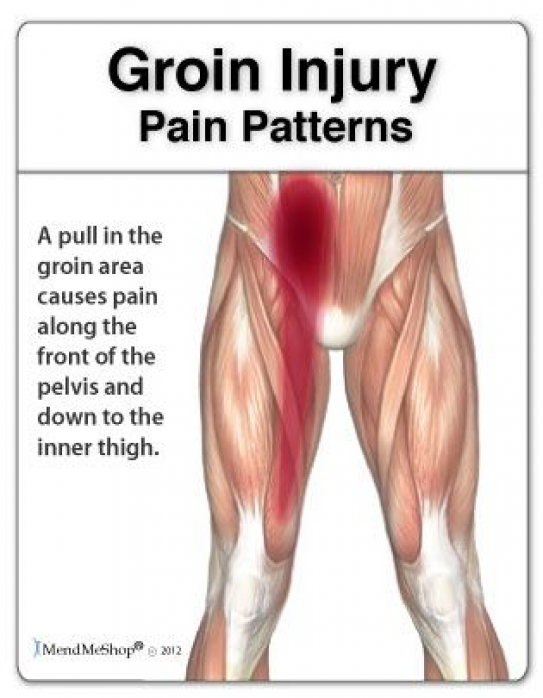
Pain in front of pelvis
18 Possible Causes of Pelvic Pain in Women
If you have pain below your belly button and above your legs, it counts as pelvic pain. It can be caused by a lot of things. It may be a harmless sign that you’re fertile, a digestive disorder, or a red flag that you need to go to the hospital.
If you have a sharp pain in the lower right part of your belly, are vomiting, and have a fever, it could be appendicitis. If you have these symptoms, go to the ER. An infected appendix may need surgery. If it bursts, it can spread the infection inside your body. This can cause serious complications.
Do you have belly pain, cramps, bloating, and diarrhea or constipation that keeps coming back? Talk to your doctor to figure out the problem. It could be IBS, sometimes called spastic colon. Doctors aren’t sure what causes it. Diet changes, stress management, and medications may help.
Ever feel a painful twinge between periods? You may be feeling your body ovulate. When you do, the ovary releases an egg along with some fluid and blood. It can cause irritation. This feeling is called mittelschmerz -- German for "middle" and "pain." That’s because it happens midway through your monthly cycle. The pain may switch sides from month to month. It isn't harmful and usually goes away in a few hours.
You can usually feel these cramps in your lower belly or back. They typically last 1 to 3 days. Why the pain? Every month, your uterus builds up a lining of tissue. That’s where an embryo can implant and grow. If you don't get pregnant, the lining breaks down and is shed during your period. When the uterus tightens to push it out, you get a cramp. Try a heating pad and over-the-counter pain relievers to ease pain. Exercise and de-stressing can help, too. You can also talk to your doctor about PMS pain. Certain birth control pills or antidepressants may help.
This happens when an embryo implants somewhere outside of the uterus and begins to grow. This usually happens in the fallopian tubes. Sharp pelvic pain or cramps (particularly on one side), vaginal bleeding, nausea, and dizziness are symptoms.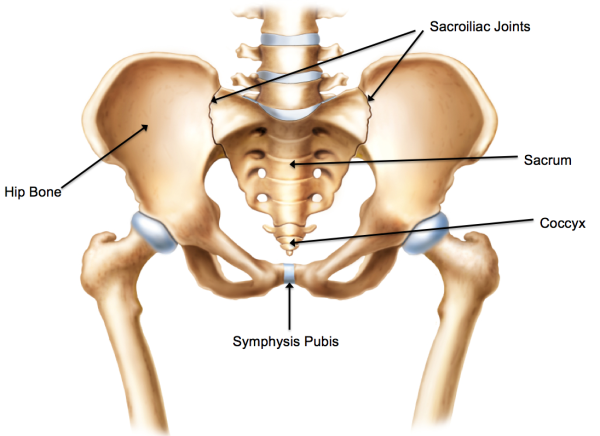 Get medical help right away. This is a life-threatening emergency.
Get medical help right away. This is a life-threatening emergency.
Pelvic pain is a warning sign of some STDs. Two of the most common are chlamydia and gonorrhea (shown here through a microscope). You often get both at the same time. They don't always cause symptoms. But when they do, you may have pain when you pee, bleeding between periods, and abnormal vaginal discharge. See your doctor. It’s also important to get partners checked and treated, too, so you don’t pass the infection back and forth.
This is a complication of sexually transmitted diseases. It's the No. 1 preventable cause of infertility in women. It can cause permanent damage to the uterus, ovaries, and fallopian tubes. Belly pain, fever, abnormal vaginal discharge, and pain during sex or urination can be symptoms. Get it treated right away to avoid damage. It is treated with antibiotics. In severe cases, you may need to be hospitalized. Get your partner treated, too.
Ovaries release eggs when you ovulate. Sometimes a follicle doesn't open to release the egg. Or it recloses after it does and swells with fluid. This causes an ovarian cyst. They’re usually harmless and go away on their own. But they may cause pelvic pain, pressure, swelling, and bloating. And if a cyst bursts or twists, it can cause sudden, severe pain, sending you to the emergency room. Doctors can spot them during a pelvic exam or ultrasound.
Sometimes a follicle doesn't open to release the egg. Or it recloses after it does and swells with fluid. This causes an ovarian cyst. They’re usually harmless and go away on their own. But they may cause pelvic pain, pressure, swelling, and bloating. And if a cyst bursts or twists, it can cause sudden, severe pain, sending you to the emergency room. Doctors can spot them during a pelvic exam or ultrasound.
These grow on or in the wall of the uterus. While they’re sometimes called fibroid tumors, they are not cancerous. Fibroids are common in women in their 30s and 40s. They usually don’t cause problems. But some women may have pressure in the belly, low back pain, heavy periods, painful sex, or trouble getting pregnant. Talk with your doctor if you need treatments to shrink or remove them.
In some women, there is tissue growing outside the uterus that is similar to tissue that lines the uterus. It can happen on the ovaries, fallopian tubes, bladder, intestines, and other parts of the body.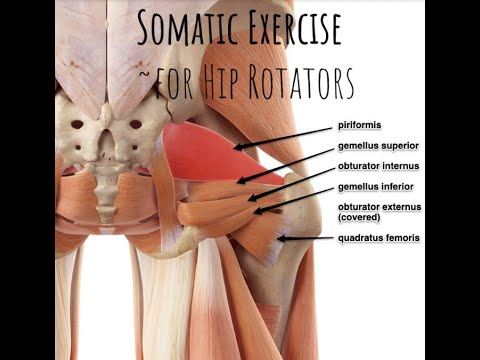 When it's time for your period, these clumps of tissue break down. But the tissue has no way to leave the body. While this is rarely dangerous, it can cause pain and form scar tissue that may make it tough to get pregnant. There are several treatment options. Pain medications, birth control pills, hormones to stop periods, surgery with small incisions, and even a hysterectomy (taking out your uterus) are options.
When it's time for your period, these clumps of tissue break down. But the tissue has no way to leave the body. While this is rarely dangerous, it can cause pain and form scar tissue that may make it tough to get pregnant. There are several treatment options. Pain medications, birth control pills, hormones to stop periods, surgery with small incisions, and even a hysterectomy (taking out your uterus) are options.
