Excessive leg cramping
Causes, Pain Relief & Prevention
Overview
Leg Cramps at NightWhat are leg cramps?
Leg cramps are sudden, involuntary, intense muscle pains usually in your calf, foot or thigh. You might also know them as a “charley horse.” Sometimes the cramp may cause your leg to spasm – to tighten uncontrollably. Although painful to live with, cramps are generally harmless.
What does a leg cramp feel like?
A leg cramp feels like a clenched, contracted muscle tightened into a knot. It can be severely uncomfortable, painful or even unbearable. Your muscles in the area might hurt for hours after the cramp goes away.
How do I stop a leg cramp?
Try forcefully stretching the affected muscle (for example, stretch your calf muscle by flexing your foot upward). Jiggle your leg, massage it, or force yourself to walk. It might also help to apply ice or heat – use a heating pad or take a warm bath. (Read the “Management and Treatment” section for more tips. )
Unfortunately, there are no pills or injections that instantly relieve a leg cramp when it’s happening. There are, however, ways that may prevent the cramp from happening in the first place (see the “Prevention” section).
Can you get leg cramps at night?
Leg cramps at night happen when you’re not very active, or when you’re asleep. They may wake you up, make it harder for you to fall back asleep and leave you feeling sore all night. Yearly, monthly, weekly, nightly – the frequency of leg cramps depends on the person. Nocturnal leg cramps can happen to anyone at any age, but they happen most often to older adults. Of people over age 60, 33% will have a leg cramp at night at least once every two months. Nearly every adult age 50 and older will have them at least one time. Seven percent of children will, as well. Approximately 40% of pregnant women will experience leg cramps at night. The reason behind that is thought to be that the extra weight of pregnancy strains the muscles.
Three-quarters (75%) of all reported leg cramps happen at night.
How long do leg cramps last?
An instance of a leg cramp can last from several seconds to several minutes.
Who gets leg cramps?
The older you are, the more likely you are to have leg cramps. This is because your tendons (the tissues that connect your muscles to your bones) naturally shorten as you age. You’re also more likely to get them if you’re a woman. Up to 60% of adults get leg cramps at night, as do up to 40% of children and teenagers.
Are leg cramps a sign of something serious?
Leg cramps can sometimes be a symptom of a serious health condition. (See the “Symptoms and Causes” section.) If you are concerned that you have a serious health condition, don’t hesitate to contact your healthcare provider and report your symptoms, including your leg cramps.
How common are leg cramps?
Leg cramps are very common and normal, especially at night.
What is the difference between leg cramps and Restless Legs Syndrome (RLS)?
Although both nocturnal leg cramps (leg cramps at night) and restless legs syndrome tend to happen to you at night or when you’re at rest, restless legs syndrome doesn’t cause the severe pain. Restless legs syndrome is uncomfortable, but not agonizing. It’s a crawling sensation that makes you want to move your legs. When you do move, the restlessness stops, but there is still discomfort.
Restless legs syndrome is uncomfortable, but not agonizing. It’s a crawling sensation that makes you want to move your legs. When you do move, the restlessness stops, but there is still discomfort.
Symptoms and Causes
What causes leg cramps?
Some leg cramps happen for no known reason and they are called “idiopathic” cramps. “Secondary” leg cramps are a symptom or complication of a more serious health condition. The primary cause of idiopathic leg cramps is up for debate. Possible causes of them include:
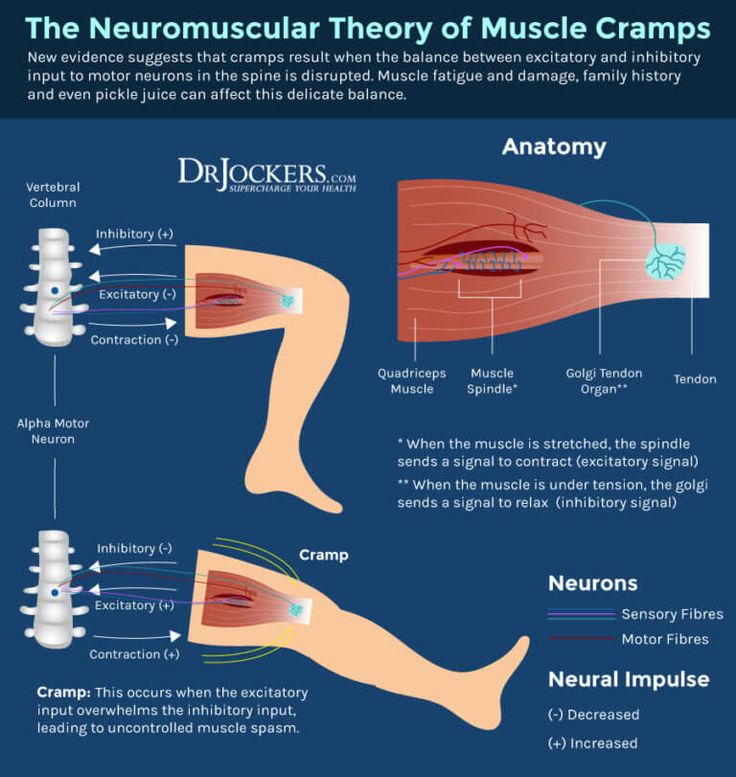
- Involuntary nerve discharges.
- Restriction in the blood supply.
- Stress.
- Too much high-intensity exercise.
Women who are pregnant often have leg cramps during the day and at night.
Possible causes for leg cramps at night (nocturnal leg cramps) include:
- Sitting for long periods of time.
- Overusing the muscles.
- Standing or working on concrete floors.
- Sitting improperly.
Leg cramps are not likely to cause:
- Broken bones.

- Fainting.
- Nausea.
- Numbness.
What medications may cause leg cramps?
Drugs have side effects. It’s possible that a prescription you’re taking could be causing your leg cramps. In that case, work closely with your healthcare provider to determine the pros and cons of the medication vs. its side effects. It’s possible that your healthcare provider may be able to put you on a different medication that doesn’t have leg cramps as a side effect. Medicines that have leg cramps as a side effect include:
- Albuterol/Ipratropium (Combivent®).
- Conjugated estrogens.
- Clonazepam (Klonopin®).
- Diuretics.
- Gabapentin (Neurontin®).
- Naproxen (Naprosyn®).
- Pregabalin (Lyrica®)
- Statins.
- Zolpidem (Ambien®).
Others may include: Amoxicillin, bromocriptine (Parlodel), bupropion (Wellbutrin), celecoxib (Celebrex®), cetirizine (Zyrtec), chromium, cinacalcet (Sensipar), ciprofloxacin (Cipro), citalopram (Celexa), donepezil (Aricept), eszopiclone (Lunesta), fluoxetine (Prozac), IV iron sucrose, lansoprazole (Prevacid), levalbuterol, levothyroxine, metformin, niconitis acid, nifedipine, rivastigmine (Exelon), sertraline (Zoloft), telmisartan (Micardis), teriparatide (Forteo®) and teriparatide raloxifene (Evista®).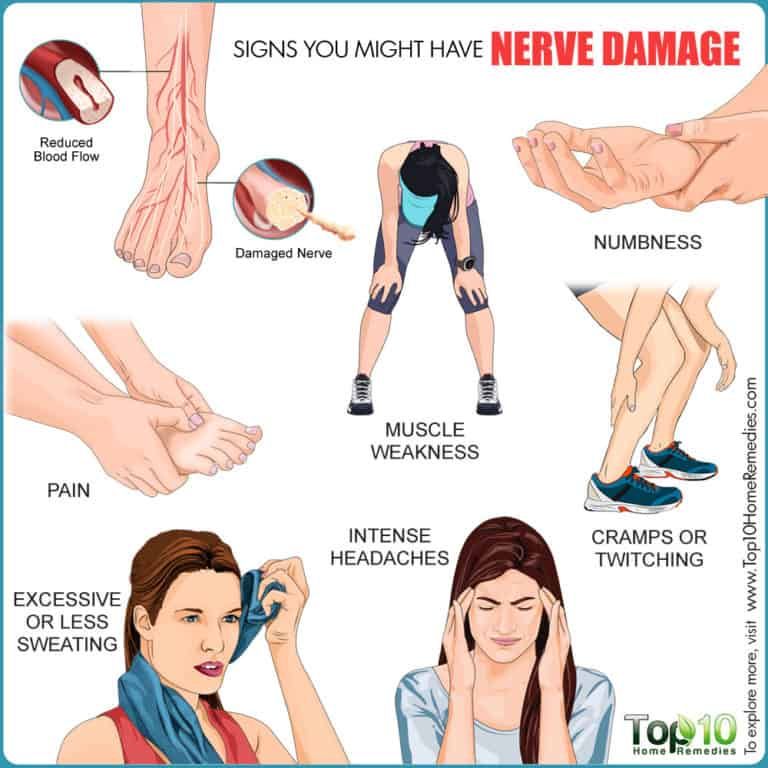
What medical problems can cause leg cramps?
