or 2 in every 1,000 mothers.
Postpartum psychosis causes significant changes to your mood and behaviour. Your mood may become manic (lots of energy and racing thoughts), psychotic (an altered sense of reality) and/or you may feel depressed (low energy and mood).
Your symptoms may include:
- extreme sudden mood swings
- being aggressive, violent or agitated
- speaking in a disordered or nonsensical way, and finding it hard to concentrate
- feeling paranoid, having irrational or delusional thoughts or beliefs
- having hallucinations and changes in sense perception (like smelling, hearing or seeing things that are not there)
- not being able to sleep, sometimes for days
- responding in an unusual or inappropriate way towards your baby
- thinking of or planning to harm yourself or your baby
Symptoms of postpartum psychosis usually start to show in the first week or 2 after you’ve given birth, although they may take up to 12 weeks to appear.
If you notice these changes in yourself, or someone close to you, it’s important you seek professional help. See your GP, local hospital emergency department, or call a support service such as the ForWhen helpline or one of the others listed at the end of this article.
How is postpartum psychosis diagnosed?
Postpartum psychosis is a very serious mental illness that is diagnosed by a psychiatrist. If your doctor thinks you may have postnatal psychosis, they may admit you to hospital for psychiatric assessment and care.
How is postpartum psychosis treated?
Postpartum psychosis is treatable. After getting the necessary treatment, you are likely to make a full recovery.
To begin with, you will most likely need to go to hospital, where you will be safe, and doctors can monitor you closely. This first phase of treatment can take weeks or months, depending on your symptoms and how well you respond to treatment. It will take time and further treatment for you to recover fully.
Treatment options for postpartum psychosis include:
- Medications such as antidepressants, mood stabilisers, and antipsychotic medicines.
- Ectroconvulsive therapy (a process that stimulates brain neurons with an electric current to treat mania, psychosis and severe depression). You might need this if your symptoms are severe, medicines alone are not working and your symptoms mean you’re at high risk (for example, if you are at risk of self-harm).
- Psychological therapies, such as cognitive behaviour therapy (CBT).
How can I help my partner, family or friend if I think they might have postpartum psychosis?
If you suspect your partner or loved one is showing signs of postpartum psychosis, you may need to arrange urgent treatment. While this may be difficult, it is necessary. Both the mother and the baby could be at risk, and delaying treatment can make things more complex and mean recovery take longer.
If you or someone close to you is having thoughts of self-harm or you are worried for your baby’s safety, go to the nearest hospital emergency department or call triple zero (000) and ask for an ambulance.
Where can I go for advice and support?
Experiencing or caring for someone during a mental health crisis can be frightening, but help is available 24 hours a day.
- Ask your GP or maternal health nurse for advice.
- Call one of these support services:
- PANDA (Perinatal Anxiety & Depression Australia) — 1300 726 306
- ForWhen — 1300 24 23 22 (Monday to Friday, 9.00am to 4.30pm)
- Gidget Foundation — online and telehealth support — 1300 851 758
- Beyond Blue — 1300 22 4636
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Centre of Perinatal Excellence (COPE) (Management of postpartum psychosis), Centre of Perinatal Excellence (COPE) (Post-partum psychosis), PANDA (About post natal psychosis), PANDA (Postnatal anxiety and depression: signs and symptoms), Royal Women's Hospital (Post-partum psychosis)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2022
Back To Top
Related pages
- Postnatal depression
- Baby blues
Need more information?
Postpartum Psychosis | Peach Tree
Postpartum psychosis Postpartum or puerperal psychosis is a rare perinatal mood disorder about which most new mothers know very little or nothing at all
Read more on Peach Tree Perinatal Wellness website
Postpartum psychosis - COPE
COPE's purpose is to prevent and improve the quality of life of those living with emotional and mental health problems that occur prior to and within the perinatal period.
Read more on COPE - Centre of Perinatal Excellence website
Anxiety & Depression in Pregnancy & Early Parenthood
If you are reading this, you may have concerns about your thoughts, feelings or behaviours, or those of your partner or someone close to you who is pregnant or recently had a baby.
Read more on Perinatal Anxiety and Depression Australia (PANDA) website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Acute psychosis in pregnancy - A case managed effectively in accordance with the MBRRACE recommendations
Introduction
Women are at a higher risk of experiencing new-onset severe mental illness in the early postpartum period than at any other time in their lives. Almost a quarter of women who died between six weeks and one year postnatally died from psychiatric disorders [1].
The MBRRACE 2015 report identified a number of key messages to improve the care of pregnant women with mental illnesses. The report outlines ‘red flags’ which require urgent senior psychiatric assessment and considerations for admission to a mother and baby unit (Figures 1 and 2) [1]. Also highlighted is the importance of including a comprehensive psychiatric history in order to understand the progression of behavior. Furthermore, it is advised that an identified individual should co-ordinate care, where multiple mental health teams are involved [1]. The enquiry also details a new theme of partner and family involvement. This is especially important when a collateral history is required, particularly when capacity may be compromised. The MBRRACE enquiry also reports that some maternal deaths have been attributed to a failure in excluding organic causes, which may present as acute psychosis in pregnancy [1]. The case below is a successful model of how acute psychosis in pregnancy can be effectively managed in accordance to the recommendations of the MBRRACE 2015 report.
