Maternal birth trauma
Birth trauma (emotional) | Pregnancy Birth and Baby
Birth trauma (emotional) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is birth trauma?
'Birth trauma' is distress experienced by a mother during or after childbirth. While trauma can be physical, it is often emotional and psychological.
Birth trauma is not just about what happened during labour and the birth. It can also refer to how you, as the mother, are left feeling afterwards. Sometimes the effects of birth trauma can emerge and continue for some time after you've given birth.
At the time of birth, you may have felt fearful, helpless or unheard. After the birth, it's possible to feel shocked, guilty or numb and even experience panic attacks or anxiety.
If you notice any of these symptoms, you may be experiencing birth trauma. If so, you are certainly not alone. It's been estimated that up to 1 in 3 women who give birth may experience birth trauma.
Many women find the experience of childbirth emotionally traumatic. Birth trauma can't always be prevented, but there are things you can do to reduce your risk. If you are experiencing any signs of trauma, support and treatment are available.
What are the risk factors for birth trauma?
There are many factors that can contribute to birth trauma. These include:
- your childbirth experience not going to plan, or not matching your expectations
- having a difficult labour or experiencing labour complications
- needing intervention during labour, such as an assisted delivery (using forceps or ventouse) or an emergency caesarean
- you or your baby suffering birth injury
- your baby needing medical attention after the birth
- stillbirth or neonatal death
- not receiving the care or support you needed at the time of birth, or afterwards
- previous birth trauma
- a tendency to experience anxiety
A woman may be especially at risk of trauma during pregnancy, birth and after the birth if she experienced trauma earlier in her life. This can include domestic violence, childhood sexual abuse, rape and migration-related trauma.
This can include domestic violence, childhood sexual abuse, rape and migration-related trauma.
Can birth trauma be prevented?
Childbirth doesn't always go to plan. Many women who experience birth trauma are unable to avoid it because the risk factors (for example, a history of trauma) are beyond their control.
However, there are ways to help reduce the risk of birth trauma:
- Prepare for childbirth: Antenatal classes, for example, help you know what to expect and your options.
- Try to have realistic expectations: There is no 'right' way to give birth. Things don't always go to plan and some things are beyond your control.
- Try to keep an open mind: No one can predict what will or won't happen during pregnancy and birth.
- Establish a support network: Surround yourself with people who can support you.
- Seek mental health support: If you are prone to anxiety or depression, or if you had a difficult pregnancy or labour, counselling can help you come to terms with what happened.

How is birth trauma treated?
If you think you could be experiencing emotional trauma, it's very important to seek help as early as possible — which benefits both you and your family.
Some psychological symptoms, including the 'baby blues', are very common around the time of birth. But if you still feel distressed 2 or more weeks after the birth, you could have postnatal depression or anxiety.
In some cases, not getting treatment for birth trauma can lead to post-traumatic stress disorder (PTSD). One Australian study found that more than 1 in 20 mothers may show signs of PTSD at 12 weeks after giving birth.
It may help you to:
- talk to a midwife immediately after the birth about your experience
- talk to your doctor, midwife or maternal child health nurse at any stage about how you feel
- ask for practical and emotional support from friends and family
- use self-help measures, such as exercise and mindfulness
If needed, therapy or medicines can also be used as treatment. Your doctor is the best person to advise you on this.
Your doctor is the best person to advise you on this.
Where can I go for more support and advice?
As well as asking your doctor or nurse for advice, you can get help and information from:
- Pregnancy, Birth and Baby — call 1800 882 436 to speak to a maternal child health nurse (7 days a week, 7am to midnight AEST).
- The Australian Birth Trauma Association offers advice, resources and a peer-to-peer support service.
- The Centre of Perinatal Excellence (COPE) provides information and a list of support services.
- Perinatal Anxiety & Depression Australia (PANDA) — call 1300 726 306 to speak with a counsellor (Mon to Fri, 9am to 7.30pm AEST).
Sources:
Australasian Birth Trauma Association (What is birth trauma), Australasian Birth Trauma Association (What is psychological birth trauma), Centre of Perinatal Excellence (When things don’t go to plan), Perinatal Anxiety & Depression Australia (Childbirth trauma), SA Health (South Australian Perinatal Practice Guideline - Managing women in distress after a traumatic birth experience), Centre of Perinatal Excellence (Preparing for birth), Centre of Perinatal Excellence (Recovering from a traumatic birth), Psychological Medicine (A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events), Perinatal Anxiety & Depression Australia (Complicated births), Perinatal Anxiety & Depression Australia (During pregnancy)Learn more here about the development and quality assurance of healthdirect content.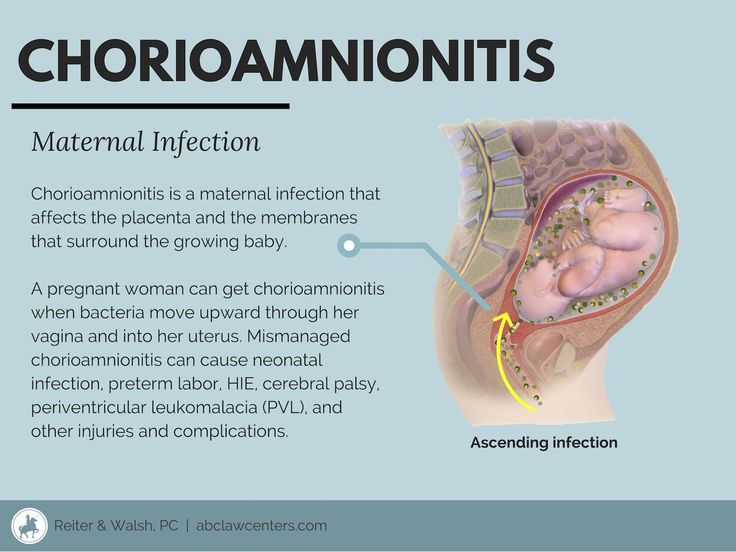
Last reviewed: May 2021
Back To Top
Related pages
- Mum's first few days after giving birth
- Your physical and emotional wellbeing
- Baby blues
- Birth injury (to the mother)
- Birth injury (to the baby)
Need more information?
