Normal sugar level during pregnancy
Gestational Diabetes - Symptoms, Treatments
Gestational Diabetes
It can be a scary diagnosis, but it’s one that’s fairly common.
Nearly 10 percent of pregnancies in the U.S. are affected by gestational diabetes every year. So know that you’re not alone.
And know that it doesn’t mean that you had diabetes before you conceived or that you will have diabetes after you give birth. It means that, by working with your doctor, you can have a healthy pregnancy and a healthy baby. No matter what, you have all the support you need for both you and your baby.
We don’t know what causes gestational diabetes...
But we know that you are not alone. It happens to millions of women. We do know that the placenta supports the baby as it grows. Sometimes, these hormones also block the action of the mother’s insulin to her body and it causes a problem called insulin resistance. This insulin resistance makes it hard for the mother’s body to use insulin. And this means that she may need up to three times as much insulin to compensate.
Gestational diabetes can also start when the mother’s body is not able to make and use all the insulin it needs for pregnancy. Without enough insulin, glucose can’t leave the blood and be changed into energy. When glucose builds up in the blood, it’s called hyperglycemia.
Whatever the cause, you can work with your doctor to come up with a plan and maintain a healthy pregnancy through birth. Ask questions. Ask for help. There are many ways to combat gestational diabetes.
How You Can Treat ItThe key is to act quickly. As treatable as it is, gestational diabetes can hurt you and your baby.
Treatment aims to keep your blood glucose (blood sugar) levels normal. It can include special meal plans and regular physical activity. It can also include daily blood glucose testing and insulin injections.
We suggest the following target for women testing blood glucose levels during pregnancy:
- Before a meal: 95 mg/dl or less
- One hour after a meal: 140 mg/dl or less
- Two hours after a meal: 120 mg/dl or less
Always remember that this is treatable—and working with your health care team can help ensure a healthy pregnancy.
As with all forms of diabetes, diet and exercise can help you gain the upper hand. With gestational diabetes, maintaining a balanced diet is integral to your success. Your doctor can help you develop a meal plan that makes sense for you, helping you identify the best foods and quick meal ideas that can help you stay healthy and strong.
Exercise is critical as well. Work with your doctor to determine the level of activity that’s safe for you and your baby throughout your pregnancy. Use our resources as well to stay in touch with ideas for daily activity. The important thing to remember is to take action as quickly as you can, to stay with it, and to stay on top of your condition. It’s treatable. It’s manageable. And it’s a fight that you can win.
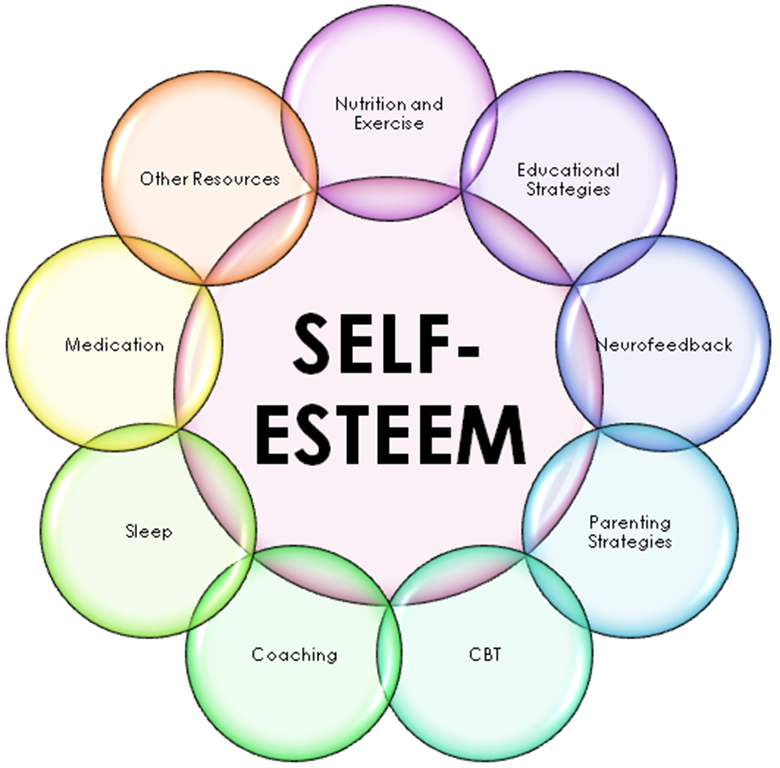
Are you depressed?
Nutrition
Fitness
Symptoms, Causes, Diet, Diagnosis, and Treatment
Written by WebMD Editorial Contributors
Medically Reviewed by Nivin Todd, MD on January 17, 2023
In this Article
- What Is Gestational Diabetes?
- Gestational Diabetes Symptoms
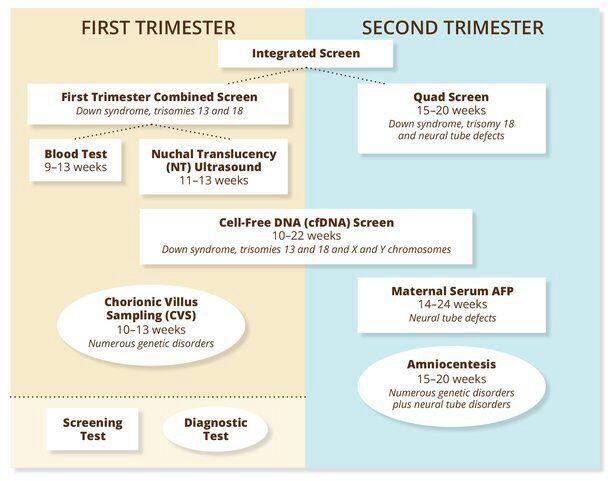
- Normal Blood Sugar Levels During Pregnancy: Chart
- Gestational Diabetes Causes
- Gestational Diabetes Risk Factors
- Gestational Diabetes Tests and Diagnosis
- Gestational Diabetes Treatment
- Target Blood Sugar Levels for Women During Pregnancy
- Diet and Exercise for Gestational Diabetes
- Gestational Diabetes Prevention
- Will Gestational Diabetes Affect My Baby?
- Will I Get Type 2 Diabetes?