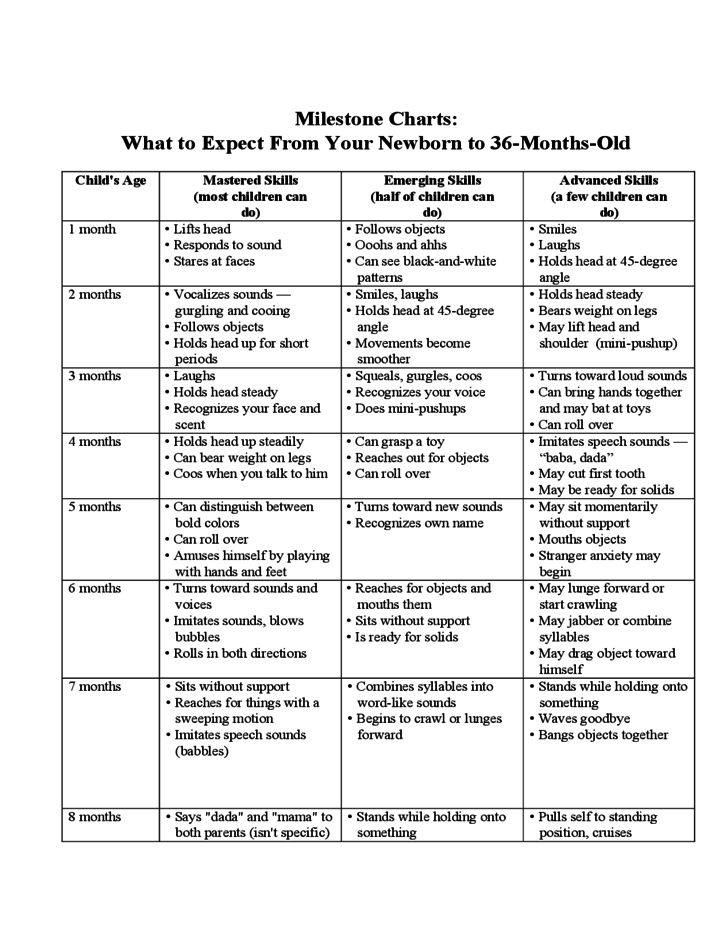
Figure 1: Red flags requiring urgent psychiatric assessment [1]
Figure 2: Criteria for admission to a mother and baby unit [1]
Case report
A multiparous 37-year-old woman, 36+5 weeks pregnant, was found at home by her 7-year-old son, on her knees with blood on her hands. She presented to the emergency department with suicidal ideation, extreme distress and evidence of self-harm. She was deluded regarding the safety of her children, including her unborn baby, stating that ‘they were all dead’. A collateral history taken from her husband revealed a three-week deterioration in her mood and that she had begun to reference films and books as part of her reality.
Her past medical history included: a congenital heart murmur and gestational diabetes, effectively managed by diet control and regular midwife reviews. As per the NICE guidelines, a depression and anxiety screen was carried out during the booking visit, to identify early signs of mental health problems that may arise during pregnancy [2]. On admission, the Consultant Obstetrician took a comprehensive collateral history from the husband, which ruled out any previous psychiatric history.
On admission, the Consultant Obstetrician took a comprehensive collateral history from the husband, which ruled out any previous psychiatric history.
A full examination was unable to be carried out due to her high levels of anxiety, but there was evidence of self-harm in the form of scratch marks on her stomach and an injury to the back of her head. She was not verbally responsive, but was continuously muttering ‘just kill me now’. Due to the severity of her presentation, the emergency psychiatric team was contacted immediately and reviewed the patient within the hour. A mental state examination revealed that the patient lacked capacity at the time. Following the psychiatric review, she was immediately commenced on olanzapine and lorazepam, and was transferred to the maternity ward with 1:1 registered mental nurse and ward staff care, allowing for continuous direct observations. Due to her potential suicide intentions, ligature risks were identified within the bay she was placed in. All staff were notified of the patient’s high suicidal risk and necessary measures were carried to minimise any potential risk to herself and others.
All staff were notified of the patient’s high suicidal risk and necessary measures were carried to minimise any potential risk to herself and others.
Once the patient was stabilized, investigations were performed to rule out possible organic causes such as: infection, hepatic encephalopathy, lupus, hypoglycaemia, thyroid dysfunction, electrolyte imbalance, substance abuse, trauma, space occupying lesions and domestic violence. Investigations carried out included: blood tests, blood cultures and arterial blood gases, urine MCS and toxicology screen, lupus screen, liver ultrasound and CT head. The CT scan showed no abnormalities however, blood results showed deranged liver function and metabolic acidosis and antibiotics were commenced in accordance with trust guidelines. Routine questions regarding domestic violence were also documented and ruled out.
Once the psychotic symptoms were stabilized, there was no indication for immediate delivery. However, a category 2 caesarean section was performed within 24 hours, due to an abnormal CTG, which showed foetal distress. The baby remained in special care post-birth due to peripheral cyanosis and some chest recession; leading to the patient expressing feelings of indifference and reduced bonding with her child. After discussion with the consultant psychiatrist, she was maintained on olanzapine and commenced on promethazine post-operatively. The liver function tests and acidosis normalised after the delivery of the baby.
