Migraine early pregnancy sign
Causes, Treatments, When to Worry
Migraine and Pregnancy: Causes, Treatments, When to Worry- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
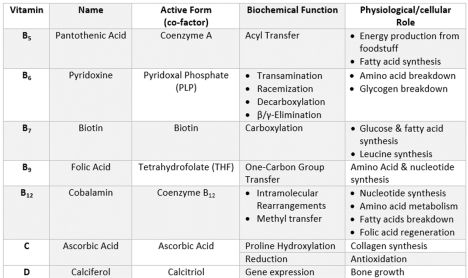
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
We’re gonna give it to you straight: Pregnancy can mess with your head. And we’re not just talking about brain fog and forgetfulness. We’re also talking about headaches — migraine attacks, in particular.
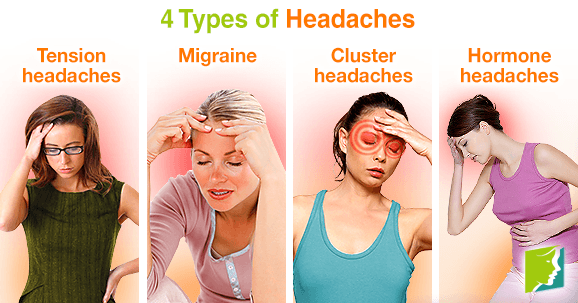
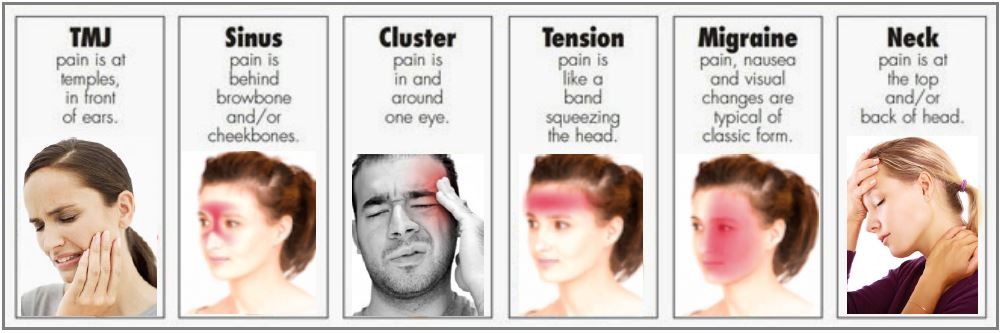
Migraine is a type of headache that can cause intense throbbing, usually on one side of the head. Imagine having a 3-year-old living behind your eye socket and relentlessly pounding a drum. Each beat sends waves of agony through your skull. The pain can make natural childbirth seem like a walk in the park.
Well, almost. Maybe we shouldn’t go that far — but migraine attacks can be very painful.
Migraine affects about 30 million Americans, 75 percent of whom are women. While many women (up to 80 percent) find that their migraine attacks improve with pregnancy, others struggle on.
In fact, about 15 to 20 percent of pregnant women experience migraine. Women who have migraine attacks with “aura” — a neurological event that accompanies or proceeds migraine and can manifest as flashing lights, wavy lines, vision loss, and tingling or numbness — generally don’t see their headaches improve during pregnancy, according to experts.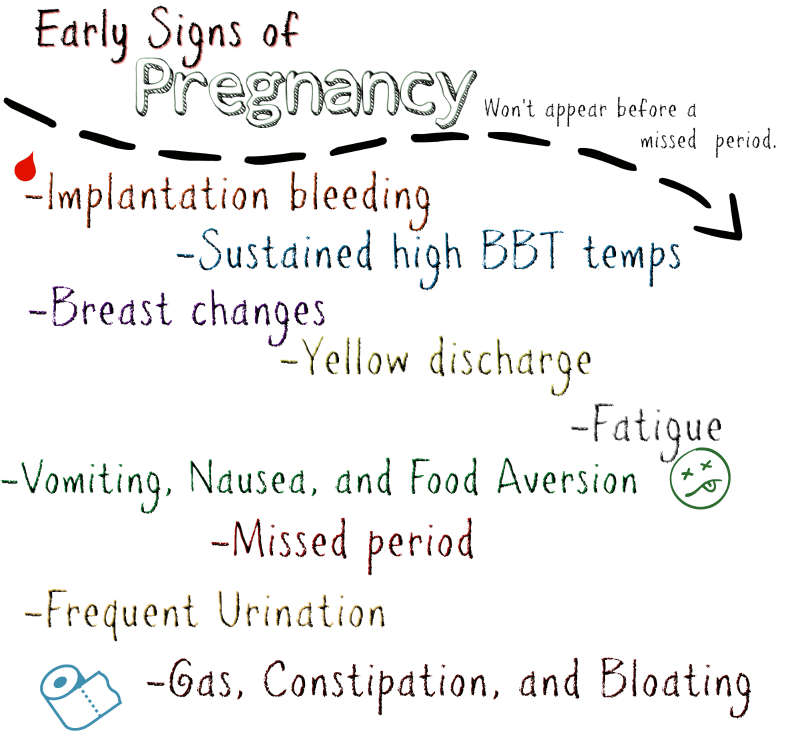
So what’s a mom-to-be to do when a migraine attack strikes? What’s safe to take and what’s not? Is migraine ever dangerous enough that you should seek emergency medical care?
Most headaches during pregnancy — including migraine — are nothing to worry about. But that’s not to say that migraine attacks aren’t incredibly annoying, and, in some cases, dangerous for pregnant women and their babies.
Here’s everything you need to know about migraine during pregnancy so you can tackle the pain — head on.
Migraine headaches seem to have a genetic component, which means they tend to run in families. That said, there’s usually a triggering event that unleashes them. One of the most common triggers — at least for women — is fluctuating hormone levels, particularly the rise and fall of estrogen.