Do you have to pee often, or does it hurt when you do? Or do you feel like your bladder is full? It could be a UTI. This happens when germs get into your urinary tract. Treating it quickly can keep it from it getting serious. But if it spreads to the kidneys, it can cause serious damage. Signs of a kidney infection include fever, nausea, vomiting, and pain in one side of the lower back.
These are globs of salt and minerals that your body tries to get rid of in urine. They can be as tiny as a grain of sand or as large as a golf ball. And boy can they hurt! Your urine may turn pink or red from blood.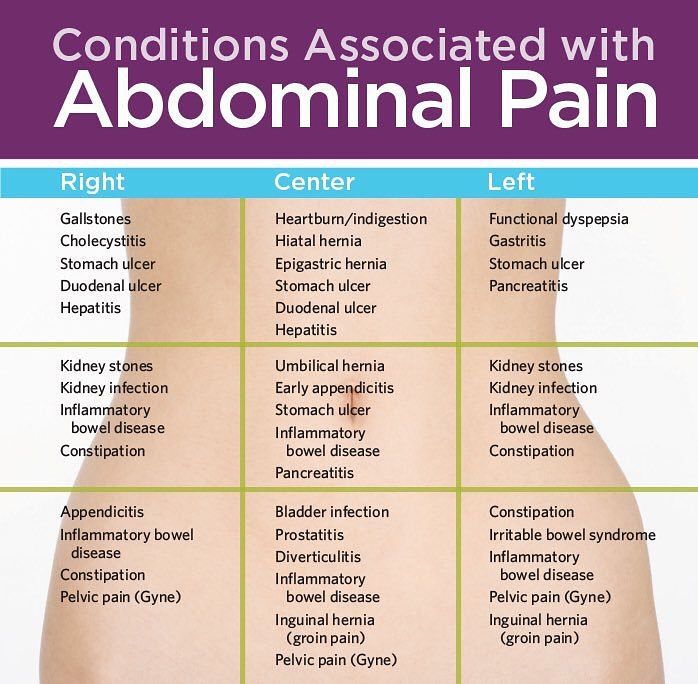 See your doctor if you think you have a kidney stone. Most will pass out of your system on their own, but some need treatment. Even if they can pass on their own, your doctor can help with pain medication and will tell you to drink lots of water.
See your doctor if you think you have a kidney stone. Most will pass out of your system on their own, but some need treatment. Even if they can pass on their own, your doctor can help with pain medication and will tell you to drink lots of water.
This condition causes ongoing pain and is related to inflammation of the bladder (illustrated here). It’s most common in women in their 30s and 40s. Doctors aren’t sure why it happens. People with severe IC may need to pee several times an hour. You might also feel pressure above the pubic area, pain when you urinate, and pain during sex. Although this can be a long-term condition, there are ways to ease the symptoms and avoid flares.
As you get older, this may happen. Your bladder or uterus drops into a lower position. It usually isn't a serious health problem, but it can be uncomfortable. You may feel pressure against the vaginal wall, or your lower belly may feel full. It may also give you an uncomfortable feeling in the groin or lower back and make sex hurt.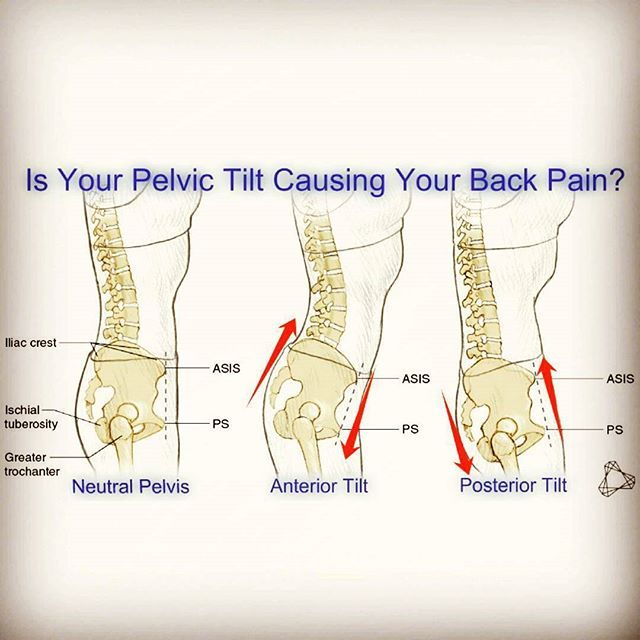 Special exercises like Kegel’s or surgery may help.
Special exercises like Kegel’s or surgery may help.
We’ve all seen varicose veins in legs. (This is a picture of one in the upper thigh.) They can sometimes happen in the pelvis, too. When blood backs up in veins, they become swollen and painful. This is known as pelvic congestion syndrome. This is a condition that's difficult to diagnose and treat. It tends to hurt worse when you sit or stand. Lying down may feel better. But because the best treatment is still unclear, you need to work with your doctor to learn what the options are and to find what works well for you.
If you've had surgery or an infection, you could have ongoing pain from this. Adhesions are a type of scar tissue inside your body. They form between organs or structures that aren’t meant to be connected. Adhesions in your belly can cause pain and other problems, depending on where they are. In some cases, you may need a procedure or surgery to get rid of them.
Does it hurt when you ride a bike or have sex? If it burns, stings, or throbs around the opening of your vagina, it could be this. The feelings can be ongoing or come and go. Before you’re diagnosed with this, your doctor will rule out other causes. This isn’t caused by an infection. Treatment options range from medication to physical therapy.
The feelings can be ongoing or come and go. Before you’re diagnosed with this, your doctor will rule out other causes. This isn’t caused by an infection. Treatment options range from medication to physical therapy.
This can be caused by many things. Most are treatable. It could be a vaginal infection, or you just may need more lubrication. The medical name is dyspareunia. Sometimes the pain gets better after sexual therapy. This type of talk therapy can focus on inner conflicts about sex or past abuse.
If you have pain that lasts at least 6 months, it’s considered chronic. It may be so bad it messes with your sleep, career, or relationships. See your doctor. Most of the conditions we've covered get better with treatment. Sometimes, even after a lot of testing, the cause of pelvic pain remains a mystery. But your doctor can still help you find ways to feel better.
Screening Tests Every Woman Needs
Medically Reviewed by Nayana Ambardekar, MD on November 02, 2021
Remember that old saying, "An ounce of prevention is worth a pound of cure"? Getting checked early can help you stop diseases like cancer, diabetes, and osteoporosis in the very beginning, when they’re easier to treat.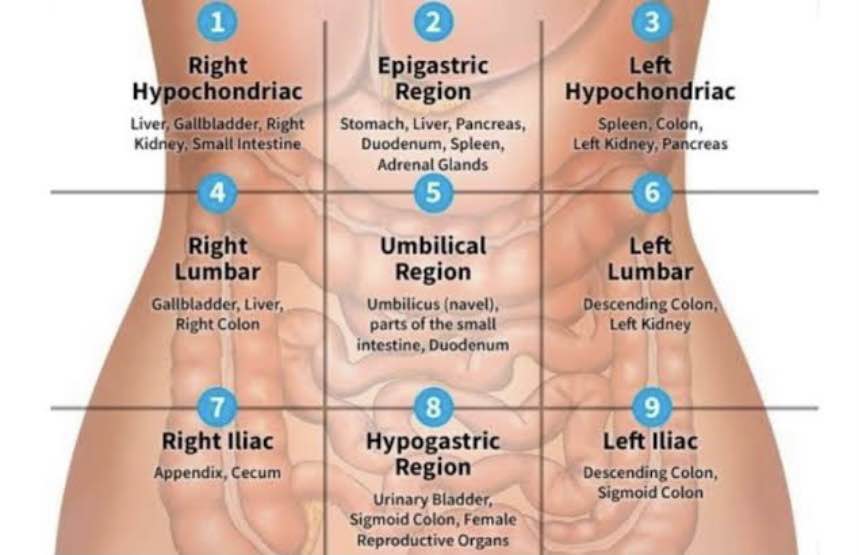 Screening tests can spot illnesses even before you have symptoms. Which screening tests you need depends on your age, family history, your own health history, and other risk factors.