The baby remained in special care post-birth due to peripheral cyanosis and some chest recession; leading to the patient expressing feelings of indifference and reduced bonding with her child. After discussion with the consultant psychiatrist, she was maintained on olanzapine and commenced on promethazine post-operatively. The liver function tests and acidosis normalised after the delivery of the baby.
Over the following days, she reported increased sleeping difficulties, which correlated with the deterioration in her mental state. On day four postnatally, she expressed distressing persecutory delusions and visual hallucinations. A subsequent psychiatric liaison assessment concluded that she was high risk and unfit for discharge. An admission to the Mother and Baby Unit (MBU) was discussed with the patient and her husband. As the patient voluntarily agreed to admission, sectioning under the mental health act was not required [3].
Discussion
Acute Psychosis in pregnancy is an obstetric emergency, due to the potential risk of death to both mother and baby. The MBRRACE report identifies numerous cases, which have resulted in fatal consequences, some of which were attributed to poor management. The MBRRACE (2006-2008) enquiry reported a case of a woman who became increasingly anxious throughout her normal pregnancy and developed delusional beliefs [4]. Although her mental health deteriorated postnatally, at no point was psychiatric referral considered. A diagnosis of anxiety was made; however, the community mental health team declined her referral [4]. A few weeks later this patient took her life by violent means. This case is an example where simple presentation, such as anxiety, can mask fatal diagnoses, resulting in the poorest of outcomes [4]. This highlights the importance of vigilance when dealing with psychotic symptoms in pregnancy and having a lower threshold for referral.
The MBRRACE report identifies numerous cases, which have resulted in fatal consequences, some of which were attributed to poor management. The MBRRACE (2006-2008) enquiry reported a case of a woman who became increasingly anxious throughout her normal pregnancy and developed delusional beliefs [4]. Although her mental health deteriorated postnatally, at no point was psychiatric referral considered. A diagnosis of anxiety was made; however, the community mental health team declined her referral [4]. A few weeks later this patient took her life by violent means. This case is an example where simple presentation, such as anxiety, can mask fatal diagnoses, resulting in the poorest of outcomes [4]. This highlights the importance of vigilance when dealing with psychotic symptoms in pregnancy and having a lower threshold for referral.
The MBRRACE (2006-2008) enquiry also outlines a case whereby the misattribution of physical symptoms to psychiatric illness led to the preventable death of a new mother [4]. A woman, with a known diagnosis of an autoimmune disorder, and an unremarkable psychiatric history, presented during pregnancy with complaints of lethargy and malaise. Although a psychiatric nurse assessment showed that the patient had no evidence of depressive illness, she was diagnosed with depression. She continued to deteriorate throughout her pregnancy and developed postnatal acute confusional state, which was again attributed to depression. The patient died shortly afterwards. The report suggested that the patient’s deteriorating physical and cognitive state was likely due to her underlying autoimmune condition [4]. This case highlights the importance of excluding all possible organic causes before making a psychiatric diagnosis. As this was our patient’s first presentation of psychosis, high clinical suspicion warranted all the appropriate investigations to exclude organic causes.
A woman, with a known diagnosis of an autoimmune disorder, and an unremarkable psychiatric history, presented during pregnancy with complaints of lethargy and malaise. Although a psychiatric nurse assessment showed that the patient had no evidence of depressive illness, she was diagnosed with depression. She continued to deteriorate throughout her pregnancy and developed postnatal acute confusional state, which was again attributed to depression. The patient died shortly afterwards. The report suggested that the patient’s deteriorating physical and cognitive state was likely due to her underlying autoimmune condition [4]. This case highlights the importance of excluding all possible organic causes before making a psychiatric diagnosis. As this was our patient’s first presentation of psychosis, high clinical suspicion warranted all the appropriate investigations to exclude organic causes.
Evidence supports Mother and Infant Bonding (MIB) in the form of skin-skin contact [5]. This was significantly reduced from birth due to multiple factors. For example, due to the baby’s own health concerns, specialist care was required, away from the mother’s bedside. Efforts were made by the maternity ward staff to encourage MIB with supervised interactions including feeding and changing the baby. The husband was also encouraged to assist in these daily activities and thereby, supporting the mother and creating a safe environment for mother and baby.
For example, due to the baby’s own health concerns, specialist care was required, away from the mother’s bedside. Efforts were made by the maternity ward staff to encourage MIB with supervised interactions including feeding and changing the baby. The husband was also encouraged to assist in these daily activities and thereby, supporting the mother and creating a safe environment for mother and baby.
Due to her antipsychotic medication, she was advised to avoid breast-feeding, which further impeded on MIB. There is limited data on the safety of antipsychotic medication in pregnancy and the post-natal period, however the NICE guidelines state that there are no specific contraindications. However, guidelines state that a discussion should be had with patients regarding the risks and benefits of treatment. She was continued on antipsychotics and vigorously monitored by the psychiatric team, obstetric consultant and mental health nurse. However, due to the fluctuating nature of post-partum psychosis, she was referred and admitted to the mother and baby unit for close monitoring.
