Pain in bladder after c section
What Can Cause Bladder Problems after a C-Section?
It was recently announced that c-sections have doubled since 2000 because of the fear of labour pain, sexual dysfunction and the fear of incontinence related to vaginal delivery.
It is common knowledge that women who have a natural childbirth have a higher chance of developing incontinence later in life, it has therefore become very common for pregnant women who have experienced leakage before childbirth to be concerned. Chair of FIGO’s Safe Motherhood Committee, asserted: “worldwide there is an alarming increase in caesarean section rates". However, experts are becoming more adamant that women should not choose this option just to avoid incontinence.”
Did you have a C-Section delivery? Post a question on our forum and share your experience.
Experts are worried that women are not aware of the potential complications of having a caesarean section and that glossing over the risks and side effects are common. Maternal death and disability rates are higher with c-sections and it is known to increase conditions such as asthma. Surprisingly, research has even shown that susceptibility of incontinence is genetic to some degree, and a substantial number of women who choose c-sections over natural birth do end up leaking.
Those who choose c-sections should remember that any kind of childbirth causes tears and strains on the body, and as researcher Goldberg explains: “things tend to equalize due to wear and tear and gravity”. As your baby grows in pregnancy, your uterus becomes heavier and your supporting structures are therefore become stretched and weakened. Hormones during pregnancy also contribute to the loosening of ligaments and muscles. A study in 2011 found that c-sections only drastically lower the risk of bladder problems if a woman delivers all of her children that way. This study found that 55% of women who had vaginal birth experienced incontinence, and 59% of women who had one vaginal birth and one caesarean had incontinence. Glazener explains, “unless women are resolved to have all their deliveries by the abdominal route, caesarean section doesn’t necessarily protect from incontinence”.
Glazener explains, “unless women are resolved to have all their deliveries by the abdominal route, caesarean section doesn’t necessarily protect from incontinence”.
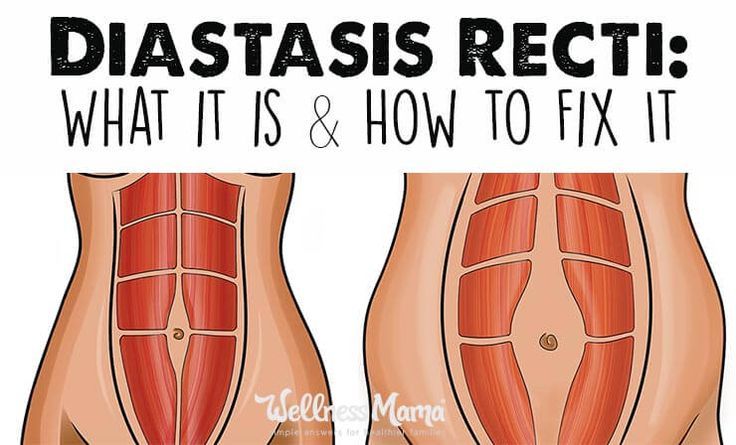
However, unique to c-sections is the scar. During a c-section an incision is made meaning a scar will form as part of the healing process. A temporary scab can form too close to the edges of the incision and as a result, the body creates scar tissue from collagen which can extend into deeper layers below the skin. These collagen fibres in scar tissue are formed in a single linear direction which can cause a variety of problems including bladder problems as the scar can attached to the front wall of your bladder causing urge incontinence and frequent urination. Physical therapist Kristen Maike explains “as everything shrinks back down after the birth, the scar begins tugging on the bladder. This makes it feel like you have to pee”. A 40 year old Doctor and mother, Ellen, is one of many women who experienced the side effects of a c-section scar.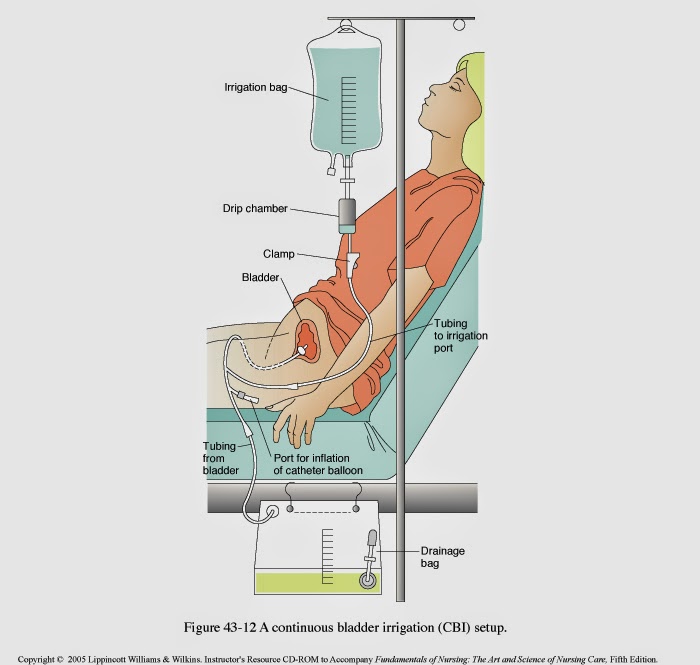 After the operation, her left leg was not responding well to the brain due to nerves being trapped – the scar was shutting off the muscles to her left leg and anterior pelvic muscles causing incontinence. Neurokinetic Therapy was used to reprogram her neurological system and restore muscular control and coordination. She was eventually able to regain leg movement and her incontinence cleared.
After the operation, her left leg was not responding well to the brain due to nerves being trapped – the scar was shutting off the muscles to her left leg and anterior pelvic muscles causing incontinence. Neurokinetic Therapy was used to reprogram her neurological system and restore muscular control and coordination. She was eventually able to regain leg movement and her incontinence cleared.
When is a C-Section Urgently Needed?
A C-Section consists of delivering the baby through a cut made in the abdomen and womb. It can be necessary for the following reasons:
- Your labour isn’t progressing as expected
- Your baby is in a bottom-down, or breech, position
- Your baby is in a sideways position or keeps changing position
- Yours or your baby’s health is at risk
- Your baby is too large for vaginal birth
- You have a serious medical condition, such as Diabetes or heart disease
- You are expecting twins
Who is More at Risk of Incontinence after a C-Section?
