Induced pain labor
Inducing labour - NHS
An induced labour is one that's started artificially. Every year, 1 in 5 labours are induced in the UK.
Sometimes labour can be induced if your baby is overdue or there's any risk to you or your baby's health.
This risk could be if you have a health condition such as high blood pressure, for example, or your baby is not growing.
Induction will usually be planned in advance. You'll be able to discuss the advantages and disadvantages with your doctor and midwife, and find out why they think your labour should be induced.
It's your choice whether to have your labour induced or not.
If your pregnancy lasts longer than 42 weeks and you decide not to have your labour induced, you should be offered increased monitoring to check your baby's wellbeing.
Why you might be induced
- if you're overdue
- if your waters have broken
- if you or your baby have a health problem
If you're overdue
Induction will be offered if you do not go into labour naturally by 42 weeks, as there will be a higher risk of stillbirth or problems for the baby.
If your waters break early
If your waters break more than 24 hours before labour starts, there's an increased risk of infection to you and your baby.
If your waters break after 34 weeks, you'll have the choice of induction or expectant management.
Expectant management is when your healthcare professionals monitor your condition and your baby's wellbeing, and your pregnancy can progress naturally as long as it's safe for both of you.
Your midwife or doctor should discuss your options with you before you make a decision.
They should also let you know about the newborn (neonatal) special care hospital facilities in your area.
If your baby is born earlier than 37 weeks, they may be vulnerable to problems related to being premature.
If your waters break before 34 weeks, you'll only be offered induction if there are other factors that suggest it's the best thing for you and your baby.
If you have a health condition or your baby is not thriving
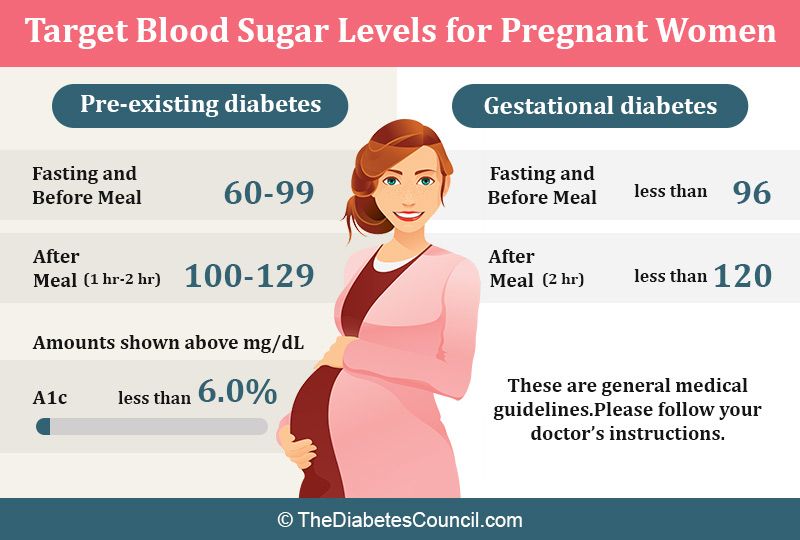
You may be offered an induction if you have a condition that means it'll be safer to have your baby sooner, such as diabetes, high blood pressure or intrahepatic cholestasis of pregnancy.
If this is the case, your doctor and midwife will explain your options to you so you can decide whether or not to have your labour induced.
Membrane sweep
Before inducing labour, you'll be offered a membrane sweep, also known as a cervical sweep, to bring on labour.
To carry out a membrane sweep, your midwife or doctor sweeps their finger around your cervix during an internal examination.
This action should separate the membranes of the amniotic sac surrounding your baby from your cervix. This separation releases hormones (prostaglandins), which may start your labour.
Having a membrane sweep does not hurt, but expect some discomfort or slight bleeding afterwards.
If labour does not start after a membrane sweep, you'll be offered induction of labour.
Induction is always carried out in a hospital maternity unit. You'll be looked after by midwives and doctors will be available if you need their help.
How labour is induced
If you're being induced, you'll go into the hospital maternity unit.
Contractions can be started by inserting a tablet (pessary) or gel into your vagina.
Induction of labour may take a while, particularly if the cervix (the neck of the uterus) needs to be softened with pessaries or gels.
You will usually stay in the hospital maternity unit while you wait for it to work.
