Iron level for pregnancy
Pregnancy and birth: Do all pregnant women need to take iron supplements? - InformedHealth.org
Created: December 22, 2009; Last Update: March 22, 2018; Next update: 2021.
Iron supplements are particularly important for pregnant women who have anemia. In women who have normal iron levels, taking iron supplements as a precautionary measure probably doesn’t have any health benefits. They can get enough iron in their diet.
Iron is a mineral that is found in many proteins and enzymes that the body needs in order to stay healthy. Most of the iron in our bodies is found inside hemoglobin, the pigment in red blood cells. Hemoglobin transports oxygen to all of the tissues and organs in the body. If there isn’t enough iron in the blood, the amount of hemoglobin in the blood decreases too. This can reduce the oxygen supply to cells and organs.
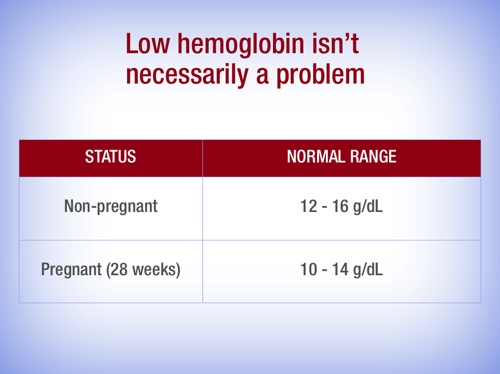
Low levels of hemoglobin are also known as anemia. At the start and towards the end of pregnancy, hemoglobin levels above 11 grams per deciliter are considered to be normal. Between three and six months of pregnancy, a small drop to 10.5 grams per deciliter is also considered to be normal.
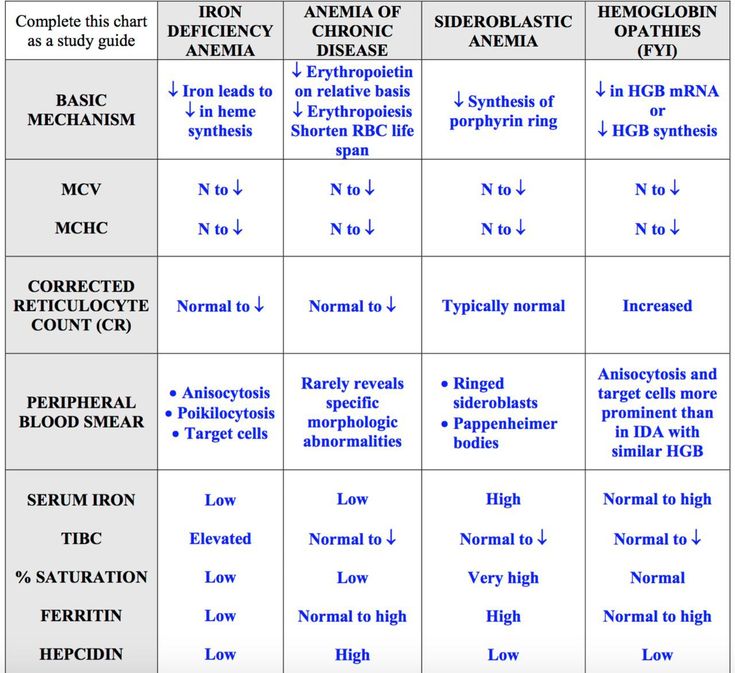
If someone’s hemoglobin levels are lower than this, the iron levels in their blood are measured too. This can help to determine whether their low hemoglobin levels are due to a lack of iron (iron deficiency). Because the body can store a certain amount of iron, another blood value is also measured to find out how full the body’s iron stores are. If someone’s iron stores are empty but their hemoglobin levels are normal, they are said to have latent (hidden) or non-anemic iron deficiency.
Women have several blood tests during pregnancy. One thing that is tested is their iron levels, so iron deficiency anemia can be detected early on and treated using iron supplements.
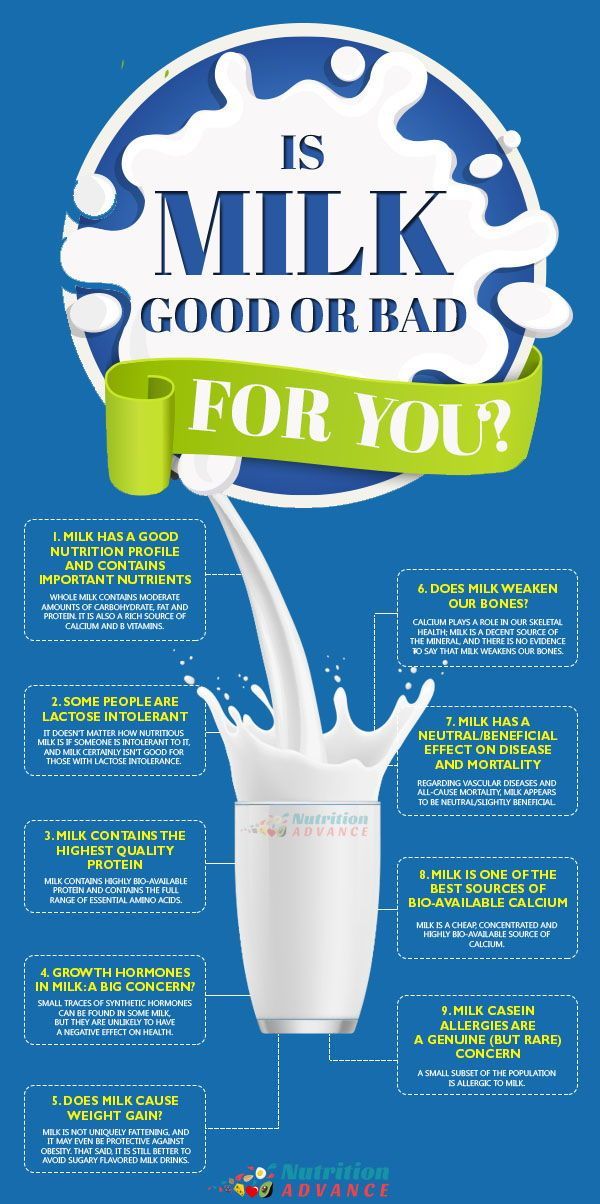
Which foods have iron in them?