Women with gestational diabetes and women who smoke often are at risk of developing incontinence after a c-section. However, just like vaginal birth, it is not impossible for things to go wrong. One risk is damage to your bladder or to the tubes that connect the kidneys to the bladder during the incision. This often requires further incontinence surgery.
However, just like vaginal birth, it is not impossible for things to go wrong. One risk is damage to your bladder or to the tubes that connect the kidneys to the bladder during the incision. This often requires further incontinence surgery.
Are you currently pregnant and experiencing leaks? Read about managing incontinence during pregnancy.
Most women see improvements or completely cure their incontinence after a c-section with the help of pelvic floor exercises. Expert Maike asserts, “it’s worth checking with your Doctor or a pelvic floor physical therapist to ensure you are doing these exercises correctly”. You can read about how to do pelvic floor exercises here. Incontinence requires the ideal protective products to manage leaks. For light incontinence, we recommend small shaped pads and pull up pants. If your incontinence is heavy to severe, we recommend using pull ups, all in ones or large pads.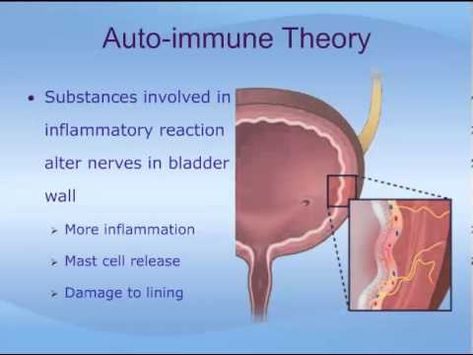 Here are some of our product recommendations:
Here are some of our product recommendations:
Ideal For: Moderate to Severe Incontinence
Prices Online:Incontinence Supermarket: £6.49 to £12.60 (Packs of 20, 22, 24, 26) Allanda: £6.49 to £12.59 (Packs of 20, 22, 24, 26)
TENA PantsIdeal For:
Moderate to Heavy Incontinence
Prices Online:Incontinence Supermarket: £4.89 to £13.95 (Packs of 8, 9, 10, 12, 14, 15, 18) Allanda: £7.20 to £13.95 (Packs of 8, 9, 10, 12, 14, 15, 18)
Attends Contours Ideal For:Light to Heavy Incontinence
Prices Online:Incontinence Supermarket: £6. 20 to £9.40 (Packs of 21, 28, 35, 42) Allanda: £6.20 to £9.40 (Packs of 21, 28, 35, 42)
20 to £9.40 (Packs of 21, 28, 35, 42) Allanda: £6.20 to £9.40 (Packs of 21, 28, 35, 42)
I Couldn't Pee and Other Things I Didn't Expect After My C-Section
The actual surgical recovery was a cinch, but there were some super uncomfortable side effects I definitely hadn’t prepared for.
I had a scheduled cesarean section (aka C-section) at 38 weeks due to a pesky placenta situation. I was, of course, nervous for my first time in the operating room — and for major abdominal surgery, at that.
I was also anxious to meet my baby and see for myself — in real life and not on an ultrasound monitor — that he was just right.
Despite my fears, the surgery was a cinch. My placenta previa thankfully didn’t pose a problem during the delivery, and today the evidence of my incision is barely there.
And, as for my little boy, well, his 10 little fingers and toes are just delicious.
So aside from the mesh undies and post-op scar creams that other moms are always suggesting, I thought I was in the clear.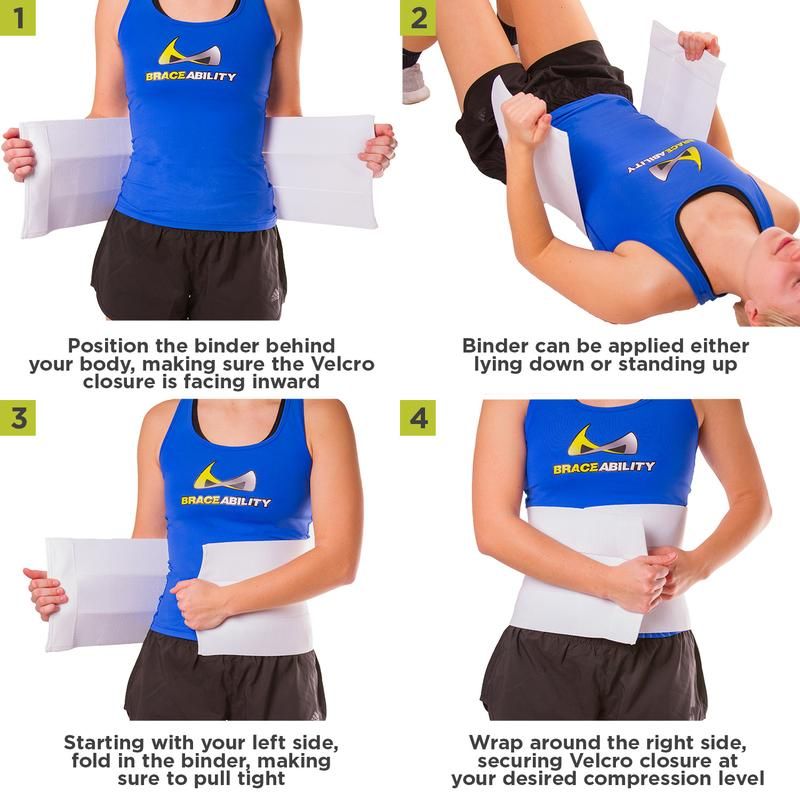 Right? Wrong.
Right? Wrong.
Yes, the actual surgical recovery was quick: I was walking around as soon as those horrid compression devices were stripped from my legs, and I was bounding up and down my stairs practically the moment I arrived home with my son — with only some Tylenol and Motrin to keep the occasional pain at bay. (Talk about stubborn new mom adrenaline!)
But there was C-section aftermath — super intense, although certainly not life-threatening, side effects — that I never fully expected. And they are, in fact, much more common than I thought.
I was warned about some post-op swelling, but I came home from the hospital larger — much larger — than I was during my entire pregnancy.
I felt like I looked roughly 20 months pregnant while already holding my newborn in my arms. I envisioned being able to easily button the cute pajamas I brought to the hospital, but instead I could barely tell where my legs ended and feet began.