If you've had no contractions after 6 hours, you may be offered another tablet or gel.
If you have a controlled-release pessary inserted into your vagina, it can take 24 hours to work. If you are not having contractions after 24 hours, you may be offered another dose.
Sometimes a hormone drip is needed to speed up the labour. Once labour starts, it should proceed normally, but it can sometimes take 24 to 48 hours to get you into labour.
What induced labour feels like
Induced labour is usually more painful than labour that starts on its own, and you may want to ask for an epidural.
Your pain relief options during labour are not restricted by being induced. You should have access to all the pain relief options usually available in the maternity unit.
If you are induced you'll be more likely to have an assisted delivery, where forceps or ventouse suction are used to help the baby out.
If induction of labour does not work
Induction is not always successful, and labour may not start.
Your obstetrician and midwife will assess your condition and your baby's wellbeing, and you may be offered another induction or a caesarean section.
Your midwife and doctor will discuss all your options with you.
Natural ways to start labour
There are no proven ways of starting your labour yourself at home.
You may have heard that certain things can trigger labour, such as herbal supplements and having sex, but there's no evidence that these work.
Other methods that are not supported by scientific evidence include acupuncture, homeopathy, hot baths, castor oil and enemas.
Having sex will not cause harm, but you should avoid having sex if your waters have broken as there's an increased risk of infection.
For more information on induction, you can read the NICE information for the public on induction of labour.
Video: When would I be induced and what's involved?
In this video, a midwife describes what an induction of labour is and what is involved.
Media last reviewed: 20 March 2020
Media review due: 20 March 2023
Induced labour | Pregnancy Birth and Baby
What is an induced labour?
Labour normally starts naturally any time between 37 and 42 weeks of pregnancy. The cervix softens and starts to open, you will get contractions, and your waters break.
In an induced labour, or induction, these labour processes are started artificially. It might involve mechanically opening your cervix, breaking your waters, or using medicine to start off your contractions — or a combination of these methods.
In Australia, about 1 in 3 women has an induced labour.
What are the differences between an induced and a natural labour?
An induced labour can be more painful than a natural labour. In natural labour, the contractions build up slowly, but in induced labour they can start more quickly and be stronger. Because the labour can be more painful, you are more likely to want some type of pain relief.
If your labour is induced, you are also more likely to need other interventions, such as the use of forceps or ventouse (vacuum) to assist with the birth of your baby. You will not be able to move around as much because the baby will be monitored more closely than during a natural labour.
You will only be offered induced labour if there is a risk to you or your baby's health. Your doctor might recommend induced labour if:
- you are overdue (more than 41 weeks pregnant)
- there is a concern the placenta is not working as it should
- you have a health condition, such as diabetes, kidney problems, high blood pressure or pre-eclampsia
- the baby is making fewer movements, showing changes in its heart rate, or not growing well
- your waters have broken, but the contractions have not started naturally
- you are giving birth to more than one baby (twins or multiple birth)
Not everyone can have an induced labour. It is not usually an option if you have had a caesarean section or major abdominal surgery before, if you have placenta praevia, or if your baby is breech or lying sideways.
It is not usually an option if you have had a caesarean section or major abdominal surgery before, if you have placenta praevia, or if your baby is breech or lying sideways.
Can I decide whether to have an induced labour?
If you are overdue, you might decide to wait and see if labour will start naturally. However, if there is a chance you or your baby are at risk of complications, you might need to consider induced labour before your due date.
When making your decision, discuss the risks and benefits with your doctor. Do not be afraid to ask lots of questions, such as:
- Why do I need an induction?
- How will it affect me and my baby?
- What will happen if I do not have the induction?
- What procedures are involved and how will you care for me and my baby?
You might need to consider several other health concerns. For example, there is a higher risk of stillbirth or other problems if your baby is not born before 42 weeks, and an increased risk of infection if your waters break more than 24 hours before labour starts.
What can I expect with an induced labour?
During the late stages of your pregnancy, your healthcare team will carry out regular checks on your health and your baby's heath. These checks help them decide whether it is better to induce labour or to keep the baby inside. Always tell your doctor or midwife if you notice your baby is moving less than normal.
If they decide it is medically necessary to induce labour, first your doctor or midwife will do an internal examination by feeling inside your vagina. They will feel your cervix to see if it is ready for labour. This examination will also help them decide on the best method for you.