Psychological Trauma - Birth Trauma
Read more on Australasian Birth Trauma Association website
Physical Trauma - Birth Trauma
For many women who have suffered from physical trauma as a result of childbirth, and who are struggling to cope, is it vital that healthcare providers
Read more on Australasian Birth Trauma Association website
What is Birth Trauma? - Birth Trauma
The delivery of a baby is a positive event for many women, but for some it can be a mixed experience or even very negative, resulting in physical and/or
Read more on Australasian Birth Trauma Association website
Considerations for birthing after birth trauma - Birth Trauma
In this post we consider some important points when making decisions about birthing after a birth trauma experience.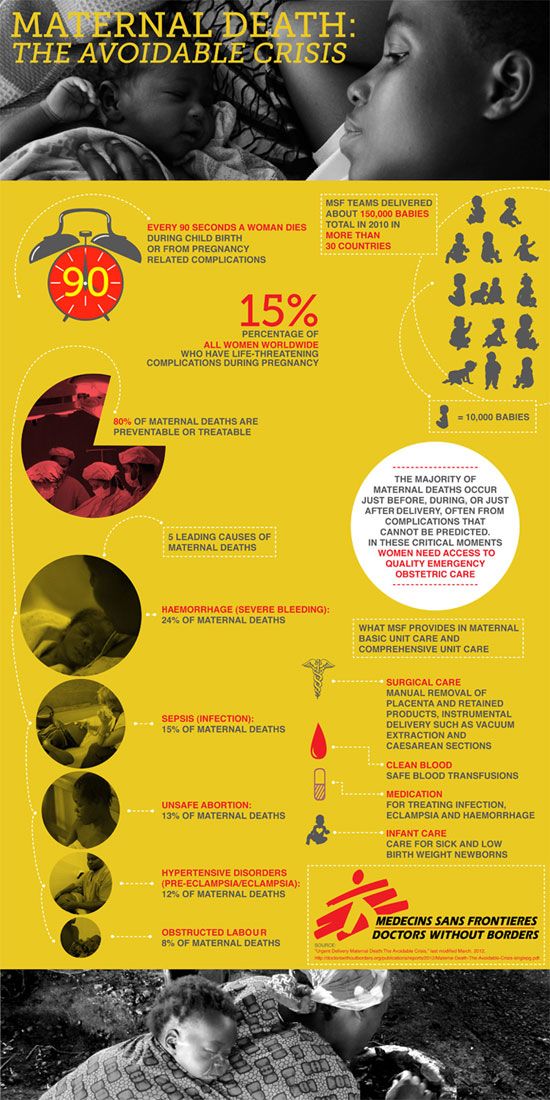
Read more on Australasian Birth Trauma Association website
Childbirth trauma and recovery | PANDA
While many pregnant women and their partners know birthing their baby will be hard work, very few expect labour and childbirth could be complicated.
Read more on Perinatal Anxiety and Depression Australia (PANDA) website
Family & Friends - Birth Trauma
If you are reading this then you may have someone close to you that has been impacted by a difficult birth experience, be it a partner, loved one or someone
Read more on Australasian Birth Trauma Association website
Early Postnatal - Birth Trauma
The early postnatal period is a time of emotional change for most women. Some women may experience distress or symptoms of depression at this time if they
Some women may experience distress or symptoms of depression at this time if they
Read more on Australasian Birth Trauma Association website
thinknatal - Birth Trauma
We have developed THINKNATALTM, a series of educational resources aimed at providing support and information on a variety of topics that are often excluded or
Read more on Australasian Birth Trauma Association website
Caesarean Section - Birth Trauma
Being abdominal surgery, pain in the early months is very common after a caesarean section (C-section) and needs to be managed with rest, pain relief, and
Read more on Australasian Birth Trauma Association website
Information for Parents (to be) - Birth Trauma
First we want you to know that we are with you and we are here for you. You are not alone.Times are challenging, staying at home, working from home, home
You are not alone.Times are challenging, staying at home, working from home, home
Read more on Australasian Birth Trauma Association website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.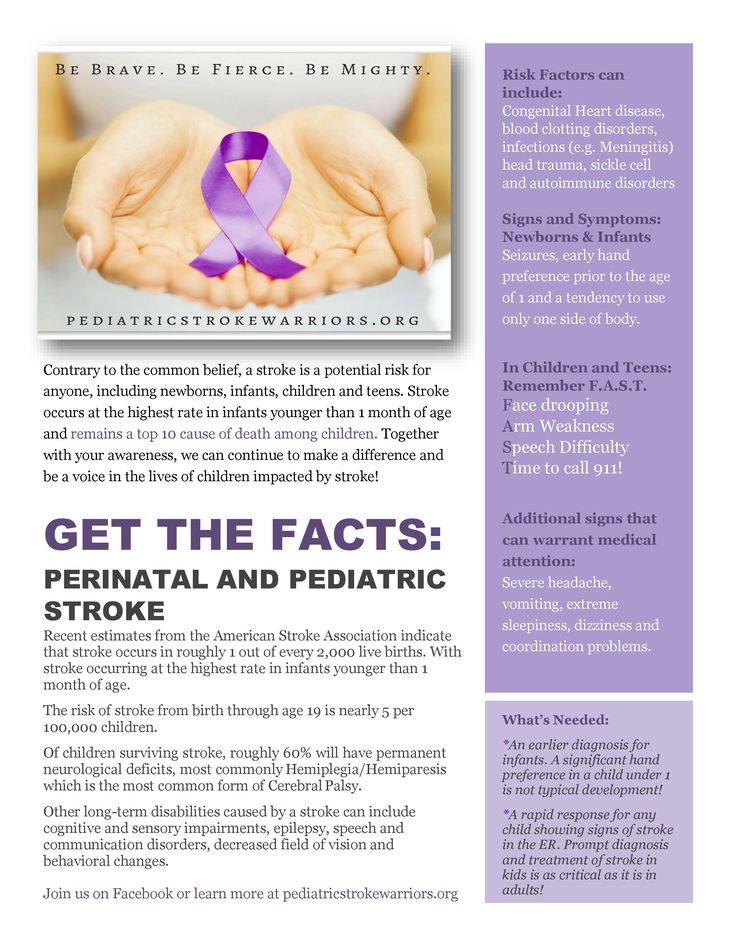
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Birth injury (to the mother)
Birth injury (to the mother) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is birth injury?
Birth injuries are physical injuries experienced during childbirth, and can affect either the mother or the baby.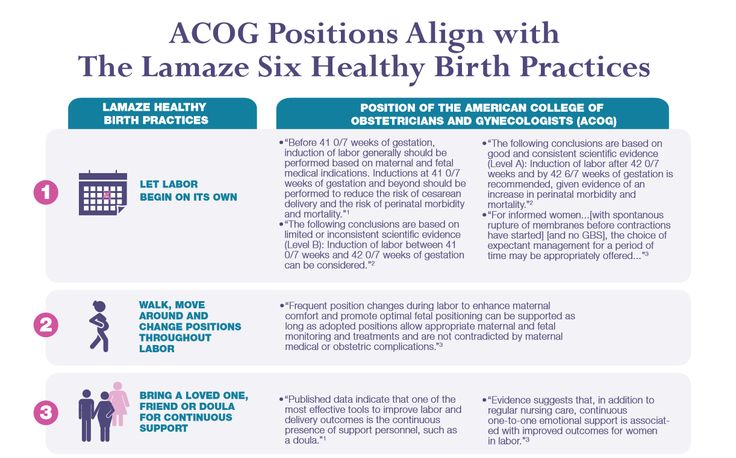 In newborn babies, a birth injury (often called 'neonatal birth trauma') can include many things, from bruising to a broken bone.