Oh, and finding shoes to mash my feet into for my son’s bris 8 days after delivery caused a proper meltdown.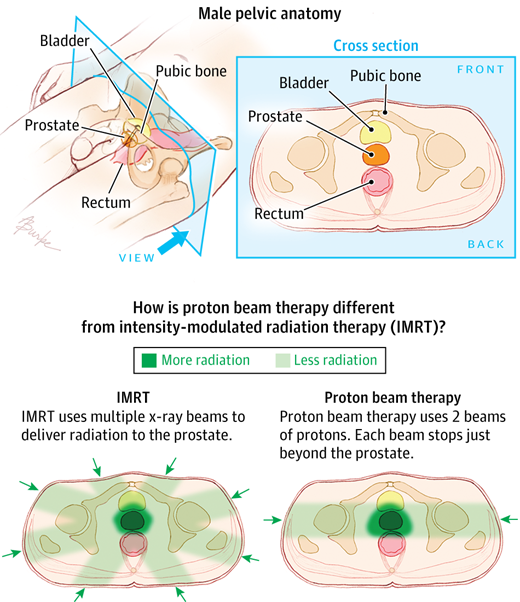 (Hello, hormones!)
(Hello, hormones!)
Anita Saha, MD, FACOG, notes that what I experienced is called postpartum edema — otherwise known as “the unspoken aftermath.” And, yes, to me it was just as jarring as it sounds, although apparently not uncommon.
“The cause of postpartum edema is directly related to what your body is programmed to do normally during a pregnancy,” explains Saha, a New Jersey-based obstetrician/gynecologist. “By the beginning of the third trimester, your blood has increased its plasma volume, without increasing red blood cells.”
That, she says, coupled with the dilution of albumin (a protein that keeps water in our veins) and the dilation of our veins themselves to increase blood flow to the placenta, causes swelling — especially in the feet, ankles, and legs, which due to gravity, have trouble getting blood back to the heart. These veins, she says, become “leaky.”
I wasn’t too swollen when I arrived at the hospital, but once I delivered, it really was like the weight in my abdomen dispersed throughout my body.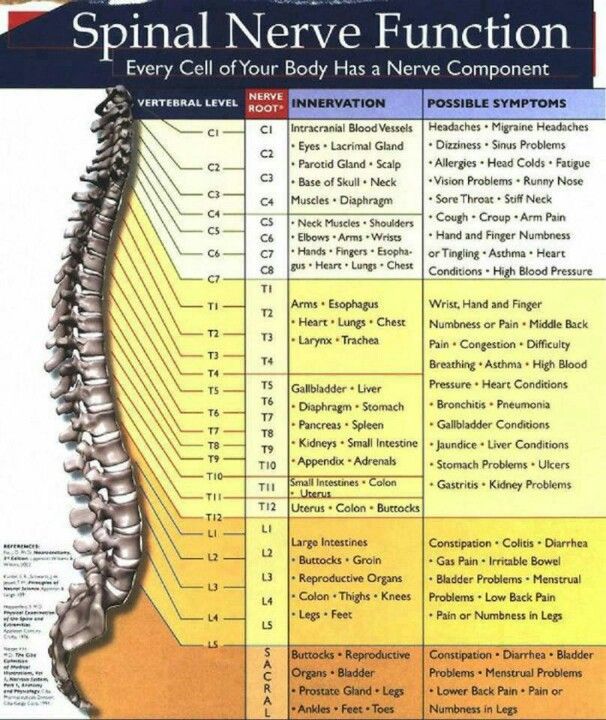 That’s because, says Saha, all that extra blood in my uterus (that was once pressing down on the inferior vena cava and the veins in the pelvis) did actually spread into circulation and into those “leaky” veins… hence even more swelling.
That’s because, says Saha, all that extra blood in my uterus (that was once pressing down on the inferior vena cava and the veins in the pelvis) did actually spread into circulation and into those “leaky” veins… hence even more swelling.
Saha notes that while the aftermath can affect all types of deliveries, people who have C-sections sometimes experience more immediate swelling because they receive more IV fluids during the process. Lucky us!
While it seemed like an eternity, Saha says edema usually resolves in 7 to 10 days. When it finally did, it was like a literal weight was lifted.
As soon as I was given the go-ahead, I asked to have the Foley catheter that was inserted into my bladder before my C-section removed so I could move around and get my blood flowing.
I did, but my bladder apparently didn’t realize that it was supposed to work on its own.
Many hours and numerous trips to the bathroom later, I still couldn’t pee. Only after two attempts to reinsert the catheter (holy smokes was this painful), did my body kick into gear.
While I originally thought my extreme swelling was the culprit, Saha says this is usually due to the epidural or spinal anesthesia — which causes a relaxation in the bladder muscle and therefore an increase in bladder capacity.
Post-epidural urinary retention is the official term for this common post-delivery side effect.
This can occur despite having a Foley catheter inserted to help with constant drainage during a C-section and post-op. As Saha explains it, hospitals have protocols about when the catheter can be removed, usually after 12 to 24 hours.
But as she points out, “Despite protocols, individuals metabolize and clear the anesthesia in their body at a different pace. That means that some patients will have urinary retention because they are still experiencing the effects of the opioid medications in the epidural and/or spinal.”
It’s important to note, Saha says, that proper emptying of the bladder doesn’t mean dribbling or small amounts of frequent urination. Reaching this milestone means having a normal flow — and more communication with patients is needed to address this so they don’t have a problem later.
Reaching this milestone means having a normal flow — and more communication with patients is needed to address this so they don’t have a problem later.
(Pooping is a whole other story that many new moms can tell. Are you worried your stitches will pop? Yes, yes you are.)
Perhaps I wasn’t sure if my abdomen even hurt after the surgery because the day I got home — so a little more than 72 hours post-op — I began developing a horribly painful and itchy rash across my midsection.
Which suddenly appeared on my lower back. And my upper thighs. Seemingly anywhere the surgical antiseptic (in my case, chlorhexidine) was applied.
And it lasted for more than a week.
I was literally walking around with ice packs secured by my underwear band to relieve the itchiness and additional swelling.
While I thought my case was an anomaly, Saha notes that chlorhexidine allergy isn’t rare.
“I also see allergies in the exact distribution of the adhesive tape that is on the surgical drape, so it looks like a band at the level of the belly button going around the sides. Some people also have allergies where the adhesive is on the inner thigh for the Foley catheter,” she explains.