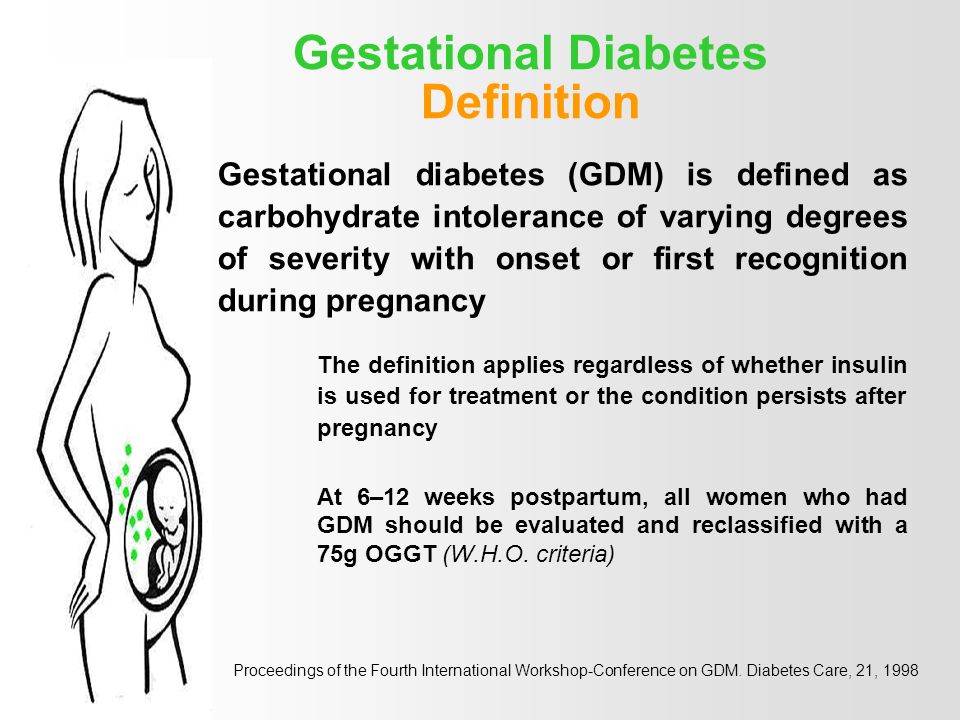
What Is Gestational Diabetes?
Gestational diabetes is a condition in which your blood sugar levels become high during pregnancy.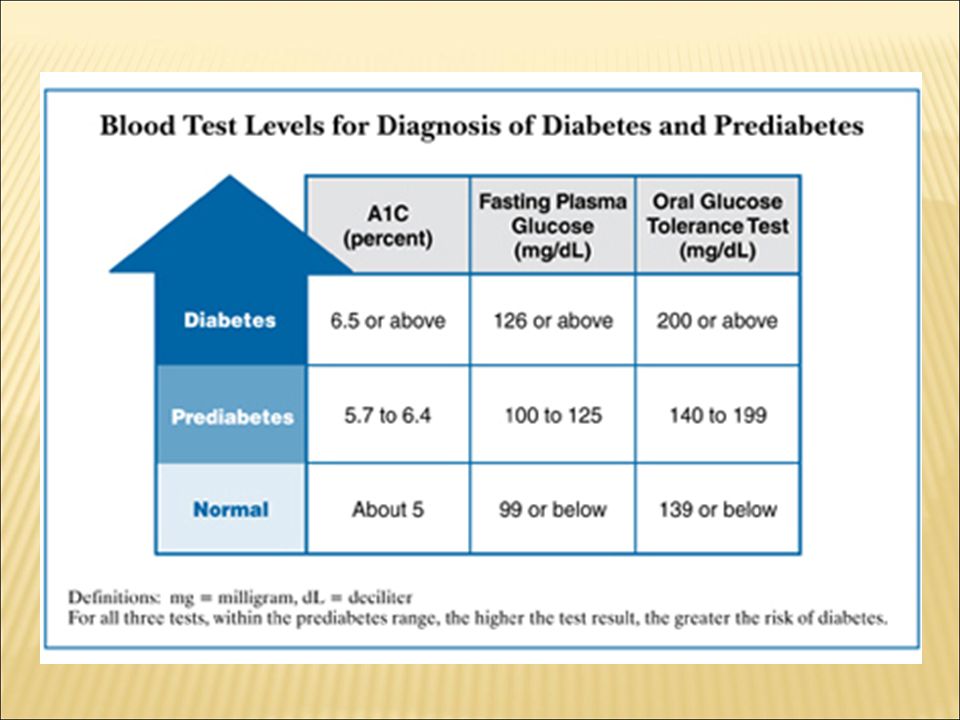 It affects up to 10% of women who are pregnant in the U.S. each year. It affects pregnant people who haven’t ever been diagnosed with diabetes.
It affects up to 10% of women who are pregnant in the U.S. each year. It affects pregnant people who haven’t ever been diagnosed with diabetes.
There are two classes of gestational diabetes. Those with class A1 can manage it through diet and exercise. Those who have class A2 need to take insulin or other medications.
Gestational diabetes goes away after you give birth. But it can affect your baby’s health, and it raises your risk of getting type 2 diabetes later in life. You can take steps so you and your baby stay healthy.
Gestational Diabetes Symptoms
If you have gestational diabetes, you usually don’t have symptoms or might chalk them up to pregnancy. Most find out that they have it during a routine screening.
You may notice that:
- You’re thirstier than usual
- You’re hungrier and eat more than usual
- You pee more than usual
Normal Blood Sugar Levels During Pregnancy: Chart
Gestational Diabetes Causes
When you eat, your pancreas releases insulin, a hormone that helps move a sugar called glucose from your blood to your cells, which use it for energy.
During pregnancy, your placenta makes hormones that cause glucose to build up in your blood. Usually, your pancreas can send out enough insulin to handle it. But if your body can’t make enough insulin or stops using insulin as it should, your blood sugar levels rise, and you get gestational diabetes.
Gestational Diabetes Risk Factors
You’re more likely to get gestational diabetes if you:
- Were overweight before you got pregnant
- Are Black, Asian, Hispanic or Latinx, Alaska Native, Pacific Islander, or Native American
- Have blood sugar levels that are higher than they should be but not high enough to be diabetes (this is called prediabetes)
- Have a family member with diabetes
- Have had gestational diabetes before
- Have polycystic ovary syndrome (PCOS) or another health condition linked to problems with insulin
- Have high blood pressure, high cholesterol, heart disease, or other medical complications
- Have given birth to a large baby (weighing more than 9 pounds)
- Have had a miscarriage
- Have given birth to a baby who was stillborn or had certain birth defects
- Are older than 25
Gestational Diabetes Tests and Diagnosis
Gestational diabetes usually happens in the second half of pregnancy. Your doctor will check for it between weeks 24 and 28, or sooner if you're at high risk.