Furthermore, patients should be advised, that this may be the primary presentation of bipolar affective disorder; the patient and the family should be advised on how to identity ‘red flag’ symptoms. Similarly, the patient should be told that this episode of pregnancy-related psychosis may re-present, requiring closer monitoring in subsequent pregnancies. Further follow- up was not possible with this patient after discharge from mother and baby unit, however the importance of continuous monitoring for these patients should not be over-looked. Additionally, in line with the NICE guidelines on suspected child abuse and neglect, child protection officer and social services were contacted, as other children were involved [6].
This interesting case shows how the NICE guidelines can be effectively applied in practice, along side adhering to the recommendations outlined in the MBBRACE 2015 report.
References
- Cantwell R, Knight M, Oates M, Shakespeare J (2015) on behalf of the MBRRACE-UK mental health chapter writing group.
 Lessons on maternal mental health. In: Knight M, Tuffnell D, Kenyon S, Shakespeare J, Gray R, Kurinczuk JJ (Eds.) on behalf of MBRRACE-UK. Saving Lives, Improving Mothers’ Care - Surveillance of maternal deaths in the UK 2011-13 and lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009-13. Oxford: National Perinatal Epidemiology Unit, University of Oxford. Pp: 22-41.
Lessons on maternal mental health. In: Knight M, Tuffnell D, Kenyon S, Shakespeare J, Gray R, Kurinczuk JJ (Eds.) on behalf of MBRRACE-UK. Saving Lives, Improving Mothers’ Care - Surveillance of maternal deaths in the UK 2011-13 and lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009-13. Oxford: National Perinatal Epidemiology Unit, University of Oxford. Pp: 22-41. - NICE (2017) Antenatal and postnatal mental health: clinical management and service guidance.
- Department of Health (2015) Mental Health Act 1983: reference guide. (1st edn.) Norwich: TSO. 2021 Copyright OAT. All rights reserv
- Cantwell R, Clutton-Brock T, Cooper G, Dawson A, Drife J, et al. (2011) Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. BJOG 118 Suppl 1: 1-203. [Crossref]
- Cleveland, L., Hill, C.
 , Pulse, W., DiCioccio, H., Field, T. and White-Traut, R. (2017). Systematic Review of Skin-to-Skin Care for Full-Term, Healthy Newborns. J Obstet Gynecol Neonatal Nurs, 46: 857-869. [Crossref]
, Pulse, W., DiCioccio, H., Field, T. and White-Traut, R. (2017). Systematic Review of Skin-to-Skin Care for Full-Term, Healthy Newborns. J Obstet Gynecol Neonatal Nurs, 46: 857-869. [Crossref] - NICE (2017) Child abuse and neglect. NICE guideline.
Editorial Information
Editor-in-Chief
Alessandro Buda
University of Milano Bicocca
Italy
Article Type
Case Report
Publication History
Received: November 05, 2017
Accepted: December 01, 2017
Published:December 05, 2017
Copyright
©2017 Jain E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Jain E (2017) Acute Psychosis in Pregnancy - A case managed effectively in accordance with the MBRRACE recommendations. 1: DOI: 10.15761/OGR.1000117
1: DOI: 10.15761/OGR.1000117
Figure 1: Red flags requiring urgent psychiatric assessment [1]
Figure 2: Criteria for admission to a mother and baby unit [1]
Psychosis in women (postpartum, during pregnancy)
Contents↓[show]
Psychosis is an acute disorder of mental functions, in which sudden mood swings occur, inappropriate behavior is noted, in some cases delusional thoughts and hallucinations appear. Signs of psychosis in women appear most acutely and rapidly against the background of hormonal changes or any shocks. Psychosis during pregnancy or after the birth of a child cannot be treated at home without the help of a specialist.
Specialists of the Yusupov Hospital offer comfortable conditions, quality service and high-level medical care to patients. Psychiatrists carry out complex treatment of various types of neurosis in patients over the age of 18 years.
Pregnancy psychosis
Pregnancy psychosis is a common condition characterized by a distorted perception of reality, depression, tearfulness and mood swings. Psychosis is most common in late pregnancy and persists for a period of time after the baby is born.
Psychosis is most common in late pregnancy and persists for a period of time after the baby is born.
Psychoses in pregnant women develop due to several reasons:
- hormonal changes;
- emotional instability and anxious expectations of future events;
- mental illness;
- hereditary predisposition to mental disorders;
- past infectious diseases and weakened immune system;
- intoxication of the body due to the use of alcohol or drugs;
- lack of vitamin B and other nutrients.
Severe stress during pregnancy is the greatest danger to the fetus. Psychosis, the symptoms and signs of which appear during pregnancy in women, can lead to low birth weight or premature birth. Women who, before pregnancy, noted the occurrence of stress in themselves under the influence of various stimuli, when planning a pregnancy, you should contact a psychiatrist to exclude psychosis when carrying a child.
Experienced psychiatrists at the Yusupov Hospital accompany patients with this problem throughout their pregnancy. Modern methods of correction allow you to effectively deal with the initial signs of emotional distress, anxiety and psychosis.
Modern methods of correction allow you to effectively deal with the initial signs of emotional distress, anxiety and psychosis.