It can take from a few hours to as long as 2 to 3 days to induce labour. It depends how your body responds to the treatment. It is likely to take longer if this is your first pregnancy or you are less than 37 weeks pregnant.
What options are there to induce labour?
There are different ways to induce labour. Your doctor or midwife will recommend the best method for you when they examine your cervix. You may need a combination of different strategies. You will need to provide written consent for the procedure.
You may need a combination of different strategies. You will need to provide written consent for the procedure.
Sweeping the membranes
During a vaginal examination, the midwife or doctor makes circular movements around your cervix with their finger. This action should release a hormone called prostaglandins. You do not need to be admitted to hospital for this procedure and it is often done in the doctor's room. This can be enough to get labour started, meaning you will not need any other methods.
Risks: This is a simple and easy procedure; however, it does not always work. It can be a bit uncomfortable, but it does not hurt.
Oxytocin
A synthetic version of the hormone oxytocin is given to you via a drip in your arm to start your contractions. When the contractions start, the amount of oxytocin is adjusted so you keep on having regular contractions until the baby is born. This whole process can take several hours.
Risks: Oxytocin can make contractions stronger, more frequent and more painful than in natural labour, so you are more likely to need pain relief.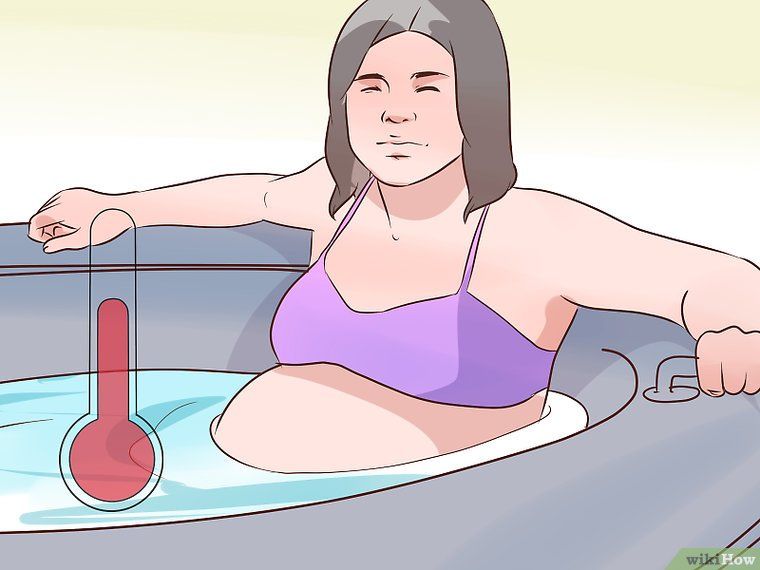 You will not be able to move around much because of the drip in your arm and you will also have a fetal monitor around your abdomen to monitor your baby.
You will not be able to move around much because of the drip in your arm and you will also have a fetal monitor around your abdomen to monitor your baby.
Sometimes the contractions can come too quickly, which can affect the baby's heart rate. This can be controlled by slowing down the drip or giving you another medicine.
Artificial rupture of membranes ('breaking your waters')
Artificial rupture of membranes (ARM) is used when your waters do not break naturally. Your doctor or midwife inserts a small hook-like instrument through your vagina to make a hole in the membrane sac that is holding the amniotic fluid. This will increase the pressure of your baby's head on your cervix, which may be enough to get labour started. Many women will also need oxytocin to start their contractions.
Risks: ARM can be a bit uncomfortable but not painful. There is a small increased risk of a prolapsed umbilical cord, bleeding or infection.