Your doctor will check for it between weeks 24 and 28, or sooner if you're at high risk.
Your doctor will give you a glucose tolerance test: You’ll drink 50 grams of glucose in a sweet drink, which will raise your blood sugar. An hour later, you’ll take a blood glucose test to see how your body handled all that sugar. If the results show that your blood sugar is higher than a certain level, you’ll need a 3-hour oral glucose tolerance test. For this test, you’ll take a blood glucose test after you have fasted for at least 8 hours (your doctor’s office will tell you exactly how long to fast for) and then drink a beverage containing 100 grams of glucose. After that, you’ll take a blood glucose test every hour for the next 3 hours. Your doctor can also test you by having you fast for at least 8 hours, take a blood glucose test, drink a drink containing 75 grams of glucose, and then take a blood glucose test once an hour for the next 2 hours.
If you’re at high risk but your test results are normal, your doctor might test you again later in your pregnancy to make sure you still don’t have it.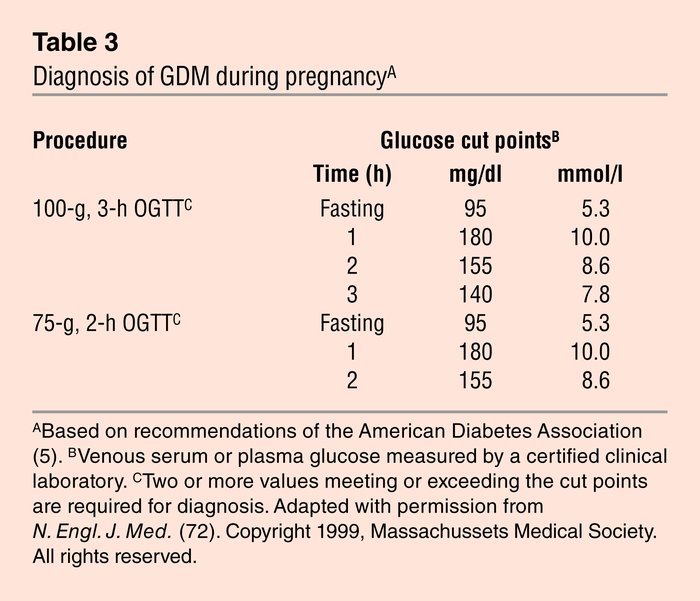
Gestational Diabetes Treatment
If you have gestational diabetes, you’ll need treatment as soon as possible to keep yourself and your baby healthy during your pregnancy and delivery. Your doctor will ask you to:
- Check your blood sugar levels four or more times a day
- Check your urine for ketones, chemicals that mean that your diabetes isn’t under control
- Eat a healthy diet
- Make exercise a habit
Your doctor will keep track of your weight and your baby’s development. They might give you insulin or another medicine to keep your blood sugar under control.
Target Blood Sugar Levels for Women During Pregnancy
The American Diabetes Association recommends these targets for pregnant women who test their blood sugar:
- Before a meal: 95 mg/dL or less
- An hour after a meal: 140 mg/dL or less
- Two hours after a meal: 120 mg/dL or less
Diet and Exercise for Gestational Diabetes
Take these simple steps to stay well:
Eat a healthy, low-sugar diet. Talk to your doctor to be sure you’re getting the nutrition you need. Follow a meal plan made for someone with diabetes:
Talk to your doctor to be sure you’re getting the nutrition you need. Follow a meal plan made for someone with diabetes:
- Trade sugary snacks like cookies, candy, and ice cream for natural sugars like fruits, carrots, and raisins. Add vegetables and whole grains, and watch your portion sizes.
- Have three small meals along with two or three snacks about the same times every day.
- Get 40% of your daily calories from carbs and 20% from protein. Most of the carbs should be complex, high-fiber carbs, with fat being between 25% and 40%.
- Aim for 20-35 grams of fiber a day. Foods such as whole-grain breads, cereals, and pasta; brown or wild rice; oatmeal; and vegetables and fruits will help get you there.
- Limit your total fat to less than 40% of your daily calories. Saturated fat should be less than 10% of all the calories you eat.
- Eat a variety of foods to make sure you get enough vitamins and minerals. You may need to take a supplement to cover your bases.
 Ask your doctor if they think you should take one.
Ask your doctor if they think you should take one.
Exercise throughout your pregnancy. You can exercise when you have gestational diabetes as long as your doctor says it’s OK. Being active is a good way to help manage your blood sugar. Staying fit during pregnancy is also good for your posture and can curb some common problems, like backaches and fatigue.
- Get active as soon as possible. Aim for 30 minutes of moderate activity most days of the week. Running, walking, swimming, and biking are good options. If you are not active now, start slowly and build up to 30 minutes a day.
- Was there a workout that you were doing before you found out you were pregnant? Do you have an activity that you love? Check with your doctor to see if you can keep it up, if you should make some changes, or if it's better to try something else.
- Exercise can lower your blood sugar. So when you work out, always have a form of quick sugar with you, such as glucose tablets or hard candy.
Get the right prenatal care: Your doctor can check to see if you have gestational diabetes and offer advice on food, activity, and weight loss. They can also point you to other health professionals, like nutritionists, that can help.
If you have morning sickness, eat small snacks. Nibble on crackers, cereal, or pretzels before you get out of bed. As you go through your day, have small meals often and avoid fatty, fried, and greasy foods.
If you take insulin, make sure you've got a plan to deal with low blood sugar. Throwing up can make your glucose level drop. Talk to your doctor if you're not sure what to do.
Gestational Diabetes Prevention
You can lower your risk before you get pregnant by:
- Eating a healthy diet
- Staying active
- Losing extra weight
Will Gestational Diabetes Affect My Baby?