Sometimes leg cramps happen to you for no reason, but other times they could possibly be a sign or symptom of a health condition. If you have any of the following conditions, it’s possible that your leg cramps are a result of that condition. Also keep in mind that if you don’t already know if you have any of these conditions, your leg cramps may be a sign that you do. Always consult your healthcare provider if you think your leg cramps are a symptom of a more serious medical condition.
Leg cramps can possibly be a sign of lifestyle choices such as:
- Alcoholism: An addiction to alcohol.
- Pregnancy.
- Dehydration: The lack of sufficient water in the body. (This sign is debated among experts.)
Leg cramps can also possibly be a sign of serious conditions including:
- ALS (amyotrophic lateral sclerosis/Lou Gehrig’s disease): Progressive neuromuscular disease.

- Cardiovascular disease: Heart conditions caused by blood clots or diseased blood vessels. Also, coronary artery disease: The narrowing or blockage of the coronary arteries.
- Cirrhosis of the liver: Scarring of the liver.
- Diabetes: A disease that prevents your body from properly using the energy from the food you eat.
- Flat feet: The absence of the supportive arch in the foot.
- Hypokalemia: Low potassium levels in your blood.
- Kidney failure (hemodialysis): A condition in which one or both kidneys no longer work correctly.
- Osteoarthritis (degenerative joint disease): The corrosion of the cartilage that protects your bones. Also, lumbar canal stenosis: A narrowing of the spinal canal in the lower back.
- Parkinson’s disease: A neurological movement disorder.
- Peripheral artery disease: Narrowing of the arteries.
 Also, peripheral neuropathy: Damage or dysfunction of one or more nerves.
Also, peripheral neuropathy: Damage or dysfunction of one or more nerves.
Cancer treatments like chemotherapy can cause nerve damage, which may cause leg cramps.
There are rumors that leg cramps can also be a sign of the following conditions. Fortunately, that is not the case. Leg cramps are unlikely to be a sign of:
- Labor (giving birth).
- Lung cancer.
- Menopause.
- Multiple sclerosis.
Leg cramps are not likely to be a sign of a deficiency in:
- Alanine transaminase.
- Albumin.
- Bilirubin.
- Calcium.
- Creatinine.
- Glucose.
- Magnesium.
- Zinc, vitamin B12 or vitamin D.
What are the warning signs that leg cramps are coming?
Unfortunately, leg cramps happen very suddenly. There are no warning signs. However, there are risk factors such as pregnancy and the use of medications that have leg cramps as a side effect.
Diagnosis and Tests
How are leg cramps diagnosed?
Your healthcare provider will need to know your medical history, medications and a description of what you’re experiencing. Be specific. Report your symptoms to your healthcare provider and include the following information:
Be specific. Report your symptoms to your healthcare provider and include the following information:
- When the leg cramps started happening.
- What your pain feels like.
- When the cramps happen (at night, for example, or after vigorous exercise).
- How long the cramps last.
- Any other symptoms you’re experiencing.
Your healthcare provider will need to tell the difference between your leg cramps from other conditions that may resemble them:
- Claudication.
- Peripheral neuropathy.
- Myositis.
- Restless legs syndrome.
To distinguish those differences, your healthcare provider may:
- Check the palpation of pulses.
- Evaluate physical sensations such as pinpricks.
- Test deep tendon reflexes.
- Test the strength of your leg.
Do I need to have any testing done to diagnose my leg cramps?
Blood, urine and other routine tests are not helpful in diagnosing leg cramps but they may help identify previously undiagnosed medical conditions that have leg cramps as a symptom. For example, your healthcare provider will likely perform typical tests such as taking your blood pressure, and that can reveal cardiac and vascular risks.
For example, your healthcare provider will likely perform typical tests such as taking your blood pressure, and that can reveal cardiac and vascular risks.
What questions might my healthcare provider ask about my leg cramps?
To help your healthcare provider diagnose you, they may ask the following questions about your leg cramps:
- When do you experience the leg cramps?
- How often do your leg cramps occur?
- How would you describe your leg cramps?
- How long do the leg cramps last?
- What medications are you currently taking?
- What known medical conditions do you have?
- Are you concerned about medical conditions that may be causing your leg cramps?
- Are you having any symptoms of another medical condition?
Management and Treatment
What can I do to make leg cramps go away if they happen?
You want to get rid of a leg cramp the moment it strikes. You might be finishing up an exercise routine, or you might be awakened in the middle of the night. In moments like that there are, unfortunately, no magical injections that can instantly relieve your pain. However, there are eight steps to take to possibly get rid of a leg cramp:
In moments like that there are, unfortunately, no magical injections that can instantly relieve your pain. However, there are eight steps to take to possibly get rid of a leg cramp:
- Stretch. Straighten your leg and then flex it, pulling your toes towards your shin to stretch the muscles.
- Massage. Use your hands or a roller to massage the muscles.
- Stand. Get up. Press your feet against the floor.
- Walk. Wiggle your leg while you walk around.
- Apply heat. Use a heating pad or take a warm bath.
- Apply cold. Wrap a bag of ice in a towel and apply it to the area.
- Pain killers. Take ibuprofen or acetaminophen to help with the pain.
- Elevate. Prop up your leg after the cramp starts to feel better.
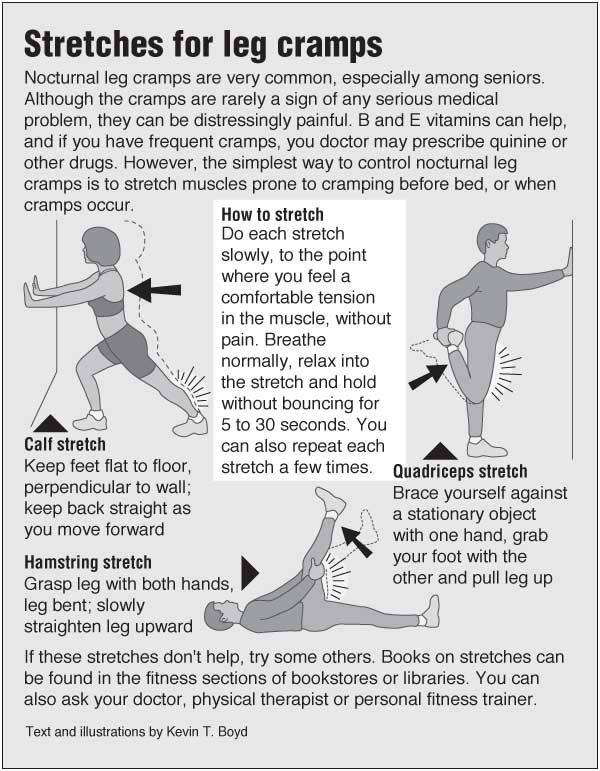
What kinds of stretches help get rid of leg cramps?
Try this if your cramp is in your calf muscle: While standing (or sitting with your leg unfolded before you), straighten your leg and lift your foot until your toes are pointing at your shin.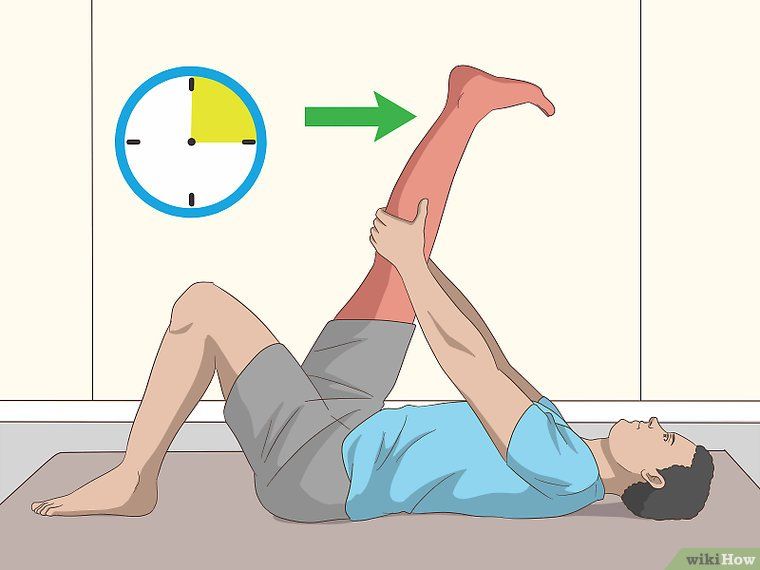 Pull on your toes if you are able to reach them. You could also try walking around on your heels.
Pull on your toes if you are able to reach them. You could also try walking around on your heels.
What medicines may help with leg cramps?
At this time, there is no recommended medication that can prevent leg cramps 100% of the time. However, there are some prescription medications that show a little evidence of preventing leg cramps. Under your healthcare provider’s watchful eye, you might want to try the following:
- Carisoprodol (Soma®): A muscle relaxant.