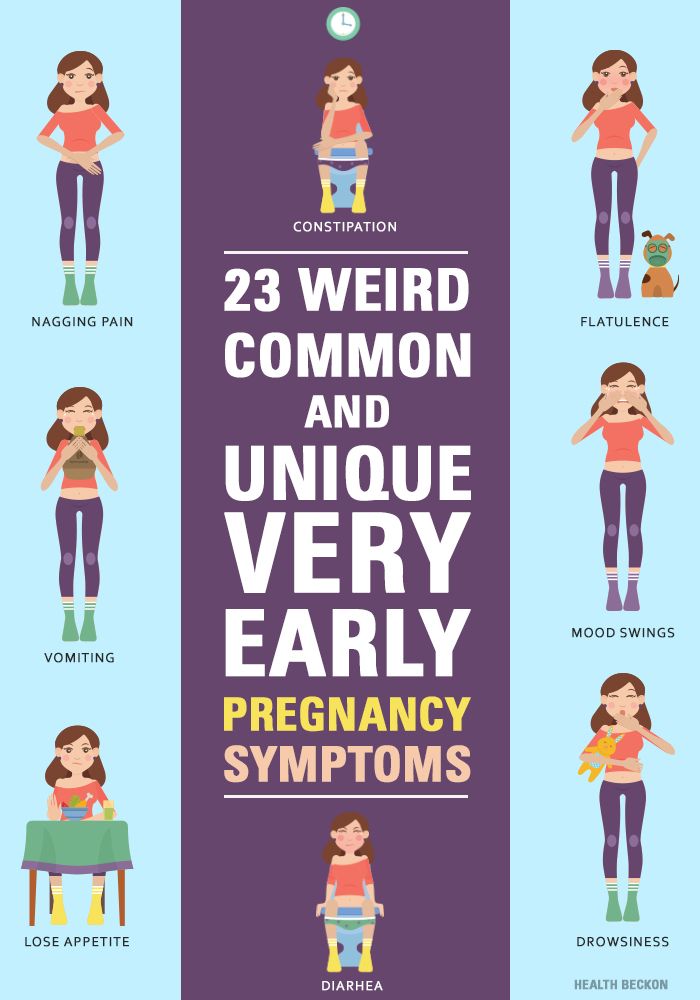
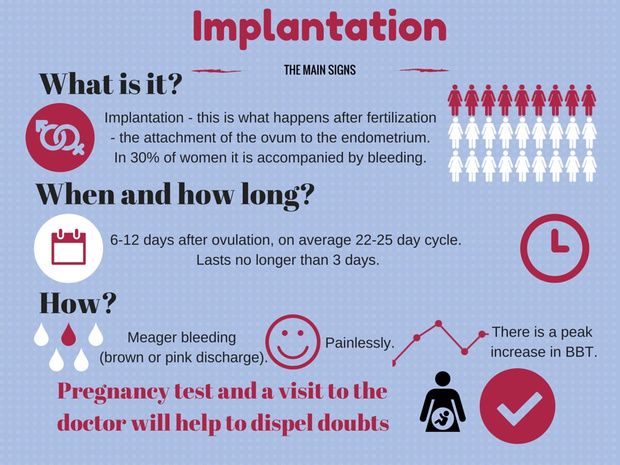
Moms-to-be who get migraine attacks tend to experience them most often in the first trimester of pregnancy, when hormone levels, including estrogen, haven’t yet stabilized. (In fact, headaches in general are an early pregnancy sign for a lot of women.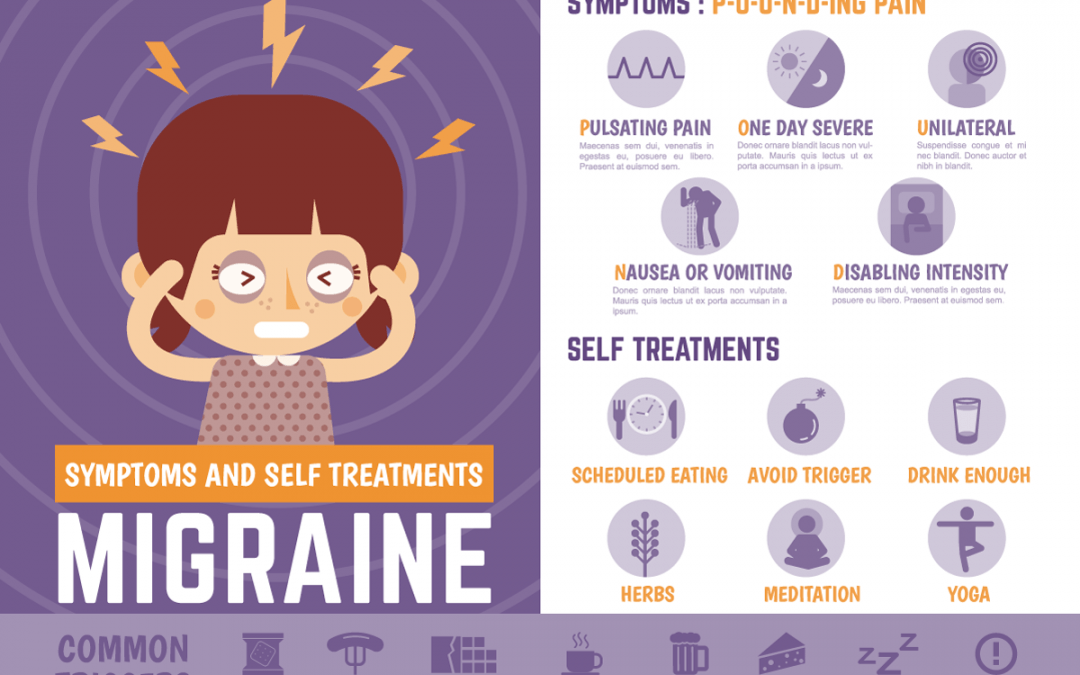 )
)
An increase in blood volume, which is also common in the first trimester, can be an additional factor. As blood vessels in the brain expand to accommodate extra blood flow, they can press against sensitive nerve endings, causing pain.
Other common migraine triggers, whether you’re pregnant or not, include:
- Not getting enough sleep. The American Academy of Family Physicians recommends 8–10 hours per night when you’re pregnant. Sorry, Jimmy Fallon — we’ll catch you on the flip side.
- Stress.
- Not staying hydrated. According to the American Migraine Foundation, one-third of those who get migraine headaches say dehydration is a trigger. Pregnant women should aim for 10 cups (or 2.4 liters) of fluid daily. Try to drink them earlier in the day so sleep isn’t interrupted by nighttime visits to the bathroom.