In newborn babies, a birth injury (often called 'neonatal birth trauma') can include many things, from bruising to a broken bone.
In mothers, birth injuries range from tearing in the vaginal area to damage to the pelvic floor.
Birth injuries in mothers typically fall into 2 main categories:
Injuries to the perineal area
- Perineal tears and episiotomy — around 3 in 4 women who give birth vaginally experience 'perineal trauma' (a tear or surgical cut to the area between the vagina and anus).
- Nerve damage — occasionally, nerves in the perineal area can get damaged during childbirth, which can lead to a painful condition called pudendal neuralgia.
- Haemorrhoids (piles) — these are swollen veins around the anus that you might feel as lumps. While they can be painful or itchy, they are usually not serious.
Injuries to the pelvic floor
- Muscle damage — the 'pelvic floor' is a group of muscles inside the pelvis that helps hold the uterus, bladder and bowel in place.
 In up to half of all women who give birth vaginally, there are permanent changes to the pelvic floor due to over-stretching or tearing (avulsion).
In up to half of all women who give birth vaginally, there are permanent changes to the pelvic floor due to over-stretching or tearing (avulsion). - Pelvic organ prolapse — if the pelvic muscles are damaged or weakened, the organs inside the pelvis can drop down towards the vagina, causing bladder and bowel problems.
While these birth injuries are physical, many mothers can experience emotional or psychological distress — before, during or after the birth. This is known as birth trauma. There are ways to decrease your risk of birth trauma, and both treatment and support are available.
What causes birth injury?
If you suffer a birth injury, the cause was most likely something out of your control.
Some of the main risk factors for birth injury include:
- the position of the baby, such as in a breech birth
- having a large baby (over 4kg)
- having a very quick or very long labour
- labour complications
- assisted delivery using forceps or ventouse (vacuum)
- having a small or unusually shaped pelvis
Can birth injury be prevented?
Although it's often not possible to prevent birth injury, there are some things you can do during pregnancy to reduce your risk:
- Exercise regularly (make sure you do pregnancy safe exercise).

- Strengthen your pelvic muscles with daily pelvic floor exercises.
- Avoid getting constipated or straining on the toilet, as this can weaken your pelvic muscles.
- Giving birth by caesarean could prevent some birth injuries, but this is major surgery so carries health risks of its own.
How is birth injury treated?
Some birth injuries are minor and may heal on their own — for example, a minor perineal tear or graze. Other injuries need treatment at the time, such as a deeper tear that needs stitches. You may also need some pain relief.
If you had a more serious birth injury, such as a significant tear or damage to the muscles of the pelvic floor, treatment may include physiotherapy and exercises to strengthen your pelvic floor muscles. Some women may need to use pessaries in their vagina or surgery to repair a prolapse.
Sometimes, signs of pelvic floor damage or prolapse are not detected and treated until much later.
If you have had a birth injury, you may be at more risk of it happening again with your next baby. Your doctor will talk to you about whether you should consider a planned caesarean section next time.
Your doctor will talk to you about whether you should consider a planned caesarean section next time.
If you experience any ongoing symptoms, such as pelvic pain or bladder and bowel problems, you should see your doctor.
Resources and support
- Talk to your doctor, midwife or obstetrician.
- You can call Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse (7 days a week, 7am to midnight AET).
- The Continence Foundation of Australia offers information and support to people with bowel and bladder problems. You can call the helpline on 1800 33 00 66 between 8am and 8pm (AEST), Monday to Friday.
- Visit the Australasian Birth Trauma Association website for information and support, including peer-to-peer support.
- Visit the PANDA (Perinatal Anxiety & Depression Australia) website for information and support after a traumatic birth. You can call the PANDA national helpline on 1300 726 306 ((Mon to Fri, 9am to 7.
 30pm AEST).
30pm AEST).
Sources:
Mater Mothers Hospital (Labour and birth - assisted vaginal birth), Medical Hypotheses (The significance of incomplete skull fracture in the birth injury), Stanford Children's Health (Birth injury), Australian Commission on Safety and Quality in Health Care (Neonatal birth trauma), Cerebral Palsy Alliance Research Foundation (What causes cerebral palsy), Medscape (Birth trauma), Merck Manual (Birth injuries in newborns), Australian Institute of Health and Welfare (Australia's mothers and babies data visualisations perineal status), PANDA (Childbirth trauma)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Related pages
- When birth doesn't go to plan
- Birth injury (to the baby)
- Birth trauma (emotional)
Need more information?
Psychological Trauma - Birth Trauma
Read more on Australasian Birth Trauma Association website
What is Birth Trauma? - Birth Trauma
The delivery of a baby is a positive event for many women, but for some it can be a mixed experience or even very negative, resulting in physical and/or
Read more on Australasian Birth Trauma Association website
Birth trauma (emotional)
Birth trauma affects many women. But there are ways to reduce your risk of an emotionally traumatic childbirth, while support and treatment are available if you experience symptoms.
But there are ways to reduce your risk of an emotionally traumatic childbirth, while support and treatment are available if you experience symptoms.
Read more on Pregnancy, Birth & Baby website
Early Postnatal - Birth Trauma
The early postnatal period is a time of emotional change for most women. Some women may experience distress or symptoms of depression at this time if they
Read more on Australasian Birth Trauma Association website
Family & Friends - Birth Trauma
If you are reading this then you may have someone close to you that has been impacted by a difficult birth experience, be it a partner, loved one or someone
Read more on Australasian Birth Trauma Association website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Birth and beyond - Ngala
Exciting times are ahead!Birth comes after lots of anticipation and preparation
Read more on Ngala website
Looking after your body after having a baby
Over the last 9 months, your body has had to change to accommodate your growing baby and preparing to give birth.
Read more on Pregnancy, Birth & Baby website
Bladder weakness after birth
Leaking urine after childbirth is very common. It can be embarrassing and inconvenient, but there are ways to improve bladder weakness.