We normally get iron in the food we eat. Meat has a lot of iron in it, from hemoglobin in the animal’s body. Liver is particularly high in iron.
It’s harder for the body to absorb iron from plant-based foods. But some plants are good sources of iron too. These include cereals, for instance in the form of whole grain flakes (breakfast cereals), and legumes such as lentils and beans. Green leafy vegetables like lamb’s lettuce and spinach, and herbs like parsley and cress, also have some iron in them.
But some plants are good sources of iron too. These include cereals, for instance in the form of whole grain flakes (breakfast cereals), and legumes such as lentils and beans. Green leafy vegetables like lamb’s lettuce and spinach, and herbs like parsley and cress, also have some iron in them.
Iron-rich foods
Iron can be taken as dietary supplements too. These are available without a prescription in the form of tablets and drops.
What are the consequences of iron deficiency in pregnancy?
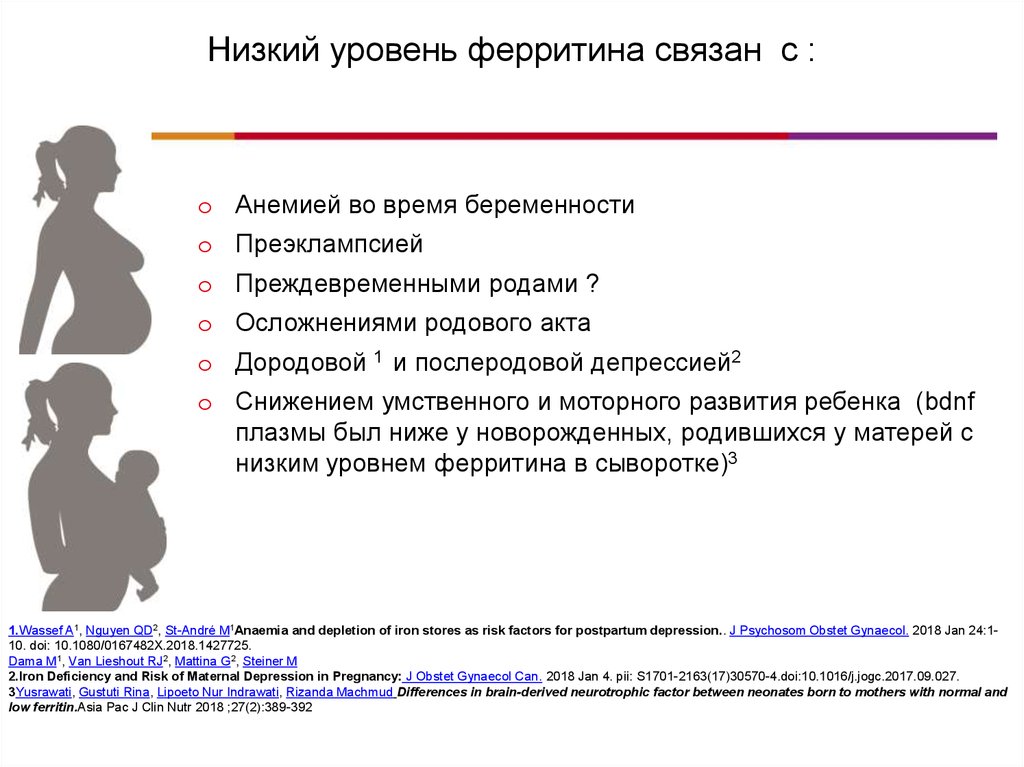
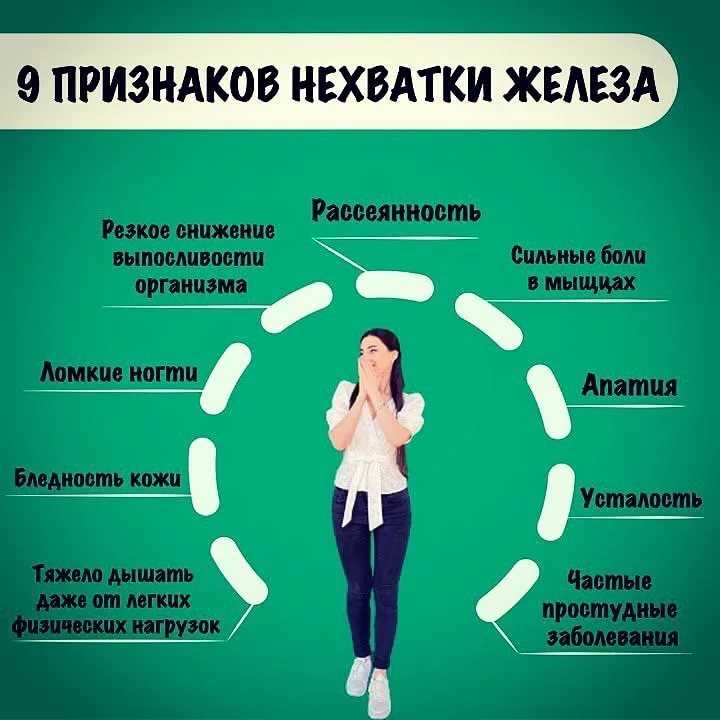
Iron deficiency anemia can make you feel tired and exhausted. Severe anemia can also lead to complications in pregnancy. For instance, it can weaken the mother’s immune system and make infections more likely. It also increases the risk of the baby weighing too little at birth (low birth weight).