- Certain foods. These include chocolate, aged cheeses, wines (not that you should be drinking any of those), and foods containing monosodium glutamate (MSG).

- Exposure to bright, intense light. Light-related triggers include sunlight and florescent lighting.
- Exposure to strong smells. Examples include paints, perfumes, and your toddler’s explosive diaper.
- Weather changes.
A migraine attack while you’re pregnant will look a lot like a migraine attack when you’re not pregnant. You’re apt to experience:
- throbbing head pain; usually it’s one-sided — behind one eye, for example — but it can occur all over
- nausea
- sensitivity to light, smells, sounds, and movement
- vomiting
When you’re pregnant, you have to think twice about everything you put into your body. Is it OK to have that second cup of coffee? What about a nibble of Brie? When you’re hit with the mother of all headaches — migraine — you want real relief quickly. But what are your options?
At-home remedies
These should be your first line of defense to avoid and treat migraine:
- Know your triggers.
 Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack.
Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack. - Hot/cold compresses. Figure out what eases migraine pain for you. A cold pack (wrapped in a towel) placed over your head can numb the pain; a heating pad around your neck can ease tension in tight muscles.
- Stay in the dark. If you have the luxury, retreat to a dark, quiet room when a migraine attack hits. Light and noise can make your headache worse.
Medications
If you’re like a lot of pregnant women, you may loathe the idea of taking medication. Nevertheless, migraine attacks can be intense, and sometimes the only thing that’ll snuff out the pain is medication.
Safe to take
According to the American Academy of Family Physicians (AAFP), drugs safe to use for migraine in pregnancy are:
- Acetaminophen. This is the generic name of the drug in Tylenol.
 It’s also sold under many other brand names.
It’s also sold under many other brand names. - Metoclopramide. This drug is often used to increase the speed of stomach emptying but also sometimes prescribed for migraine, especially when nausea is a side effect.
Possibly safe to take under certain circumstances
- Non-steroidal anti-inflammatory drugs (NSAIDS). These include ibuprofen (Advil) and naproxen (Aleve) and are only OK in the second trimester of pregnancy. Earlier than that there’s an increased chance of miscarriage; later than that there can be complications like bleeding.
- Triptans. These include Imitrex and Amerge. While their use during pregnancy is somewhat controversial — there’s not a lot of well-performed research proving their safety — many doctors think the benefits of their use outweigh any risks.
No-gos
- Full-dose aspirin. If you’re to kick it old school and pop some aspirin, don’t.
 Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine.
Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine. - Opioids. According to the Centers for Disease Control and Prevention (CDC), opioid use during pregnancy can lead to preterm birth, stillbirth, and certain birth defects. If an opioid is prescribed, it should be for limited use and carefully monitored by your doctor.
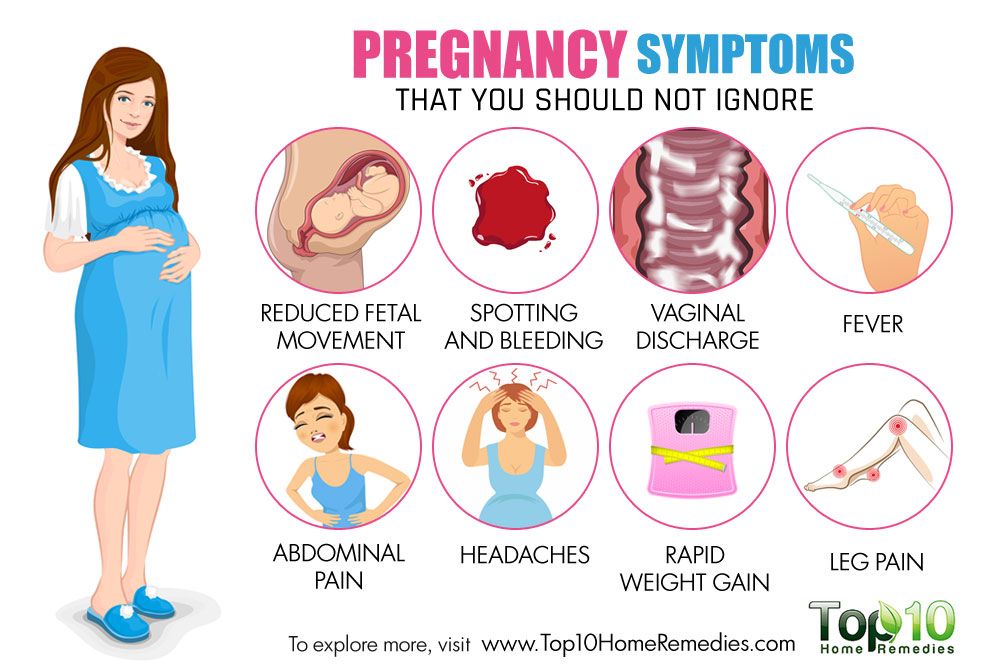
According to a 2019 study, pregnant women with migraine attacks have an increased risk of certain complications, including:
- having high blood pressure while pregnant, which may progress to preeclampsia
- delivering a low birth weight baby
- having a cesarean delivery
Older research shows that pregnant women with migraine have a higher risk of stroke. But — take a deep breath — experts say that the risk is still very low.
That’s the bad news — and it’s important to keep it in perspective. The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
- you have a first-time headache during pregnancy
- you have a severe headache
- you have high blood pressure and a headache
- you have a headache that won’t go away
- you have a headache accompanied by changes in your vision, such as blurry vision or sensitivity to light
Thanks to a more constant supply of hormones, most women get a break from migraine attacks during pregnancy. For an unlucky few, though, their migraine struggles continue. If you’re one of them, you’ll be more limited in what you can take and when you can take it, but treatment options are available.
Make a migraine management plan with your doctor early on in your pregnancy (and ideally, before), so you have tools at the ready.