Read more on Pregnancy, Birth & Baby website
Birth injury (to the baby)
While some babies do experience birth injury, giving birth in Australia is very safe. Most birth injuries to babies are temporary, and in many cases treatment is available.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.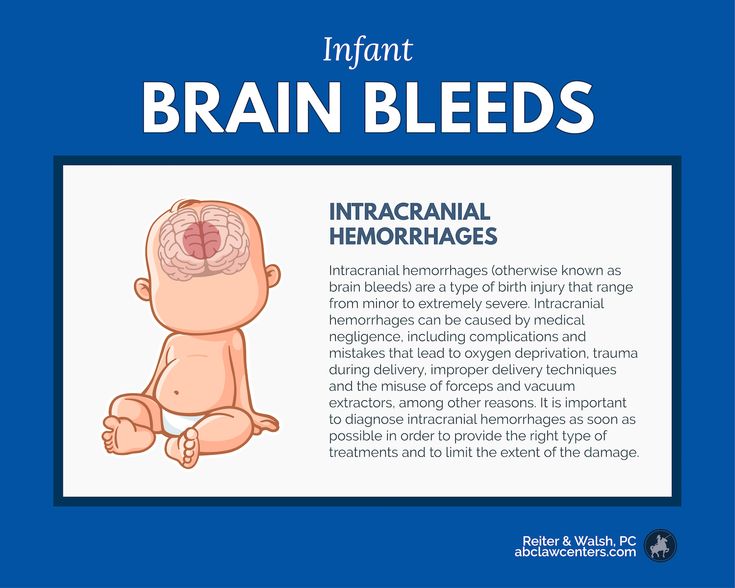
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Birth trauma. What is birth trauma?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Birth trauma is a collective concept that includes various damage to tissues and organs of a woman in labor or a newborn, caused by the action of birth forces. Among the birth injuries of the mother, there are hematomas, ruptures of the vulva, perineum and vagina, damage to the uterus, the formation of urogenital and enterogenital fistulas, and deformities of the pelvic bones. Many birth injuries can be life threatening. Diagnosis of birth injuries is based on external examination, gynecological examination, instrumental methods. Treatment of maternal birth injuries, as a rule, requires emergency surgical assistance and the involvement of narrow specialists (urologists, proctologists, traumatologists). nine0006
ICD-10
P10-P15 Birth trauma
- Common causes of maternal birth injuries
- Birth injuries of the vulva and vagina
- Vulvar and vaginal hematomas
- Tears of the vulva and vagina
- Birth injuries of the perineum
- Perineal tear symptoms
- Diagnosis and treatment of perineal tears
- Birth trauma of the uterus
- Uterine ruptures
- Classification of uterine ruptures
- Symptoms of uterine rupture
- Uterine rupture emergency
- Cervical tears
- Symptoms of cervical rupture
- Diagnosis and treatment of cervical tears
- Other birth injuries
- Uterine eversion
- Sprains and ruptures of the pelvic joints
- Urogenital and rectovaginal fistulas
nine0015 Prevention of birth injuries - Prices for treatment
General
Childbirth is a difficult test for the newborn fetus and mother. Therefore, after the birth of a child, experts often state the presence of various birth injuries and postpartum disorders in a woman in labor and a newborn. In obstetrics and gynecology, maternal and child birth injuries are distinguished. Birth injuries of a newborn include damage to the peripheral and central nervous systems of various nature and severity, injuries to bones and soft tissues, and internal organs. As part of this review, the main birth injuries that occur in women will be considered. nine0006
Therefore, after the birth of a child, experts often state the presence of various birth injuries and postpartum disorders in a woman in labor and a newborn. In obstetrics and gynecology, maternal and child birth injuries are distinguished. Birth injuries of a newborn include damage to the peripheral and central nervous systems of various nature and severity, injuries to bones and soft tissues, and internal organs. As part of this review, the main birth injuries that occur in women will be considered. nine0006
Significant stretching of the mother's birth canal during childbirth often leads to their damage. These injuries - birth injuries, can be superficial, non-rough in nature (for example, abrasions, cracks) and heal on their own in the early postpartum period, and remain unrecognized. In some cases, birth injuries are so significant that they can lead to serious postpartum complications, disability and even death of a woman. Among birth injuries of the mother there are hematomas; ruptures of the vulva, perineum, vagina, body and cervix; inversion of the uterus; sprains and ruptures of the joints of the pelvis; urogenital and enterogenital fistulas. nine0006
nine0006
Birth injury
Common causes of maternal birth injuries
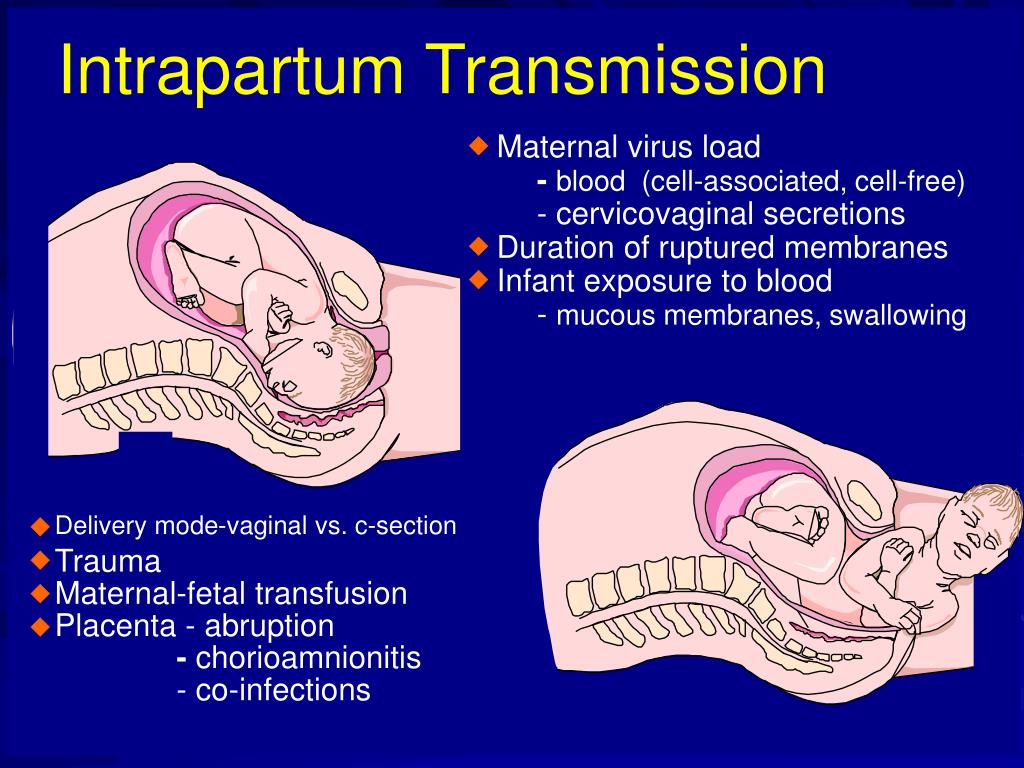
The variety of variants of maternal birth injuries can be caused by various mechanical and histopathic causes. The mechanical factors in the occurrence of birth injuries include violent or discoordinated labor activity, the provision of operational aids during childbirth (the application of forceps, vacuum extraction of the fetus, manual separation of the placenta, fruit-destroying operations), excessive labor stimulation, irrational management of the straining period, inadequate protection of the perineum, etc. e. Post-term pregnancy, transverse position of the fetus, breech presentation of the fetus, premature birth, narrow pelvis, polyhydramnios, multiple pregnancy, placenta previa can contribute to birth injuries. nine0006
Histopathic causes of birth injuries are due to a burdened obstetric and gynecological history of the woman in labor. So, the causes of birth injuries of the uterus can be surgical interventions in the past (caesarean section, metroplasty, conservative myomectomy, complete or partial perforation of the uterus during abortion, etc.), which lead to the formation of a scar on the uterus and, as a result, inadequate contractility of the myometrium in childbirth.