- Diltiazem (Cartia XT®): A calcium-channel blocker.
- Orphenadrine (Norflex®): Treats muscle spasms and relieves pain and stiffness in muscles.
- Verapamil: A calciuim-channel blocker.
What vitamins may help with leg cramps?
No vitamin is likely to help with a leg cramp 100% of the time. However, some experts do recommend that you take a vitamin B12 complex.
Does quinine help with leg cramps?
Quinine was thought to show some promise with healing leg cramps, but it is no longer recommended. There are potentially life-threatening side effects: arrhythmias, thrombocytopenia and hypersensitivity reactions.
There are potentially life-threatening side effects: arrhythmias, thrombocytopenia and hypersensitivity reactions.
When should I get my leg cramps treated at the Emergency Department?
Go to the emergency department (ED) if a leg cramp lasts longer than 10 minutes or becomes unbearably painful. Also go if a leg cramp happens after you touch a substance that could be poisonous or infectious. For example, if you have a cut in your skin that touches dirt, you could get a bacterial infection like tetanus. Exposure to mercury, lead or other toxic substances should also be reason to go to the emergency department.
Is there a surgery that could help with my leg cramps?
At this time, surgery is not recommended as a cure for leg cramps.
Prevention
How can I reduce my risk of getting leg cramps?
Experts can’t promise that you’ll never have a leg cramp again, but there are some steps you can take that might reduce your risk!
- Make sure that you stay hydrated – drink six to eight glasses of water each day.
 Don’t drink as much alcohol and caffeine.
Don’t drink as much alcohol and caffeine. - Adjust how you sleep. Use pillows to keep your toes pointed upwards if you sleep on your back. If you lie on your front, try hanging your feet over the end of the bed. Both positions can keep you in a relaxed position.
- Gently stretch your leg muscles before you go to sleep.
- Keep blankets and sheets loose around your feet so that your toes are not distorted.
- Wear shoes that fit you well and support your feet.
- Perform frequent leg exercises.
- Stretch your muscles before and after you exercise.
- Experiment with mild exercise right before bed. Walk on the treadmill or ride a bicycle for a few minutes.
What kinds of stretches help prevent leg cramps?
Try the following to prevent leg cramps in your calves: Stand about three feet (one meter) away from a wall. Lean forward. Touch the wall with your arms outstretched while keeping your feet flat. Count to five before you stop, and do it over and over again for at least five minutes. Repeat three times per day.
Repeat three times per day.
Outlook / Prognosis
Can leg cramps be cured?
Leg cramps don’t have a cure at this time. Fortunately, there are steps you can take to prevent leg cramps (see the “Prevention” section) and manage your leg cramps (see the “Management and Treatment” section).
Can leg cramps get worse?
The severity of a leg cramp is difficult if not impossible to predict. Some people see improvement with prevention and treatment plans, while others struggle. It is possible that your cramps will feel worse and happen more often as you age.
Living With
How do I take care of myself?Come up with a treatment plan with your healthcare provider that includes a prevention plan and an in-the-moment treatment plan. Ideas for a prevention plan include several activities you may want to do every day:
- Exercise: Do leg exercises during the day, and mild, brief walking or biking right before bed.

- Hydration: Drink eight glasses of water each day and avoid alcohol and caffeinated beverages.
- Medications and vitamins: Take all vitamins and medications (including muscle relaxants) exactly how they’re prescribed by your healthcare provider.
- Prepare your bed space: Keep a heating pad and massage roller next to your bed.
- Shoes: Purchase supportive shoes.
- Sleeping position: Experiment with different positions to see if one works better than another. Keep your toes up if you’re on your back and hang your feet over the end of the bed if you lie on your front.
- Stretch: Stretch your legs before and after exercising, and right before you go to sleep.
Your in-the-moment treatment plan could include the eight steps mentioned in the Management and Treatment section:
- Stretch. Straighten your leg and then flex it, pulling your toes towards your shin to stretch the muscles (using a towel can assist).
- Massage. Use your hands or a roller to massage the muscles.
- Stand. Get up. Press your feet against the floor.
- Walk. Wiggle your leg while you walk around.
- Apply heat. Use a heating pad or take a warm bath.
- Apply cold. Wrap a bag of ice in a towel and apply it to the area.
- Pain killers. Take ibuprofen or acetaminophen to help with the pain.
- Elevate. Prop up your leg after the cramp starts to feel better.
See your healthcare provider if your leg cramps are unbearably painful, happen frequently or last for a long time. Also, talk to your healthcare provider right away if you have any of the following symptoms in addition to leg cramps:
- Muscle cramps in other parts of your body.
- Significant pain.
- Swelling or numbness in the leg.
- Changes in the skin of your leg.
- Waking up over and over again with leg cramps.
- If your leg cramps are stopping you from getting enough sleep.
- If you have fluid abnormalities or electrolyte imbalances.
- See your healthcare provider immediately if you’re concerned that your leg cramps are a symptom of an underlying serious medical condition.
- Do you think that my leg cramps are a symptom of an underlying condition?
- Can you show me the best exercises I can do to stretch my muscles?
- Can you show me the best massage techniques I can use to help with my leg cramps?
- Is it safe for me to take medication for my leg cramps? Which medications should I take?
- Do you recommend that I see a physical therapist, sleep specialist, massage therapist, or other specialist?
- How can I help my child when they have a leg cramp?
- Should I keep an eye out for symptoms other than leg cramps that might indicate a more serious condition?
- How often should I come back to visit you about my leg cramps?
A note from Cleveland Clinic
Leg cramps can be unpredictable and agonizing. They can affect your sleep, your exercise routine and your general quality of life. They’re common – very normal – and, fortunately, temporary, and there are steps you can take to manage them. Do your best to avoid risk factors, avoid medications with leg cramps as a side effect and take recommended preventative measures.
They can affect your sleep, your exercise routine and your general quality of life. They’re common – very normal – and, fortunately, temporary, and there are steps you can take to manage them. Do your best to avoid risk factors, avoid medications with leg cramps as a side effect and take recommended preventative measures.
If you’re concerned about the severity and duration of your leg cramps, or think that they may be caused by a serious condition, don’t hesitate to contact your healthcare provider. Ask questions and voice your concerns. You don’t have to just “live with” leg cramps.
Causes, Pain Relief & Prevention
Overview
Leg Cramps at NightWhat are leg cramps?
Leg cramps are sudden, involuntary, intense muscle pains usually in your calf, foot or thigh. You might also know them as a “charley horse.” Sometimes the cramp may cause your leg to spasm – to tighten uncontrollably. Although painful to live with, cramps are generally harmless.
What does a leg cramp feel like?
A leg cramp feels like a clenched, contracted muscle tightened into a knot. It can be severely uncomfortable, painful or even unbearable. Your muscles in the area might hurt for hours after the cramp goes away.
It can be severely uncomfortable, painful or even unbearable. Your muscles in the area might hurt for hours after the cramp goes away.
How do I stop a leg cramp?
Try forcefully stretching the affected muscle (for example, stretch your calf muscle by flexing your foot upward). Jiggle your leg, massage it, or force yourself to walk. It might also help to apply ice or heat – use a heating pad or take a warm bath. (Read the “Management and Treatment” section for more tips.)
Unfortunately, there are no pills or injections that instantly relieve a leg cramp when it’s happening. There are, however, ways that may prevent the cramp from happening in the first place (see the “Prevention” section).
Can you get leg cramps at night?
Leg cramps at night happen when you’re not very active, or when you’re asleep. They may wake you up, make it harder for you to fall back asleep and leave you feeling sore all night. Yearly, monthly, weekly, nightly – the frequency of leg cramps depends on the person. Nocturnal leg cramps can happen to anyone at any age, but they happen most often to older adults. Of people over age 60, 33% will have a leg cramp at night at least once every two months. Nearly every adult age 50 and older will have them at least one time. Seven percent of children will, as well. Approximately 40% of pregnant women will experience leg cramps at night. The reason behind that is thought to be that the extra weight of pregnancy strains the muscles.
Nocturnal leg cramps can happen to anyone at any age, but they happen most often to older adults. Of people over age 60, 33% will have a leg cramp at night at least once every two months. Nearly every adult age 50 and older will have them at least one time. Seven percent of children will, as well. Approximately 40% of pregnant women will experience leg cramps at night. The reason behind that is thought to be that the extra weight of pregnancy strains the muscles.
Three-quarters (75%) of all reported leg cramps happen at night.
How long do leg cramps last?
An instance of a leg cramp can last from several seconds to several minutes.
Who gets leg cramps?
The older you are, the more likely you are to have leg cramps. This is because your tendons (the tissues that connect your muscles to your bones) naturally shorten as you age. You’re also more likely to get them if you’re a woman. Up to 60% of adults get leg cramps at night, as do up to 40% of children and teenagers.