Some people also have allergies where the adhesive is on the inner thigh for the Foley catheter,” she explains.
“Unfortunately, it is impossible to predict who will develop an allergy when using a substance for the first time,” she adds.
I was reluctant to take anything for the discomfort because, well, I was a nervous new breastfeeding mom.
Saha advises topical hydrocortisone or Benadryl lotion for the reaction, but to avoid oral antihistamines and cold medications because they may drop your milk supply — which may not just naturally appear when your baby does.
Yep, I will write that again: Your milk supply might not just naturally appear when your baby does.
I was able to physically breastfeed my baby as soon as I was given the post-surgical green light. And he was a natural. He had a good latch. We got into a proper position. And he was getting all the good stuff colostrum provides.
But that was all he was getting, and I had to pump, pump, pump (starting on day 3 of my hospital stay) to make my actual milk come in.
It was exhausting and upsetting — and I felt guilty, like I was failing at the first task that I wanted to accomplish as a mom.
Finally, after several days of nonstop pumping and feeding (and a few bottles of supplemental formula later, thanks to our pediatrician’s guidance), our exclusive breastfeeding relationship began — and pretty much lasted that way for roughly 10 months.
Clearly, I was not alone.
“This is, unfortunately, the most common problem for all patients after delivery,” notes Saha. “It can take up to 5 days for the transitional milk — the white appearing milk — to come in after any delivery.”
And it’s the hardest for moms who’ve had a planned C-section. Why? “With vaginal delivery, natural oxytocin is released during the labor process that triggers the breasts to start the milk production process — in conjunction with the hormone prolactin,” explains Saha.
“It is true that the separation of the placenta from the uterus does cause hormonal shifts that transition your body into milk production mode, but it is also well known that this transition happens slower after a first time C-section,” she says.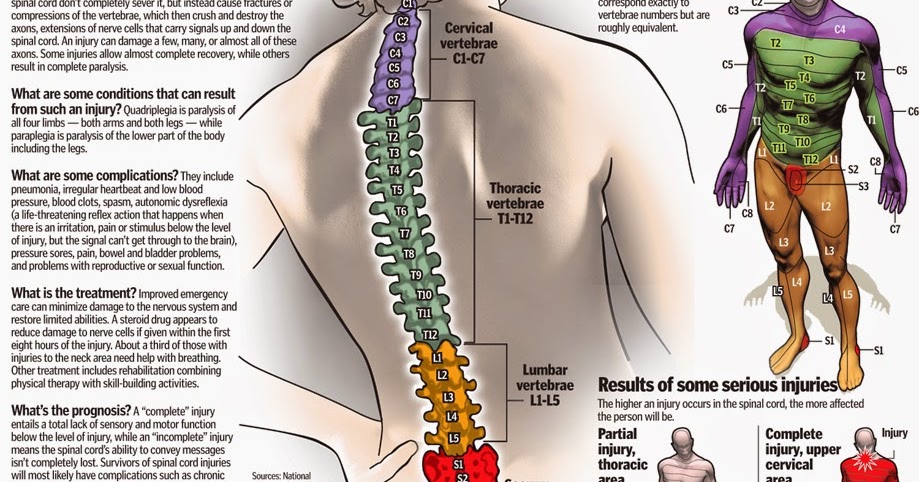
“With a planned C-section, there is no preceding labor. These patients have the hardest time getting their breast milk to come in typically,” Saha explains.
Of course, there may be other post-op factors at work, and lactation consultants should be on hand to help patients — and not just with the technical aspects of breastfeeding. They should also make sure that new moms know that they’re not alone, that fed is ultimately best, and that supplementing with formula until one’s milk comes in (even if the goal is to exclusively breastfeed when it does) is just fine.
And new moms shouldn’t feel guilty like I did.
But, then again, bouts of mom guilt — as well as learning to roll with the punches starting at that miraculous moment you’re given your new baby to hold — is kind of like an initiation into motherhood.
Barbara Kimberly Seigel is a New York City-based editor and writer who has explored everything — from wellness and health to parenting, politics, and pop culture — through her words. She’s currently living the freelance life as she tackles her most rewarding role yet — mom. Visit her website.
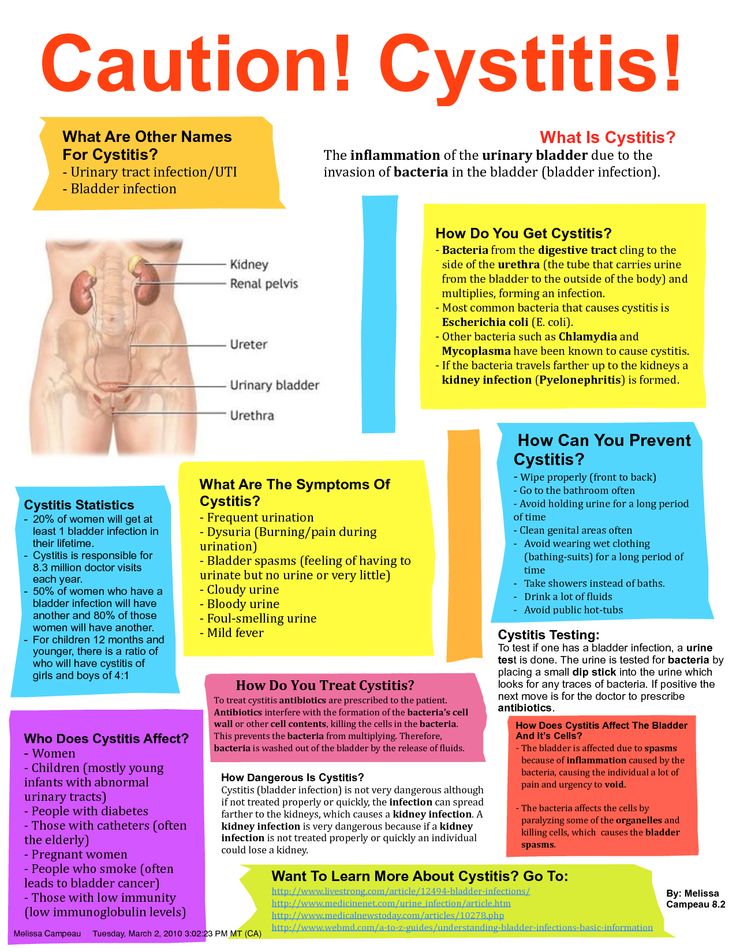
Postpartum cystitis ⛑ Symptoms, diagnosis and treatment of postpartum cystitis
Inflammation of the bladder shortly after childbirth - postpartum cystitis - is relatively rare in the era of antibiotics. Statistics state that only 1 to 4% of puerperas 1 are at risk of experiencing it. And, as a rule, all such patients had manifestations of the disease even before pregnancy.