Screening tests can spot illnesses even before you have symptoms. Which screening tests you need depends on your age, family history, your own health history, and other risk factors.
The earlier you find breast cancer, the better your chance of a cure. Small breast-cancers are less likely to spread to lymph nodes and vital organs like the lungs and brain. If you’re in your 20s or 30s, some experts recommend that your health care provider perform a breast exam as part of your regular check-up every one to three years. You may need more frequent screenings if you have any extra risk factors.
Mammograms are low-dose X-rays that can often find a lump before you ever feel it, though normal results don’t completely rule out cancer. Some experts recommend that while you’re in your 40s you should have a mammogram every year. Recommendations vary between 1 and 2 years for mammograms from your 50s through your 70s. Of course, your doctor may recommend more frequent screenings if you’re at higher risk.
Cervical cancer (pictured) is easy to prevent. The cervix is a narrow passageway between the uterus (where a baby grows) and the vagina (the birth canal). Your doctor may use Pap smears and or HPV testing to screen. Pap smears find abnormal cells on the cervix, which can be removed before they ever turn into cancer. The main cause of cervical cancer is the human papillomavirus (HPV), a type of STD.
During a Pap smear, your doctor scrapes some cells off your cervix and sends them to a lab for analysis. Your doctor will talk to you about whether you need a pap test alone or in combination with HPV testing. They will also talk to you about how often you need to be screened. If you're sexually active and at risk, you'll need vaginal testing for chlamydia and gonorrhea every year.
HPV vaccines can protect women under 26 from several strains of HPV. The vaccines don't protect against all the cancer-causing strains of HPV, however, and not all cervical cancers start with HPV. So routine cervical cancer screening is still important.
So routine cervical cancer screening is still important.
Osteoporosis is a state when a person’s bones are weak and fragile. After menopause, women start to lose more bone mass, but men get osteoporosis, too. The first symptom is often a painful break after even a minor fall, blow, or sudden twist. In Americans age 50 and over, the disease contributes to about half the breaks in women and 1 in 4 among men. Fortunately, you can prevent and treat osteoporosis.
A special type of X-ray called dual energy X-ray absorptiometry (DXA) can measure bone strength and find osteoporosis before breaks happen. It can also help predict the risk of future breaks. This screening is recommended for all women age 65 and above. If you have risk factors for osteoporosis, you may need to start sooner.
There are several kinds of skin cancer, and early treatment can be effective for them all. The most dangerous is melanoma (shown here), which affects the cells that produce a person’s skin coloring. Sometimes people have an inherited risk for this type of cancer, which may increase with overexposure to the sun. Basal cell and squamous cell are common non-melanoma skin cancers.
Sometimes people have an inherited risk for this type of cancer, which may increase with overexposure to the sun. Basal cell and squamous cell are common non-melanoma skin cancers.
Watch for any changes in your skin markings, including moles and freckles. Pay attention to changes in their shape, color, and size. Some experts recommend that you should also get your skin checked by a dermatologist or other health professional during your regular physicals.
As you get older, your risk of high blood pressure increases, especially if you are overweight or have certain bad health habits. High blood pressure can cause life-threatening heart attacks or strokes without any warning. So working with your doctor to control it can save your life. Lowering your blood pressure can also prevent long-term dangers like heart disease and kidney failure.
Blood pressure readings include two numbers. The first (systolic) is the pressure of your blood when your heart beats. The second (diastolic) is the pressure between beats.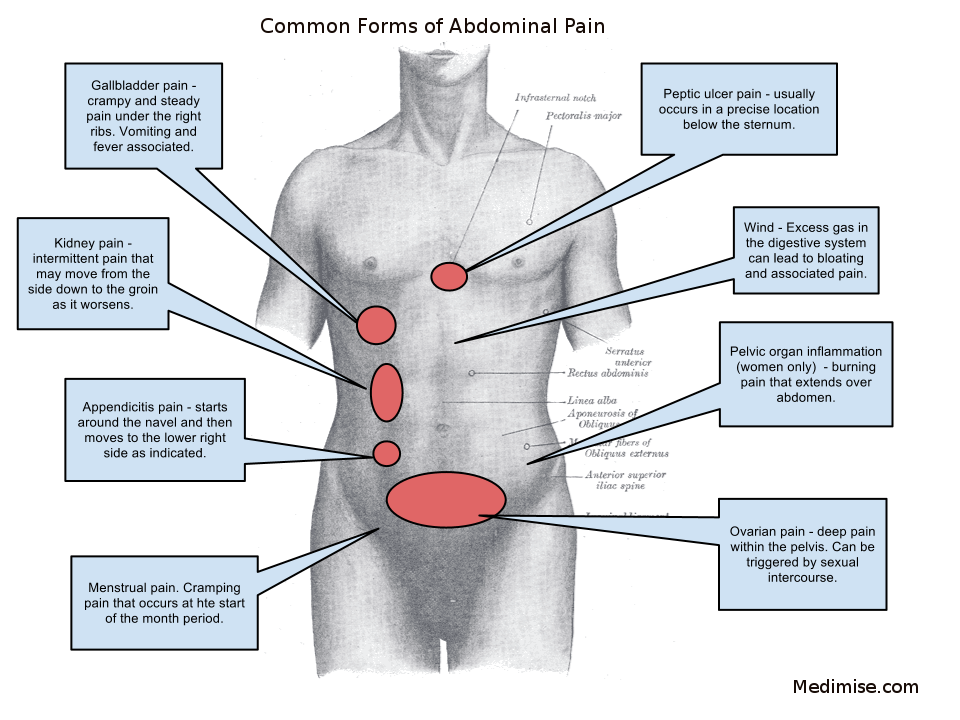 Normal adult blood pressure is less than 120/80. High blood pressure, also called hypertension, is 130/80 or above. In between is considered elevated, a sort of early warning stage. Ask your doctor how often to have your blood pressure checked.
Normal adult blood pressure is less than 120/80. High blood pressure, also called hypertension, is 130/80 or above. In between is considered elevated, a sort of early warning stage. Ask your doctor how often to have your blood pressure checked.
High cholesterol can cause plaque to clog your arteries (seen here in orange). Plaque can build up for many years without symptoms, eventually causing a heart attack or stroke. High blood pressure, diabetes, and smoking can all cause plaque to build up, too. It's a condition called hardening of the arteries or atherosclerosis. Lifestyle changes and medications can lower your risk.