Prostaglandins
A synthetic version of the hormone prostaglandins is inserted into your vagina to soften your cervix and prepare your body for labour.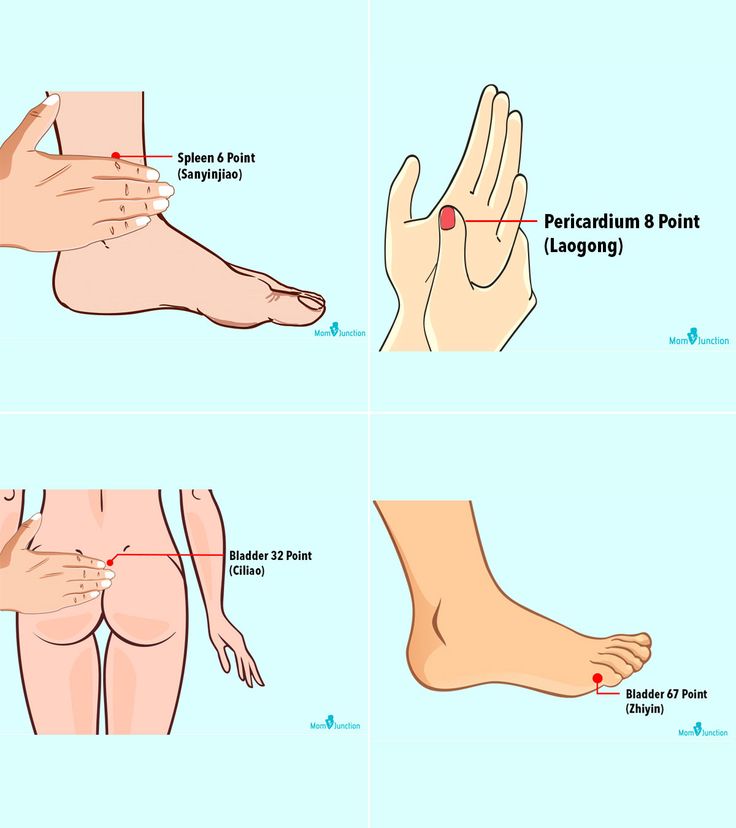 It can be in the form of a gel, which may be given in several doses (usually every 6 to 8 hours), or a pessary and tape (similar to a tampon), which slowly releases the hormone over 12 to 24 hours. You will need to lie down and stay in hospital after the prostaglandins is inserted. You may also then need ARM if your waters have not broken, or oxytocin to bring on the contractions.
It can be in the form of a gel, which may be given in several doses (usually every 6 to 8 hours), or a pessary and tape (similar to a tampon), which slowly releases the hormone over 12 to 24 hours. You will need to lie down and stay in hospital after the prostaglandins is inserted. You may also then need ARM if your waters have not broken, or oxytocin to bring on the contractions.
Prostaglandins gel is often the preferred method of inducing labour since it is the closest to natural labour. Tell your midwife or doctor straight away if you start to experience painful, regular contractions 5 minutes apart for your first baby, or 10 minutes apart for subsequent babies, or if your waters break, because these are both signs that your labour is beginning.
Risks: Some women find their vagina is sore after the prostaglandin gel, or they might experience nausea, vomiting or diarrhoea. These side effects are rare and there is no evidence that induction using prostaglandin is any more painful than a natural labour.
Very rarely, the contractions can come too strongly, which can affect the baby's heart rate. This can be controlled by giving you another medicine or removing the pessary.
You need to let your doctor or midwife know immediately if you start bleeding, or if your baby is moving less, because this could be a sign that something is wrong.
Cervical ripening balloon catheter
A cervical ripening balloon catheter is a small tube attached to a balloon that is inserted into your cervix. The balloon is inflated with saline, which usually puts enough pressure on your cervix for it to open. It stays in place for up to 15 hours, and then you will be examined again.
Tell your midwife or doctor straight away if you start to experience painful, regular contractions 5 minutes apart for your first baby, or 10 minutes apart for subsequent babies, or if your waters break, because these are both signs that your labour is beginning.
You may also need ARM or oxytocin if you are using a cervical ripening balloon catheter.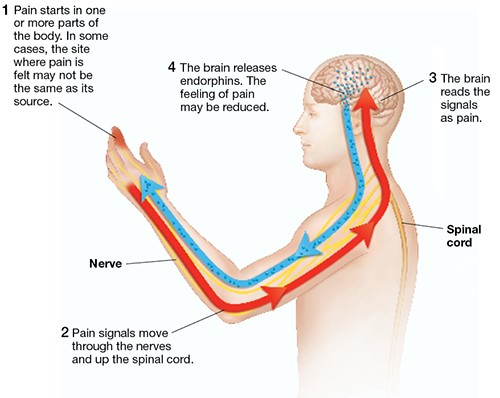
Risks: Inserting the catheter can be a bit uncomfortable but not painful.
You also need to let your doctor or midwife know immediately if you start bleeding, or your baby is moving less, because this could be a sign that something is wrong.