Are leg cramps a sign of something serious?
Leg cramps can sometimes be a symptom of a serious health condition. (See the “Symptoms and Causes” section.) If you are concerned that you have a serious health condition, don’t hesitate to contact your healthcare provider and report your symptoms, including your leg cramps.
How common are leg cramps?
Leg cramps are very common and normal, especially at night.
What is the difference between leg cramps and Restless Legs Syndrome (RLS)?
Although both nocturnal leg cramps (leg cramps at night) and restless legs syndrome tend to happen to you at night or when you’re at rest, restless legs syndrome doesn’t cause the severe pain. Restless legs syndrome is uncomfortable, but not agonizing. It’s a crawling sensation that makes you want to move your legs. When you do move, the restlessness stops, but there is still discomfort.
Symptoms and Causes
What causes leg cramps?
Some leg cramps happen for no known reason and they are called “idiopathic” cramps. “Secondary” leg cramps are a symptom or complication of a more serious health condition. The primary cause of idiopathic leg cramps is up for debate. Possible causes of them include:
“Secondary” leg cramps are a symptom or complication of a more serious health condition. The primary cause of idiopathic leg cramps is up for debate. Possible causes of them include:
- Involuntary nerve discharges.
- Restriction in the blood supply.
- Stress.
- Too much high-intensity exercise.
Women who are pregnant often have leg cramps during the day and at night.
Possible causes for leg cramps at night (nocturnal leg cramps) include:
- Sitting for long periods of time.
- Overusing the muscles.
- Standing or working on concrete floors.
- Sitting improperly.
Leg cramps are not likely to cause:
- Broken bones.
- Fainting.
- Nausea.
- Numbness.
What medications may cause leg cramps?
Drugs have side effects. It’s possible that a prescription you’re taking could be causing your leg cramps. In that case, work closely with your healthcare provider to determine the pros and cons of the medication vs. its side effects. It’s possible that your healthcare provider may be able to put you on a different medication that doesn’t have leg cramps as a side effect. Medicines that have leg cramps as a side effect include:
its side effects. It’s possible that your healthcare provider may be able to put you on a different medication that doesn’t have leg cramps as a side effect. Medicines that have leg cramps as a side effect include:
- Albuterol/Ipratropium (Combivent®).
- Conjugated estrogens.
- Clonazepam (Klonopin®).
- Diuretics.
- Gabapentin (Neurontin®).
- Naproxen (Naprosyn®).
- Pregabalin (Lyrica®)
- Statins.
- Zolpidem (Ambien®).
Others may include: Amoxicillin, bromocriptine (Parlodel), bupropion (Wellbutrin), celecoxib (Celebrex®), cetirizine (Zyrtec), chromium, cinacalcet (Sensipar), ciprofloxacin (Cipro), citalopram (Celexa), donepezil (Aricept), eszopiclone (Lunesta), fluoxetine (Prozac), IV iron sucrose, lansoprazole (Prevacid), levalbuterol, levothyroxine, metformin, niconitis acid, nifedipine, rivastigmine (Exelon), sertraline (Zoloft), telmisartan (Micardis), teriparatide (Forteo®) and teriparatide raloxifene (Evista®).
What medical problems can cause leg cramps?
Sometimes leg cramps happen to you for no reason, but other times they could possibly be a sign or symptom of a health condition. If you have any of the following conditions, it’s possible that your leg cramps are a result of that condition. Also keep in mind that if you don’t already know if you have any of these conditions, your leg cramps may be a sign that you do. Always consult your healthcare provider if you think your leg cramps are a symptom of a more serious medical condition.
Leg cramps can possibly be a sign of lifestyle choices such as:
- Alcoholism: An addiction to alcohol.
- Pregnancy.
- Dehydration: The lack of sufficient water in the body. (This sign is debated among experts.)
Leg cramps can also possibly be a sign of serious conditions including:
- ALS (amyotrophic lateral sclerosis/Lou Gehrig’s disease): Progressive neuromuscular disease.

- Cardiovascular disease: Heart conditions caused by blood clots or diseased blood vessels. Also, coronary artery disease: The narrowing or blockage of the coronary arteries.
- Cirrhosis of the liver: Scarring of the liver.
- Diabetes: A disease that prevents your body from properly using the energy from the food you eat.
- Flat feet: The absence of the supportive arch in the foot.
- Hypokalemia: Low potassium levels in your blood.
- Kidney failure (hemodialysis): A condition in which one or both kidneys no longer work correctly.
- Osteoarthritis (degenerative joint disease): The corrosion of the cartilage that protects your bones. Also, lumbar canal stenosis: A narrowing of the spinal canal in the lower back.
- Parkinson’s disease: A neurological movement disorder.
- Peripheral artery disease: Narrowing of the arteries.
 Also, peripheral neuropathy: Damage or dysfunction of one or more nerves.
Also, peripheral neuropathy: Damage or dysfunction of one or more nerves.
Cancer treatments like chemotherapy can cause nerve damage, which may cause leg cramps.
There are rumors that leg cramps can also be a sign of the following conditions. Fortunately, that is not the case. Leg cramps are unlikely to be a sign of:
- Labor (giving birth).
- Lung cancer.
- Menopause.
- Multiple sclerosis.
Leg cramps are not likely to be a sign of a deficiency in:
- Alanine transaminase.
- Albumin.
- Bilirubin.
- Calcium.
- Creatinine.
- Glucose.
- Magnesium.
- Zinc, vitamin B12 or vitamin D.
What are the warning signs that leg cramps are coming?
Unfortunately, leg cramps happen very suddenly. There are no warning signs. However, there are risk factors such as pregnancy and the use of medications that have leg cramps as a side effect.
Diagnosis and Tests
How are leg cramps diagnosed?
Your healthcare provider will need to know your medical history, medications and a description of what you’re experiencing. Be specific. Report your symptoms to your healthcare provider and include the following information:
Be specific. Report your symptoms to your healthcare provider and include the following information:
- When the leg cramps started happening.
- What your pain feels like.
- When the cramps happen (at night, for example, or after vigorous exercise).
- How long the cramps last.
- Any other symptoms you’re experiencing.
Your healthcare provider will need to tell the difference between your leg cramps from other conditions that may resemble them:
- Claudication.
- Peripheral neuropathy.
- Myositis.
- Restless legs syndrome.
To distinguish those differences, your healthcare provider may:
- Check the palpation of pulses.
- Evaluate physical sensations such as pinpricks.
- Test deep tendon reflexes.
- Test the strength of your leg.
Do I need to have any testing done to diagnose my leg cramps?
Blood, urine and other routine tests are not helpful in diagnosing leg cramps but they may help identify previously undiagnosed medical conditions that have leg cramps as a symptom. For example, your healthcare provider will likely perform typical tests such as taking your blood pressure, and that can reveal cardiac and vascular risks.
For example, your healthcare provider will likely perform typical tests such as taking your blood pressure, and that can reveal cardiac and vascular risks.
What questions might my healthcare provider ask about my leg cramps?
To help your healthcare provider diagnose you, they may ask the following questions about your leg cramps:
- When do you experience the leg cramps?
- How often do your leg cramps occur?
- How would you describe your leg cramps?
- How long do the leg cramps last?
- What medications are you currently taking?
- What known medical conditions do you have?
- Are you concerned about medical conditions that may be causing your leg cramps?
- Are you having any symptoms of another medical condition?
Management and Treatment
What can I do to make leg cramps go away if they happen?
You want to get rid of a leg cramp the moment it strikes. You might be finishing up an exercise routine, or you might be awakened in the middle of the night. In moments like that there are, unfortunately, no magical injections that can instantly relieve your pain. However, there are eight steps to take to possibly get rid of a leg cramp:
In moments like that there are, unfortunately, no magical injections that can instantly relieve your pain. However, there are eight steps to take to possibly get rid of a leg cramp:
- Stretch. Straighten your leg and then flex it, pulling your toes towards your shin to stretch the muscles.
- Massage. Use your hands or a roller to massage the muscles.
- Stand. Get up. Press your feet against the floor.
- Walk. Wiggle your leg while you walk around.
- Apply heat. Use a heating pad or take a warm bath.
- Apply cold. Wrap a bag of ice in a towel and apply it to the area.
- Pain killers. Take ibuprofen or acetaminophen to help with the pain.
- Elevate. Prop up your leg after the cramp starts to feel better.
What kinds of stretches help get rid of leg cramps?
Try this if your cramp is in your calf muscle: While standing (or sitting with your leg unfolded before you), straighten your leg and lift your foot until your toes are pointing at your shin. Pull on your toes if you are able to reach them. You could also try walking around on your heels.
Pull on your toes if you are able to reach them. You could also try walking around on your heels.
What medicines may help with leg cramps?