Last medically reviewed on May 6, 2020
- Parenthood
- Pregnancy
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- About opioid use during pregnancy. (2020).
cdc.gov/pregnancy/opioids/basics.html - Bushnell CD, et al. (2009). Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. DOI:
10.1136/bmj.b664 - Experts comment on research suggesting links between migraine and stroke risk in pregnancy, as published in the BMJ. (2009).
sciencemediacentre.org/experts-comment-on-research-suggesting-links-between-migraine-and-stroke-risk-in-pregnancy-as-published-in-the-bmj-2/ - Mayans L, et al. (2018). Acute migraine headache: Treatment strategies.
aafp.org/afp/2018/0215/p243.html#sec-6 - Mayo Clinic Staff. (2017). Nutrition and healthy eating.
mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256 - Migraine.
 (2019).
(2019).
womenshealth.gov/a-z-topics/migraine - Migraine and pregnancy: What moms-to-be need to know. (2017).
americanmigrainefoundation.org/resource-library/understanding-migrainemigraine-and-pregnancy-what-moms-to-be-need-to-know/ - Migraine headaches during pregnancy. (n.d.).
stanfordchildrens.org/en/topic/default?id=migraine-headache-90-P02476 - Migraine headaches during pregnancy. (n.d.).
chop.edu/conditions-diseases/migraine-headaches-during-pregnancy - Pregnancy and breastfeeding: Key issues for women who have migraine and become pregnant. (n.d.).
migrainetrust.org/living-with-migraine/coping-managing/pregnancy-breastfeeding/ - Skajaa N, et al. (2019). Pregnancy, birth, neonatal, and postnatal neurological outcomes after pregnancy with migraine. DOI:
10.1111/head.13536 - Sleep and pregnancy. (2017).
familydoctor.org/getting-enough-sleep-pregnancy/ - Top 10 migraine triggers and how to deal with them.
 (2017).
(2017).
americanmigrainefoundation.org/resource-library/top-10-migraine-triggers-and-how-to-deal-with-them/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
May 6, 2020
Written By
Donna Christiano
Edited By
Jessica Jondle
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Copy Edited By
Christina Guzik, BA, MBA
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
related stories
5 Tips for Managing Pregnancy Challenges with Migraine
How Improving Sleep Can Prevent Migraine Attacks
Headache During Pregnancy: What You Need to Know
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
How Symptom Tracking Can Help You Find Relief from Migraine
Read this next
5 Tips for Managing Pregnancy Challenges with Migraine
Medically reviewed by Carolyn Kay, M.
 D.
D.Managing migraine throughout pregnancy can be a challenge, but there are options that can help limit attacks.
READ MORE
How Improving Sleep Can Prevent Migraine Attacks
Medically reviewed by Seunggu Han, M.D.
A lack of rest can trigger migraine attacks. Here are eight ways you can improve the quality of your sleep for migraine relief.
READ MORE
Headache During Pregnancy: What You Need to Know
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
Headache during pregnancy can be a painful problem. Your doctor can help determine what is causing your headaches and the most effective and safe…
READ MORE
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
Medically reviewed by Deena Kuruvilla, MD
During a migraine attack, sometimes the only thing you can do is make yourself as comfortable as possible while you ride out the neurological storm.
READ MORE
How Symptom Tracking Can Help You Find Relief from Migraine
Medically reviewed by Deena Kuruvilla, MD
Symptom tracking can be a helpful tool to better understand and manage your migraine pain.
READ MORE
What Are the Symptoms of Hyperovulation?
Hyperovulation has few symptoms, if any. It's typically diagnosed after an individual develops multiple pregnancies at once.
READ MORE
Pregnancy Friendly Recipe: Creamy White Chicken Chili with Greek Yogurt
This pregnancy-friendly spin on traditional chili is packed with the nutrients your body needs when you're expecting.
READ MORE
What You Should Know About Consuming Turmeric During Pregnancy
Consuming turmeric in pregnancy is a debated subject.
 We'll tell you if it's safe.
We'll tell you if it's safe.READ MORE
Pregnancy-Friendly Recipe: Herby Gruyère Frittata with Asparagus and Sweet Potatoes
Medically reviewed by Kathy W. Warwick, R.D., CDE
So easy and delicious. This frittata is high in protein and rich in essential nutrients your body needs to support a growing baby. Bonus: You can…
READ MORE
The Best Stretch Mark Creams and Belly Oils for Pregnancy in 2023
Stretch marks are easier to prevent than erase. If you're seeking a preventive, we've gathered a few of the best stretch mark creams for pregnancy.
READ MORE
Causes, Treatments, When to Worry
Migraine and Pregnancy: Causes, Treatments, When to Worry- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
We’re gonna give it to you straight: Pregnancy can mess with your head. And we’re not just talking about brain fog and forgetfulness. We’re also talking about headaches — migraine attacks, in particular.
Migraine is a type of headache that can cause intense throbbing, usually on one side of the head. Imagine having a 3-year-old living behind your eye socket and relentlessly pounding a drum. Each beat sends waves of agony through your skull. The pain can make natural childbirth seem like a walk in the park.
Well, almost. Maybe we shouldn’t go that far — but migraine attacks can be very painful.
Migraine affects about 30 million Americans, 75 percent of whom are women. While many women (up to 80 percent) find that their migraine attacks improve with pregnancy, others struggle on.
In fact, about 15 to 20 percent of pregnant women experience migraine. Women who have migraine attacks with “aura” — a neurological event that accompanies or proceeds migraine and can manifest as flashing lights, wavy lines, vision loss, and tingling or numbness — generally don’t see their headaches improve during pregnancy, according to experts.
So what’s a mom-to-be to do when a migraine attack strikes? What’s safe to take and what’s not? Is migraine ever dangerous enough that you should seek emergency medical care?
Most headaches during pregnancy — including migraine — are nothing to worry about. But that’s not to say that migraine attacks aren’t incredibly annoying, and, in some cases, dangerous for pregnant women and their babies.
Here’s everything you need to know about migraine during pregnancy so you can tackle the pain — head on.
Migraine headaches seem to have a genetic component, which means they tend to run in families. That said, there’s usually a triggering event that unleashes them. One of the most common triggers — at least for women — is fluctuating hormone levels, particularly the rise and fall of estrogen.