Your baby will probably be healthy if you and your doctor manage your blood sugar while you have gestational diabetes.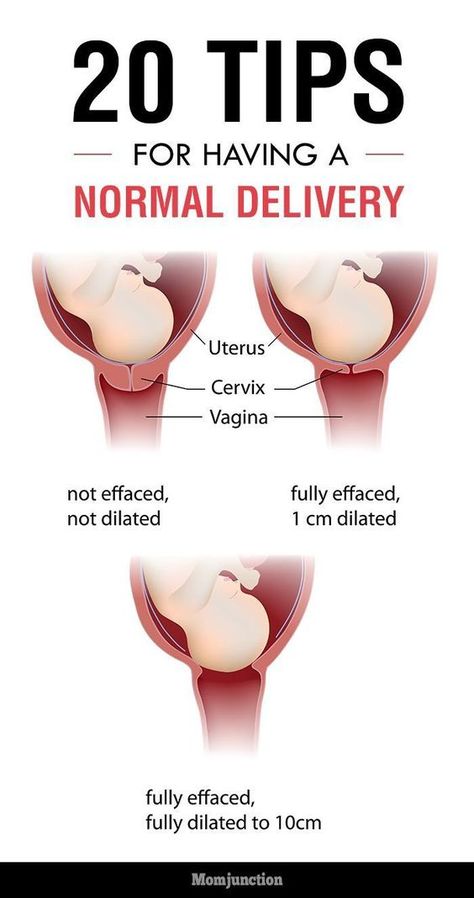
Right after you give birth, doctors will check your newborn's blood sugar level. If it’s low, your baby may need to get glucose through an IV until it comes back up to normal.
Gestational diabetes raises the chance that your baby will be larger than normal. It's also linked to jaundice, in which the skin looks yellowish. Jaundice generally fades quickly with treatment.
Although your child will be more likely than other kids to get type 2 diabetes later on, a healthy lifestyle (including a good diet and lots of physical activity) can cut that risk.
Will I Get Type 2 Diabetes?
Because you had gestational diabetes, you have a greater chance of having type 2 diabetes. But it won’t definitely happen, and you can take action to prevent that.
Your blood sugar levels will likely return to normal about 6 weeks after childbirth. (Your doctor will check on that.) If it does, you should get follow-up tests at least every 3 years; your doctor may recommend yearly testing.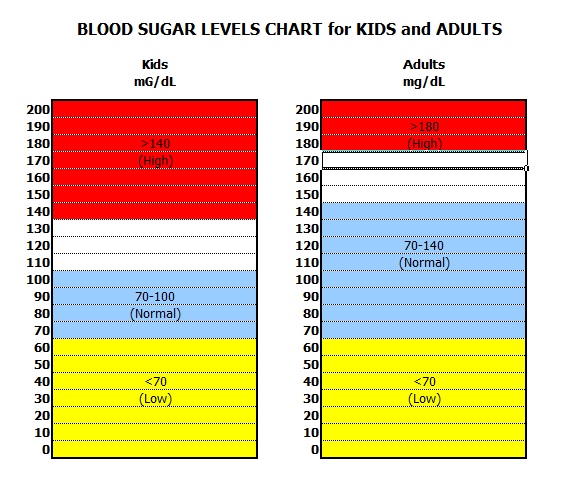
To lower your risk:
- Try to keep your weight in a healthy range. Not sure what that is? Ask your doctor.
- Eat a good diet that includes lots of vegetables, whole grains, fruits, and lean protein.
- Make exercise a habit.
If you plan to have another baby, keep in mind that you are more likely to get gestational diabetes again. Ask your doctor if there are any lifestyle changes that would help you avoid that.
Gestational diabetes in pregnancy - treatment and diagnosis of diabetes in pregnant women in Moscow, Clinical Hospital on Yauza
Consult a gynecologist
Service in two languages: Russian, English.
Leave your phone number and we will call you back.
Contents
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Specialists of the Yauza Clinical Hospital diagnose and treat gestational diabetes and its complications. For a comfortable pregnancy and the safety of the expectant mother and baby, we exercise strict control over the blood sugar level of a pregnant woman, if necessary, prescribe a specially designed diet and medications.
Make an appointment with a gynecologist
- About 7% of pregnant women have manifestations of gestational diabetes. In 50% of cases, the disease is asymptomatic
- Gestational diabetes in pregnancy significantly increases the risk of pregnancy complications for both mother and fetus
- Perinatal mortality increases by 2-3% with a combination of diabetes mellitus and pregnancy
Pregnancy diabetes (gestational diabetes) is an increase in blood glucose that first occurs during pregnancy but is not high enough to warrant a diagnosis of diabetes mellitus.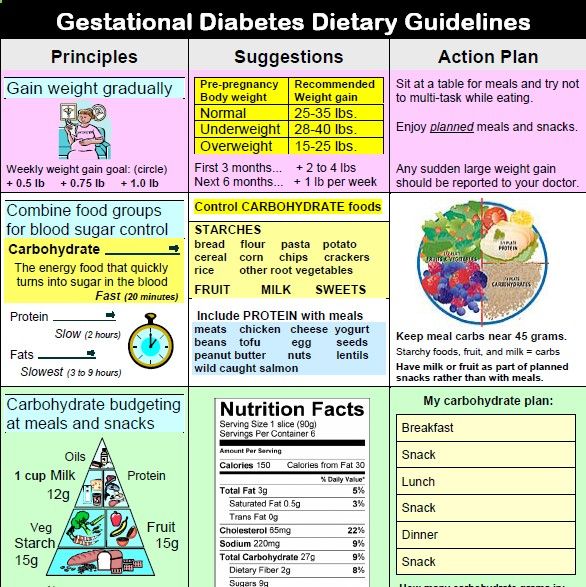 These are hidden disorders of carbohydrate metabolism that threaten to develop into diabetes mellitus.
These are hidden disorders of carbohydrate metabolism that threaten to develop into diabetes mellitus.
Pregnant blood glucose norm
During pregnancy, all women experience changes in insulin sensitivity and glucose tolerance. This is fine. The difference between the norm and pathology in the degree of change.
Blood tests for diabetes during pregnancy - norm and pathology
- If the test of venous blood taken on an empty stomach shows a glucose level of more than 5.1 mmol / l, this is the norm for pregnant women.
- From 5.1 to 7.0 mmol / l - gestational diabetes.
- If 7.0 mmol / l or more - diabetes mellitus.
- Testing capillary blood (taken from a fingerstick) for the diagnosis of gestational diabetes mellitus is not recommended.