At this time, there is no recommended medication that can prevent leg cramps 100% of the time. However, there are some prescription medications that show a little evidence of preventing leg cramps. Under your healthcare provider’s watchful eye, you might want to try the following:
- Carisoprodol (Soma®): A muscle relaxant.
- Diltiazem (Cartia XT®): A calcium-channel blocker.
- Orphenadrine (Norflex®): Treats muscle spasms and relieves pain and stiffness in muscles.
- Verapamil: A calciuim-channel blocker.
What vitamins may help with leg cramps?
No vitamin is likely to help with a leg cramp 100% of the time. However, some experts do recommend that you take a vitamin B12 complex.
Does quinine help with leg cramps?
Quinine was thought to show some promise with healing leg cramps, but it is no longer recommended. There are potentially life-threatening side effects: arrhythmias, thrombocytopenia and hypersensitivity reactions.
There are potentially life-threatening side effects: arrhythmias, thrombocytopenia and hypersensitivity reactions.
When should I get my leg cramps treated at the Emergency Department?
Go to the emergency department (ED) if a leg cramp lasts longer than 10 minutes or becomes unbearably painful. Also go if a leg cramp happens after you touch a substance that could be poisonous or infectious. For example, if you have a cut in your skin that touches dirt, you could get a bacterial infection like tetanus. Exposure to mercury, lead or other toxic substances should also be reason to go to the emergency department.
Is there a surgery that could help with my leg cramps?
At this time, surgery is not recommended as a cure for leg cramps.
Prevention
How can I reduce my risk of getting leg cramps?
Experts can’t promise that you’ll never have a leg cramp again, but there are some steps you can take that might reduce your risk!
- Make sure that you stay hydrated – drink six to eight glasses of water each day.
 Don’t drink as much alcohol and caffeine.
Don’t drink as much alcohol and caffeine. - Adjust how you sleep. Use pillows to keep your toes pointed upwards if you sleep on your back. If you lie on your front, try hanging your feet over the end of the bed. Both positions can keep you in a relaxed position.
- Gently stretch your leg muscles before you go to sleep.
- Keep blankets and sheets loose around your feet so that your toes are not distorted.
- Wear shoes that fit you well and support your feet.
- Perform frequent leg exercises.
- Stretch your muscles before and after you exercise.
- Experiment with mild exercise right before bed. Walk on the treadmill or ride a bicycle for a few minutes.
What kinds of stretches help prevent leg cramps?
Try the following to prevent leg cramps in your calves: Stand about three feet (one meter) away from a wall. Lean forward. Touch the wall with your arms outstretched while keeping your feet flat. Count to five before you stop, and do it over and over again for at least five minutes. Repeat three times per day.
Repeat three times per day.
Outlook / Prognosis
Can leg cramps be cured?
Leg cramps don’t have a cure at this time. Fortunately, there are steps you can take to prevent leg cramps (see the “Prevention” section) and manage your leg cramps (see the “Management and Treatment” section).
Can leg cramps get worse?
The severity of a leg cramp is difficult if not impossible to predict. Some people see improvement with prevention and treatment plans, while others struggle. It is possible that your cramps will feel worse and happen more often as you age.
Living With
How do I take care of myself?Come up with a treatment plan with your healthcare provider that includes a prevention plan and an in-the-moment treatment plan. Ideas for a prevention plan include several activities you may want to do every day:
- Exercise: Do leg exercises during the day, and mild, brief walking or biking right before bed.

- Hydration: Drink eight glasses of water each day and avoid alcohol and caffeinated beverages.
- Medications and vitamins: Take all vitamins and medications (including muscle relaxants) exactly how they’re prescribed by your healthcare provider.
- Prepare your bed space: Keep a heating pad and massage roller next to your bed.
- Shoes: Purchase supportive shoes.
- Sleeping position: Experiment with different positions to see if one works better than another. Keep your toes up if you’re on your back and hang your feet over the end of the bed if you lie on your front.
- Stretch: Stretch your legs before and after exercising, and right before you go to sleep.
Your in-the-moment treatment plan could include the eight steps mentioned in the Management and Treatment section:
- Stretch. Straighten your leg and then flex it, pulling your toes towards your shin to stretch the muscles (using a towel can assist).
- Massage. Use your hands or a roller to massage the muscles.
- Stand. Get up. Press your feet against the floor.
- Walk. Wiggle your leg while you walk around.
- Apply heat. Use a heating pad or take a warm bath.
- Apply cold. Wrap a bag of ice in a towel and apply it to the area.
- Pain killers. Take ibuprofen or acetaminophen to help with the pain.
- Elevate. Prop up your leg after the cramp starts to feel better.
See your healthcare provider if your leg cramps are unbearably painful, happen frequently or last for a long time. Also, talk to your healthcare provider right away if you have any of the following symptoms in addition to leg cramps:
- Muscle cramps in other parts of your body.
- Significant pain.

- Swelling or numbness in the leg.
- Changes in the skin of your leg.
- Waking up over and over again with leg cramps.
- If your leg cramps are stopping you from getting enough sleep.
- If you have fluid abnormalities or electrolyte imbalances.
- See your healthcare provider immediately if you’re concerned that your leg cramps are a symptom of an underlying serious medical condition.
- Do you think that my leg cramps are a symptom of an underlying condition?
- Can you show me the best exercises I can do to stretch my muscles?
- Can you show me the best massage techniques I can use to help with my leg cramps?
- Is it safe for me to take medication for my leg cramps? Which medications should I take?
- Do you recommend that I see a physical therapist, sleep specialist, massage therapist, or other specialist?
- How can I help my child when they have a leg cramp?
- Should I keep an eye out for symptoms other than leg cramps that might indicate a more serious condition?
- How often should I come back to visit you about my leg cramps?
A note from Cleveland Clinic
Leg cramps can be unpredictable and agonizing.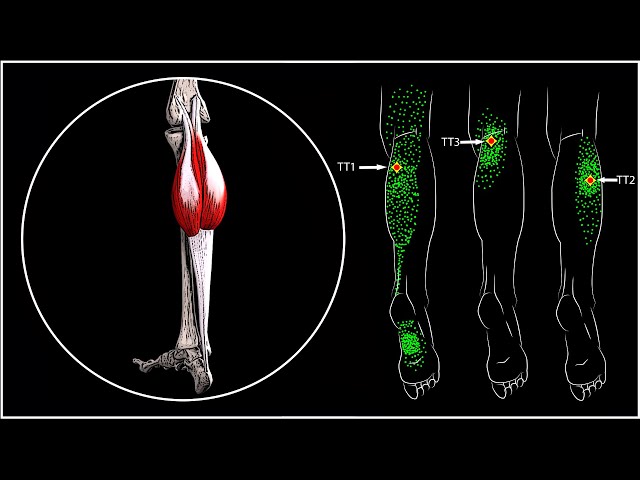 They can affect your sleep, your exercise routine and your general quality of life. They’re common – very normal – and, fortunately, temporary, and there are steps you can take to manage them. Do your best to avoid risk factors, avoid medications with leg cramps as a side effect and take recommended preventative measures.
They can affect your sleep, your exercise routine and your general quality of life. They’re common – very normal – and, fortunately, temporary, and there are steps you can take to manage them. Do your best to avoid risk factors, avoid medications with leg cramps as a side effect and take recommended preventative measures.
If you’re concerned about the severity and duration of your leg cramps, or think that they may be caused by a serious condition, don’t hesitate to contact your healthcare provider. Ask questions and voice your concerns. You don’t have to just “live with” leg cramps.
Leg cramps
Throughout life, probably, every person is faced with cramps, especially in the legs.
They are found both in absolutely healthy people and can be a symptom of some diseases.
A cramp is a sudden, involuntary spasm (contraction) of a muscle. It can occur during sleep, during physical exertion, and also at rest.
There are main types of seizures: tonic (prolonged and severe tension) and clonic (muscle twitching), as well as mixed.
Localization is more often in the calf and foot muscles, the contraction lasts from a few seconds to several tens of minutes and is facilitated by a strong stretching of the muscles. There are also complaints about the localization of seizures - hips, shoulder girdle, wrists, abdominal wall.
After a spasm, persistent soreness can persist for several hours or even days.
The most effective way to relieve spasm is to stretch the affected muscle.
Causes of leg cramps
Physiological - occurs after significant physical exertion, especially after a long period of low activity or in the absence of a warm-up before exercise, during pregnancy, with a sedentary lifestyle, hypothermia or overheating (during swimming in cool water, with heat stroke), dehydration of the body (with increased sweating, the use of a small amount of liquid).
Leg cramps in pregnant women are usually associated with micronutrient deficiencies, and only as an additional reason they mention poor circulation, varicose veins, and edema.
With the growth of the abdomen, due to a change in the center of gravity and weight gain, the calf muscles “clog”, become denser and shorter. This in itself impairs circulation, blood flow and lymph flow in the legs.