That is, childbirth exacerbates an existing bladder infection. Therefore, it makes sense for women to take care of their health in advance, before conception. nine0005
The complex phytopreparation Canephron ® N will help with this. The product produced using the phytoneering technology has a strictly dosed composition of each tablet or drop, and has proven effectiveness against acute and chronic cystitis 2, 3 .
A prophylactic course of treatment at the planning stage of pregnancy will help maintain the health of the urinary system during pregnancy. And it can save you from having to take anti-cystitis medications in the postpartum period when you need to breastfeed your baby. nine0005
Symptoms and signs of cystitis after childbirth
Symptoms of cystitis after childbirth are not much different from the classical clinical picture.
During the first 2 weeks after childbirth, puerperas begin to worry about:
- discomfort and pain in the bladder area, in the lower abdomen;
- irresistible desire to jog a little every 30-60 minutes;
- portions of urine are meager, the feeling of emptying the bladder does not come for long; nine0023 in the process of urination, pain, burning are noted.
Temperature may remain unchanged, but fever is also possible.
In general, the severity of manifestations is determined by the type of disease. Subacute proceeds more easily, gangrenous - acutely, with fever and a critical deterioration in the general condition 4 .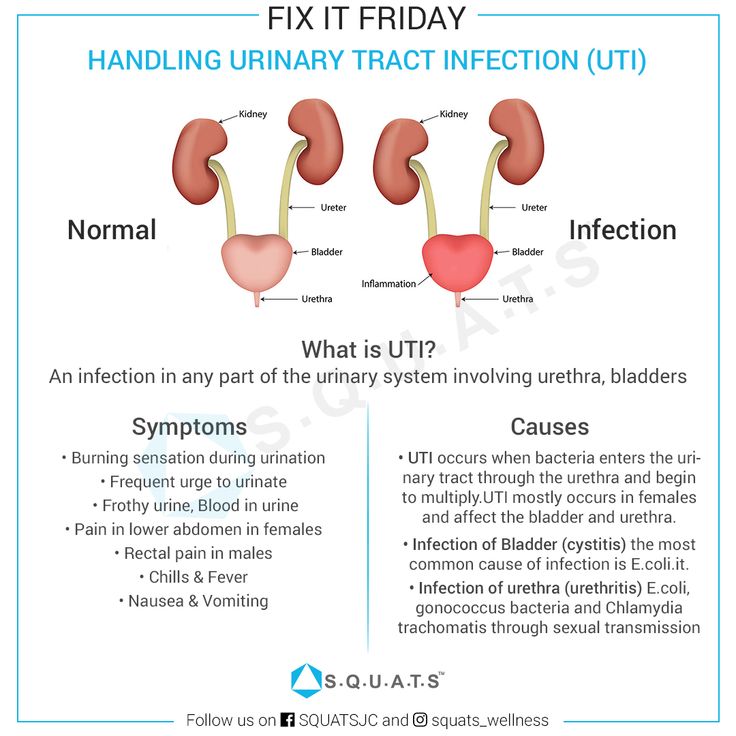
Approximately 40% of patients will have mild disease and will not require antibiotic therapy 5 . If cystitis causes serious inconvenience and spoils the quality of life, you can turn to herbal medicine. nine0005
Canephron ® N drops or tablets contain a complex of active ingredients of plant origin that have anti-inflammatory, antispasmodic and antibacterial effects in urinary bladder infections 6 . And, if necessary, can be used during lactation 7 .
Causes of puerperal cystitis
The main cause of puerperal cystitis is an inadequately treated bladder infection before pregnancy. The peculiarity is that infection can take place long before conception:
- neglect of hygiene procedures;
- frequent unprotected intimacy with a risk of contracting sexually transmitted infections;
- life in asocial conditions, when a woman simply neglects hygiene and prevention of urinary infections.
Secondary reason: during childbirth through the birth canal, the baby changes the anatomical parameters of the pelvic organs, including the bladder. Such changes weaken the immune system of the body and contribute to the activation of the infection. nine0005
Often the causative agent is Escherichia coli - a bacterium that enters the bladder from the vagina during vaginosis and as a result of neglect of sexual hygiene.
The problem is that E. coli is often resistant to antibiotics, deeply embedded in the lining of the bladder. And therefore, even before pregnancy, such cystitis is difficult to treat with chemotherapy drugs. In addition, viruses can be the causative agent.
Against this background, bioflavonoids, alkaloids and phenolcarboxylic acids of the components of Canephron 9 give the best effect0003 ® H 6 .
Postpartum cystitis treatment
Treatment of any infection in a woman who has just given birth is a complex medical problem. For each sick woman in childbirth, a decision is made individually, so you need to consult a doctor.
The traditional approach to treating cystitis after childbirth involves the use of antibiotics. In order to kill pathogenic bacteria and not harm the baby, women stop breastfeeding for the duration of treatment. nine0005
It is rational to do a urine culture before prescribing drugs and check to which drugs the bacteria-causative agents of the process have retained sensitivity 8 .
With extended resistance of microbes, it is advisable to add Canephron ® N to the treatment regimen, because it actively works even with antibiotic resistance. Drops and tablets Canephron ® N are produced using phytoneering technology - strict quality control from the stage of seed selection to the preparation of dosage forms. nine0005
The active components of the three medicinal plants themselves have a marked antibacterial effect. Plus, make bacteria more susceptible to antibiotics 9 . It is important to note that the antibacterial effect of Kanefron ® N is primarily associated not with the aggressive action of the drug against microorganisms, but with the suppression of the ability of Escherichia coli to attach to the bladder epithelium. For this reason Canephron ® N, unlike antibiotics, is safe for beneficial intestinal microflora. nine0005
It is important to note that the antibacterial effect of Kanefron ® N is primarily associated not with the aggressive action of the drug against microorganisms, but with the suppression of the ability of Escherichia coli to attach to the bladder epithelium. For this reason Canephron ® N, unlike antibiotics, is safe for beneficial intestinal microflora. nine0005
At the end of treatment for cystitis, the woman can resume breastfeeding.