So, the causes of birth injuries of the uterus can be surgical interventions in the past (caesarean section, metroplasty, conservative myomectomy, complete or partial perforation of the uterus during abortion, etc.), which lead to the formation of a scar on the uterus and, as a result, inadequate contractility of the myometrium in childbirth.
The likelihood of birth canal injuries increases in the presence of anatomical defects of the genitals (intrauterine septum, uterine hypoplasia, bicornuate uterus), cervical rigidity in late primiparas, uterine hyperanteflexia. Also, birth injuries can be caused by cervicitis, adenomyosis, endometritis, colpitis, cystic drift and chorionepithelioma. In the etiopathogenesis of birth trauma, there are often several aggravating factors. nine0006
Birth injuries of the vulva and vagina
Hematomas of the vulva and vagina
Hematomas of the vulva and vagina are caused by stretching and rupture of blood vessels in the thickness of the soft tissues with intact integuments. In this case, the blood pouring out of the damaged vessel accumulates in the fiber and under the mucosa, forming a hematoma.
In this case, the blood pouring out of the damaged vessel accumulates in the fiber and under the mucosa, forming a hematoma.
With birth injuries of soft tissues in the vulva and vagina, a blue-purple tumor appears, the size of which can reach the head of a newborn. Hematomas cause a feeling of discomfort (bursting, pressure), soreness. Large progressive hematomas extend to the pelvic tissue and may be accompanied by the development of hemorrhagic shock. Small hemorrhages usually resolve on their own; with large hematomas, their suppuration is possible. Recognition of birth injuries of soft tissues occurs during external examination and gynecological examination. nine0006
Surgical tactics are indicated for large (more than 4-5 cm in diameter) and progressive hematomas. At the same time, the tissues above the hematoma are opened, the accumulated blood is removed, the bleeding vessel is isolated and tied up, the wound is sewn up tightly. With an infected hematoma, the wound is not sutured. With a progressive hematoma, abdominotomy is sometimes required.
With a progressive hematoma, abdominotomy is sometimes required.
Tears of the vulva and vagina
Birth injuries of the vulva and vagina are most common in primiparas. Mild cracks and tears are usually asymptomatic and do not require intervention. Tears in the clitoris, urethra, vagina are accompanied by the formation of hematomas, massive bleeding, hemorrhagic shock. nine0006
Birth injuries of the vagina can be spontaneous and violent. In the latter case, the causes of birth injuries are various obstetric operations. Vaginal tears can occur in its upper, middle, or lower sections; be superficial or deep, reaching the tissue of the small pelvis and abdominal cavity.
Birth injuries of the tissues of the vulva are detected during examination. To exclude internal tears, it is necessary to examine the walls of the vagina with the help of mirrors. nine0006
Treatment of birth injuries of the vulva and vagina is exclusively surgical.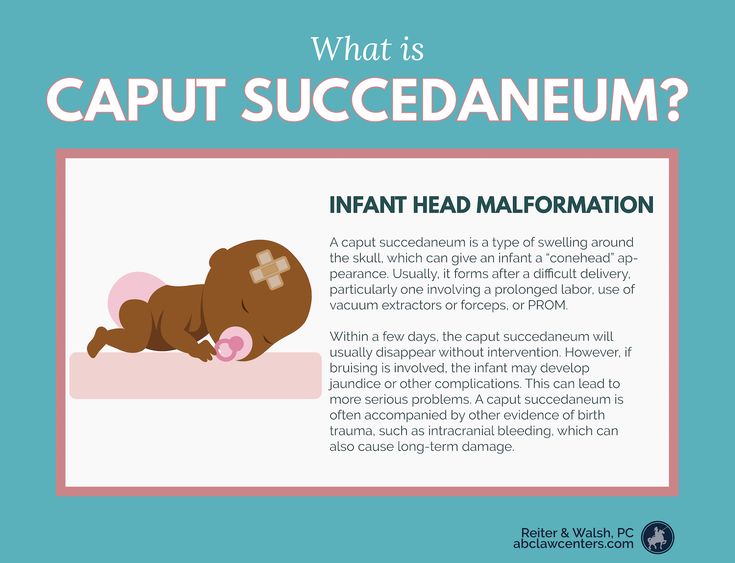 After catheterization of the bladder with a metal catheter, the tears are sutured with catgut sutures. In the postoperative period, antimicrobial therapy and vaginal baths with antiseptics are prescribed. Unrecognized vaginal tears may heal uncomplicated or become infected. Deep tears can subsequently lead to secondary vaginal atresia, necessitating vaginoplasty. nine0006
After catheterization of the bladder with a metal catheter, the tears are sutured with catgut sutures. In the postoperative period, antimicrobial therapy and vaginal baths with antiseptics are prescribed. Unrecognized vaginal tears may heal uncomplicated or become infected. Deep tears can subsequently lead to secondary vaginal atresia, necessitating vaginoplasty. nine0006
Birth injuries of the perineum
Birth injuries of the perineum include violent or spontaneous ruptures of the skin, fiber and muscle-fascial tissues of the pelvic floor. Birth injuries of the perineum occur in 7-15% of women in labor, and much more often in primiparas. Perineal ruptures are often combined with birth injuries of the vagina.
Protrusion and cyanosis of the tissues of the pelvic floor, swelling and luster of tissues, cracks testify to the threat of birth injury of the perineum. If there is a threat of birth injury of the perineum, they resort to a median dissection of tissues - perineotomy or a lateral incision - episiotomy, followed by suturing. nine0006
nine0006
Perineal tear symptoms
Depending on the depth of the birth injury, 3 degrees of perineal ruptures are distinguished.
With a rupture of the perineum of the 1st degree, the integrity of the skin and subcutaneous tissue in the region of the posterior commissure is violated. II degree of perineal rupture is characterized by additional injuries of the pelvic floor muscles (including the muscles that lift the anus), the back or side walls of the vagina. With a birth injury of the perineum of the III degree, the rupture of the external sphincter, and sometimes the walls of the rectum, joins the above injuries. nine0006
Birth injuries of the perineum are manifested by a violation of the integrity of tissues and bleeding.