During intense training, microtraumas appear in the muscles and the transmission of nerve impulses that regulate muscle contraction and relaxation is disrupted. This can cause involuntary spasms.
Metabolic occur in various diseases: cirrhosis of the liver, renal failure, diabetes mellitus, diseases of the thyroid and parathyroid glands, lack of vitamins D and B, electrolyte disorders (deficiency of magnesium, potassium, calcium, iron), malabsorption syndrome, on the background of hyperthermia, infection and intoxication, with vascular pathology (chronic venous insufficiency), post-traumatic conditions.
In diabetes, the functioning of the autonomic nervous system is disrupted. The greatest loads are experienced by peripheral nerve endings in the limbs, which cause the development of neuropathy. And neuropathy in 40% of cases is accompanied by convulsions.
And neuropathy in 40% of cases is accompanied by convulsions.
In chronic venous insufficiency, stagnation of blood occurs in the veins, which causes swelling of tissues, disruption of local metabolism and, in particular, the mechanism of entry of magnesium, potassium, and calcium into cells. Spontaneous muscle contraction occurs, accompanied by severe soreness. To understand that it is the veins that are the cause - pay attention to the presence of edema, especially in the evening, discomfort and fatigue in the legs, itching and burning, especially in the feet, visible, well-drawn veins under the skin on the legs, spider veins and spider veins.
Redistribution of fluids in the body: true convulsions can also be noted in conditions where there is an unusual distribution of fluid in the body. An example is cirrhosis of the liver, in which there is an accumulation of fluid in the abdominal cavity (ascites). Similarly, seizures are a relatively common complication of the rapid changes in body fluids that occur during dialysis for kidney failure.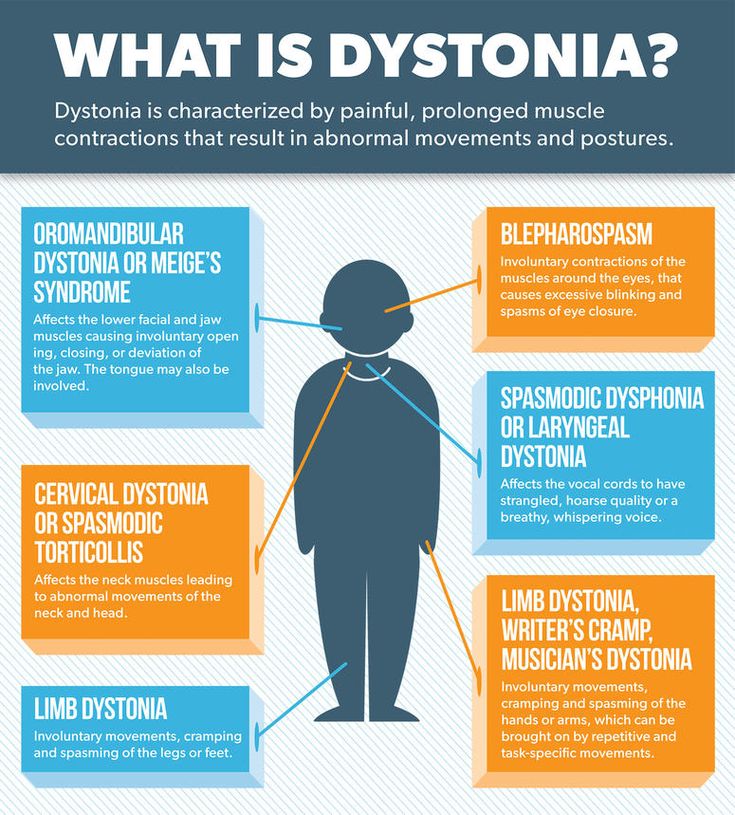
Seizures are seen in any circumstance that reduces the availability of calcium or magnesium in body fluids, such as after taking diuretics, hyperventilation, excessive vomiting, lack of calcium and/or magnesium in the diet, inadequate absorption of calcium due to vitamin D deficiency, reduced parathyroid function .
Low potassium levels: Low blood potassium levels sometimes cause muscle cramps, although muscle weakness is more common with hypokalemia.
A lack of certain vitamins can also lead directly or indirectly to muscle cramps. These include deficiencies in thiamine (B1), pantothenic acid (B5), and pyridoxine (B6). The exact role of deficiency of these vitamins in causing seizures is unknown.
Medications Convulsions may occur when taking drugs more often than diuretics, calcium channel blockers, statins, steroid hormones, retinoids, psychotropic drugs, immunosuppressants, etc.
Neurological may occur in diseases such as polyneuropathy, including dysfunction of the lumbar and sacral plexuses, flat feet, hereditary diseases, Parkinson's disease.
The basis is the deterioration of the innervation of the muscles that help pump blood from the lower extremities. With this variant of seizures, are characteristic:
- Lower back pain and fatigue
- Mobility restriction
- Presence of osteochondrosis and hernias
Spasms are often manifested against the background of stress and psycho-emotional stress.
Idiopathic convulsions ie when the cause cannot be found.
To reduce the risk of seizures, it is recommended:
- Balanced diet and intake of mineral and vitamin complexes
- Drinking mode
- Comfortable and rational footwear
- Exercise to stimulate the muscles of the legs
- massage, contrast shower
If convulsions are short-term and rarely occur, first of all it is necessary to assess the situation in which they occurred, perhaps they are physiological, but if they are frequent and prolonged, it is necessary to contact a specialist in person to exclude serious diseases. It must be remembered that convulsions are only a symptom.
It must be remembered that convulsions are only a symptom.
It is initially recommended to visit a therapist, if necessary, he will refer to a narrower specialist:
- Orthopedist
- Phlebologist
- Neurologist
- Vertebrologist
- Rheumatologist
- Endocrinologist
From laboratory diagnostics, can be offered:
- 250003 HPLC determination of vitamin B5 (pantothenic acid)
- 250004 HPLC determination of vitamin B6 (pyridoxine)
- 250002 Vitamin B1 (thiamine) determination by HPLC
- 0 Vitamin B12 (Cyanocobalamin)
- 0
Glycosylated hemoglobin
- 080002 Parathyroid hormone
- 300103 Thyroid function diagnostics (screening)
- 080006 25-OH Vitamin D (25-Hydroxyvitamin D)
- 110006 Complete blood count + ESR with leukocyte formula
- 0 Cholesterol (total)
- 0 Glucose
- 0 Urea
- 0
Creatinine
- 0
Gamma-glutamine transferase
- 0 Alkaline phosphatase
- 0
Alanine aminotransferase
- 0 Aspartate aminotransferase
- 0 Iron
- 0 Magnesium
- 0
Calcium (Ca2+), Sodium (Na+), Potassium (K+), Chlorine (Cl-)
References
- J.
 Wasson. Clinical symptoms: from patient complaints to differential diagnosis. A complete systematic guide. / Translation from English. Publishing house BINOM, Moscow, 2016 ISBN978-5-9518-0533-1
Wasson. Clinical symptoms: from patient complaints to differential diagnosis. A complete systematic guide. / Translation from English. Publishing house BINOM, Moscow, 2016 ISBN978-5-9518-0533-1 - Clinical guidelines (protocol) for the provision of emergency medical care for convulsions in children (Russian Society for Emergency Medicine Union of Pediatricians of Russia), 2015
- Neurology. Textbook. Suslina Z.A., Piradov M.A., Maksimova M.Yu. M.: Practice. 2015
- RUSSIAN CLINICAL RECOMMENDATIONS FOR THE DIAGNOSIS AND TREATMENT OF CHRONIC DISEASES OF THE VEINS, Association of Phlebologists of Russia All-Russian Society of Surgeons Approved by the expert meeting on 10.02.13, Moscow
Muscle cramps - treatment, symptoms, causes, diagnosis
- Muscle cramps are involuntary and intense muscle contractions without a period of relaxation.
- Almost everyone has experienced a seizure episode at least once in their life.
- There are different types of seizures and different causes.

- Many different medications can cause muscle cramps.
- In most cases, muscle cramps can be stopped by relaxing (stretching) the muscle.
- Muscle cramps can often be prevented by measures such as a nutritious diet with sufficient micronutrients and adequate fluid intake.
Muscle cramps is an involuntary and violent contraction of a muscle without a period of relaxation. When muscles that can be controlled voluntarily, such as the muscles of the arms or legs, are used, they alternately contract and relax as certain movements are made in the limbs. The muscles that support the head, neck and torso work in synchrony and maintain the position of the body. A muscle (or even a few muscle fibers) can be involuntarily in a state of spasm. If the spasm is strong and persistent, then this leads to the appearance of convulsions. Muscle cramps are often visualized or palpated in the region of the muscle involved.