Prevention of cystitis after childbirth
Preventing the development of postpartum cystitis is easy and difficult at the same time.
On the one hand, it is enough to protect yourself from genitourinary infections, not to infect the membrane of the bladder before pregnancy and childbirth. Use condoms, lube. But it is very rare to maintain the sterility of the urinary tract.
On the other hand, if the infection nevertheless took place, then it is not always possible to completely get rid of pathogens. Even in the absence of symptoms of cystitis, many women have asymptomatic bacteriuria - the excretion of microbes in the urine. Therefore, at the stage of observation in the antenatal clinic, pregnant women are examined for the sterility of the urogenital area. nine0005
Even in the absence of symptoms of cystitis, many women have asymptomatic bacteriuria - the excretion of microbes in the urine. Therefore, at the stage of observation in the antenatal clinic, pregnant women are examined for the sterility of the urogenital area. nine0005
Shortly before delivery, the bacterial purity of the vaginal mucosa is assessed. If pathogenic microbes are found, local treatment is prescribed. The vagina is treated with antibacterial gels, ointments, candles are placed, hygiene procedures are carried out. By such measures, the safety of the vagina is achieved and the risk of infection of the bladder during childbirth is removed.
But the best prevention of cystitis after childbirth is considered to be adequate treatment of inflammation at the stage of preparation for pregnancy. Here you can apply the whole range of available methods, one of the safest and most effective is taking Kanefron 9 drops or tablets.0003 ® H for 2-4 weeks. It can be combined with antimicrobial drugs.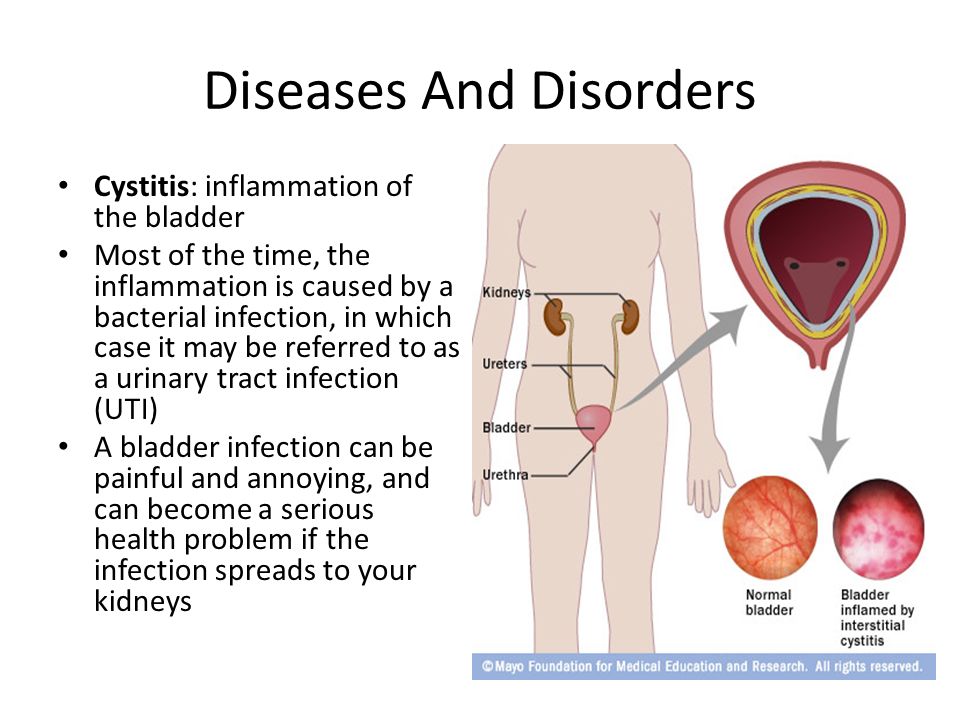
1 Le J., Briggs F. F., McKeown A., Bustillo G. Urinary tract infections during pregnancy. Ann. Pharmacother. 2004; 38(10): 1692-701.
2 Amdiy Refat Eldarovich, Al-Shukri Salman Khasunovich, and co-authors. "Experience in the use of Kanefron in the treatment of acute uncomplicated cystitis in women" Urological Gazette, vol. 6, No. 2, 2016, pp. 16-22.
3 Yu.G. Alyaev, A.V. Amosov, E.A. Sultanova // "Possibilities of using Kanefron N in the treatment of chronic cystitis", ММА them. THEM. Sechenov. "EFFICIENT PHARMACOTHERAPY. Urology and Nephrology" №2.
4 Rai, Rakhi et al. “Gangrenous Cystitis in A Woman Following Vaginal Delivery: An Uncommon Occurrence - A Case Report.” Journal of clinical and diagnostic research : JCDR 9.11 (2015): QD13-4.
5 Ferry S. A., Holm S. E., Stenlund H., Lundholm R., Monsen T. J. The natural course of uncomplicated lower urinary tract infection in women illustrated by a randomized placebo controlled study.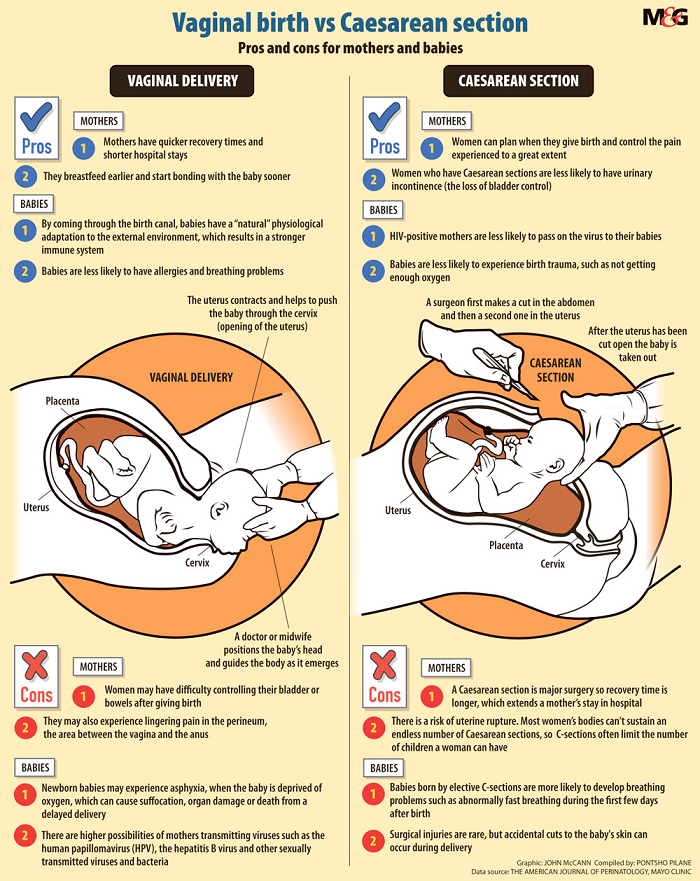 J. Infect. Dis. 2004; 36(4):296-301.