To get your cholesterol checked, may need to fast for 9 to 12 hours. Then you’ll take a blood test that measures total cholesterol, LDL "bad" cholesterol, HDL "good" cholesterol, and triglycerides (blood fat). Your doctor will talk to you about when to start and how often to check your levels.
One-third of Americans with diabetes don’t know they have it.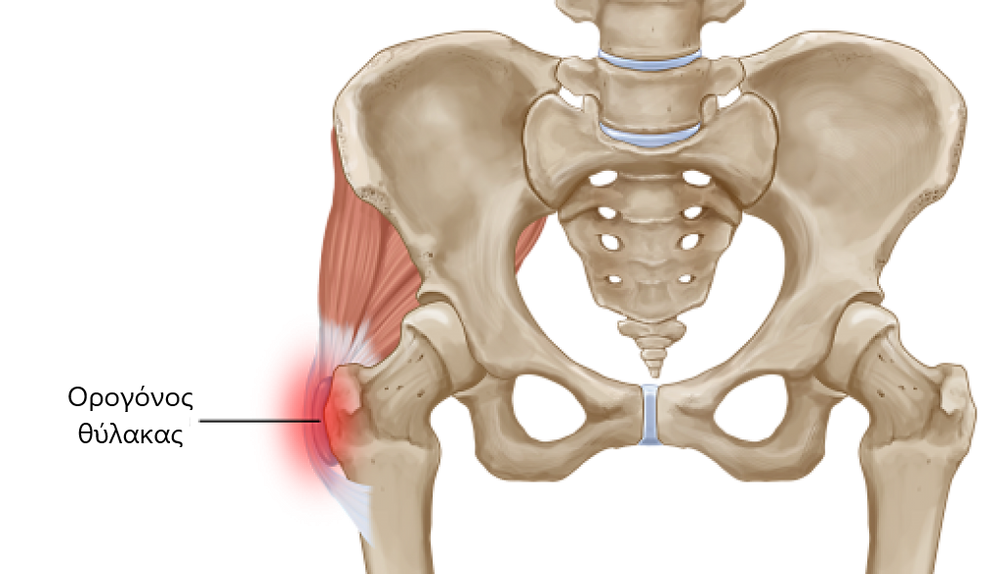 Diabetes can cause heart or kidney disease, stroke, blindness from damage to the blood vessels of the retina (shown here), and other serious problems. You can control diabetes with diet, exercise, weight loss, and medication, especially when you find it early. Type 2 diabetes is the most common form of the disease. Type 1 diabetes is usually diagnosed in children and young adults.
Diabetes can cause heart or kidney disease, stroke, blindness from damage to the blood vessels of the retina (shown here), and other serious problems. You can control diabetes with diet, exercise, weight loss, and medication, especially when you find it early. Type 2 diabetes is the most common form of the disease. Type 1 diabetes is usually diagnosed in children and young adults.
You’ll probably have to fast for eight hours or so before having your blood tested for diabetes. A blood sugar level of 100-125 may show prediabetes; 126 or higher may mean diabetes. Other tests include the A1C test and the oral glucose tolerance test. Your doctor will talk to you about when to start and how often to check your levels. Talk to your doctor about getting tested if you have a higher risk, like a family history of diabetes.
HIV is the virus that causes AIDS. It’s spread through sharing blood or body fluids with an infected person, such as through unprotected sex or dirty needles. Pregnant women with HIV can pass the infection to their babies.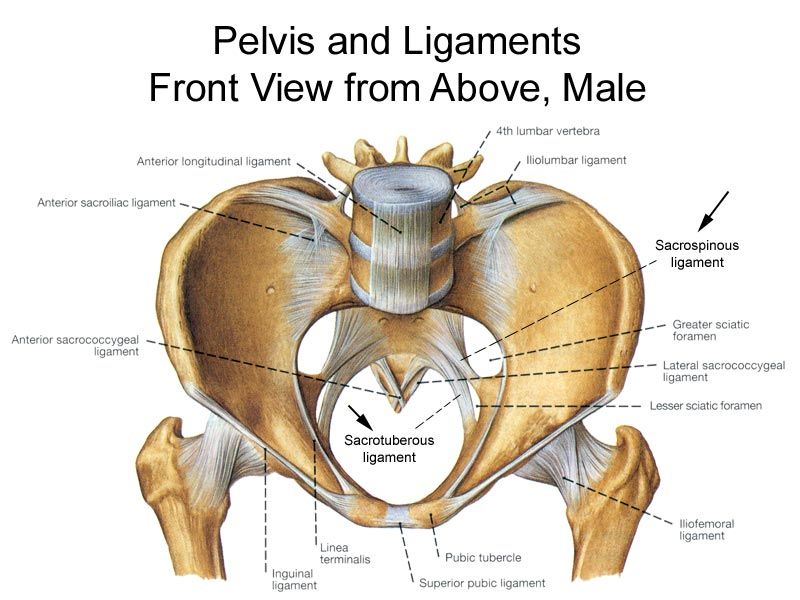 There is still no cure or vaccine, but early treatment with anti-HIV medications can help the immune system fight the virus.
There is still no cure or vaccine, but early treatment with anti-HIV medications can help the immune system fight the virus.
HIV can be symptom-free for many years. The only way to find out if you have the virus is with blood tests. The ELISA or EIA test looks for antibodies to HIV. If you get a positive result, you'll need a second test to confirm the results. Everyone who is at risk and sexually active should get tested. The USPSTF recommends that clinicians screen for HIV infection in adolescents and adults ages 15 to 65. Younger adolescents and older adults who are at increased risk should also be screened.
Most newly infected people test positive around two months after being exposed to the virus. But in rare cases it may take up to six months to develop HIV antibodies. Use a condom during sex to avoid getting or passing on HIV or other STDs. If you have HIV and are pregnant, talk with your doctor about reducing the risk to your unborn child.
Colorectal cancer is the second most common cause of cancer death after lung cancer. Most colon cancers come from polyps (abnormal masses) that grow on the inner lining of the large intestine. The polyps may or may not be cancerous. If they are, the cancer can spread to other parts of the body. Removing polyps early, before they become cancerous, can prevent it completely.
Most colon cancers come from polyps (abnormal masses) that grow on the inner lining of the large intestine. The polyps may or may not be cancerous. If they are, the cancer can spread to other parts of the body. Removing polyps early, before they become cancerous, can prevent it completely.
A colonoscopy is a common screening test for colorectal cancer. While you’re mildly sedated, a doctor inserts a small flexible tube equipped with a camera into your colon. If they find a polyp, they can often remove it right then. Another type of test is a flexible sigmoidoscopy, which looks into the lower part of the colon. If you’re at average risk, screening usually starts at age 45. Your doctor may also screen you with different kinds of take home stool cards.
Glaucoma happens when pressure builds up inside your eye. Without treatment, it can damage the optic nerve and cause blindness. Often, it produces no symptoms until your vision has already been damaged.