Moms-to-be who get migraine attacks tend to experience them most often in the first trimester of pregnancy, when hormone levels, including estrogen, haven’t yet stabilized. (In fact, headaches in general are an early pregnancy sign for a lot of women. )
)
An increase in blood volume, which is also common in the first trimester, can be an additional factor. As blood vessels in the brain expand to accommodate extra blood flow, they can press against sensitive nerve endings, causing pain.
Other common migraine triggers, whether you’re pregnant or not, include:
- Not getting enough sleep. The American Academy of Family Physicians recommends 8–10 hours per night when you’re pregnant. Sorry, Jimmy Fallon — we’ll catch you on the flip side.
- Stress.
- Not staying hydrated. According to the American Migraine Foundation, one-third of those who get migraine headaches say dehydration is a trigger. Pregnant women should aim for 10 cups (or 2.4 liters) of fluid daily. Try to drink them earlier in the day so sleep isn’t interrupted by nighttime visits to the bathroom.
- Certain foods. These include chocolate, aged cheeses, wines (not that you should be drinking any of those), and foods containing monosodium glutamate (MSG).

- Exposure to bright, intense light. Light-related triggers include sunlight and florescent lighting.
- Exposure to strong smells. Examples include paints, perfumes, and your toddler’s explosive diaper.
- Weather changes.
A migraine attack while you’re pregnant will look a lot like a migraine attack when you’re not pregnant. You’re apt to experience:
- throbbing head pain; usually it’s one-sided — behind one eye, for example — but it can occur all over
- nausea
- sensitivity to light, smells, sounds, and movement
- vomiting
When you’re pregnant, you have to think twice about everything you put into your body. Is it OK to have that second cup of coffee? What about a nibble of Brie? When you’re hit with the mother of all headaches — migraine — you want real relief quickly. But what are your options?
At-home remedies
These should be your first line of defense to avoid and treat migraine:
- Know your triggers.
 Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack.
Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack. - Hot/cold compresses. Figure out what eases migraine pain for you. A cold pack (wrapped in a towel) placed over your head can numb the pain; a heating pad around your neck can ease tension in tight muscles.
- Stay in the dark. If you have the luxury, retreat to a dark, quiet room when a migraine attack hits. Light and noise can make your headache worse.
Medications
If you’re like a lot of pregnant women, you may loathe the idea of taking medication. Nevertheless, migraine attacks can be intense, and sometimes the only thing that’ll snuff out the pain is medication.
Safe to take
According to the American Academy of Family Physicians (AAFP), drugs safe to use for migraine in pregnancy are:
- Acetaminophen. This is the generic name of the drug in Tylenol.
 It’s also sold under many other brand names.
It’s also sold under many other brand names. - Metoclopramide. This drug is often used to increase the speed of stomach emptying but also sometimes prescribed for migraine, especially when nausea is a side effect.
Possibly safe to take under certain circumstances
- Non-steroidal anti-inflammatory drugs (NSAIDS). These include ibuprofen (Advil) and naproxen (Aleve) and are only OK in the second trimester of pregnancy. Earlier than that there’s an increased chance of miscarriage; later than that there can be complications like bleeding.
- Triptans. These include Imitrex and Amerge. While their use during pregnancy is somewhat controversial — there’s not a lot of well-performed research proving their safety — many doctors think the benefits of their use outweigh any risks.
No-gos
- Full-dose aspirin. If you’re to kick it old school and pop some aspirin, don’t.
 Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine.
Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine. - Opioids. According to the Centers for Disease Control and Prevention (CDC), opioid use during pregnancy can lead to preterm birth, stillbirth, and certain birth defects. If an opioid is prescribed, it should be for limited use and carefully monitored by your doctor.
According to a 2019 study, pregnant women with migraine attacks have an increased risk of certain complications, including:
- having high blood pressure while pregnant, which may progress to preeclampsia
- delivering a low birth weight baby
- having a cesarean delivery
Older research shows that pregnant women with migraine have a higher risk of stroke. But — take a deep breath — experts say that the risk is still very low.
That’s the bad news — and it’s important to keep it in perspective. The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
- you have a first-time headache during pregnancy
- you have a severe headache
- you have high blood pressure and a headache
- you have a headache that won’t go away
- you have a headache accompanied by changes in your vision, such as blurry vision or sensitivity to light
Thanks to a more constant supply of hormones, most women get a break from migraine attacks during pregnancy. For an unlucky few, though, their migraine struggles continue. If you’re one of them, you’ll be more limited in what you can take and when you can take it, but treatment options are available.
Make a migraine management plan with your doctor early on in your pregnancy (and ideally, before), so you have tools at the ready.
Last medically reviewed on May 6, 2020
- Parenthood
- Pregnancy
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- About opioid use during pregnancy. (2020).
cdc.gov/pregnancy/opioids/basics.html - Bushnell CD, et al. (2009). Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. DOI:
10.1136/bmj.b664 - Experts comment on research suggesting links between migraine and stroke risk in pregnancy, as published in the BMJ. (2009).
sciencemediacentre.org/experts-comment-on-research-suggesting-links-between-migraine-and-stroke-risk-in-pregnancy-as-published-in-the-bmj-2/ - Mayans L, et al. (2018). Acute migraine headache: Treatment strategies.
aafp.org/afp/2018/0215/p243.html#sec-6 - Mayo Clinic Staff. (2017). Nutrition and healthy eating.
mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256 - Migraine.
 (2019).
(2019).
womenshealth.gov/a-z-topics/migraine - Migraine and pregnancy: What moms-to-be need to know. (2017).
americanmigrainefoundation.org/resource-library/understanding-migrainemigraine-and-pregnancy-what-moms-to-be-need-to-know/ - Migraine headaches during pregnancy. (n.d.).
stanfordchildrens.org/en/topic/default?id=migraine-headache-90-P02476 - Migraine headaches during pregnancy. (n.d.).
chop.edu/conditions-diseases/migraine-headaches-during-pregnancy - Pregnancy and breastfeeding: Key issues for women who have migraine and become pregnant. (n.d.).
migrainetrust.org/living-with-migraine/coping-managing/pregnancy-breastfeeding/ - Skajaa N, et al. (2019). Pregnancy, birth, neonatal, and postnatal neurological outcomes after pregnancy with migraine. DOI:
10.1111/head.13536 - Sleep and pregnancy. (2017).
familydoctor.org/getting-enough-sleep-pregnancy/ - Top 10 migraine triggers and how to deal with them.