Severe anemia is rare in healthy pregnant women who eat a balanced diet. But anemia can cause serious health problems in women who don’t, or can’t, eat a balanced diet.
When does it make sense to take iron supplements?
A lot of pregnant women take iron supplements because they think their bodies need more iron during pregnancy. Pregnant women with normal iron levels in their blood are also often advised to take iron supplements in order to prevent anemia. Mild anemia doesn’t affect the child, though.
Pregnant women with normal iron levels in their blood are also often advised to take iron supplements in order to prevent anemia. Mild anemia doesn’t affect the child, though.
Anemia is only a problem if it is more severe and lasts a long time. If someone is diagnosed with iron deficiency anemia, they are usually prescribed high-dose iron supplements.
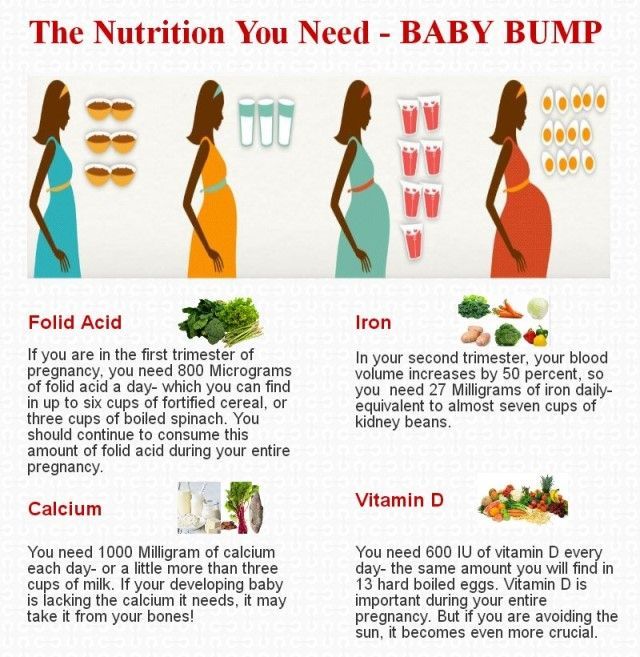
According to German health authorities, pregnant or breastfeeding women need 20 to 30 mg of iron per day. It can be particularly difficult for vegetarians to get that amount of iron in their diet alone. But iron deficiency problems would be detected in the standard blood tests.
Do women with normal iron levels benefit from taking iron supplements?
There are more than 60 studies on the use of iron supplements in pregnancy. A total of more than 40,000 women took part in the studies. The results show that, if women have normal iron levels, taking 30 mg of iron per day as a precautionary measure doesn’t have any noticeable health benefits for them or for their children.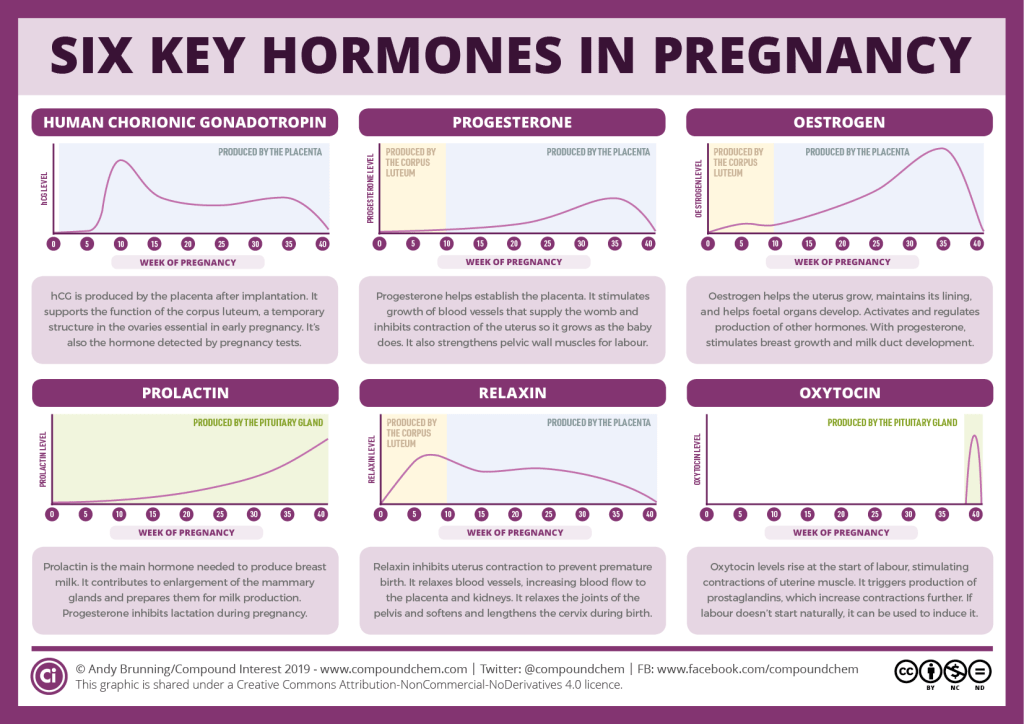 Although iron supplements were found to lower the risk of anemia, they didn’t influence the number of preterm births, the number of babies with a low birth weight (under 2,500 grams) or infections in pregnant women.