How often you should get your eyes checked depends on your age and risk factors.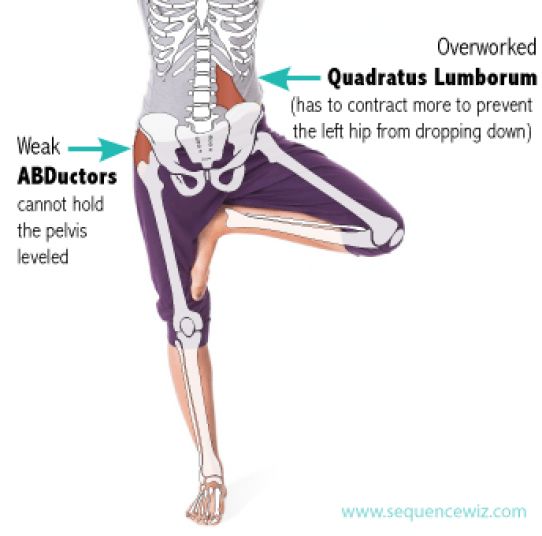 They include being African-American or Hispanic, being over 60, eye injury, steroid use, and a family history of glaucoma. Talk to your doctor about how often and when to start glaucoma screening.
They include being African-American or Hispanic, being over 60, eye injury, steroid use, and a family history of glaucoma. Talk to your doctor about how often and when to start glaucoma screening.
It's good health sense to talk with your doctor about screening tests. Some tests, such as a Pap test or breast exam, should be a routine part of every woman’s health care. Other tests might be necessary based on your risk factors. Proper screening won’t always prevent a disease, but it can often find a disease early enough to give you the best chance of overcoming it.
IMAGES PROVIDED BY:
1) Medioimages/Photodisc
2) Scott Camazine/Phototake
3) Creatas
4) Steve Gschmeissner/Photo Reasearchers, Inc.
5) Pulse Picture Library/CMP Images
6) BISP/Phototake
7) Dr. Tony Brian/Photo Researchers Inc.
8) Phanie/Photo Researchers Inc.
9) Dr. Kenneth Greer/Visuals Unlimited
10) Lauren Shear/Photo Researchers, Inc.
11) Steve Cole / the Agency Collection
12) Jose Luis Pelaez/Blend Images
13) Zephyr/Photo Researchers, Inc.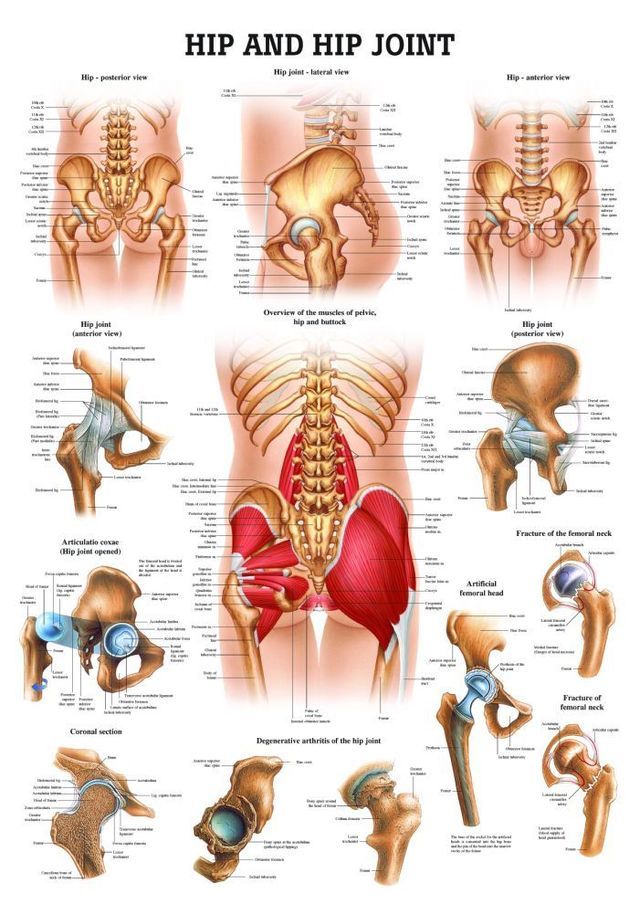
14) Lester Lefkowitz/Photographer's Choice
15) ISM/Phototake
16) Pulse Picture Library/CMP Images / Phototake
17) Dr. David R. Phillips/Visuals Unlimited
18) Southern Illinois University/ Photo Researchers, Inc.
19) Banana Stock
20) ISM/Phototake
21) BSIP/Phototake
22) ISM/Phototake
23) Thinkstock
24) ER Productions/Blend Images
SOURCES:
American Academy of Dermatology: "Skin cancer detection."
American Cancer Society web site.
American Diabetes Association web site.
American Diabetes Association: "Diabetes Statistics."
CDC: "Diabetes," "Understanding Mammograms," "Basic Information about HIV and AIDS," "HIV Testing Basics for Consumers."
Cowie, C. Diabetes Care, 2006.
FamilyDoctor.org: "Preventive Services for Healthy Living."
Glaucoma Research Foundation web site.
Healthfinder.gov: "Get Screened."
Lab Tests Online: "Screening Tests for Adults (Ages 30-49).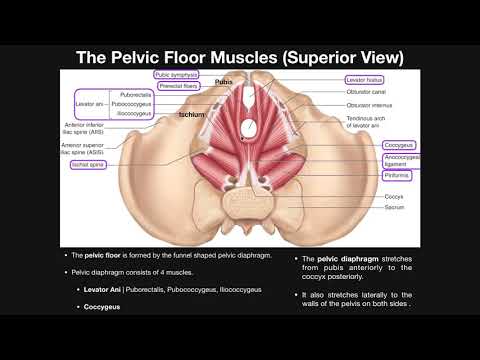 "
"
National Cancer Institute, Surveillance Epidemiology and End Results.
National Cancer Institute: "Human Papillomavirus (HPV) Vaccine."
National Cholesterol Education Program: "Detection, Evaluation, and Treatment of High Cholesterol in Adults (Adult Treatment Panel III)."
National Heart Lung and Blood Institute, National Institutes of Health: "High Blood Pressure," "What are High Blood Pressure and Prehypertension?"
National Osteoporosis Foundation: "Having a Bone Density Test," "Why Bone Health is Important."
The Biology Project (University of Arizona): "Introduction to ELISA Activity," "Introduction to Western Blot Activity."
U.S. Preventive Services Task Force: "Screening for Breast Cancer."
© 2021 WebMD, LLC. All rights reserved. View privacy policy and trust info
Pain in the pelvic area - causes, examination and treatment | Symptoms
Menstrual cramps
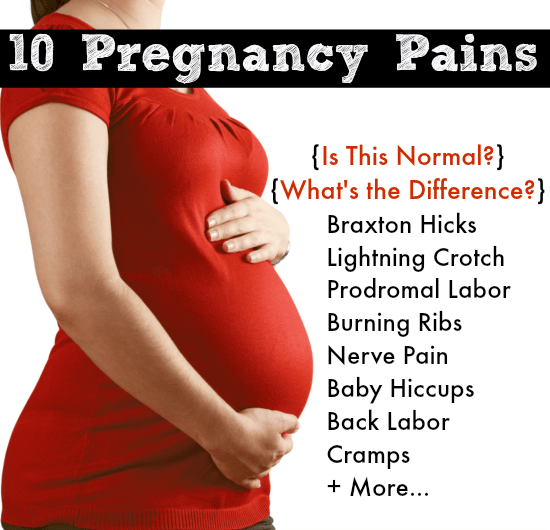
Symptoms: Sharp or crampy pains that begin a few days before or during menstruation, are most intense within about 24 hours after the onset of menstruation and subside after 2 to 3 days, often accompanied by headache, nausea, constipation, diarrhea, or frequent urination. urination.
urination.