- If during an oral glucose tolerance test (when 75 g of glucose is taken orally during the study) after an hour the glucose level is more than 10.
 0 mmol/l, and after two hours the blood glucose level is in the range of 7.8-8.5 mmol/l - then for pregnant women this is a normal indicator.
0 mmol/l, and after two hours the blood glucose level is in the range of 7.8-8.5 mmol/l - then for pregnant women this is a normal indicator.
To better understand what gestational diabetes, or diabetes in pregnancy, is, you need to talk a little about hormonal changes in the body in pregnant women.
Causes of gestational diabetes
Hormonal changes that occur during pregnancy are associated with increased production of large amounts of steroid hormones. Some of them, such as cortisol and progesterone, have a significant effect on cell receptors, increasing their resistance to insulin.
This leads to an increase in blood glucose levels and requires a significant increase in insulin production by the pancreas. In cases where the compensatory capacity of the pancreas is not enough, sugar metabolism gets out of control and a condition called gestational diabetes or gestational diabetes develops.
This condition occurs quite often. Between 3 and 10% of pregnant women develop pathological insulin resistance leading to gestational diabetes.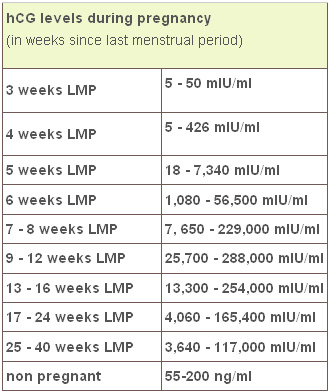
Unlike diabetes mellitus diagnosed before pregnancy, pathological insulin resistance that occurs during pregnancy does not cause fetal malformations and in most cases does not require insulin treatment. But, nevertheless, uncompensated gestational diabetes can significantly complicate the course of pregnancy.
Specialists of the Yauza Clinical Hospital diagnose, treat and prevent diabetes in pregnant women and its complications, such as impaired fetal growth. The doctors of the Clinical Hospital on the Yauza strictly control the blood sugar level of a pregnant woman, if necessary, prescribe a specially designed diet. This ensures a comfortable pregnancy and the safety of the expectant mother and baby.
Pregnancy diabetes - consequences for the child
Large disproportionate fruit. The most important and frequent complication of gestational diabetes is fetal growth failure. Developing in conditions of increased blood glucose levels, which penetrate the fetoplacental barrier, the fetus is forced to compensate for the increased sugar level with its own insulin.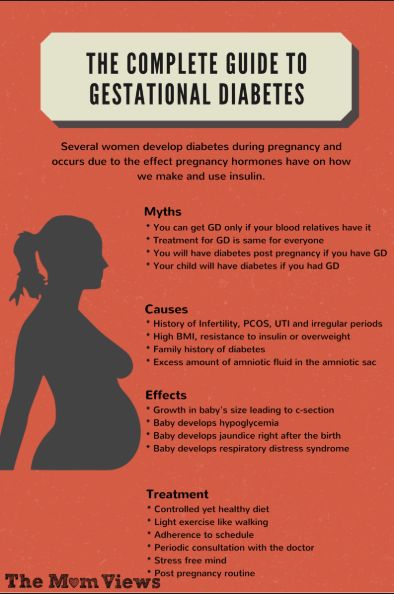 Due to the fact that the structure of insulin and growth hormone are very similar, high levels of insulin stimulate the growth of the fetus. The problem is that a large fetus develops. In such a fetus, body proportions differ from those of normally developing newborns, in which the volume of the head is larger than the volume of the shoulder girdle. In fetuses with uncompensated gestational diabetes, the size of the shoulder girdle predominates, and the size of the abdomen increases. This leads to the fact that during childbirth after the fetus's head passes through the birth canal, the shoulders can get stuck (shoulder dystocia) and the child, along with the mother, can be severely injured or die.
Due to the fact that the structure of insulin and growth hormone are very similar, high levels of insulin stimulate the growth of the fetus. The problem is that a large fetus develops. In such a fetus, body proportions differ from those of normally developing newborns, in which the volume of the head is larger than the volume of the shoulder girdle. In fetuses with uncompensated gestational diabetes, the size of the shoulder girdle predominates, and the size of the abdomen increases. This leads to the fact that during childbirth after the fetus's head passes through the birth canal, the shoulders can get stuck (shoulder dystocia) and the child, along with the mother, can be severely injured or die.
Polyhydramnios or oligohydramnios. In addition, in gestational diabetes, the balance of the amount of amniotic fluid can be disturbed and either polyhydramnios or oligohydramnios develops. This is a serious risk factor for intrauterine fetal death or premature birth.
Underdevelopment of the lungs. In gestational diabetes, the lungs of the fetus mature later, as the production of surfactant (a special lubrication of the inner walls of the alveoli, where oxygen is exchanged in the lungs) is disrupted. Therefore, premature birth in gestational diabetes is especially dangerous.
Hypoglycemia and metabolic disorders in the fetus. Due to the constant increased production of its own insulin during pregnancy, immediately after birth, the child is in a state of hypoglycemia with electrolyte imbalance, which threatens his life.
All this dictates the need for the earliest possible detection of gestational diabetes in pregnant women, the level of sugar in the blood of a pregnant woman and to prevent the development of complications.
.