Although iron supplements were found to lower the risk of anemia, they didn’t influence the number of preterm births, the number of babies with a low birth weight (under 2,500 grams) or infections in pregnant women.
Side effects and dose
When it comes to iron intake, finding the right balance is key. It’s not only too little iron that can cause problems – too much iron can be unhealthy too. Although our bodies can store a certain amount of extra iron, higher-dose iron supplements may cause side effects. These include, in particular, gastrointestinal (stomach and bowel) problems like constipation, nausea, vomiting and diarrhea. When taken on an empty stomach, they can damage the lining of the stomach.
Some experts recommend only taking iron supplements once or twice a week rather than every day – but at a higher dose (such as 120 mg). Research has found that iron supplements can even prevent anemia when taken only once a week. The idea is that taking iron supplements less often will enable women to take them for longer, and lower the likelihood of side effects.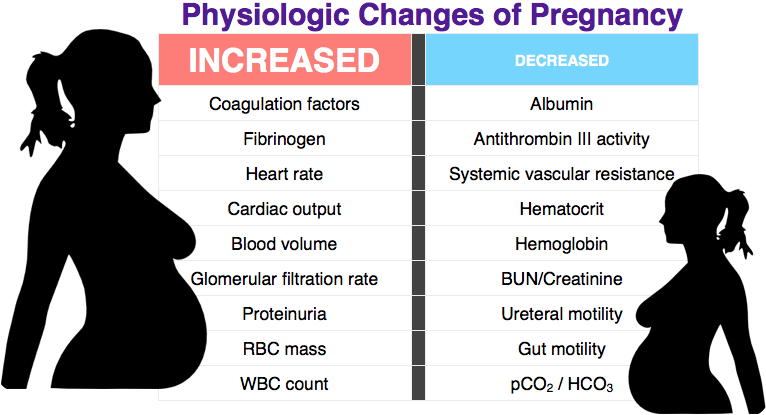 But it’s not clear whether that is really the case.
But it’s not clear whether that is really the case.
Keep iron supplements out of children’s reach
Like all medications, iron tablets should be kept out of children’s reach. Even if iron is “only” a natural mineral, an accidental overdose can be life-threatening for children.
Sources
Bundesinstitut für Risikobewertung (BfR). Fragen und Antworten zu Eisen in Lebensmitteln. December 01, 2008.
Pena-Rosas JP, De-Regil LM, Garcia-Casal MN, Dowswell T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev 2015; (7): CD004736. [PMC free article: PMC8918165] [PubMed: 26198451]
Pena-Rosas JP, De-Regil LM, Gomez Malave H, Flores-Urrutia MC, Dowswell T. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev 2015; (10): CD009997. [PMC free article: PMC7092533] [PubMed: 26482110]
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
Low iron in pregnancy: Spot the symptoms of anemia
During pregnancy, a woman needs twice the amount of iron that a nonpregnant woman needs.
You need iron to keep yourself healthy and to also support your developing baby. Iron helps your red blood cells deliver oxygen to the baby and to your tissues. Without high iron stores or consuming enough iron during pregnancy, you could develop iron deficiency anemia.
Risks associated with anemia during pregnancy include:
- Premature birth
- Low birth weight baby
- Infection
- Poor healing
- Prenatal and postpartum depression
Maternal anemia can also place the mother at an increased risk of death during and after childbirth. Severe anemia can lead to circulatory decompensation, increased cardiac output, an increased risk of hemorrhage and decreased ability to tolerate blood loss, leading to circulatory shock and death. Infants born of iron-deficient mothers are at high risk for having iron deficiency at birth.
Getting enough iron is important for both you and your baby.