Diagnosis and treatment of perineal tears
Birth injuries of the perineum are recognized after the birth of the placenta. To do this, the obstetrician-gynecologist spreads the genital gap, examines the walls of the vagina and the cervix. More often damage to the perineum during childbirth occurs not along the midline, but extramedially, but there is also a central gap between the posterior commissure and the muscle that lifts the anus. nine0006
More often damage to the perineum during childbirth occurs not along the midline, but extramedially, but there is also a central gap between the posterior commissure and the muscle that lifts the anus. nine0006
Restoration of the integrity of the tissues of the perineum is performed by suturing under local infiltration or general anesthesia. Separate catgut sutures are placed on the damaged walls of the vagina and rectum, pelvic floor muscles, subcutaneous tissue and perineal skin. In the postpartum period, sutures are processed, a thorough toilet of the wound after each defecation and urination, and constipation is prevented.
Birth injuries of the uterus
Uterine ruptures
Uterine rupture is one of the most severe birth injuries and occurs in 0.015% -0.1% of the total number of births. When the uterus ruptures, the integrity of the walls of its body is violated. The lethality of women with birth trauma of the uterus from shock, anemia and septic complications reaches 3-4%. Many women who have had uterine rupture develop hypoxic encephalopathy later on. Fetal death in uterine rupture is close to 100%. nine0006
Many women who have had uterine rupture develop hypoxic encephalopathy later on. Fetal death in uterine rupture is close to 100%. nine0006
Classification of uterine ruptures
There are uterine ruptures that occurred during pregnancy and during childbirth. According to the pathogenetic signs of birth trauma, spontaneous (mechanical, histopathic and mechanical-histopathic) and violent (traumatic, mixed) uterine ruptures are distinguished. According to the birth trauma clinic, uterine ruptures can be threatening, begun, completed.
According to the degree of damage to the walls of the uterus, a birth injury can take the form of a crack, incomplete rupture and complete rupture penetrating into the abdominal cavity. By localization, there is a rupture of the bottom of the uterus, its body, the lower segment, as well as a complete separation of the uterus from the vaginal vaults (colpoporexis) in the transverse position of the fetus. nine0006
Symptoms of uterine rupture
The clinic of birth trauma of the uterus depends on the causes, stage, degree, localization of the rupture. The severity of manifestations and consequences are largely due to the accompanying background - in the presence of somatic diseases of the woman in labor, gestosis, physical and mental exhaustion, infection, etc., irreversible changes quickly develop in the body.
The severity of manifestations and consequences are largely due to the accompanying background - in the presence of somatic diseases of the woman in labor, gestosis, physical and mental exhaustion, infection, etc., irreversible changes quickly develop in the body.
For threatening rupture of the uterus, excessive labor activity with painful strong contractions, deformity of the uterus in the form of an hourglass, development of edema of the cervix, vagina and vulva, difficulty urinating, anxiety of the woman in labor are typical. With the onset of uterine rupture, the listed symptoms are supplemented by convulsive contractions, the appearance of sanious or bloody discharge from the vagina, and hematuria. nine0006
With the completed rupture of the uterus, after a sharp pain and burning sensation in the abdomen, labor activity stops, the woman in labor calms down, becomes depressed, apathetic. Due to the development of hemorrhagic and painful shock, pallor of the skin, hypotension, tachycardia rapidly increase, cold sweat, nausea and vomiting appear. After rupture of the uterus, parts of the fetus are partially or completely palpated in the abdominal cavity, there is no fetal heartbeat. External bleeding with this birth injury can be significant or scanty, depending on the size and location of uterine rupture. nine0006
After rupture of the uterus, parts of the fetus are partially or completely palpated in the abdominal cavity, there is no fetal heartbeat. External bleeding with this birth injury can be significant or scanty, depending on the size and location of uterine rupture. nine0006
Uterine rupture emergency
If there is a threat of uterine rupture, it is necessary to immediately stop labor and complete labor by surgery - caesarean section or fruit-destroying surgery. With the onset or completed uterine rupture, cerebrosection is performed, the fetus and placenta are removed, amniotic fluid and blood are removed, and hemostasis is performed. The volume of intervention for these birth injuries ranges from supravaginal amputation to hysterectomy. Uterine suturing is possible in young patients with recent and small ruptures of a linear nature, the absence of infection. nine0006
At the same time, it is necessary to carry out adequate replenishment of blood loss, anti-shock infusion-transfusion therapy, and correction of hemocoagulation.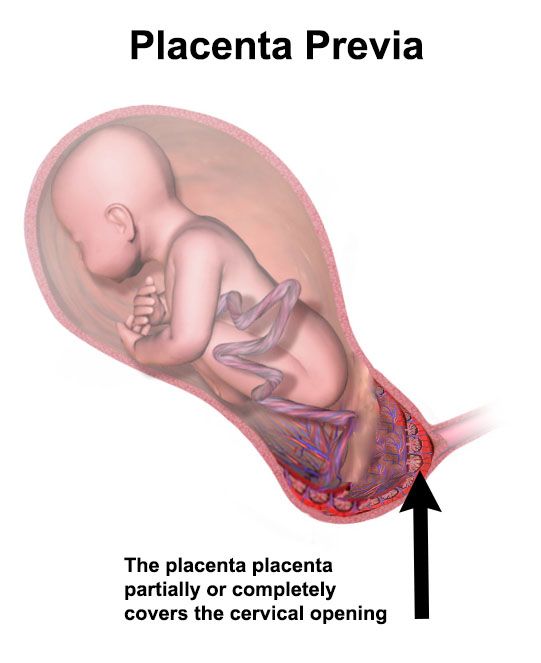 If birth injuries of the uterus were not recognized, bleeding or peritonitis may develop, as well as the death of the puerperal. With infectious complications, laparotomy, removal of the uterus with appendages (panhysterectomy), drainage of the abdominal cavity, and massive antibiotic therapy are undertaken.
If birth injuries of the uterus were not recognized, bleeding or peritonitis may develop, as well as the death of the puerperal. With infectious complications, laparotomy, removal of the uterus with appendages (panhysterectomy), drainage of the abdominal cavity, and massive antibiotic therapy are undertaken.
Cervical tears
This type of birth injury occurs according to various authors in 3-60% of women in labor. Cervical ruptures (violent or spontaneous) are divided into 3 degrees according to the depth of damage: I - a defect of no more than 2 cm; II - defect more than 2 cm, but not reaching the vaginal vaults; III - a defect that reaches the vaults and passes to them. Cervical ruptures are usually localized in the lateral sections, more often on the left.
Symptoms of cervical tears
Birth injuries of the cervix are manifested by postpartum bleeding from the vagina after the birth of the placenta and contraction of the uterus. Blood flowing from the genital tract has a scarlet color, is released in a continuous stream or in the form of a large number of clots in the absence of external damage to the birth canal. Sometimes there is little or no bleeding. If the branches of the uterine arteries are damaged, there is a massive outpouring of blood or the formation of hematomas in the paracervical tissue, a clinic of hemorrhagic shock. nine0006
Blood flowing from the genital tract has a scarlet color, is released in a continuous stream or in the form of a large number of clots in the absence of external damage to the birth canal. Sometimes there is little or no bleeding. If the branches of the uterine arteries are damaged, there is a massive outpouring of blood or the formation of hematomas in the paracervical tissue, a clinic of hemorrhagic shock. nine0006
If cervical ruptures remain unrecognized, in the future this can lead to the development of postpartum ulcers, parametritis, pelvioperitonitis, spontaneous abortions, and cervical dysplasia.