Diagnosis of diabetes in pregnant women at the Yauza Clinical Hospital
Signs of diabetes in pregnant women
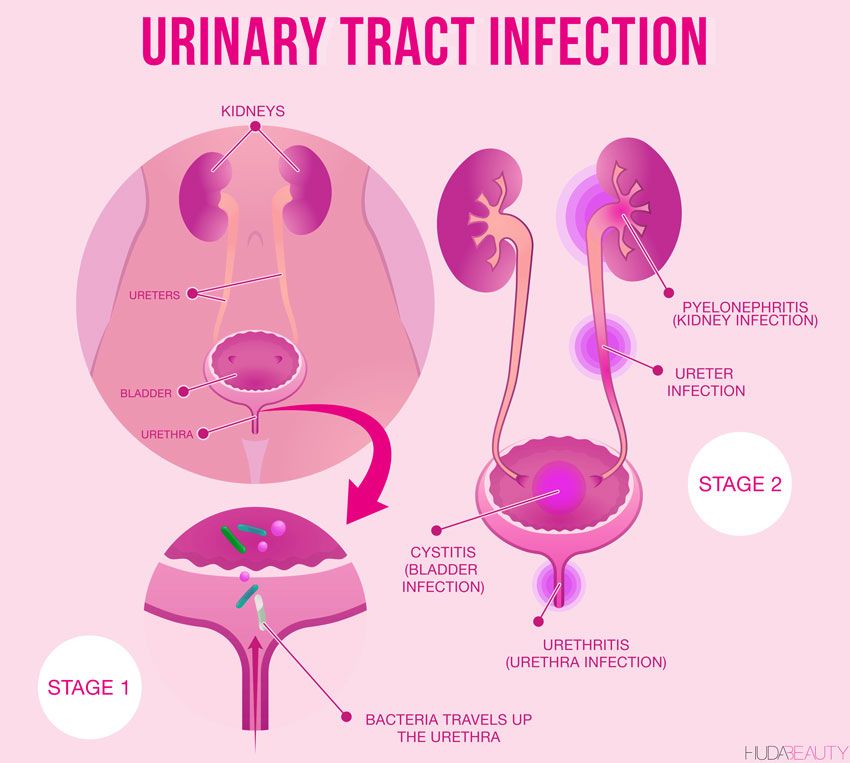
Gestational diabetes in pregnancy is not usually associated with the classic symptoms of diabetes, such as thirst or excessive urination (polyuria).
Pregnancy tests for diabetes mellitus
First phase. At the first visit of a pregnant woman to a doctor at any time, she is tested for glucose levels in venous blood - fasting glucose, regardless of food intake, glycated hemoglobin. This is the first phase of research to detect diabetes mellitus or gestational diabetes in pregnant women. If diabetes mellitus is detected, the patient is referred for observation and treatment to an endocrinologist.
Second phase. For a period of 24-28 weeks, all patients who did not show identified disorders of carbohydrate metabolism at the first study are called for a glucose tolerance test (PGTT) to detect "hidden diabetes". This is done because the occurrence of gestational diabetes is associated with the development of insulin resistance under the influence of hormones produced by the placenta. Therefore, in the vast majority of cases, gestational diabetes develops in the second half of pregnancy after 24 weeks, when there is a peak in the production of placental hormones.
Glucose tolerance test
It is carried out to detect pathological insulin resistance, characteristic of latent diabetes in pregnant women. Pregnant women undergo a two-hour test, only in the laboratory.
During the 3 days leading up to the test, the woman should eat her usual diet, including carbohydrates (>150 g of carbohydrates per day), maintain her usual physical activity. The evening before testing, dinner should include 30-50 grams of carbohydrates.
On the day of the study, before the analysis, you should not smoke and take medications that can affect the level of glucose (vitamins, glucocorticoid hormones, iron preparations, which include carbohydrates, beta-agonists, beta-blockers). You can drink water.
Venous blood is taken on an empty stomach (after 8-14 hours of fasting, usually in the morning, before breakfast).
Then the patient takes a glucose solution (75 g).
And they take blood in an hour and two after the sugar load.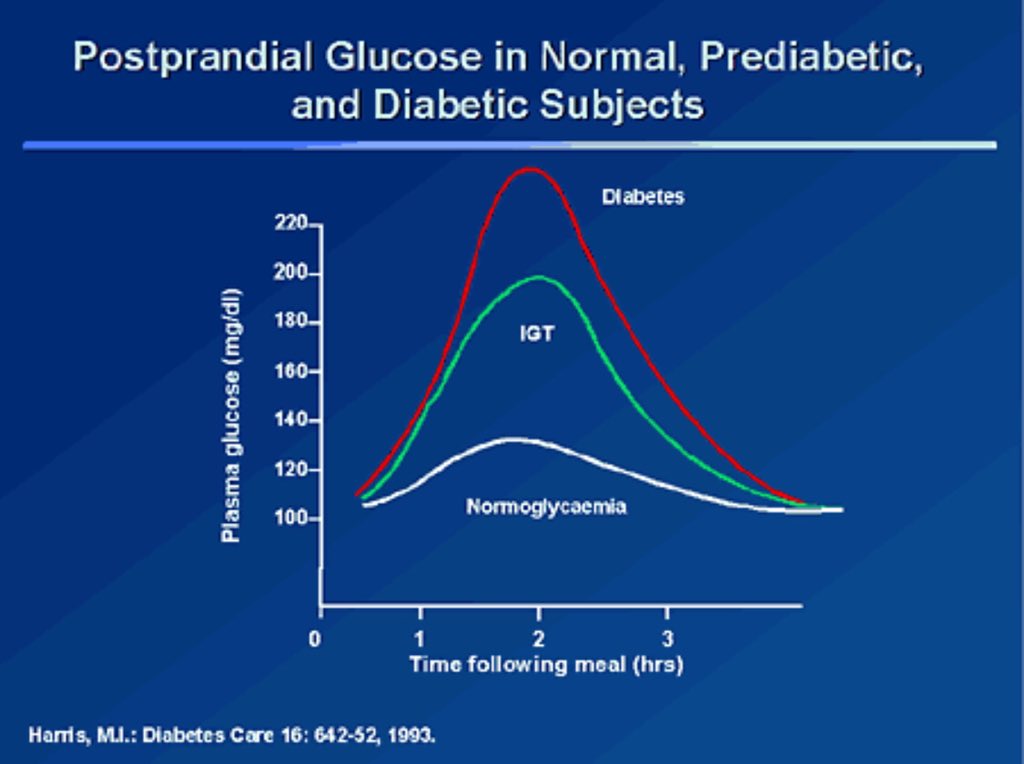 Normally, the level of glucose in the blood after a sugar load should not exceed an hour later - 10 mmol / l, after 2 hours - 8.5 mmol / l.
Normally, the level of glucose in the blood after a sugar load should not exceed an hour later - 10 mmol / l, after 2 hours - 8.5 mmol / l.
If manifest diabetes mellitus is detected, the patient is referred to an endocrinologist, gestational diabetes mellitus is treated by an obstetrician-gynecologist or therapist.
Glucose tolerance test contraindications
- Strict bed rest for a pregnant woman (until doctor's approval).
- Pronounced toxicosis of pregnant women (with nausea and vomiting).
- Acute infectious or inflammatory disease.
- Exacerbation of chronic pancreatitis.
- Dumping syndrome (syndrome of resected stomach).