Endometriosis
Signs: Sharp or crampy pain that occurs before and during the first days of menstruation, often pain during intercourse and / or bowel movements. It can eventually lead to pain that is not related to the menstrual cycle.
Pain in the middle of the menstrual cycle
Signs: Severe, sharp pain that starts suddenly; can occur on either side, but only on one side each time, occurs at the same time during the menstrual cycle, usually in the middle of the cycle between periods (when the egg is released), most intense at the beginning, but then decreases over 1-2 days, there is often slight bleeding. nine0006
Pelvic inflammatory disease
Signs: Aching pain in the pelvic area, which can be felt on one or both sides. Usually a vaginal discharge that is sometimes foul-smelling and can become pus-like and yellow-green in color as the infection progresses. Sometimes pain during urination and/or intercourse, fever or chills, nausea or vomiting.
Rupture of an ovarian cyst
Signs: Pain that starts suddenly is initially limited to one area in the lower abdomen. Sometimes dizziness, fainting, slight vaginal bleeding, nausea, or vomiting occur.
Ectopic pregnancy
Signs: Persistent (not spasmodic) pain that starts suddenly, is initially limited to one area in the lower abdomen. Often slight vaginal bleeding, sometimes dizziness, fainting, fast heartbeat, or dangerously low blood pressure (shock) caused by severe internal bleeding. nine0006
Sudden degeneration fibromas in uterus
Symptoms: Sudden pain. It is most common during the first 12 weeks of pregnancy, after childbirth or abortion. Vaginal bleeding may occur.
Torsion (twisting) of the ovarian adnexa
Signs: Severe pain that starts suddenly, occurs on one side, grows rapidly. As well as intermittent pain that comes and goes (when the ovary twists and unwinds). Often occurs in pregnant women, after the use of drugs for the treatment of infertility or with an increase in the ovaries. nine0006
Often occurs in pregnant women, after the use of drugs for the treatment of infertility or with an increase in the ovaries. nine0006
Ovarian cancer / Endometrial cancer
Signs: Gradually increasing pain. Brown or bloody discharge from the vagina. Abnormal vaginal bleeding (bleeding after menopause or bleeding between periods), sometimes weight loss.
Spikes
Signs: Pain in the pelvic area, which gradually increases, often becomes chronic. As well as pain during intercourse. No vaginal bleeding or discharge. Sometimes nausea and vomiting (suggesting intestinal blockage). In women who have had abdominal surgery or in women with a pelvic infection. nine0006
Miscarriage
Signs: Spasmodic pain in the pelvis or back, accompanied by vaginal bleeding. Other signs of early pregnancy such as breast tenderness, nausea, and missed periods.
Appendicitis
Signs: Pain that usually occurs in the lower right side of the abdomen. Loss of appetite and usually nausea and vomiting. Often fever. nine0006
Loss of appetite and usually nausea and vomiting. Often fever. nine0006
Bladder infection
Signs: Pain just above the pubic bone. Sometimes an urgent need to urinate, more frequent urination, or burning when urinating.
Diverticulitis
Signs: Pain or tenderness in the left lower abdomen, fever.
Inflammatory bowel disease (including Crohn's disease and ulcerative colitis)
Signs: Cramping pain in the abdomen, diarrhea, in ulcerative colitis often with blood in the stool, loss of appetite and weight loss. nine0006
Stones in the urinary tract
Signs: Excruciating intermittent pain in the lower abdomen, side or lower back, depending on the location of the stone, nausea and vomiting, blood in the urine.
Gastrointestinal disorders (gastroenteritis, constipation, accumulation of pus; colon cancer)
Musculoskeletal disorders (pubic bone dehiscence after childbirth, fibromyalgia and abdominal muscle tension)
Psychological factors (stress and depression)
Article "Chronic pelvic pain in women"
The problem of chronic pelvic pain in women of reproductive age occupies a special place in gynecology. Almost half of the patients who turn to the specialists of the EMC Department of Gynecology and Oncogynecology have complaints of chronic pelvic pain - discomfort for a long time in the lower abdomen, in the area below the navel. Long-term, despite the fact that conventional painkillers are ineffective, pelvic pain changes the psyche, the behavior of women, reduces the ability to work and quality of life. nine0006
Almost half of the patients who turn to the specialists of the EMC Department of Gynecology and Oncogynecology have complaints of chronic pelvic pain - discomfort for a long time in the lower abdomen, in the area below the navel. Long-term, despite the fact that conventional painkillers are ineffective, pelvic pain changes the psyche, the behavior of women, reduces the ability to work and quality of life. nine0006
Pain may be constant or intermittent, even paroxysmal, may be cyclical or not at all related to the menstrual cycle. Pain impulses arising in the genitals and surrounding tissues as a result of irritation of nerve endings are transmitted to the central nervous system, which in most women is accompanied by general weakness, irritability, anxiety, excitability, emotional lability, attention disorders, memory loss, sleep disturbances. nine0006
Chronic pelvic pain is characterized by:
-
persistent pain in the lower abdomen and lower back of varying intensity and nature (pulling, dull, burning, etc.
 ), prone to irradiation, lasting more than 6 months;
), prone to irradiation, lasting more than 6 months; -
periodic exacerbations - pain crises arising in connection with cooling, overwork, stress, etc.;
-
psycho-emotional disorders, manifested by insomnia, irritability, disability, anxiety and depression, decreased sexual function up to a complete lack of interest and sexual response; nine0006
-
no or little effect of conventional pain and antispasmodic therapy.