 (2017).
(2017).
americanmigrainefoundation.org/resource-library/top-10-migraine-triggers-and-how-to-deal-with-them/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
May 6, 2020
Written By
Donna Christiano
Edited By
Jessica Jondle
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Copy Edited By
Christina Guzik, BA, MBA
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
related stories
5 Tips for Managing Pregnancy Challenges with Migraine
How Improving Sleep Can Prevent Migraine Attacks
Headache During Pregnancy: What You Need to Know
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
How Symptom Tracking Can Help You Find Relief from Migraine
Read this next
5 Tips for Managing Pregnancy Challenges with Migraine
Medically reviewed by Carolyn Kay, M.
 D.
D.Managing migraine throughout pregnancy can be a challenge, but there are options that can help limit attacks.
READ MORE
How Improving Sleep Can Prevent Migraine Attacks
Medically reviewed by Seunggu Han, M.D.
A lack of rest can trigger migraine attacks. Here are eight ways you can improve the quality of your sleep for migraine relief.
READ MORE
Headache During Pregnancy: What You Need to Know
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
Headache during pregnancy can be a painful problem. Your doctor can help determine what is causing your headaches and the most effective and safe…
READ MORE
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
Medically reviewed by Deena Kuruvilla, MD
During a migraine attack, sometimes the only thing you can do is make yourself as comfortable as possible while you ride out the neurological storm.

READ MORE
How Symptom Tracking Can Help You Find Relief from Migraine
Medically reviewed by Deena Kuruvilla, MD
Symptom tracking can be a helpful tool to better understand and manage your migraine pain.
READ MORE
What Are the Symptoms of Hyperovulation?
Hyperovulation has few symptoms, if any. It's typically diagnosed after an individual develops multiple pregnancies at once.
READ MORE
Pregnancy Friendly Recipe: Creamy White Chicken Chili with Greek Yogurt
This pregnancy-friendly spin on traditional chili is packed with the nutrients your body needs when you're expecting.
READ MORE
What You Should Know About Consuming Turmeric During Pregnancy
Consuming turmeric in pregnancy is a debated subject.
 We'll tell you if it's safe.
We'll tell you if it's safe.READ MORE
Pregnancy-Friendly Recipe: Herby Gruyère Frittata with Asparagus and Sweet Potatoes
Medically reviewed by Kathy W. Warwick, R.D., CDE
So easy and delicious. This frittata is high in protein and rich in essential nutrients your body needs to support a growing baby. Bonus: You can…
READ MORE
The Best Stretch Mark Creams and Belly Oils for Pregnancy in 2023
Stretch marks are easier to prevent than erase. If you're seeking a preventive, we've gathered a few of the best stretch mark creams for pregnancy.
READ MORE
Migraine during pregnancy: what to do
Migraine is a benign disease, it does not affect the course of pregnancy and fetal development. However, migraine and pregnancy is a combination that requires a responsible attitude.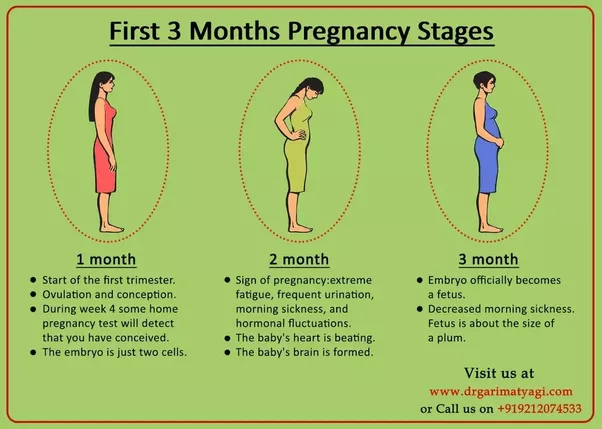 Especially with frequent migraines (more than 2 times a week) and migraines with aura, as:
Especially with frequent migraines (more than 2 times a week) and migraines with aura, as:
-
medicines approved for use, few,
-
and the approach to the treatment and prevention of migraine during this period is extremely individual: it depends on the frequency, severity and duration of headache, the degree of impact on life.
Our neurologist Daria Korobkova conducted a live broadcast on the clinic's Instagram account, where she told how migraine and pregnancy are connected, why attacks become more frequent or disappear, and answered subscribers' questions. The ether was saved, see “Air recording: migraine during pregnancy and GV.
We will tell about migraine during breastfeeding separately.
The statistics of clinical observations of migraine during pregnancy looks like this:
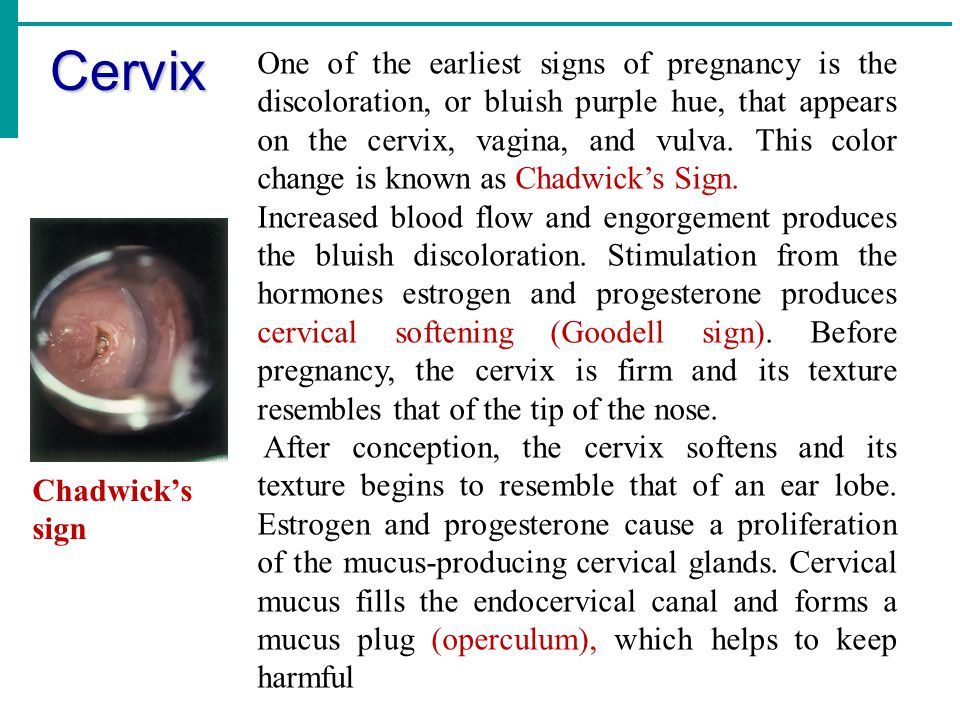
In 60-70% of pregnant women with migraine, headache attacks become less frequent, milder, or even completely disappear in the second and third trimesters. This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
In other women, migraines during pregnancy either remain unchanged or worsen. But as the duration of pregnancy increases, the proportion of such women gradually decreases:
If at the end of the first trimester the frequency and intensity of attacks persist, then it is most likely that migraine will disturb the woman throughout the entire period of pregnancy and after childbirth too.