Muscle cramps can last from a few seconds to a quarter of an hour, and sometimes longer. It is also not uncommon for the seizures to recur until the muscle relaxes. The spasmodic contractions may involve part of a muscle, the entire muscle, or several muscles that usually contract at the same time when performing movements, such as flexing several fingers. In some cases, cramps can be simultaneously in the antagonist muscles responsible for movements in opposite directions. Muscle cramps are widespread. Almost all people (according to some studies about 95% of people) have experienced seizures at some point in their lives. Muscle cramps are common in adults and become more common with age, but cramps can still occur in children. In any muscle (skeletal) in which voluntary movements are performed, there may be cramps. Cramps of the limbs, legs and feet, and especially the calf muscle, are very common.
It is also not uncommon for the seizures to recur until the muscle relaxes. The spasmodic contractions may involve part of a muscle, the entire muscle, or several muscles that usually contract at the same time when performing movements, such as flexing several fingers. In some cases, cramps can be simultaneously in the antagonist muscles responsible for movements in opposite directions. Muscle cramps are widespread. Almost all people (according to some studies about 95% of people) have experienced seizures at some point in their lives. Muscle cramps are common in adults and become more common with age, but cramps can still occur in children. In any muscle (skeletal) in which voluntary movements are performed, there may be cramps. Cramps of the limbs, legs and feet, and especially the calf muscle, are very common.
Types and causes of muscle cramps
Skeletal muscle cramps can be divided into four main types. These include "true" seizures, tetanic seizures, contractures, and dystonic seizures.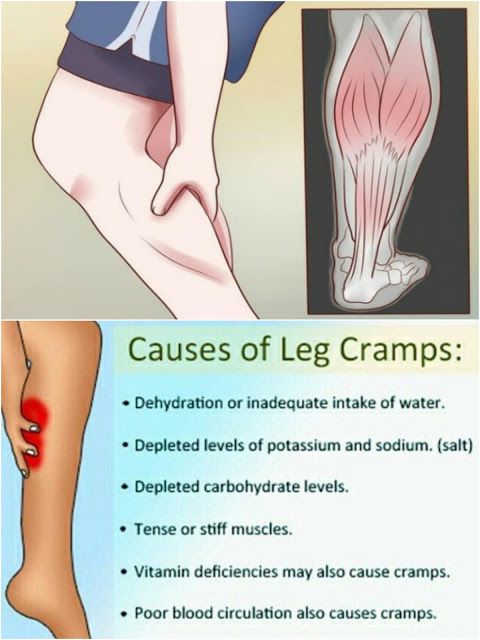 Seizures are classified according to the causes of the seizures and the muscle groups they affect.
Seizures are classified according to the causes of the seizures and the muscle groups they affect.
Types of muscle cramps
True cramps . True cramps involve part or all of a muscle or group of muscles that normally function together, such as the muscles involved in flexing several adjacent fingers. Most researchers agree that true cramps are caused by increased excitability of nerves that stimulate muscle contractions. They are overwhelmingly the most common type of skeletal muscle cramps. True seizures can occur in a variety of circumstances.
Injuries : Persistent muscle spasms may occur as a defense mechanism after an injury such as a broken bone. In this case, as a rule, spasm allows you to minimize movement and stabilize the area of injury. Injury to just the muscle can also lead to muscle spasm.
Vigorous activity: true cramps are usually associated with active muscle loading and muscle fatigue (during sports or unusual activities). Such convulsions can occur both during the activity and after, sometimes many hours later. In addition, muscle fatigue from sitting or lying down for a long period of time in an awkward position or any repetitive movement can also cause cramps. Older people are more at risk of seizures during vigorous or strenuous physical activity.
Such convulsions can occur both during the activity and after, sometimes many hours later. In addition, muscle fatigue from sitting or lying down for a long period of time in an awkward position or any repetitive movement can also cause cramps. Older people are more at risk of seizures during vigorous or strenuous physical activity.
Rest seizures : Rest seizures are very common, especially in the elderly, but can occur at any age, including childhood. Rest spasms often occur at night. Night cramps, while not life threatening, can be painful, disrupt sleep, and may recur frequently (i.e., many times a night and/or many nights a week). The actual cause of nighttime cramps is unknown. Sometimes these cramps are initiated by a movement that contracts the muscles. An example would be stretching the foot in bed, which shortens the calf muscle, where cramps are most common.
Dehydration : Sports and other strenuous exercise may cause excessive fluid loss through sweat. With this type of dehydration, the likelihood of true seizures increases. These cramps most often occur in warm weather and may be an early sign of heat stroke. Chronic dehydration due to diuretics and poor fluid intake can similarly lead to seizures, especially in the elderly. Seizures can also be associated with a lack of sodium.
With this type of dehydration, the likelihood of true seizures increases. These cramps most often occur in warm weather and may be an early sign of heat stroke. Chronic dehydration due to diuretics and poor fluid intake can similarly lead to seizures, especially in the elderly. Seizures can also be associated with a lack of sodium.
Redistribution of fluids in the body: true convulsions can also be noted in conditions where there is an unusual distribution of fluid in the body. An example is cirrhosis of the liver, in which there is an accumulation of fluid in the abdominal cavity (ascites). Similarly, seizures are a relatively common complication of the rapid changes in body fluids that occur during dialysis for kidney failure.
Low levels of electrolytes in the blood (calcium, magnesium): low blood levels of calcium or magnesium directly increase the excitability of the nerve endings innervating the muscles. This may be a predisposing factor for the spontaneous true seizures that many older people experience, and these seizures are also common in pregnant women.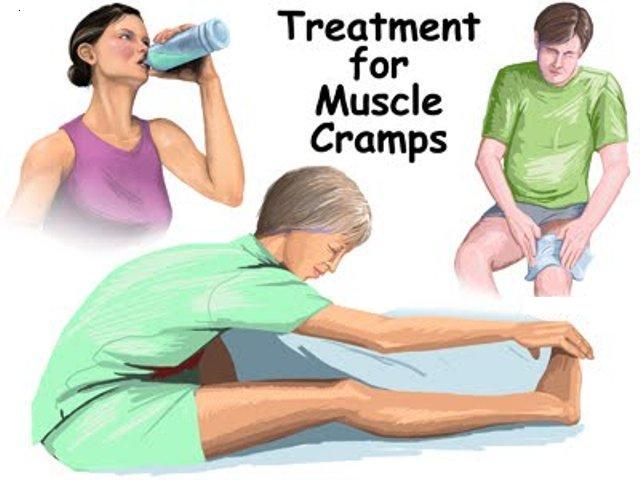 Low levels of calcium and magnesium are common in pregnant women, especially if these minerals are not getting enough from the diet. Seizures occur in any circumstance that reduces the availability of calcium or magnesium in body fluids, such as diuretics, hyperventilation, excessive vomiting, lack of calcium and/or magnesium in the diet, insufficient absorption of calcium due to vitamin D deficiency, reduced parathyroid function.
Low levels of calcium and magnesium are common in pregnant women, especially if these minerals are not getting enough from the diet. Seizures occur in any circumstance that reduces the availability of calcium or magnesium in body fluids, such as diuretics, hyperventilation, excessive vomiting, lack of calcium and/or magnesium in the diet, insufficient absorption of calcium due to vitamin D deficiency, reduced parathyroid function.
Low potassium levels: Low blood potassium levels sometimes cause muscle cramps, although muscle weakness is more common in hypokalemia.
Tetany
Tetany activates all nerve cells in the body, which then stimulate muscle contraction. In this type, convulsive contractions occur throughout the body. The name tetany comes from the spasms that occur when tetanus toxin affects the nerves. However, this name for this type of cramp is now widely used to refer to muscle cramps in other conditions, such as low blood levels of calcium and magnesium. Low levels of calcium and magnesium increase the activity of the nervous tissue non-specifically, which can lead to the appearance of tetanic seizures. Often these seizures are accompanied by signs of hyperactivity of other nerve functions in addition to muscle hyperstimulation. For example, low blood calcium not only causes muscle spasm in the hands and wrists, but it can also cause numbness and tingling sensations around the mouth and other areas of the body.
Low levels of calcium and magnesium increase the activity of the nervous tissue non-specifically, which can lead to the appearance of tetanic seizures. Often these seizures are accompanied by signs of hyperactivity of other nerve functions in addition to muscle hyperstimulation. For example, low blood calcium not only causes muscle spasm in the hands and wrists, but it can also cause numbness and tingling sensations around the mouth and other areas of the body.
Sometimes, tetanic convulsions are indistinguishable from true convulsions. Additional changes in sensation or other nerve function may not be noticeable, as the pain of a cramp may mask other symptoms.
Contractures
Contractures occur when muscles cannot relax for an even longer period than with the main types of muscle cramps. Constant spasms are caused by the depletion of adenosine triphosphate (ATP) - the energy intracellular substrate of the cell. This prevents relaxation of the muscle fibers. The nerves are inactive in this type of muscle cramp.
The nerves are inactive in this type of muscle cramp.