In some cases, it is not possible to identify its causes even with in-depth examination - this is the so-called "inexplicable" pain. For such patients, the “triangle” route - gynecologist-urologist-neurologist - becomes familiar, and pain and fear force them to turn to an oncologist. Often, for years, these patients have been treated for "inflammation of the uterus and appendages" with large doses of antibacterial drugs, and such irrational treatment aggravates the situation even more. nine0006
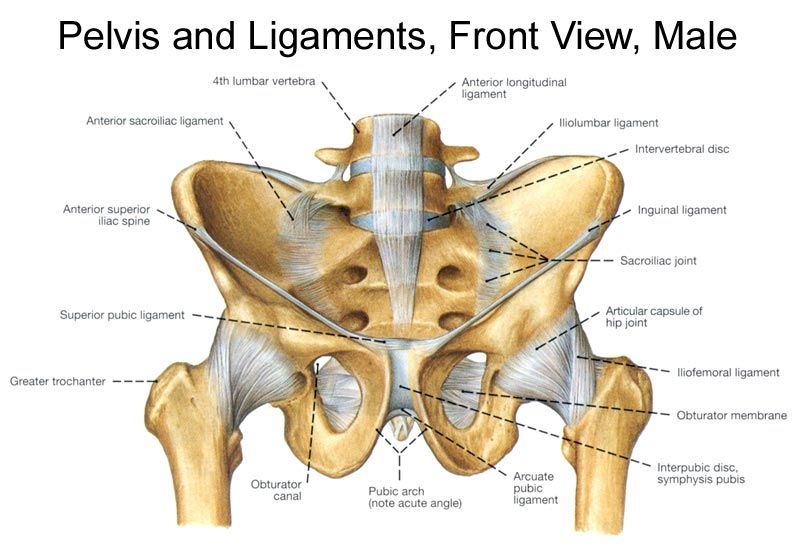
Pain is one of the most common symptoms in many gynecological diseases.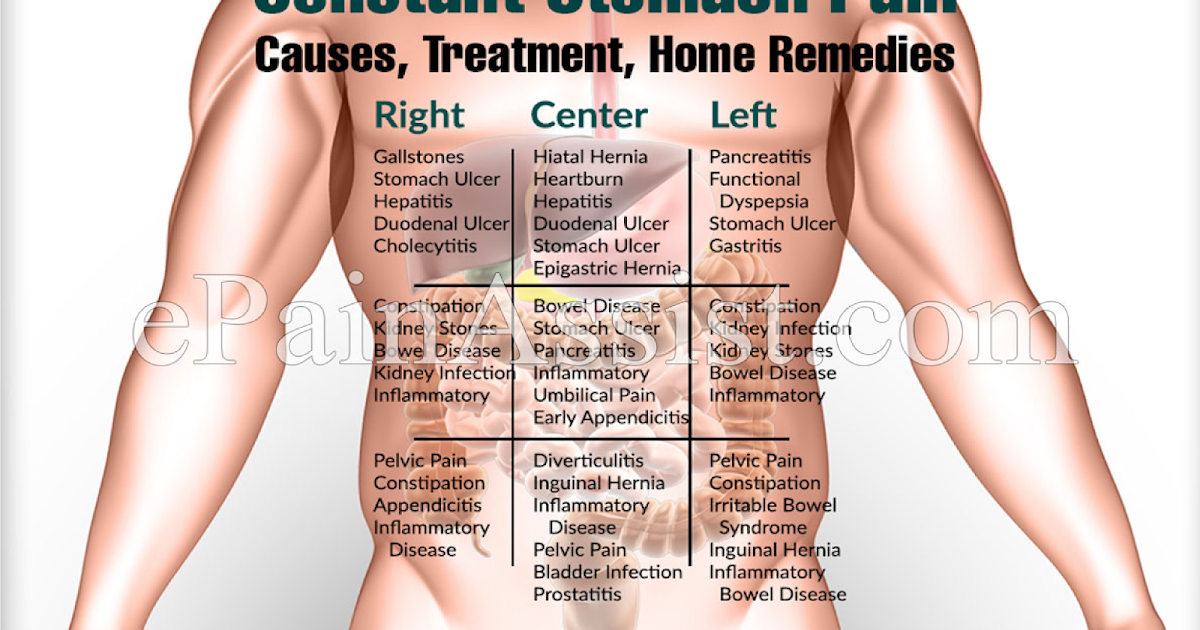 External genital endometriosis, adhesions in the pelvic cavity, chronic inflammatory diseases of the internal genital organs, internal endometriosis of the uterine body, Allen-Masters syndrome, genital tuberculosis, uterine fibroids, benign and malignant ovarian tumors, malignant neoplasms of the body and cervix, developmental anomalies genital organs with a violation of the outflow of menstrual blood - this is not a complete list of diseases and conditions that may be accompanied by chronic pelvic pain. nine0006
External genital endometriosis, adhesions in the pelvic cavity, chronic inflammatory diseases of the internal genital organs, internal endometriosis of the uterine body, Allen-Masters syndrome, genital tuberculosis, uterine fibroids, benign and malignant ovarian tumors, malignant neoplasms of the body and cervix, developmental anomalies genital organs with a violation of the outflow of menstrual blood - this is not a complete list of diseases and conditions that may be accompanied by chronic pelvic pain. nine0006
The most common misconceptions about chronic pelvic pain
Chronic pelvic pain in women can only be caused by gynecological diseases
coccygeal articulation, primary tumors of the pelvic bones, metastases to the pelvic bones and spine, bone forms of tuberculosis, pathology of the symphysis), retroperitoneal neoplasms, diseases of the peripheral nervous system (plexitis), diseases of the gastrointestinal tract (chronic colitis, irritable bowel syndrome, nonspecific ulcerative colitis, proctitis, adhesive disease), diseases of the urinary system (chronic cystitis, urolithiasis, pelvic location of the kidney, prolapse of the kidney), vascular disease (varicose veins of the small pelvis). The causes of chronic pain syndrome can also be mental illness (abdominal epileptic seizures, depressive syndrome, schizophrenia). nine0006
The causes of chronic pain syndrome can also be mental illness (abdominal epileptic seizures, depressive syndrome, schizophrenia). nine0006
Pain is usually caused by one factor, eliminating which, you can get rid of pain
In fact, in most gynecological diseases, the origin of pain is caused by several irritants at once, and it is often impossible to single out the leading factor. With uterine fibroids, pain can be caused by an increase in this organ, a violation of its blood supply and contractility of the uterine muscle, deformation of the uterine cavity by nodes, compression of the enlarged uterus or individual nodes of neighboring organs - the intestines, urinary tract, nerve plexuses, blood vessels. nine0006
In case of tumors and cysts of the ovaries, the tissues and ligaments of the ovaries are stretched (up to torsion), the maturation of the follicles is disturbed, micro-ruptures with inflammation and the formation of adhesions are possible, compression of neighboring organs by cysts
a functioning uterus with aplasia of the cervix or vagina, a rudimentary uterine horn, a closed cavity of a bicornuate or doubled uterus) and other conditions accompanied by a violation of the outflow of menstrual blood (intrauterine synechia, stenosis of the cervical canal or cicatricial changes in the vagina).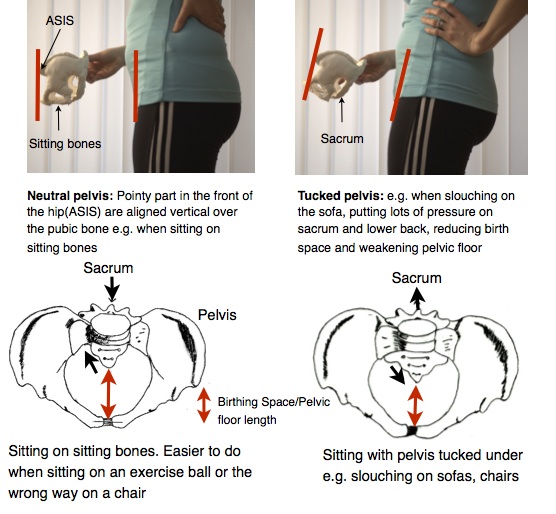 In these cases, the onset of pain is due to the expansion of closed cavities with blood and irritation of the peritoneum with almost constant hemoperitoneum, inflammation, and adhesions. Incorrect positions of the internal genital organs (bends of the uterus, prolapse, prolapse) also cause pelvic pain. nine0006
In these cases, the onset of pain is due to the expansion of closed cavities with blood and irritation of the peritoneum with almost constant hemoperitoneum, inflammation, and adhesions. Incorrect positions of the internal genital organs (bends of the uterus, prolapse, prolapse) also cause pelvic pain. nine0006