Anemia symptoms in women
Symptoms of anemia include:
- Feeling lightheaded or dizzy
- Feeling weak or tired
- Trouble concentrating
- Constant feeling of being cold
- Shortness of breath
- Rapid heartbeat
- Trouble sleeping
- Headaches
If you experience any of these symptoms, call your doctor right away.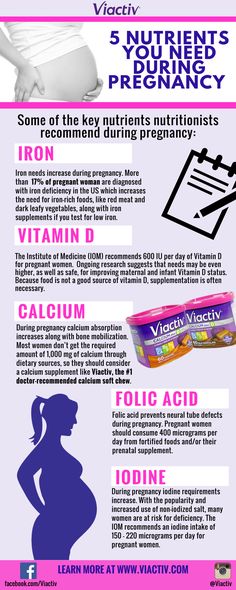
Who is considered anemic?
The World Health Organization (WHO) defines anemia in pregnant women as:
- First trimester: hemoglobin less than 11.0 g/dL
- Second trimester: hemoglobin less than 10.5 g/dL
- Third trimester: hemoglobin less than 11.0 g/dL
Pregnant women are routinely screened for anemia at their first prenatal visit and again between 24 and 28 weeks.
For nonpregnant women, hemoglobin lower than 12.0 g/dL is considered anemic according to the WHO.
Iron supplements during pregnancy
Without iron supplementation, iron deficiency anemia occurs in many pregnant women.
While nonpregnant women only need 18 mg of iron per day, pregnant women require 27 mg of iron daily. This amount is found in most prenatal vitamins. Please keep in mind that most gummy vitamins do not contain iron (as a safety precaution). If taking a gummy prenatal, you will also need an iron supplement. Placing your prenatal vitamin in a designated place such as near your toothbrush or setting an alarm on your phone may help to remind you to take this important vitamin every day.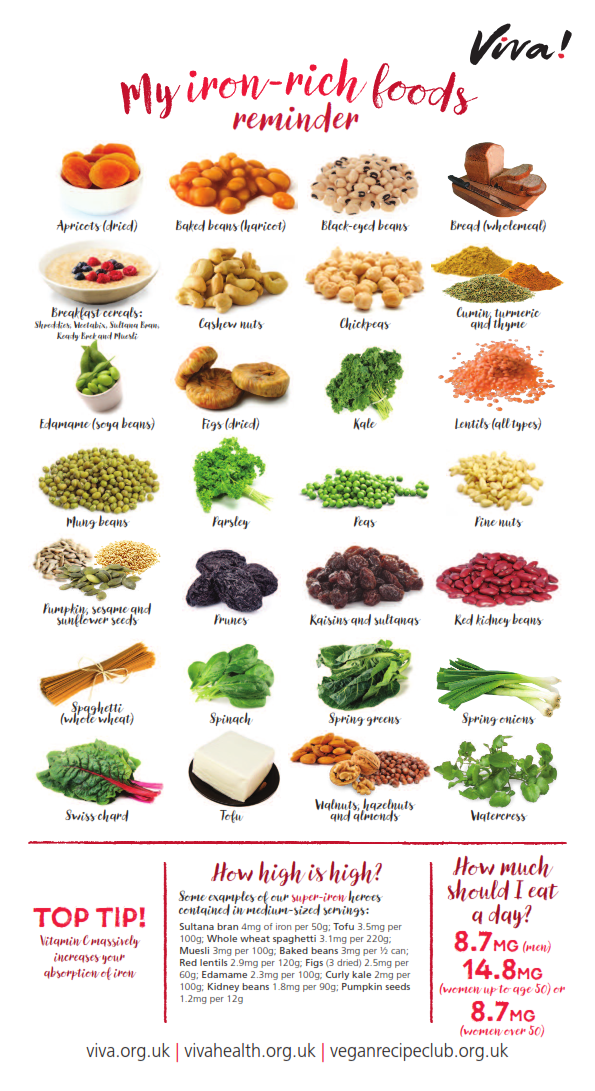
If anemia is diagnosed, your doctor or midwife will prescribe extra iron for you to take daily. In severe cases, iron can be given intravenously. It takes several weeks, sometimes months to increase iron stores in your body so taking iron routinely as prescribed is important. Continue taking your prenatal vitamin and/or supplemental iron for six to eight weeks after delivery, to increase iron stores due to blood loss after delivery.
Iron-rich foods to eat during pregnancy
In addition to taking a prenatal vitamin with iron, eat a balanced diet that includes iron-rich foods. There are two types of iron in foods: heme and nonheme. Meat, poultry and fish contain heme iron, which is much more easily absorbed by the body than nonheme or plant-based iron.
Sources of meat-based (heme) iron:
- Beef
- Chicken
- Turkey
- Organ meats
- Oysters, clams and mussels
Sources of plant-based (nonheme) iron:
- Beans
- Spinach and other leafy greens
- Potato with skin
- Nuts and seeds
- Dried fruit
- Enriched breads and cereals
Vitamin C can help your body absorb iron. When eating plant (nonheme) sources of iron, include a good source of vitamin C, like fruit or fruit juice. When drinking juice, limit to one 8 ounce glass per day due to the high sugar content.
When eating plant (nonheme) sources of iron, include a good source of vitamin C, like fruit or fruit juice. When drinking juice, limit to one 8 ounce glass per day due to the high sugar content.