Diagnosis and treatment of cervical tears
To recognize birth injuries of the cervix, all puerperas need to be examined with the help of mirrors immediately after the completion of childbirth, and also 6-48 hours after the reduction of edema and tissue stretching.
Detected ruptures of the cervix are subject to suturing immediately or delayed, no later than 2 days after birth.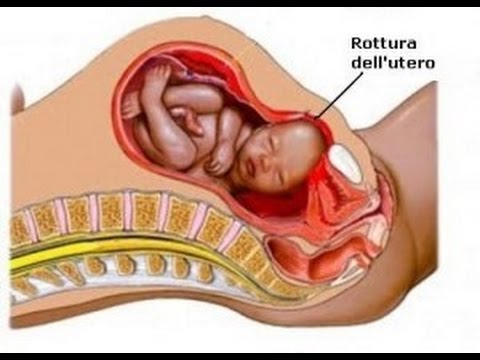 The sutures are applied to the ruptures of the neck through all layers of tissues, starting from the upper corner of the defect in the direction of the external pharynx. Due to unfavorable conditions (the presence of lochia, edema, crushing of tissues), birth injuries of the cervix often heal by secondary intention. nine0006
The sutures are applied to the ruptures of the neck through all layers of tissues, starting from the upper corner of the defect in the direction of the external pharynx. Due to unfavorable conditions (the presence of lochia, edema, crushing of tissues), birth injuries of the cervix often heal by secondary intention. nine0006
Other birth injuries
Uterine eversion
The development of acute uterine inversion is due to improper management of the afterbirth period, weakness of the uterine ligaments, and atony of the uterus. Distinguish between partial and complete eversion of the uterus. This birth injury proceeds with the phenomena of pain shock.
Treatment of uterine inversion consists in anti-shock measures and reduction of the uterus to its anatomical site under general anesthesia.
Sprains and ruptures of the pelvic joints
These birth injuries develop with excessive softening of the joints of the pelvis (symphysiopathy, symphysitis), childbirth with a premature or large fetus, obstetric benefits. In this case, the pubic bones are stretched and separated at a distance of more than 0.5 cm from each other. Rupture of the pubic joint is often accompanied by displacement of bones, damage to the bladder, urethra, and clitoris. Stretching of the sacroiliac joints leads to hemorrhages and subsequent inflammation of the joints.
In this case, the pubic bones are stretched and separated at a distance of more than 0.5 cm from each other. Rupture of the pubic joint is often accompanied by displacement of bones, damage to the bladder, urethra, and clitoris. Stretching of the sacroiliac joints leads to hemorrhages and subsequent inflammation of the joints.
The clinic of birth injuries of the pelvic joints is manifested by pain in the womb, coccyx, sacrum, aggravated by abduction of the legs, walking; gait disturbance, skin hyperemia and swelling of surrounding tissues.
Birth injuries of the pelvic region are detected during the consultation of a traumatologist during examination, palpation, radiography of the pubic, sacroiliac joint, and pelvis. Treatment of sprains of the pelvic joints requires rest, tight bandaging, wearing special corsets. A rupture of the pubic symphysis or a significant divergence of the pelvic bones requires surgical intervention. nine0006
Urogenital and rectovaginal fistulas
Birth injuries with the formation of fistulas are caused by prolonged (more than 2 hours) standing of the child's head in one plane, as a result of which a violation of blood circulation in tissues develops with their subsequent necrosis. Sometimes urogenital and rectal-vaginal fistulas are formed as a result of intraoperative damage to the walls of the bladder or rectum.
Sometimes urogenital and rectal-vaginal fistulas are formed as a result of intraoperative damage to the walls of the bladder or rectum.
Fistulas are manifested by the release of urine or gases and feces through the vagina outside the acts of urination and defecation. Such disorders are always accompanied by the development of a local inflammatory reaction in the vagina (colpitis). nine0006
Diagnosis of urogenital fistulas is made during a gynecological examination, cystoscopy; rectal-vaginal fistulas are recognized by digital rectal examination, irrigoscopy, fistulography, and rectoscopy. When detecting urogenital and rectovaginal fistulas, their surgical closure (fistuloplasty) is usually required.
Birth injury prevention
Prevention of birth injuries of the uterus requires the study of the gynecological history of the pregnant woman in the early stages, ultrasound monitoring of the state of scars on the uterus during pregnancy, hospitalization of pregnant women with the threat of traumatism during childbirth. nine0006
nine0006
Prevention of birth injuries requires the rejection of forced delivery, the use of obstetric benefits strictly according to indications.
You can share your medical history, what helped you in the treatment of birth trauma.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0006
Birth injury - causes of disease, methods, prevention
Birth injury
Sign up Clinic "OSTEOMED" provides treatment of birth injuries, rehabilitation after birth injuries in newborns, infants (infants), babies. Birth trauma is treated with effective osteopathic methods. Traditional and modern methods of reflexology (reflexotherapy) are actively used in the treatment. We carry out the restoration of the child's nervous system (NS), recovery after birth injuries. In pediatric practice, an osteopathic approach is mainly used, which is absolutely gentle and safe for babies.
 The osteopath applies gentle hand pressure on the baby's head and body to ease the effects of birth stress, and correct tension in the skull bones and restore their proper movement. Children and babies feel great after treatment and sleep better. nine0006
The osteopath applies gentle hand pressure on the baby's head and body to ease the effects of birth stress, and correct tension in the skull bones and restore their proper movement. Children and babies feel great after treatment and sleep better. nine0006 Birth injury is damage to the tissues or organs of the fetus during childbirth (birth act) due to the local action of mechanical forces on the fetus. Unfortunately, birth injuries in newborns are quite common.
90% of children have a birth injury, most often it is the cervical spine. If the diagnosis of "birth trauma" is not made, it is advisable for you to contact an osteopath if the following situations occurred during childbirth:
- long dry period
- Opening the fetal bladder by a doctor in the maternity hospital
- Stimulation of labor
- Obstetric manipulations: imposition of forceps, fruit squeezing
- The birth of a child in the pelvic presentation
- Caesarean section
- Epidural (spinal) anesthesia in women in women and after 35 years
- the birth of a large fetus, more than 4 kg
- if your child was born in a state of hypoxia: blue, did not cry immediately, there was an entanglement of the umbilical cord, low Apgar scores
- if your child had a cephalohematoma (swelling on the baby's head) - this indicates a serious injury to the bones of the skull
- your child has been diagnosed with PEP (perinatal encephalopathy), IUGR (intrauterine growth retardation)
Predisposing factors for birth trauma
The main predisposing factors leading to birth trauma are as follows:
1.