Postpartum psychosis
Postpartum psychosis most often develops in women who give birth for the first time or in repeated births that are accompanied by complications. The period from 1 to 4 weeks after the birth of a child is the most dangerous for a woman, since against the background of hormonal changes, the likelihood of a mental disorder is high.
Depressive, asthenic condition, refusal to eat, depression and thoughts of suicide are serious reasons for seeking professional help at the Yusupov Hospital. Experts have found that women whose relatives have experienced postpartum psychosis are prone to this problem, so the likelihood of developing a mental disorder is 3%.
The Yusupov Hospital selects safe drugs and methods for the treatment of postpartum psychosis. Every day, experienced psychiatrists and psychologists interact with women, who consult patients after discharge. Postpartum psychosis in women is about 9% of the total number of cases of mental disorders in women.
Postpartum psychosis in women is about 9% of the total number of cases of mental disorders in women.
Signs of psychosis in women
Symptoms of psychosis in women are varied, so a psychiatrist can make a diagnosis after a comprehensive diagnosis. Psychosis in women during pregnancy or after childbirth may have the following manifestations:
- confusion and cognitive impairment;
- mood swings;
- not accepting one's own state;
- increased anxiety or extremely positive mood;
- auditory or visual hallucinations;
- delusional thoughts;
- discrepancy between judgments and reality;
- lethargy, maintaining one posture for a long time.
In a state of psychosis, the behavior, thinking and emotional manifestations of a woman change. These changes do not allow to realistically assess the events and realize what is happening, therefore, to solve the problem, a woman needs the help of loved ones. Postpartum psychosis affects women's consciousness, so patients may be hospitalized and treated, so in some cases, relatives turn to the Yusupov hospital for help.
Postpartum psychosis affects women's consciousness, so patients may be hospitalized and treated, so in some cases, relatives turn to the Yusupov hospital for help.
When referring to a psychiatrist at the Yusupov hospital with this problem, a diagnosis is made, during which an experienced specialist studies the manifestations and nature of the symptoms. Some signs of a mental disorder may appear before the onset of psychosis and are good reasons to seek expert advice. Women before the onset of psychosis note sleep disturbance, lack of appetite, increased anxiety and irritability.
The appearance of fear, depression, problems when communicating with others are the first signs of a developing mental disorder, at this stage, a thorough examination and treatment can prevent serious consequences. When assisting patients with psychosis, psychiatrists at the Yusupov Hospital delicately justify the need for therapy, talk about the main activities and their expected impact on the mental state.
Treatment of psychosis in pregnancy
Postpartum psychosis in women whose symptoms require treatment at the initial stage of therapy is not a basis for registration. In addition, the treatment of this disorder in the Yusupov hospital is carried out anonymously. In most cases, a woman is not aware of the problem, so relatives turn to specialists for help.
Intense manifestations of psychosis during pregnancy or after childbirth may be hospitalized. Patients of the Yusupov hospital are accommodated in comfortable rooms and provided with the necessary hygiene products. Upon admission to the Yusupov hospital, a comprehensive diagnosis is carried out, during which physical problems can be identified, in this case, one of the areas of therapy is their elimination.
The treatment of psychosis in women is carried out in several stages. At the initial stage, the general practitioner, together with other specialists, takes measures to relieve symptoms. During this period, it is necessary to exclude breastfeeding, since the woman is shown taking drugs of various effects.
The next stage of treatment is psychotherapy. After stopping the manifestations of psychosis in women, there is an awareness of the problem, which can cause depression, feelings of guilt. To correct negative attitudes, the therapist uses modern techniques aimed at self-acceptance and stabilization of emotional manifestations. The support of loved ones is important in the treatment of psychosis in women, so relatives can visit the Yusupov hospital patient at any time.
For expert advice and GP visits, contact Yusupov Hospital staff and make an appointment by phone.
Psycho-emotional disorders during pregnancy. The need for their correction | Tyutyunnik V.L., Mikhailova O.I., Chukhareva N.A.
Currently, more and more attention is paid to the influence of a woman's psycho-emotional state on reproductive function, pregnancy and perinatal outcomes [2,4,14]. In recent years, in developed countries, there has been an increase in the frequency of various mental disorders in women of reproductive age, the proportion of patients taking psychotropic drugs has increased, including among women who are planning a pregnancy and pregnant women [3,6,9].
Almost all pregnant women are subject to sharp emotional swings, since the expectation of a child is associated with changes - both physical and emotional. Hormonal changes during pregnancy lead to the fact that the mood of a pregnant woman changes dramatically almost every hour.
A future mother can get rid of such emotional swings and feel calm during pregnancy by observing the rules of emotional health. Emotional balance and physical fitness are equally important for a pregnant woman, they equally help her prepare for motherhood. Due to the lack of maternal experience, a pregnant woman may experience sudden emotional outbursts. The first pregnancy is a new experience that is quite difficult to comprehend. Ignoring the fact that the emotions of a woman who is expecting a child is much more complex and sharper than usual, can lead to a number of problems, including in relations with her spouse. Acceptance of this fact is the basis of emotional health during pregnancy [1,5,11].
Also, if a woman is pregnant for the first time, she experiences many fears, which include fear of childbirth and untimely termination of pregnancy, concern about the health of the unborn child and her own health, fear of labor pains and inevitable pain, fear of partner / spouse disappointment due to changes occurring with body. Modern women have to worry about careers, financial problems, and many additional costs associated with the appearance and upbringing of a new family member.