Sources of vitamin C:
- Oranges
- Grapefruit
- Kiwi
- Broccoli
- Peppers
- Strawberries
- Watermelon
Some foods decrease the body's absorption of iron. Avoid eating high-calcium foods at the same time as iron-rich foods. Calcium is an important nutrient during pregnancy, but calcium and iron compete in the body for absorption. For best results, space your high calcium foods from your high iron foods and prenatal vitamin. Some medications such as antacids and drinking excessive coffee or tea can also reduce the absorption of iron.
Get your pregnancy questions answered
Call 800.922.0000 to schedule an appointment at the Olson Center for Women's Health.
Related stories:
You asked, we answered: What causes premature labor and how can you prevent it?
Preterm birth is currently defined as deliveries between 20 and 37 weeks of gestation. There are two main categories.
There are two main categories.
Read More
You asked, we answered: Is rib pain during pregnancy normal?
I'm pregnant for the first time and I have pain in the upper left side by my ribs – is this normal?
Read More
ANEMIA AND PREGNANCY, OUTPATIENT PRACTICE
Anemia of pregnancy is a series of anemic conditions that occur during pregnancy, complicate its course and usually disappear soon after childbirth or after its termination. Since the prevalence of anemia in pregnant women is much higher than in non-pregnant women, it is logical to assume that most of these anemias are related to the pregnancy itself. Isolation in the ICD-10 anemia of pregnant women (this code is O 99.0) in a separate heading emphasizes the peculiarity of this group of anemia, which consists in the existence of physiological and pathophysiological changes characteristic of pregnancy that contribute to the development of anemia.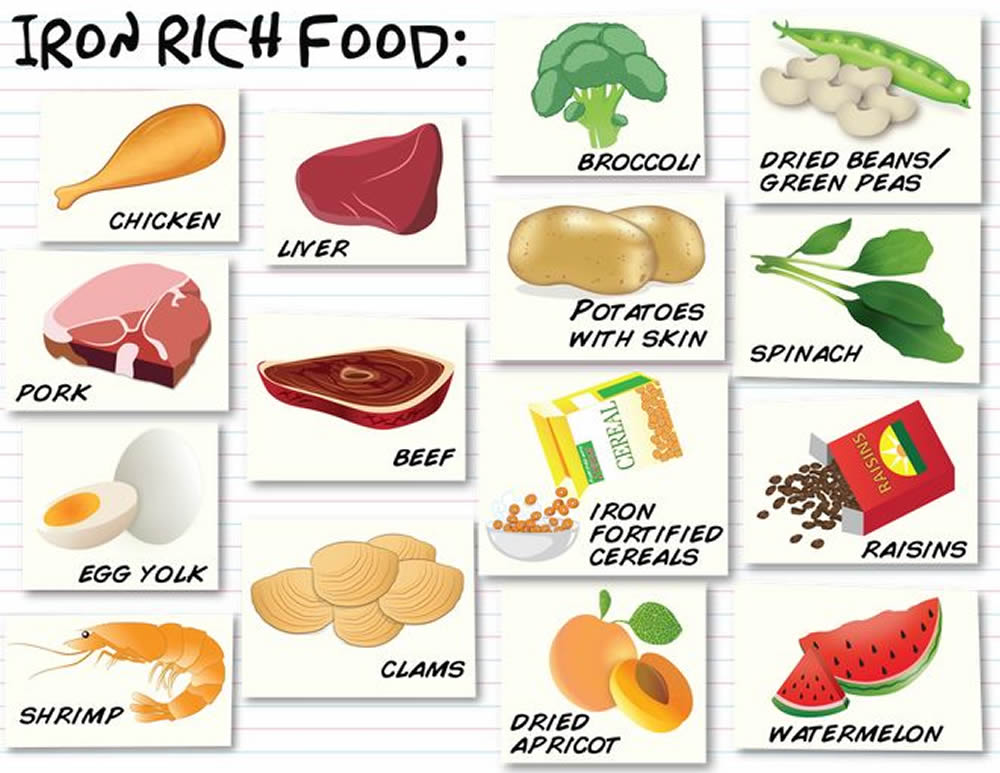
The most common consequences of anemia in pregnancy are miscarriage, premature birth, intrauterine growth retardation and an increased risk of low birth weight babies. The development of anemia in the 1st and 2nd trimesters of pregnancy is associated with a two-fold increase in the risk of preterm birth.
Most researchers believe that iron stores in the fetus do not depend on the iron content in the mother's body. The transfer of iron from the mother through the placenta is regulated by the needs of the fetus, even against the concentration gradient, and mainly occurs in the 3rd trimester of pregnancy. That is why the development of iron deficiency is possible only in premature babies.
These adverse effects of anemia in pregnancy are generally associated with hemoglobin levels < 90 g/L. With a hemoglobin level of 90-110 g / l in the second half of pregnancy, the prognosis for a woman and a child is favorable. At the same time, an increase in the concentration of Hb above 120 g / l in this period of gestation is fraught with a high risk of complications (in particular, preeclampsia).
Any pregnancy results in an increase in plasma volume, which averages 1250 ml. This is approximately 1.5 times the plasma volume in non-pregnant women. This condition is one of the main reasons for the relative decrease in Hb levels in pregnant women.