How to manage migraine during pregnancy?
The main thing here is to learn how to control seizures and, if necessary, seek medical help.
-
Follow lifestyle advice:
-
get enough sleep;
-
drink enough fluids;
-
eat fractionally and without long breaks;
-
rest;
-
avoid stressful situations.
 This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
-
Keep a headache diary. This will help you take control of migraine triggers.
Yes, these simple recommendations are sometimes enough to make attacks less frequent! Pregnancy is a special state of a woman. If in other periods of life we do not take such recommendations so seriously, then in this situation it is worth trying to change the philosophy of life and attitude towards ourselves =)
How to relieve an attack?
-
Favor non-drug methods. Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
-
dry biscuits, ginger, or applesauce may help with nausea;
-
for dehydration - diluted juice or other liquid;
-
sleep, walking or breathing exercises can also help to cope;
-
If the attacks are severe, interfere with your life, then under the supervision of a specialist, you can resort to drug therapy.
PARACETAMOL is considered the safest and can be taken throughout pregnancy.
All other drugs have nuances. For example:
-
ibuprofen can be taken in the second trimester, and in the first trimester it is better to limit, in the third trimester the drug is contraindicated for use;
-
aspirin is prohibited in the 3rd trimester and is undesirable for taking in the first two, as it can cause extremely undesirable consequences;
-
It is strictly forbidden to use ergotamine and opioid analgesics;
-
triptans are not officially approved for use during pregnancy as no controlled studies have been conducted. However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
!Other than paracetamol, we do not recommend the use of any drug without a doctor's prescription.
When to see a doctor:
-
migraine occurred for the first time during pregnancy;
-
if migraine attacks suddenly become more frequent and stronger;
-
if the aura became longer or appeared for the first time;
-
if the headache is rapidly increasing and has an unusual character;
-
if the pressure rises during the headache.
Read more articles about headaches in our Telegram channel.
How do doctors diagnose headaches? Answering questions about Ajovi and Irinex If you are pregnant and suffer from migraines
which doctor should I contact and how to treat correctly?
- Home
- >Pregnancy
Of course, migraine or chronic tension headache is not a contraindication to pregnancy. And almost every woman, regardless of the presence of any chronic diseases, wants to become a mother. However, in order to survive the most comfortable period of pregnancy in the presence of chronic migraine or headache, it is necessary to prepare for this period in advance. The better your preparation is, the easier it will be for pregnancy, childbirth and postpartum feeding of the baby. Women with migraines are advised to stop all medications at least two weeks before conception and prepare to avoid severe attacks. Ideally, this stage of preparation takes from 6 to 12 months. Clinic of headache and vegetative disorders. Veina in Moscow specializes in the treatment of migraines, headaches and other types of pain syndrome. For a long time of work under the supervision of our doctors, many pregnancies have come and gone successfully, even in difficult patients. Effective assistance was provided to expectant mothers with such diseases as:
And almost every woman, regardless of the presence of any chronic diseases, wants to become a mother. However, in order to survive the most comfortable period of pregnancy in the presence of chronic migraine or headache, it is necessary to prepare for this period in advance. The better your preparation is, the easier it will be for pregnancy, childbirth and postpartum feeding of the baby. Women with migraines are advised to stop all medications at least two weeks before conception and prepare to avoid severe attacks. Ideally, this stage of preparation takes from 6 to 12 months. Clinic of headache and vegetative disorders. Veina in Moscow specializes in the treatment of migraines, headaches and other types of pain syndrome. For a long time of work under the supervision of our doctors, many pregnancies have come and gone successfully, even in difficult patients. Effective assistance was provided to expectant mothers with such diseases as:
- migraine,
- headache,
- panic attacks and anxiety during pregnancy,
- insomnia,
- attacks of vegetovascular dystonia during pregnancy,
- pain in the neck, back, lower back during pregnancy,
- diseases during pregnancy.

Pregnancy and breastfeeding has many restrictions in taking medicines. However, some schemes for taking drugs to relieve headaches and migraines during pregnancy still exist. It is better to clarify and select them in advance together with the attending physician, and also to develop a clear algorithm of actions in case of an impending attack. Enduring pain during pregnancy with migraine is still not recommended, with the exception of the first trimester and the last weeks of the third trimester. But most importantly, non-drug methods of relieving headaches come to the aid of pregnant women, such as:
- biofeedback therapy,
- manual therapy,
- massage,
- acupuncture,
- psychotherapy.