All these fears can lead to many negative emotions, such as anxiety, depression, irritation, anxiety, stress, anger, feelings of loneliness, confusion. Most often, changes in the psycho-emotional background during pregnancy lead to the development of depressive and anxiety disorders. Until the end, the pathogenesis of these changes is unclear, several theories are discussed, it is believed that changes in the hormonal background during pregnancy, including a significant increase in estrogens, and especially progesterone, in the blood serum can exacerbate existing emotional disorders [5,7,15]. As a rule, minor manifestations in the form of irritability, tearfulness, resentment accompany manifestations of early toxicosis in the first trimester of pregnancy - nausea, vomiting, etc. [6,10]. After the disappearance of these symptoms, the neuropsychic state of pregnant women usually improves. At the same time, an important role in the development of anxiety states is played by certain physical discomfort and psychological factors, which include forced changes in lifestyle, communication in the family and with work colleagues, concern for the health of the unborn child, financial difficulties - all this contributes to the appearance or exacerbation of psycho-emotional disorders during pregnancy. For some women, the onset of pregnancy is unexpected and not always desirable, however, due to the circumstances, a decision is made to prolong this pregnancy, which can lead to a further increase in stress and anxiety [5,8,12]. It should be noted that additional psychotraumatic factors may appear during pregnancy, such as the occurrence of pregnancy complications requiring hospitalization, or the detection of congenital malformations in the fetus, which can cause negative images and feelings [1,10,12].
As a rule, minor manifestations in the form of irritability, tearfulness, resentment accompany manifestations of early toxicosis in the first trimester of pregnancy - nausea, vomiting, etc. [6,10]. After the disappearance of these symptoms, the neuropsychic state of pregnant women usually improves. At the same time, an important role in the development of anxiety states is played by certain physical discomfort and psychological factors, which include forced changes in lifestyle, communication in the family and with work colleagues, concern for the health of the unborn child, financial difficulties - all this contributes to the appearance or exacerbation of psycho-emotional disorders during pregnancy. For some women, the onset of pregnancy is unexpected and not always desirable, however, due to the circumstances, a decision is made to prolong this pregnancy, which can lead to a further increase in stress and anxiety [5,8,12]. It should be noted that additional psychotraumatic factors may appear during pregnancy, such as the occurrence of pregnancy complications requiring hospitalization, or the detection of congenital malformations in the fetus, which can cause negative images and feelings [1,10,12].
The state of psycho-emotional stress with the presence of anxiety of various levels is observed in 40% of women with a normal pregnancy [2,7,11]. Borderline neuropsychiatric disorders can be presented in the form of hypochondriacal and hysterical syndromes. However, there are other forms of gestational borderline neuropsychiatric disorders, their features are the invariable inclusion in the clinical picture of certain psychopathological phenomena directly related to pregnancy: various fears for the successful course of pregnancy, obsessive fears for the fate of the fetus, expectation of childbirth, conditioned reflex fears associated with unfavorable past pregnancies and childbirth [5,6,8]. A study of pregnant women who do not have signs of borderline neuropsychiatric disorders showed that character accentuation was established only in a quarter of women. The first trimester of pregnancy is usually characterized to some extent by the sharpening of existing character traits. Soft, vulnerable, insecure women become even more impressionable, sometimes excessively tearful, and anxious (those women who have had miscarriages in the past or this pregnancy are not going well, in this case, the fear of another abortion can become simply obsessive) ). Powerful women with a sharp character can become even more aggressive, irritable and demanding. In the third trimester of pregnancy, emotional swings may begin again in connection with the expectation of childbirth, and with them fear - especially women who have to experience this event for the first time are susceptible to it [5,6,11].
Powerful women with a sharp character can become even more aggressive, irritable and demanding. In the third trimester of pregnancy, emotional swings may begin again in connection with the expectation of childbirth, and with them fear - especially women who have to experience this event for the first time are susceptible to it [5,6,11].