J. Infect. Dis. 2004; 36(4):296-301.
6 R. E. Amdiy. "Possibilities for the treatment of acute uncomplicated cystitis in women without the use of antibiotics" Urological Gazette, no. Special issue, 2019, pp. 16-17.
7 Instructions for use "Canephron ®".
8 Grabe M., Bartoletti R., Bjerklund-Johansen T. E., Botto H., Cai T., Qek M., Koves B., Naber K. G., Pickard R. S., Tenke P., Wagenlehner F., Wullt B Guidelines on urological infections. European Association of Urology; 2015.
9 Yu. G. Alyaev, A V. Amosov et al. // "The use of the herbal preparation Canephron N in patients with chronic cystitis and urolithiasis." Urology, 2005, №4:29-33
Recovery after caesarean section | Kaplan Medical Center
בתי חולים > קפלן > Home page > Medical departments > Obstetrics and Gynecology > Recovery after caesarean section
- from: nine0023 Professor Eddie Weisbuch
A caesarean section is a surgical procedure, a complete abdominal operation with the use of anesthesia.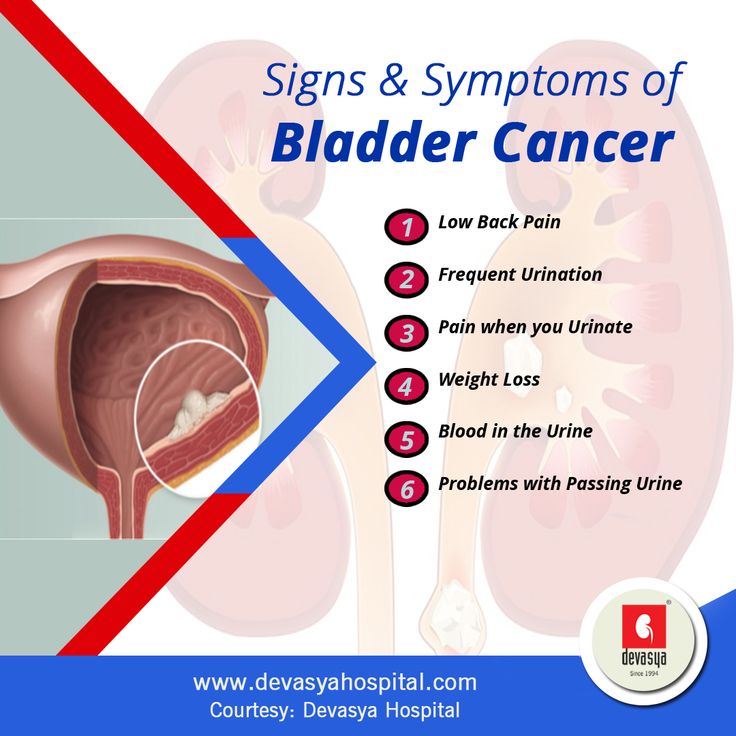 The rate of recovery after caesarean depends on compliance with the basic rules of behavior. The most important recommendation is to try to get out of bed as soon as possible to prevent the occurrence of the so-called "vein thrombosis", which is considered a relatively common complication after this operation. nine0164 Once the operation is over, you will be escorted to the intensive care unit, where you will spend about 2 hours without the child. The policy of the Kaplan Medical Center is not to separate mother and baby for a long time, therefore, in the absence of contraindications from the mother and child, feeding is allowed as soon as the woman comes to her senses after the operation. Our staff will help attach the baby (skin-to-skin contact) so that he does not freeze and help to arrange feeding if there are no contraindications for mother and child. After that, the woman and the baby are transferred to the postpartum ward, where they will spend about 4 days. Approximately six hours after the operation, the catheter will be removed from the bladder and you will be able to get out of bed and sit in a chair.