Contracture may be the result of genetic inheritance (eg, McArdle disease, which is a defect in the breakdown of glycogen to sugar in muscle cells) or acquired conditions (eg, hyperthyroid myopathy, which is a muscle disease associated with an overactive thyroid gland) . Convulsions of the type of contractures are rare.
Dystonic seizures
The last category of seizures are dystonic seizures, in which muscles not involved in the intended movement are affected and contracted. Muscles that are involved in this type of cramp include antagonistic muscles that usually work in the opposite direction of the intended movement and/or others that enhance the movement. Some dystonic spasms usually affect small muscle groups (eyelids, cheeks, neck, larynx, etc.). The arms and hands may be affected during repetitive movements such as writing (writer's cramp), playing a musical instrument. These activities can also lead to true cramps due to muscle fatigue.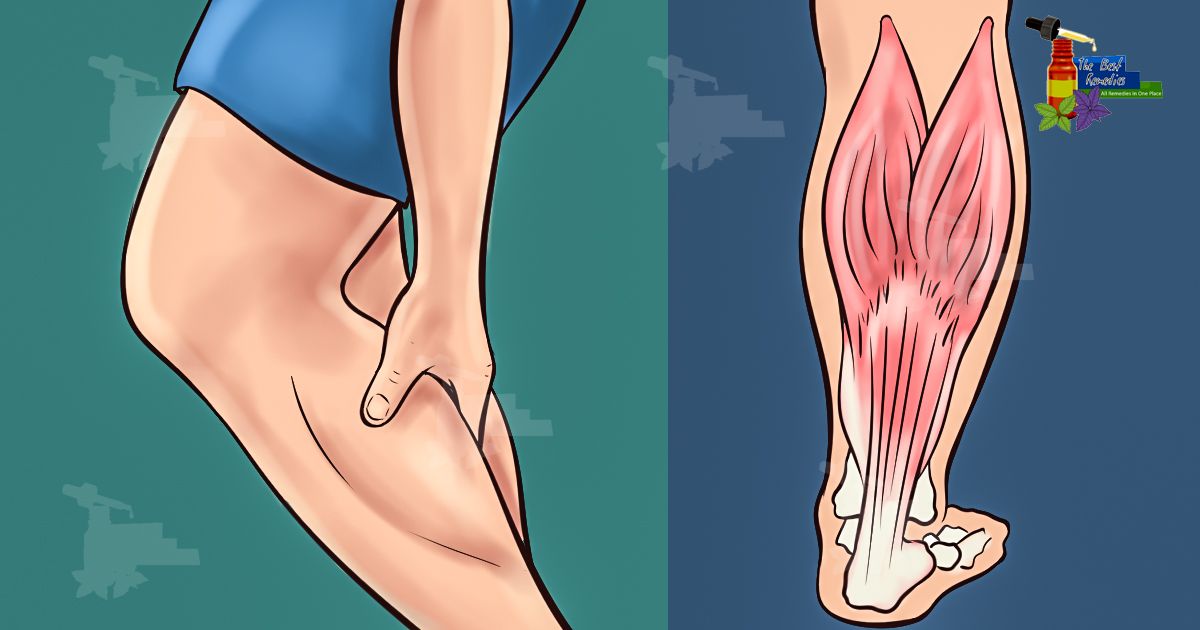 Dystonic seizures are not as common as true seizures.
Dystonic seizures are not as common as true seizures.
Other types of seizures
Some seizures are caused by a number of nerve and muscle disorders. For example, these are diseases such as amyotrophic lateral sclerosis (Lou Gehrig's disease), accompanied by muscle weakness and atrophy; radiculopathy in degenerative diseases of the spine (hernia, disc protrusion, osteophytes), when root compression is accompanied by pain, impaired sensitivity and sometimes convulsions. Seizures can also occur with peripheral nerve damage, such as diabetic neuropathy.
Crumpy . This type of cramps, as a rule, describes cramps in the calf muscle, and associate their appearance with muscle overstrain and the presence of degenerative changes in the spine (osteochondrosis of the lumbar spine, lumbar ischialgia). In addition, cramps are possible with disorders of the vascular circulation in the lower extremities (with obliterating endarteritis or post-thrombophlebitic syndrome). Also, various biochemical disorders in the triceps muscle of the leg can be the cause of cramps.
Also, various biochemical disorders in the triceps muscle of the leg can be the cause of cramps.
Many medicines can cause seizures. Strong diuretics such as furosemide or vigorous fluid removal from the body, even with less potent diuretics, can induce seizures as dehydration and sodium loss occur. At the same time, diuretics often cause loss of potassium, calcium and magnesium, which can also cause seizures.
Medicines such as donepezil (Aricept, which is used to treat Alzheimer's disease) and neostigmine (Prostigmine, used for myasthenia gravis), asraloxifene (Evista) is used to prevent osteoporosis in postmenopausal women - may cause seizures. Tolcapone (Tasmar), which is used to treat Parkinson's disease, has been shown to cause muscle cramps in at least 10% of patients. True seizures have been reported with nifedipine and the drugs Terbutaline (Brethine) and albuterol (Proventil, Ventolin). Some medicines used to lower cholesterol, such as lovastatin (Mevacor), can also cause seizures.
Seizures are sometimes observed in addicts during cessation of sedatives.
Lack of certain vitamins can also lead directly or indirectly to muscle cramps. These include deficiencies in thiamine (B1), pantothenic acid (B5), and pyridoxine (B6). The exact role of deficiency of these vitamins in causing seizures is unknown.
Poor circulation in the legs leads to a lack of oxygen in the muscle tissue and can cause severe muscle pain (intermittent claudication) that occurs when walking. It usually occurs in the calf muscles. But the pain in vascular disorders in such cases is not caused by the muscle cramp itself. This pain may be more related to the buildup of lactic acid and other chemicals in muscle tissue. Cramps in the calf muscles can also be associated with a violation of the outflow of blood in varicose veins and, as a rule, cramps in the calf muscles occur at night.
Symptoms and diagnosis of muscle cramps
Characteristically, a cramp is often quite painful. As a rule, the patient has to stop activities and urgently take measures to relieve seizures; the person is unable to use the affected muscle during the seizure. Severe cramps may be accompanied by soreness and swelling, which can sometimes persist for up to several days after the cramp has subsided. At the time of the cramp, the affected muscles will bulge, feel hard and tender to the touch.
As a rule, the patient has to stop activities and urgently take measures to relieve seizures; the person is unable to use the affected muscle during the seizure. Severe cramps may be accompanied by soreness and swelling, which can sometimes persist for up to several days after the cramp has subsided. At the time of the cramp, the affected muscles will bulge, feel hard and tender to the touch.
Diagnosis of seizures is usually not difficult, but finding out the causes may require both a thorough medical history and instrumental and laboratory examinations.
Treatment
Most seizures can be interrupted by stretching the muscle. For many leg and foot cramps, this stretch can often be achieved by standing up and walking. With cramps in the calf muscles, it is possible to bend the ankle with the help of the hand, while lying in bed with the leg extended straight. In writing spasm, pressing the hand against the wall with the fingers down will stretch the flexors of the fingers.
Gentle muscle massage can also be done to help relax a cramped muscle. If the cramp is associated with fluid loss, as is often the case with strenuous exercise, rehydration and restoration of electrolyte levels is necessary.
Muscle relaxants may be used in the short term in certain situations to allow muscles to relax during injury or other conditions (eg, radiculopathy). These drugs include cyclobenzaprine (Flexeril), orphenadrine (NORFLEX), and baclofen (Lioresal).
In recent years, injections of therapeutic doses of botulinum toxin (Botox) have been successfully used for certain dystonic muscle disorders that are localized to a limited muscle group. A good response may last several months or more, and injections may be repeated.
Treatment of seizures that are associated with specific diseases, usually focuses on the treatment of the underlying disease.
In cases where seizures are severe, frequent, prolonged, difficult to treat, or not associated with an obvious cause, then in such cases, both additional examination and more intensive treatment are required.
Prevention of seizures
Adequate nutrition with sufficient fluids and electrolytes is essential to prevent possible seizures, especially during strenuous exercise or during pregnancy.
Night cramps and other rest cramps can often be prevented with regular stretching exercises, especially if performed before bed.
Magnesium and calcium supplements are also a good way to prevent seizures, but caution is required when prescribing them in the presence of renal insufficiency. In the presence of hypovitaminosis, it is necessary to take vitamins of group B, vitamin D, E.
If the patient is taking diuretics, it is necessary to take potassium supplements.
Recently, the only drug that is widely used for the prevention, and sometimes for the treatment of seizures, is quinine. Quinine has been used for many years in the treatment of malaria. The action of quinine is due to a decrease in muscle excitability. However, quinine has a number of serious side effects that limit its use to all groups of patients (nausea, vomiting, headaches, heart rhythm disturbances, hearing impairment, etc.