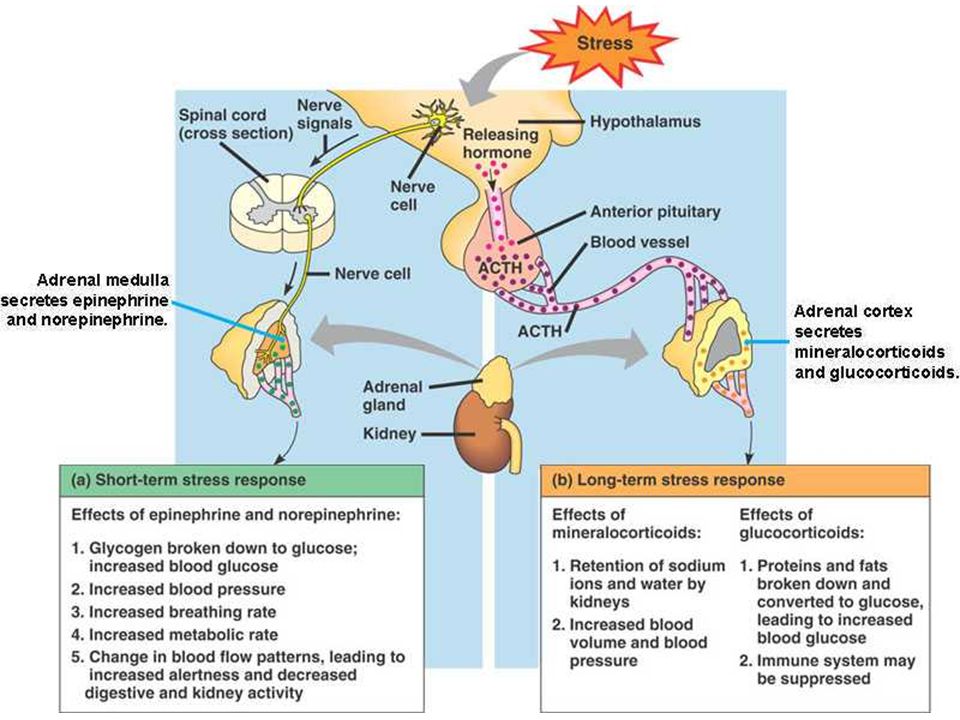
Anxiety disorders may first appear during pregnancy, there may be a change in the course of already existing disorders. In one retrospective study in women with panic attacks, 20% of cases showed a decrease in symptoms during pregnancy, 54% remained unchanged, and 26% worsened the course of the disease [12]. The detection of depression in pregnant women is difficult. Many symptoms, such as emotional lability, increased fatigue, changes in appetite and cognitive decline, are often found in physiologically normal pregnancy. Under stress, the hormones of the adrenal glands of the mother release catecholamines (stress hormones) into the blood, and during the experience of positive emotions (joy, calm, etc. ), the hypothalamic structures produce endorphins, which, penetrating through the placental barrier, directly affect the fetus. Consequently, mother and child are a single neurohumoral organism, and each of them equally suffers from the adverse influence of the outside world, which is recorded in long-term memory, affecting the entire subsequent life of the child. Positive maternal emotions cause an increase in the growth of the fetus and an increase in the level of its sensory perception.
), the hypothalamic structures produce endorphins, which, penetrating through the placental barrier, directly affect the fetus. Consequently, mother and child are a single neurohumoral organism, and each of them equally suffers from the adverse influence of the outside world, which is recorded in long-term memory, affecting the entire subsequent life of the child. Positive maternal emotions cause an increase in the growth of the fetus and an increase in the level of its sensory perception.
According to the literature [2,5,11,15], a significant effect of anxiety disorders on the course of pregnancy and perinatal outcomes has been noted: the frequency of placental insufficiency, fetal growth retardation, premature birth, the birth of children with low body weight, which subsequently affects negatively on long-term forecast for them.
Thus, emotional swings are dangerous not only for the woman herself, but also for her unborn child. When a pregnant woman experiences stress, her body produces more of the hormone cortisol, the main “stress hormone”. Cortisol increases blood pressure and blood sugar levels, negatively affects the strength of the immune system - which, of course, adversely affects the health of the child.
Cortisol increases blood pressure and blood sugar levels, negatively affects the strength of the immune system - which, of course, adversely affects the health of the child.
Stress during pregnancy is dangerous for a variety of reasons. Chronic stress experienced for several weeks can slow down the development of the cells of the body of the embryo, the growth of the fetus. This increases the risk of miscarriage or spontaneous abortion or premature birth. Elevated levels of stress hormones can damage the brain of an unborn baby and lead to parenting problems later on.
Psychological stress in the perinatal period brings with it a whole range of problems that require serious attention to the psychological sphere of a pregnant woman in order to avoid obstetric and other complications. However, diagnostic criteria for the transition of the stress syndrome from the link of adaptation to the link of pathogenesis of various diseases have not yet been found [2,4,15].
Emotional control is necessary to maintain normal emotional balance during pregnancy. A pregnant woman who successfully manages her emotions is aware of the changing emotional balance and is ready to accept what is happening to her.
A pregnant woman who successfully manages her emotions is aware of the changing emotional balance and is ready to accept what is happening to her.
There are several basic rules that will help to cope with emotional imbalance:
• You must come to terms with the fact that physical and emotional changes are an inevitable part of the pregnancy period. You need to understand that this is a temporary stage that will last only a few months and end a maximum of 1-2 months after the birth of the child.
• Each trimester of pregnancy brings new changes, both in the body and in the emotional state. The main source of information about pregnancy is special literature and the experience of women who have recently given birth, who can share their feelings and experiences.
• A pregnant woman is responsible for the emergence of a new life. Taking care of yourself means taking care of your child. Proper nutrition, rest and self-indulgence are essential.
• A pregnant woman should be open to dialogue and not be afraid to discuss her problems with a gynecologist, partner or friends - anyone who can provide emotional support. You should not keep fears and worries in yourself - this will only aggravate internal tension.
You should not keep fears and worries in yourself - this will only aggravate internal tension.
• Changes associated with pregnancy can lead to low energy and, as a result, rapid fatigue. You need to slow down, re-prioritize your work, and give yourself a break.
• Emotional tension and negative emotions can be overcome by being distracted by pleasant activities or hobbies. When emotions overwhelm you, try to analyze what is bothering you, and then find an adequate solution.