The rate of recovery after caesarean depends on compliance with the basic rules of behavior. The most important recommendation is to try to get out of bed as soon as possible to prevent the occurrence of the so-called "vein thrombosis", which is considered a relatively common complication after this operation. nine0164 Once the operation is over, you will be escorted to the intensive care unit, where you will spend about 2 hours without the child. The policy of the Kaplan Medical Center is not to separate mother and baby for a long time, therefore, in the absence of contraindications from the mother and child, feeding is allowed as soon as the woman comes to her senses after the operation. Our staff will help attach the baby (skin-to-skin contact) so that he does not freeze and help to arrange feeding if there are no contraindications for mother and child. After that, the woman and the baby are transferred to the postpartum ward, where they will spend about 4 days. Approximately six hours after the operation, the catheter will be removed from the bladder and you will be able to get out of bed and sit in a chair.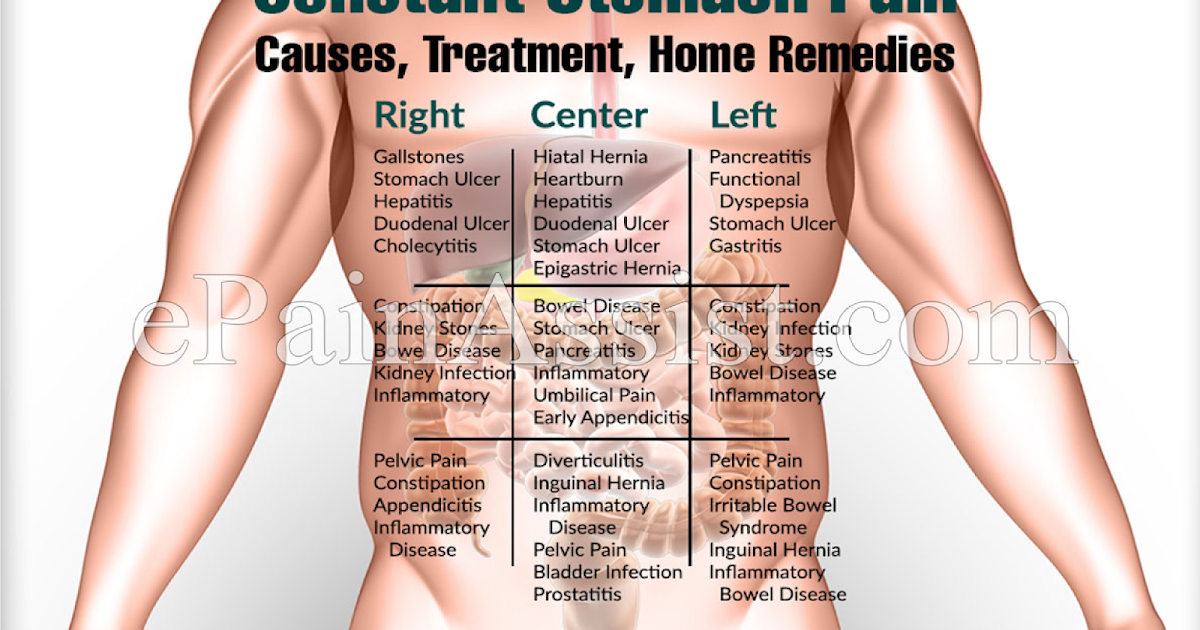 The next day, after the doctor's examination and bandaging, you can take a shower, walk around the ward and, of course, take care of your baby. The development of lactation after a caesarean section is almost the same as in women who have given birth naturally. It is most convenient in the first days after a cesarean section to feed the baby lying on its side. In this position, the postoperative suture will be least affected. In the future, it is possible to feed the baby in a sitting or standing position. nine0005
The next day, after the doctor's examination and bandaging, you can take a shower, walk around the ward and, of course, take care of your baby. The development of lactation after a caesarean section is almost the same as in women who have given birth naturally. It is most convenient in the first days after a cesarean section to feed the baby lying on its side. In this position, the postoperative suture will be least affected. In the future, it is possible to feed the baby in a sitting or standing position. nine0005
What are the main problems during postoperative recovery?
Pain : As after any surgery, you will experience pain, but there are several ways to relieve this condition. Pain caused by uterine contractions is a normal postpartum condition. But this must be reported to the medical staff and, if necessary, you will be prescribed painkillers. As in the case of pain in the incision area.
Nausea : Many suffer from nausea - this is a normal reaction of the body.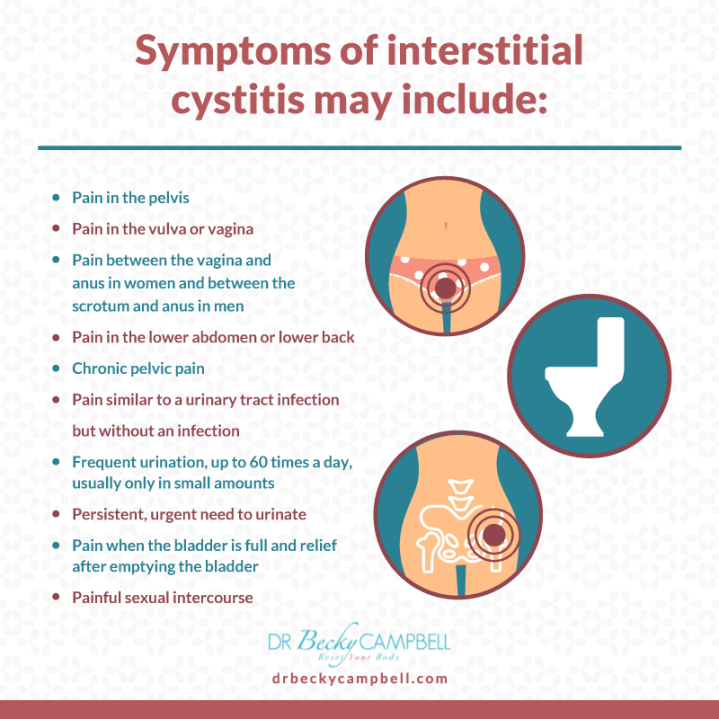 Be sure to tell the medical staff and you will be given a prophylactic intravenously. nine0164 Thirst and hunger : No food is allowed for the first few hours after surgery. Drinking is allowed, but only water or tea. Sugary and carbonated drinks are banned to prevent gas formation. Subsequently, the load on the gastrointestinal tract in the postoperative period should be increased gradually. On the second day, you can eat boiled meat, cereals, low-fat broth. Starting from the third day, the mother can already afford a more complete diet, taking into account breastfeeding. nine0164 Bleeding : As with any woman after childbirth, you will experience vaginal bleeding as a result of normal postpartum uterine changes. You should monitor the amount and color of the discharge, and if the bleeding increases or changes color (usually a brownish-pinkish discharge), notify the medical staff immediately.
Be sure to tell the medical staff and you will be given a prophylactic intravenously. nine0164 Thirst and hunger : No food is allowed for the first few hours after surgery. Drinking is allowed, but only water or tea. Sugary and carbonated drinks are banned to prevent gas formation. Subsequently, the load on the gastrointestinal tract in the postoperative period should be increased gradually. On the second day, you can eat boiled meat, cereals, low-fat broth. Starting from the third day, the mother can already afford a more complete diet, taking into account breastfeeding. nine0164 Bleeding : As with any woman after childbirth, you will experience vaginal bleeding as a result of normal postpartum uterine changes. You should monitor the amount and color of the discharge, and if the bleeding increases or changes color (usually a brownish-pinkish discharge), notify the medical staff immediately.
Constipation : these postoperative symptoms are really unpleasant, but natural.