 Pathology of the prenatal period.
Pathology of the prenatal period. 2. Pathology of the antenatal period. nine0006
3. Wrong course of pregnancy.
4. Toxicosis, preeclampsia.
5. Placenta previa.
6. Infection of the birth canal (vagina, uterus, etc.).
7. Genital diseases of the mother (woman), diseases of the genital organs: salpingitis, inflammation of the appendages, salpingoophoritis, endometritis, vaginitis, vulvovaginitis, sexually transmitted diseases (venous diseases, venous diseases), infections, inflammatory diseases of the genital organs. nine0006
8. Extragenital diseases (diseases) of the mother. Diseases of the cardiovascular system, Rh incompatibility (Rh conflict) have a particularly strong influence.
9. Preterm pregnancy (fetal miscarriage).
10. Prolongation of pregnancy (post-term fetus).
11. Intrauterine fetal hypoxia (VGP, VUG, VUGP), chronic intrauterine hypoxia (lack of oxygen).
12. Cesarean section (birth trauma during caesarean section).

13. The use of a vacuum extractor in childbirth (vacuum extraction, vacuum extractors, a comprehensive vacuum system for obstetrics, a vacuum extractor). Vacuum fruit extraction.
14. Rapid delivery, stimulation in childbirth.
15. Stress, neurosis, neurasthenia.
16. Increased risk if previous pregnancies ended badly (miscarriage, stillbirth, stillbirth, congenital malformations - congenital malformations). nine0006
Mechanism of development, pathogenesis of birth trauma
What is the mechanism of development of birth trauma, its pathogenesis? All of the above factors cause fetal hypoxia and reduce the resistance of its organs and tissues, especially the brain. All this leads to traumatic effects during childbirth.
Classification of lesions of the nervous system in children
Neonatologist, neurologist, neuropathologist, microneuropathologist distinguish 2 main types of birth injuries (classification by localization): nine0006
1.
 Birth trauma of the central nervous system (CNS).
Birth trauma of the central nervous system (CNS). 2. Birth trauma of the peripheral nervous system (PNS).
There are also the following pathologies: obstetric paralysis (obstetric paralysis), intracranial birth injury (for example, traumatic brain birth injury of the head, brain, cerebellum), birth injury of the spinal cord (for example, birth injury of the cervical spine, neck), birth injuries of peripheral nerves , birth injury of soft tissues (for example, birth tumor), birth injury of bones, skeletal system (for example, fracture of the collarbone), birth injury of internal organs. Separately, obstetric trauma due to obstetric manipulations is singled out, especially in case of an abnormal course of childbirth. nine0006
Consequences of birth injuries
The consequences of birth trauma are varied. Hemorrhages in the brain, paralysis (paralysis), paresis (paresis), retarded growth and development of arms or legs, impaired muscle tone, convulsions, hypertension syndrome, intracranial hypertension, hydrocephalus, convulsive and non-convulsive seizures, damage to cranial nerves, liquorodynamic disorders, decerebrate rigidity, cerebral palsy (ICP), perinatal encephalopathy (PEP), psychomotor retardation, speech retardation, minimal brain dysfunction, pneumonia, urosepsis and the worst consequences.
 nine0006
nine0006 Birth injury prevention
How to avoid birth trauma in newborns? To avoid birth injuries, you must follow a number of recommendations:
- Plan conception and pregnancy in advance.
- Treat chronic conditions before pregnancy.
- Eliminate alcohol (alcoholic beverages), smoking (quit smoking) 3 months before conception and during pregnancy.
- Carry out activities aimed at the prevention and treatment of intrauterine fetal hypoxia. nine0016
- Give birth in a good health facility.
- Prior to delivery (1 month in advance) communicate with such specialists as an obstetrician, gynecologist, midwife, neonatologist, neurologist, microneurologist, neuropathologist, resuscitator who will take part in childbirth.
- Eat well and take vitamins during pregnancy.
- During pregnancy, attend childbirth preparation courses.
- During pregnancy, rest more and work less, walk in the fresh air.
- During pregnancy, regularly visit a medical institution such as a antenatal clinic, conduct the necessary tests, examinations, and studies.

- During pregnancy, avoid contact with infectious patients (especially those with diseases such as influenza, adenovirus infection, parainfluenza, MS infection (respiratory syncytial infection), rotavirus infection (rotavirus infection), SARS, herpes (herpetic infection), rubella, measles, mumps (mumps, mumps), chicken pox (chickenpox), chlamydia, Ebola, plague, HIV infection, tuberculosis, diphtheria, tetanus, echinococcosis, toxoplasmosis, teratogenic infections). nine0016
- Carry out activities aimed at preventing Rh conflict (take into account the Rh blood of the father and mother Rh, use a condom during oral sex).
- During pregnancy, try to avoid exposure to pathological factors such as ionizing radiation, radio waves (microwave ovens, microwave ovens, microwave ovens, x-rays, radiography, MRI - magnetic resonance imaging, NMRI (nuclear magnetic resonance imaging), CT (computed tomography), cellular phone, smartphone, tablet, computer). nine0016
- Exclude the intake of the following: medicines, medicines, medicines, medicines, dietary supplements, dietary supplements not prescribed by a doctor.
 Do not engage in self-medication, uncontrolled intake of drugs.
Do not engage in self-medication, uncontrolled intake of drugs.
Signs of birth trauma
Many parents, fathers and mothers ask us: “What are the first signs that a child has a birth injury?”, “How to determine a birth injury in a child, a newborn?” “Does the baby have a birth injury?” "What are the signs of birth trauma, the consequences of birth trauma?". You should consult a doctor if you notice any of the following signs: nine0006
Online entry
Online record
Date of visit
20.12.2022
Doctors
Our specialists
Smirnov Andrey Valerievich
Clinic Osteomeda, neurologist-pool, candidate of medical sciences, member of ENRO, ENRO, ENRO, ENRO, ENRO, ENRO, ENRO, ENRO, ENRO, ENR doctor of osteopathy in Europe (registration number 248041051021), lecturer at the School of Osteopathy on the Neva at the Department of Neurology, St. Petersburg Institute of Higher Education
Kristina Aleksandrovna Zoller
Neurologist-osteopath, candidate of medical sciences, member of ENRO and ROSA, doctor of osteopathy in Europe (registration number 204115070812), director of the "School of Osteopathy on the Neva", head of the course of osteopathy at the Department of Neurology, SPbIUVE
Kaprielov Karen Aleksandrovich
Osteopath, member of ENRO, doctor of osteopathy of Europe (registration number 244046031012), manual therapist
Cherny Roman Anatolyevich
Osteopath, member of ENRO, doctor of osteopathy of Europe (registration number 22212) School of Osteopathy on the Neva" at the Department of Neurology, St.