Prenatal diabetes monitoring
Blood glucose monitoring, self-monitoring diary
When diagnosing gestational diabetes, it is necessary to establish strict control of sugar levels throughout the subsequent pregnancy and during childbirth. To do this, regularly examine the blood for sugar (glucose). In addition, the patient conducts self-monitoring using a glucometer.
In addition, the patient conducts self-monitoring using a glucometer.
It is recommended that a pregnant woman keep a diary of observations in which to record:
- blood glucose level (normal <5.1 mmol/l),
- the presence of ketone bodies in the urine, which is determined by test strips sold in a pharmacy (normally, ketone bodies are absent),
- blood pressure readings (normal <130|80 mmHg),
- fetal movements,
- body weight,
- diet.
Expert ultrasound
Conducting an expert ultrasound examination reveals signs of intrauterine suffering of the fetus (diabetic fetopathy), polyhydramnios. Most often, this is a sign of chronically elevated blood glucose levels, penetrating into the blood of the fetus. This requires urgent correction of the diet and normalization of the level of glycemia (blood sugar). If necessary, insulin therapy.
Make an appointment
Treatment of gestational diabetes
Diet for gestational diabetes
In most cases, it is sufficient to follow a special diet recommended by a nutritionist based on the body mass index of the pregnant woman and her taste preferences.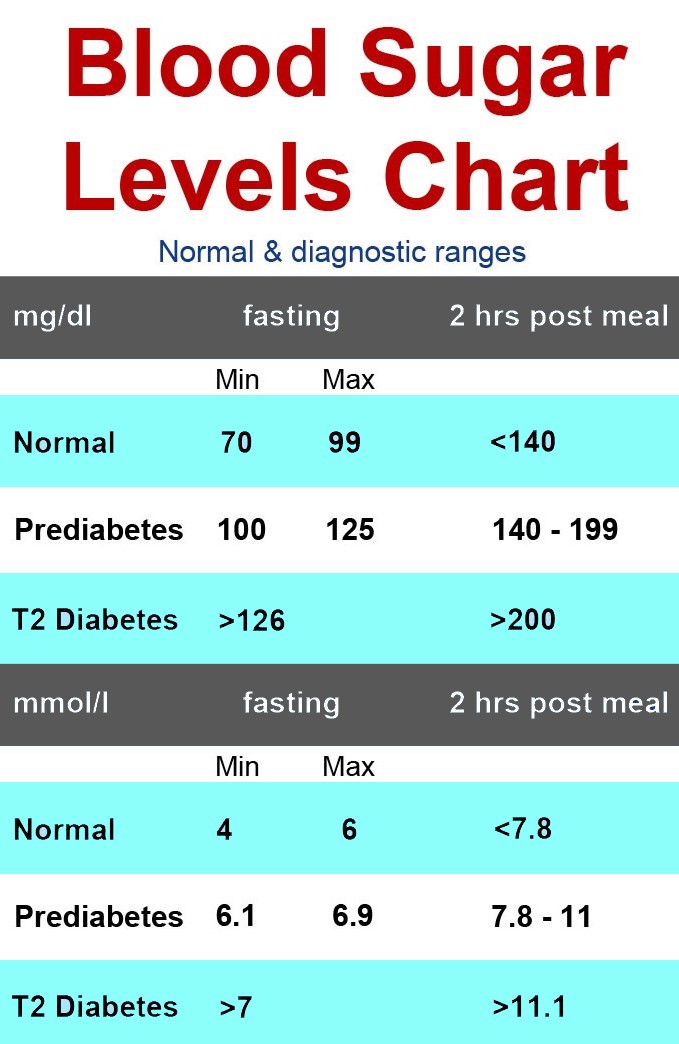 The effectiveness of diet therapy is determined by the maintenance of normal blood glucose levels. Diet in pregnancy diabetes recommends:
The effectiveness of diet therapy is determined by the maintenance of normal blood glucose levels. Diet in pregnancy diabetes recommends:
- Avoid simple carbohydrates - sweets, pastries, white bread, honey, sugar, jam, sweet drinks and fruits, ice cream.
- Limit complex carbohydrates - cereals (semolina, rice - exclude), potatoes, corn, legumes, durum wheat pasta. Distribute their intake evenly over several meals throughout the day to eliminate starvation (causes the formation of ketone bodies).
- Eat enough protein - meat, fish, seafood, poultry, mushrooms, eggs, hard cheese, dairy and sour-milk products of medium fat content (3-5%).
- It is necessary to enrich the diet with fiber and vitamins - greens, vegetables (except for boiled carrots and beets), sweet and sour berries (excluding grapes).
- Correctly choose fats, do not exceed their amount recommended by the doctor - vegetable oils (add to ready-made meals), nuts, seeds. Animal fats (butter, sausages) - limit.

- When cooking, boil, stew, steam and bake dishes. Don't fry. Do not deep fry.
A detailed menu for a pregnant woman with gestational diabetes will be compiled by a doctor, taking into account the individual characteristics of each particular woman.
It is not worth using table No. 9 in its pure form for pregnant women with diabetes mellitus due to a significant restriction of its calorie content.
In detail, what you can eat with diabetes in pregnant women will be told by the doctor at an in-person consultation.
Pharmacotherapy
In cases where the diet fails to achieve the desired control of the level of glycemia in the blood, there are signs of a negative effect on the fetus - they resort to prescribing drugs - insulin. In case of diabetes in pregnant women, antidiabetic drugs in tablets should not be used. Insulin therapy is prescribed by an endocrinologist. Pregnant women with diabetes who are on insulin therapy are jointly managed by an endocrinologist, an internist and an obstetrician-gynecologist.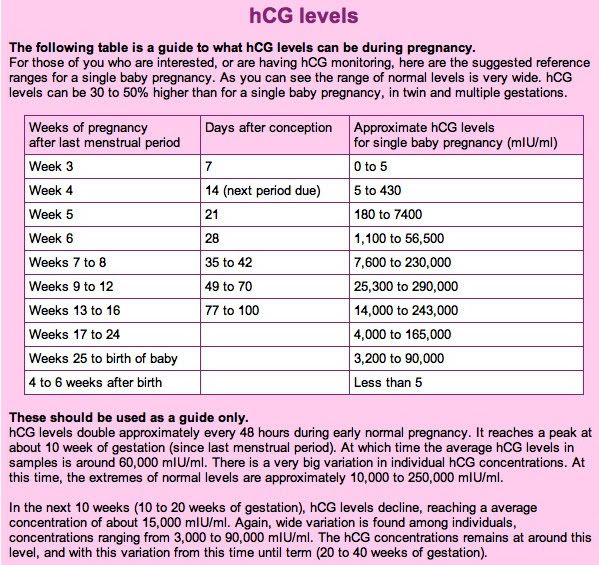
Physical activity
Patients are recommended regular physical activity - walking in the fresh air (at least 150 minutes per week), swimming.