• Engaging in certain physical activities designed specifically for expectant mothers will help improve both physical and emotional health.
• The main components of emotional health during pregnancy are rest and comfort.
However, unfortunately, during pregnancy, a woman cannot always cope with nervous tension, irritability, anxiety, excitement and other symptoms of stress on her own. Therefore, in some situations, she needs medical help.
The relative risk of using drugs during pregnancy makes it difficult to choose therapy, therefore, for the correction of psycho-emotional disorders that occur during pregnancy, herbal drugs that have practically no side effects can be considered as highly safe therapy.
The basis of anti-anxiety complex herbal remedies is valerian. It has been used in traditional medicine for many years for its hypnotic and sedative effects and remains a highly sought after remedy to this day. The mild hypnotic effect of valerian makes it possible to use it for the relief of shallow insomnia caused by anxiety. In addition, the vegetotropic effect of valerian is well known, its ability to have a uniform effect on both mental and somatic (vegetative) symptoms of anxiety. Valerian preparations also have anxiolytic and neuroprotective effects. The spectrum of side effects of valerian is very narrow and practically limited only to allergic reactions. Although valerian extract is metabolized by the cytochrome P450 system, it has virtually no effect on the metabolism of other drugs, and thus unwanted drug interactions are excluded.
Among the phytopreparations used by clinicians for the treatment of psycho-emotional disorders, Persen, a modern combined sedative preparation of plant origin, is widely used to relieve stress symptoms (anxiety, irritability and emotional stress) without causing drowsiness. Along with valerian, the composition of the drug includes dry extracts of medicinal plants with pronounced anxiolytic activity - peppermint and lemon balm (Table 1). The additional antispasmodic effect of peppermint makes it possible to successfully use the drug in patients with a pronounced somatic component of the anxiety syndrome. In addition, lemon balm has a nootropic (increased concentration and speed of problem solving), antioxidant effect. Persen is administered orally to adults and adolescents over 12 years old, 2-3 coated tablets, 2-3 times / day, Persen forte - inside to adults and adolescents over 12 years old, 1-2 capsules 2-3 times / day.
Along with valerian, the composition of the drug includes dry extracts of medicinal plants with pronounced anxiolytic activity - peppermint and lemon balm (Table 1). The additional antispasmodic effect of peppermint makes it possible to successfully use the drug in patients with a pronounced somatic component of the anxiety syndrome. In addition, lemon balm has a nootropic (increased concentration and speed of problem solving), antioxidant effect. Persen is administered orally to adults and adolescents over 12 years old, 2-3 coated tablets, 2-3 times / day, Persen forte - inside to adults and adolescents over 12 years old, 1-2 capsules 2-3 times / day.
The advantages of Persen over other sedatives are:
• the preparation contains only natural ingredients;
• the effectiveness and safety of herbal ingredients Persena are well studied;
• does not contain alcohol and bromine;
• can be combined with any psychotropic drugs, including antidepressants;
• effective as a fast-acting symptomatic remedy when it is necessary to stop the symptoms of anxiety, agitation, and during a course of treatment for stress conditions, anxiety and phobic disorders.
Due to the natural components of plant origin that are part of Persen, this drug can be used during pregnancy. In each case, the doctor must evaluate the benefits and risks of taking Persen and other drugs, depending on the severity of the symptoms of the disease.
Thus, to prevent possible development, as well as to treat psycho-emotional disorders in pregnant women, it is advisable to use sedatives, the effect of which softens the damaging effects of psychogenic factors.
Literature
1. Abramchenko V.V., Kovalenko N.P. Perinatal psychology: Theory, methodology, experience. Petrozavodsk, 2004. 350s.
2. Avedisova A.S. Anxiety disorders // Alexandrovsky Yu.A. "Mental disorders in general medical practice and their treatment". M: GEOTAR-MED. 2004, pp. 66–73.
3. Voznesenskaya T.G., Fedotova A.V., Fokina N.M. Persen-forte in the treatment of anxiety disorders in patients with psychovegetative syndrome // Treatment of nervous diseases. 2002. No. 3 (8). pp. 38–41.
No. 3 (8). pp. 38–41.
4. Vorobieva O.V. Psychovegetative syndrome associated with anxiety (issues of diagnosis and therapy) // Russian Medical Journal. 2006. V.14. No. 23. S. 1696–1699.
5. Grandilevskaya I.V. Psychological features of women's response to the identified pathology of pregnancy: Abstract of the thesis. dis. ... cand. psychol. Sciences. SPb., 2004.
6. Kasyanova O.A. Socio-psychological factors in preparing women for pregnancy, childbirth and motherhood: Abstract of the thesis. dis. ... cand. psychol. Sciences. Yaroslavl, 2005.
7. Kovalenko N.P. Psychoprophylaxis and psychocorrection of women during pregnancy and childbirth: Abstract of the thesis. dis. … doc. psychol. Sciences. SPb., 2001.
8. Filippova G.G. Psychological readiness for motherhood // Reader on perinatal psychology: Psychology of pregnancy, childbirth and the postpartum period. M., Izd-vo URAO, 2005. 328 p.
9 Davidson J.R.T. Pharmacotherapy of generalized anxiety // J.