botulinum therapy - prevention of migraine and headache during pregnancy
The most interesting and promising method of treating headache during pregnancy and migraine is botulinum therapy. The essence of this method is prevention.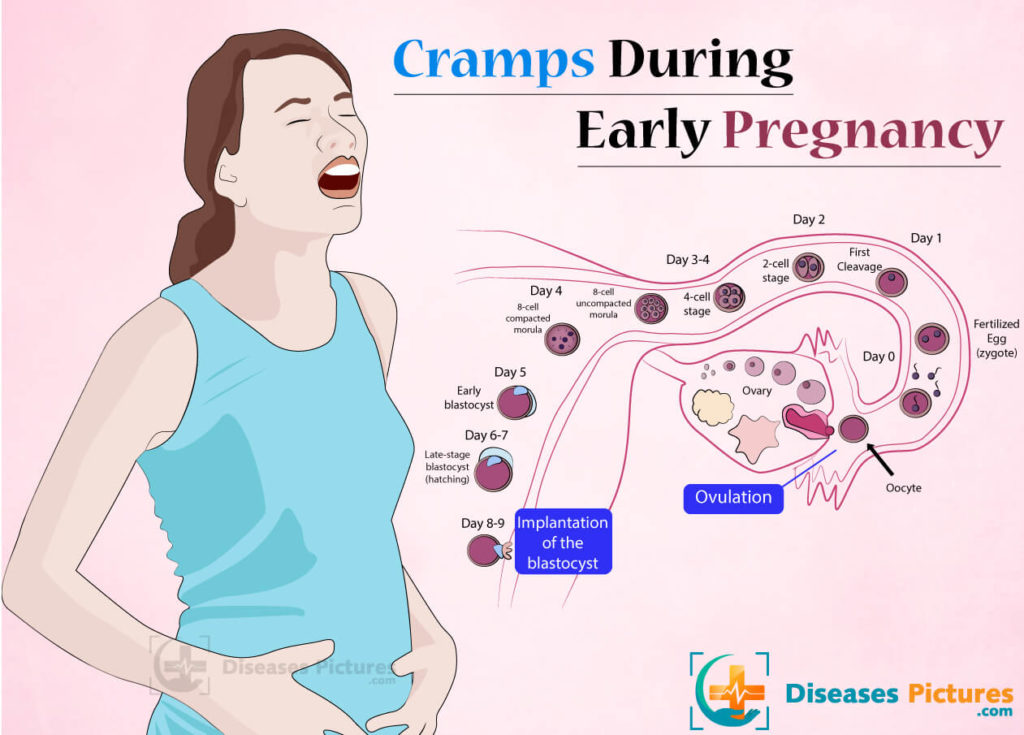 Before becoming pregnant, a woman is given injections of one of the botulinum toxin preparations (multiple injections during the year are possible). Such prophylactic treatment can significantly reduce the frequency and intensity of migraine attacks for up to six months. Thus, it is possible to minimize the frequency and severity of attacks in the most important first trimester. Then, when the laying of the organs and systems of the baby occurs, it is risky to take painkillers. To select the optimal timing and methods of treating your type of headache, it is best to contact a headache specialist a year, six months before the planned pregnancy.
Before becoming pregnant, a woman is given injections of one of the botulinum toxin preparations (multiple injections during the year are possible). Such prophylactic treatment can significantly reduce the frequency and intensity of migraine attacks for up to six months. Thus, it is possible to minimize the frequency and severity of attacks in the most important first trimester. Then, when the laying of the organs and systems of the baby occurs, it is risky to take painkillers. To select the optimal timing and methods of treating your type of headache, it is best to contact a headache specialist a year, six months before the planned pregnancy.
Authorized medicines for migraine and headache
Still, migraine and headache often take pregnant women by surprise. What painkillers are still allowed for pregnant women? During the entire period of pregnancy, you can take paracetamol at a dose of 325-500 mg up to 4 times a day. Caffeine is also allowed. So, you can drink migraine, panadol extra or solpadein fast.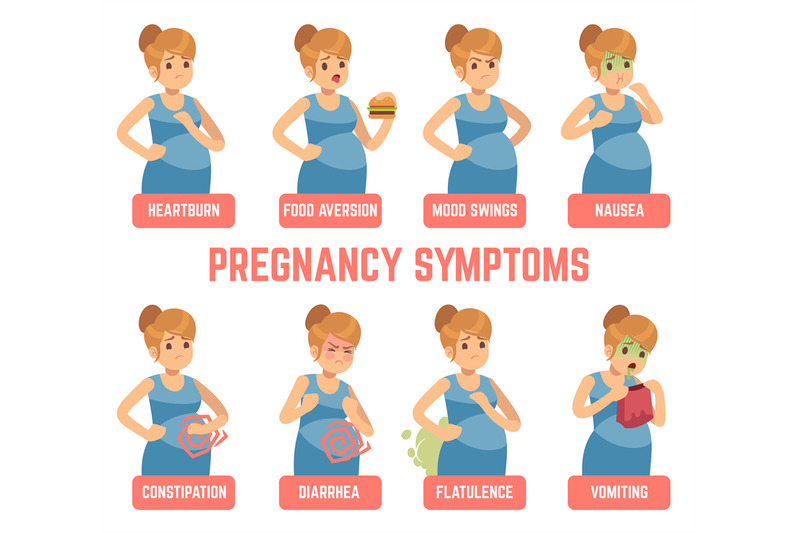 Of course, these painkillers are not very strong. And at the usual time, taking them to relieve a migraine attack is not recommended. But during pregnancy, they can be drunk absolutely fearlessly. It is effective to take aspirin, naproxen and ibuprofen during pregnancy for migraine. But they can be drunk without fear only during the first and second trimesters. When planning a pregnancy, they are undesirable. And in the third trimester it is generally prohibited.
Of course, these painkillers are not very strong. And at the usual time, taking them to relieve a migraine attack is not recommended. But during pregnancy, they can be drunk absolutely fearlessly. It is effective to take aspirin, naproxen and ibuprofen during pregnancy for migraine. But they can be drunk without fear only during the first and second trimesters. When planning a pregnancy, they are undesirable. And in the third trimester it is generally prohibited.
DRUGS FOR MIGRAINES AND HEADACHES IN PREGNANCY
There are drugs that are strictly prohibited during pregnancy. These are painkillers with phenobarbital, codeine, old tranquilizers like phenazepam and ergotamines.
Headache and migraine treatment during pregnancy
Dear expectant mothers! If you suffer from migraines, chronic headaches or other types of pain syndrome, experience a feeling of constant anxiety, panic attacks, we invite you to spend your pregnancy under the supervision of our specialists! Our doctors have harmless, but effective methods of treatment.