Prenatal diabetes - childbirth
With a compensated course of gestational diabetes, normal development of the fetus and the condition of the woman, childbirth is carried out in time in a natural way. The question of early delivery, caesarean section may arise if there are relevant indications from the mother or fetus.
Specialists of the Yauza Clinical Hospital have included mandatory fetal development screenings and tests to diagnose sugar metabolism disorders in the pregnancy monitoring program. Recommendations are given on a special diet for women with manifestations of gestational diabetes. If necessary, strict glycemic control is carried out throughout pregnancy, ensuring its successful completion and the birth of a healthy child.
Make an appointment
Cost of services
Prices for services you can see in the price list or check by phone listed on the site.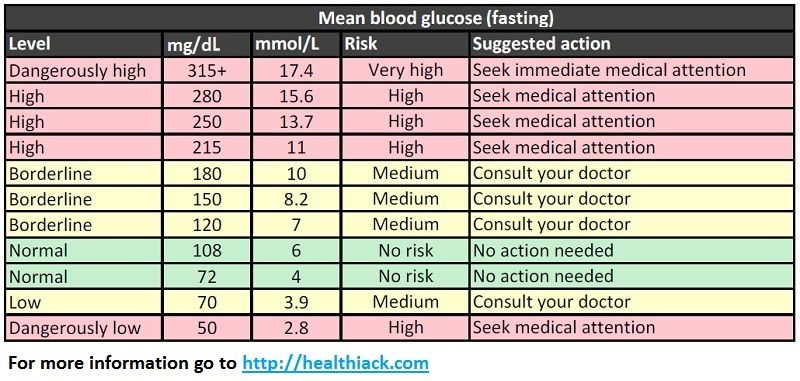
Attention! Website prices may vary.
Please check the current cost with the administrators by phone.
BOOK AN APPOINTMENT. WE WORK WITHOUT DAYS OFF
Service in two languages: Russian, English.
Leave your phone number and we will call you back.
Advantages of the clinic
More appears during pregnancy in women who did not have diabetes before.
Outside of pregnancy, blood glucose levels up to and including 6.0 mmol/L are considered normal. But pregnant women are different. The level of sugar becomes lower, due to the costs of the developing fetus, a decrease in the formation of glucose in the liver and other processes. Therefore, the value of glucose in a pregnant woman on an empty stomach of 5.1 mmol / l and higher (but up to 7.0 mmol / l), even with a single determination, indicates gestational diabetes mellitus.
Above 7.0 mmol/l is manifest diabetes, which requires immediate contact with an endocrinologist and initiation of insulin therapy. Often this means that diabetes was before pregnancy, but was not detected.
Often this means that diabetes was before pregnancy, but was not detected.
Gestational diabetes is dangerous because it can cause a number of complications during pregnancy and childbirth, namely: stillbirth, miscarriage, high risk of obesity and the development of diabetes later.
For a woman, this condition is also unsafe: the risks of preeclampsia, the need for a caesarean section and the development of diabetes mellitus after childbirth increase.
Fortunately, all these consequences can be avoided if you consult a doctor and start treatment.
Gestational diabetes is usually asymptomatic, but can sometimes present with excessive fatigue, constant thirst, frequent urination, and blurred vision. All this can be attributed to stress and weather. Therefore, it is possible to accurately diagnose with the help of tests.
After the 6th week of pregnancy, blood glucose is tested from a vein.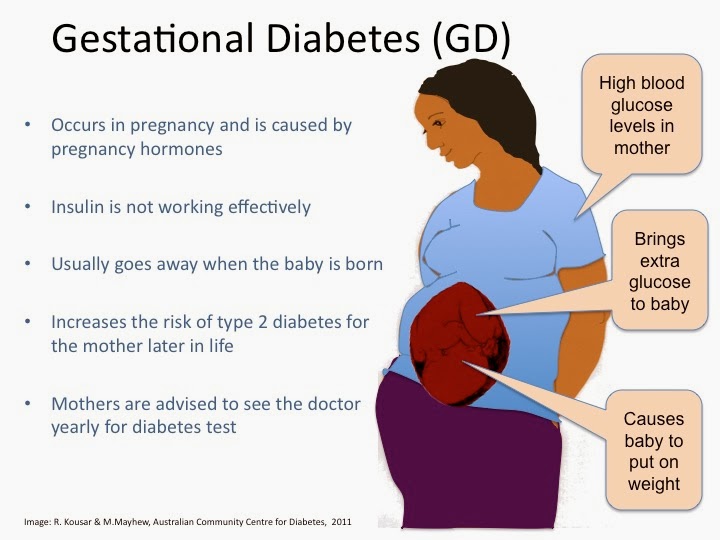 Normally, the result is up to 5.0 mmol / l inclusive. An increase in sugar to 5.1 mmol / l or more requires intervention - a consultation with an endocrinologist who will talk about the need to change diet, lifestyle, regular self-monitoring of blood sugar, in some cases, insulin treatment is prescribed.
Normally, the result is up to 5.0 mmol / l inclusive. An increase in sugar to 5.1 mmol / l or more requires intervention - a consultation with an endocrinologist who will talk about the need to change diet, lifestyle, regular self-monitoring of blood sugar, in some cases, insulin treatment is prescribed.
At 24-28 weeks, all pregnant women with normal blood glucose are given an oral glucose tolerance test (OGTT) to detect underlying disorders. OGTT is included in the list of examinations that are carried out as part of the MHI.
You can reduce your risk of gestational diabetes by making lifestyle changes. To do this, you need:
- have a BMI less than 25,
- switch to a healthy diet,
- 150 minutes of physical activity per week,
- stop smoking.
Our endocrinologists act within the framework of clinical recommendations, Russian and international, and do not prescribe unnecessary tests and drugs.