Today, the lower limit of the normal concentration of Hb in pregnant women is 110 g / l, Hb from 90 to 110 g / l is anemia of 1 degree, from 70 to 90 g / l - anemia of 2 degrees, < 70 g / l - anemia 3 tbsp.
According to WHO, 35-75% of pregnant women in the world are anaemic every year. In domestic obstetric practice, the prevalence of iron deficiency in pregnant women is considered to be high.
Pregnancy anemia is multifactorial, and iron deficiency is an important, but by no means the only, cause of anemia during pregnancy.
FORMS OF ANEMIA.
| Acquired | Hereditary |
| 1. iron deficiency 2. Post -hemorrhagic 3. 4. INEMISIA oria5. Hemolytic | 1. Thalassemias 2. Sickle cell diseases 3. Anemias in other hemoglobinopathies 4. Hemolytic anemias outside of hemoglobinopathies |
The most common types of anemia in pregnancy include iron deficiency anemia (IDA) and folic deficiency anemia, and less frequent are aplastic, megaloblastic, hemolytic anemias.
Factors that predispose to the development of IDA in pregnant women include frequent bleeding with placenta previa; anemia that existed in the patient's mother during pregnancy and prematurity of the patient, as well as seasonality and related changes in the composition of food (vitamin deficiency in the winter-spring period).
Anemia of inflammation - in recent years, there has been an increase in the number of women with urogenital infections (colpitis, cervicitis, bacterial vaginosis, pyelonephritis, etc.), which often occur latently. At the same time, about 30% of pregnant women with urogenital infections approach childbirth in a state of anemia, despite the repeated correction with iron preparations. This anemia is defined as "hypochromic anemia without iron deficiency" with normal or elevated iron stores in the body.
At the same time, about 30% of pregnant women with urogenital infections approach childbirth in a state of anemia, despite the repeated correction with iron preparations. This anemia is defined as "hypochromic anemia without iron deficiency" with normal or elevated iron stores in the body.
Complaints with anemia during pregnancy are usually rare, usually in the presence of concomitant pathology. The most characteristic are complaints of weakness, dizziness, fatigue, in more severe cases, shortness of breath, anxiety and impaired consciousness.
Examination and treatment at the outpatient stage of patients with anemia in pregnancy is carried out in accordance with the Order of the Ministry of Health of the Russian Federation dated 01.11.2012. No. 572n.
Examination at the outpatient stage:
1) Completed general clinical blood test once a month with leukocyte count, count of reticulocytes and platelets.
2) ECG in each trimester.
3) Biochemical blood test (total protein, serum iron, ferritin, transferrin, total and direct bilirubin).
4) Consultation with a general practitioner (hematologist) and further follow-up (1-2 times a month).
5) Clarification of the diagnosis and resolution of the issue of the possibility of continuing the pregnancy up to 10 weeks.
6) Bone marrow puncture (as prescribed by a hematologist).
7) CTG and dopplerometry in dynamics.
Outpatient treatment:
1) Diet rich in proteins, iron, vitamins and folates.
2) Preparations containing iron (in accordance with the Decree of the Government of the Russian Federation of December 26, 2015 N 2724-r, which contains a list of vital and essential drugs for medical use for 2016) - these are oral preparations of 3-valent iron - iron 3 hydroxide polymaltose (maltofer, fenyuls, ferrum lek). It is not recommended to stop taking iron supplements after normalization of hemoglobin levels.
3) Treatment of underlying and concomitant diseases.
Indications for hospitalization:
1) Deterioration of the pregnant woman's condition, lack of effect from outpatient treatment of pregnancy complications.
2) Planned hospitalization for delivery at 38-39 weeks.
Prevention of anemia in pregnancy.
To maintain a normal iron balance during pregnancy, it is necessary that:
1. iron stores in the woman's body by the beginning of pregnancy are adequate;
2. The pregnant woman's diet contained sufficient bioavailable iron to ensure high levels of intestinal absorption in the 2nd half of pregnancy.
The daily iron requirement of a pregnant woman is estimated at 27 mg. Lower intake in women with inadequate iron stores may lead to anemia. Iron absorption is greatly increased in the presence of ascorbic acid. Therefore, it is most beneficial to consume foods containing iron in combination with foods fortified with vitamin C.
WHO recommends 60 mg iron per day for all pregnant women in areas where the prevalence of IDA is less than 20% and 120 mg where it is above this value.
Prevention of iron deficiency during pregnancy planning is an ideal form of prevention of IDA in pregnant women.
Primary prevention of IDA in pregnant women aims to reduce the prevalence of iron deficiency during pregnancy and prevent the adverse effects it can cause on the woman and fetus.
2014
1803
382
21,2
2015
1782
462
26
Statistical data on the incidence of anemia for 6 months. 2015 and 6 months 2016
| Finished pregnancy | Anemia in pregnancy | % | |
| 2015 | 845 | 155 | 18% |
| 6 mon. 2016 | 1118 | 250 | 22.3% |
If the above incidence of anemia in pregnant women over the past 3 years, then we can say the following in 2013. and in 2015 % of this pathology among pregnant women remained approximately at the same level, in 2014 there was a slight decrease in this indicator to 21.2%.