As a rule, most patients have a combined gynecological pathology, and each of the diseases can cause pain. External endometriosis often accompanies any other gynecological disease, and uterine fibroids are combined with internal endometriosis of the uterine body. Often there is a prolapse of the uterus, affected by fibroids or adenomyosis. The presence of a combined gynecological and extragenital pathology (hernias, diseases of the gastrointestinal tract, urinary tract, osteochondrosis of the spine) can significantly complicate the determination of the true cause of pain. nine0006
Periodic pain in women is normal
This myth has been around since the 19th century.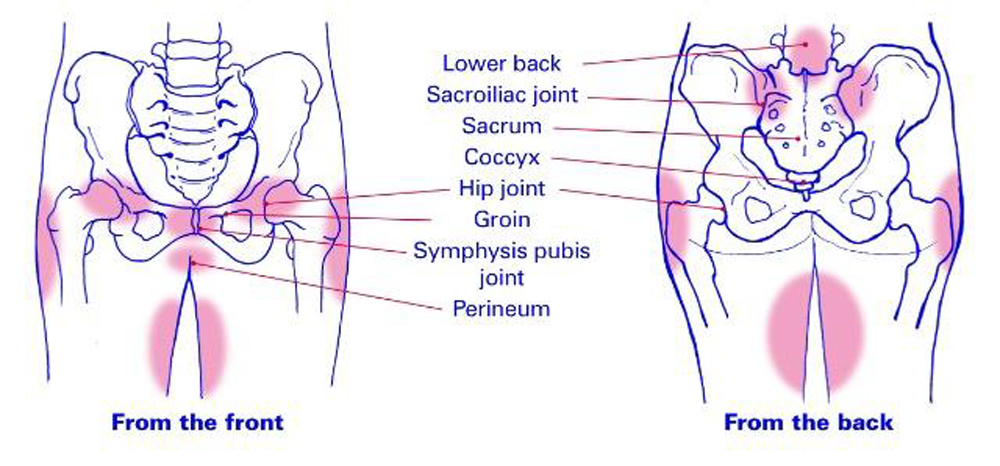 Doctors then explained menstrual pain by the instability and delicacy of the physiology of women and believed that pain during menstruation is the norm, which is very characteristic of the female body. Another "cause" of pain in women during menstruation is, according to some, a low pain threshold.
Doctors then explained menstrual pain by the instability and delicacy of the physiology of women and believed that pain during menstruation is the norm, which is very characteristic of the female body. Another "cause" of pain in women during menstruation is, according to some, a low pain threshold.
In fact, many women and girls experience pain during their periods. However, severe pain that disrupts the habitual lifestyle and level of activity cannot be the norm, and usually they are based on some kind of disease, for example, endometriosis, a hormone-dependent disease in which the lining of the uterus (endometrium) grows in other parts of the body. This is the third most common gynecological disease after uterine fibroids and various inflammatory processes in the genitals. nine0006
Therefore, every woman with severe pain during menstruation should be fully examined to determine their cause.
Early identification of the causes of pain determines the success of treatment. To establish the possible causes of pelvic pain, we work as a team with doctors of other specialties - general surgeons, oncologists, urologists, neurologists, psychologists.
To establish the possible causes of pelvic pain, we work as a team with doctors of other specialties - general surgeons, oncologists, urologists, neurologists, psychologists.
For the treatment of chronic pelvic pain, EMC gynecologists-surgeons use an approach based on reducing the invasiveness of surgical intervention, avoiding excessive radicalism, and expectant management in certain diseases of the genital area. nine0006
Laparoscopy and hysteroscopy provide us with unique diagnostic and therapeutic opportunities, which allow us to identify and eliminate possible causes of pain that are not diagnosed by other examination methods: endometriosis of the pelvic peritoneum, adhesions, anatomical disorders - hernia, peritoneal defects (Allen-Masters syndrome).
From the patient’s point of view, laparoscopic intervention, unlike laparotomy, is not perceived as a “big and difficult” operation, and the absence of intense and prolonged postoperative pain associated with the surgical wound of the anterior abdominal wall eliminates the aggravation of the initial pain due to layering on them operating rooms.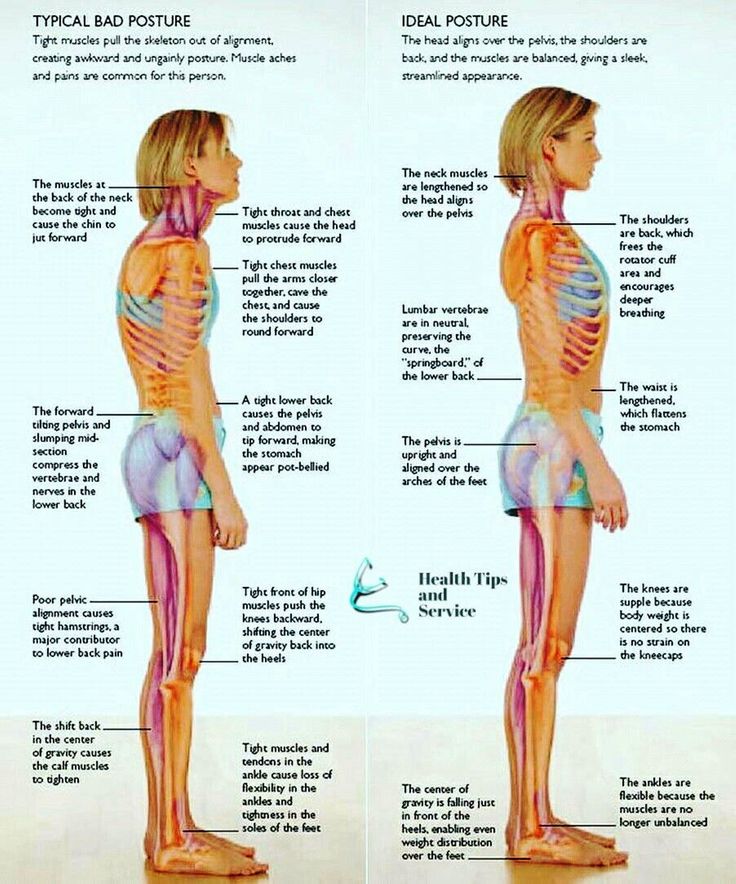 And, finally, early activation and return to physical activity, the almost absence of cosmetic defects also contribute to a quick recovery. nine0006
And, finally, early activation and return to physical activity, the almost absence of cosmetic defects also contribute to a quick recovery. nine0006
The volume of surgical intervention is chosen by EMC gynecologists depending on the age of the patient, her plans for childbearing, the severity of the detected pathology, the severity of pain. In young women, organ-preserving surgeries are performed, warning patients about the likelihood of recurrence of diseases such as endometriosis and uterine fibroids. Patients of older age groups with adenomyosis, multiple uterine fibroids, accompanied by severe pain, bleeding and leading to anemia, tumor growth and its significant size, dysfunction of neighboring organs, are shown radical operations in the volume of removal of the uterus, which we perform by laparoscopy or from a vaginal access . nine0006
In case of prolapse and prolapse of the pelvic organs, accompanied by pelvic pain, EMC gynecologists use surgical correction technologies that are fundamentally different from each other, depending on the age of the patient, to effectively eliminate gynecological pathology and restore the disturbed pelvic anatomy.