Management of patients with anemia of pregnancy in the w/c No. 2.
No. 572n.
2. When the diagnosis of anemia of pregnancy is established, the patient is referred for a consultation with a general practitioner f/c.
3. With anemia 2-3 tbsp. and not amenable to correction of anemia 1 tbsp. the woman is sent for a consultation with a hematologist.
4. Within the framework of the Birth certificate program, we prescribe free oral iron preparations to patients with anemia of pregnancy.
5. In accordance with the order of the Ministry of Health of the Republic of Kazakhstan of 21.01. No. 54 “On providing adequate nutrition for pregnant women, nursing mothers, as well as children under the age of 3 years in the Ryazan region”, we issue certificates for receiving monthly monetary compensation before childbirth to pregnant women diagnosed with anemia of 2-3 tbsp.
In order to prevent anemia in pregnant women during preconception preparation, taking into account the level of initial hemoglobin, patients are prescribed iron preparations.
As part of the classes at the "School of Pregnant Women", women from early pregnancy are told about the need for a full-fledged, rational nutrition during pregnancy in order to prevent anemia.
Anemia during pregnancy
220045, Minsk, st. Semashko, 10
This email address is being protected from spambots. You must have JavaScript enabled to view.
Version of the site for visually impaired
Healthcare Institution
Minsk Clinical Consultative Diagnostic Center
Call-Center (Registration)
| +375 17 311 10 19 (10 lines) | ||
| +375 17 355 94 50 (7 lines) | ||
| +375 29 238 00 90 (mobile MTS 4 lines) | ||
| +375 44 550 00 90 (mobile A1 4 lines) |
Apply online
Minsk Clinical Consultative and Diagnostic Center Book online Anemia refers to a decrease in the level of hemoglobin in the blood. During pregnancy, the amount of fluid in a woman's body increases, and hence the volume of circulating blood. Due to this, the blood "thinns" and the proportion of hemoglobin in its total volume falls. This is considered normal, and therefore the lower limit of the amount of hemoglobin during pregnancy is set at 110 g / l (at a rate of 120-140 g / l for a non-pregnant woman). But a further drop in hemoglobin levels is dangerous for the health and even the life of the expectant mother. Depending on the values of this indicator, anemia during pregnancy can be: The most common complications of anemia during pregnancy are: So anemia during pregnancy is by no means a harmless condition. It has serious consequences for both mother and fetus. During pregnancy, iron is consumed not only for the mother's hematopoiesis, but also for the needs of the fetus. This consumption increases especially actively at the 16–20th week, when the process of hematopoiesis in the fetus starts. By the end of pregnancy, iron stores are depleted in any woman and it takes 2-3 years to fully restore them. Other causes of anemia during pregnancy are: If we talk about risk groups for developing anemia during pregnancy, then they can include women: with multiple pregnancies and multiple births; who had menstruation for more than 5 days before pregnancy; who had symptoms of anemia during a previous pregnancy; with gestosis; with chronic diseases of the gastrointestinal tract, liver, chronic infections; vegetarians. Considering that during pregnancy the need of a woman's body for a microelement increases by 15–33%, symptoms indicating hypoxia usually come to the fore: weakness, fatigue; sleep disturbance: during the day - drowsiness, at night - insomnia; headache; dizziness, tinnitus; dyspnea; heartbeat; fainting. The tolerance of anemia symptoms is individual: someone faints at relatively high hemoglobin values, someone refuses hospitalization with hemoglobin at a level of about 70 g / l, sincerely not understanding the severity of anemia and its danger during pregnancy. That is why a clinical blood test during pregnancy is mandatory and several times. The drop in the values of iron in the blood serum and serum ferritin is also important. A decrease in the amount of the latter to 12 μg / l indicates an iron deficiency, even if hemoglobin is still normal. Treatment of anemia while expecting a baby will include diet therapy. One of the foundations of both the prevention and treatment of anemia during pregnancy is proper nutrition. Nutrition for the prevention of anemia during pregnancy should contain a sufficient amount of the substances necessary for normal hematopoiesis - this is meat, fish. In these products, iron is initially divalent, so it is easily absorbed. But diet alone may not be enough even for prevention. Iron supplements are prescribed to treat anemia. Usually limited to means for oral administration (i.e., inside) - iron preparations in injections are recommended only in severe cases and only in a hospital setting. Both Russian and foreign experts note that the prevention of anemia in pregnant women is more effective than its treatment, and the higher the hemoglobin level, the easier it is to bring it back to normal. However, common sense says the same. Therefore, when planning a pregnancy, and even more so already expecting a child, it is better to prevent anemia without waiting until iron deficiency becomes noticeable. +375 17 355 94 50 (Horizontal) +375 29 238 00 90 (mobile MTS) +375 44 550 00 90 (mobile A1) You are here:
 Everyone at risk should especially carefully monitor their condition and, if possible, take care of the prevention of anemia during pregnancy.
Everyone at risk should especially carefully monitor their condition and, if possible, take care of the prevention of anemia during pregnancy. 
 Folic -deficiency
Folic -deficiency