Can I have pain relief during induced labour?
Induced labour is usually more painful than natural labour. Depending on the type of induction you are having, this could range from discomfort with the procedure or more intense and longer lasting contractions as a result of the medication you have been given. Women who have induced labour are more likely to ask for an epidural for relief.
Because inductions are almost always done in hospital, the full range of pain relief should be available to you. There is usually no restriction on the type of pain relief you can have if your labour is induced.
Are there any risks with inducing labour?
There are some increased risks if you have an induced labour. These include that:
These include that:
- it will not work — in about 1 of 4 cases, women go on to have a caesarean
- your baby will not get enough oxygen and their heart rate is affected
- you or your baby get an infection
- your uterus tears
- you bleed a lot after the birth
What happens if the induction does not work?
Not all induction methods will work for everyone. Your doctor may try another method, or you might need to have a caesarean. Your doctor will discuss all of these options with you.
Learn more here about the development and quality assurance of healthdirect content.
Treatment of drug-induced headache (abuses) - causes, cost, appointment in St. Petersburg [MEDICA]
Experienced neurologists and cephalgologists with more than 10 years of experience work at the Headache Treatment Center. Cephalgology is a branch of neurology that deals with the targeted treatment and study of headaches.
Therefore, in the case of regular and severe headaches, it is not enough to visit a neurologist. An experienced cephalgologist will determine the cause of the pain and help eliminate it, not the symptoms. nine0003 One of the types of headache that requires the intervention of a cephalgologist is an overuse headache.
What is overuse headache?
Drug-induced or abuse headache (ADH) is a form of chronic daily headache (CDH). It develops in patients with migraine or tension-type headache (THT) with the abuse of painkillers.
What are the symptoms of AHD?
AHA is manifested by daily dull pains in the whole head and can have different intensity; The greatest strength of pain is noted, as a rule, in the morning. In addition to pain, there is often a feeling of fatigue, lightheadedness, decreased performance, irritability, and sleep disturbances. Patients with migraine against the background of constant dull pain several times a month may experience more or less typical migraine attacks: severe throbbing pain on one side, accompanied by nausea/vomiting, sensitivity to sound and light.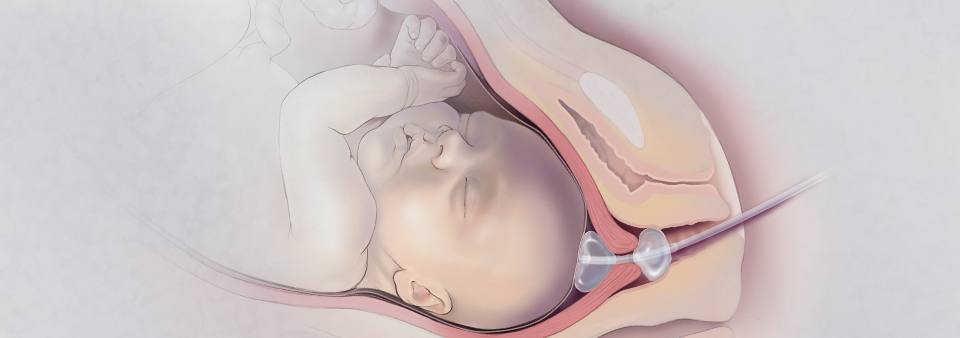 nine0005
nine0005
How and in whom does AHD develop?
The mechanism of development of drug-induced headache is not fully understood. Anyone who takes analgesics more than 3 days a week can develop AHD. Any drug that is taken for headaches can cause AHA if taken very often over a long period of time. Aspirin, paracetamol, ibuprofen, codeine - virtually all overused analgesics can lead to this problem. It is assumed that analgesics cause changes in the brain systems that conduct pain impulses over time. Over the years, the effectiveness of painkillers decreases, and the patient is forced to take increasing doses of drugs. It's not how much medication you take that matters: if you only use a full dose of an analgesic 1-2 days a week, you're unlikely to develop AHA. But if you take only 2 tablets of an analgesic, but most of the time, then the likelihood of developing AHD will increase significantly. Thus, the problem is the frequent use of drugs for a long time. nine0005
Drugs intended for the specific treatment of a migraine attack can also cause AHD if abused. These drugs include triptans and, to a greater extent, ergotamine. Similar headaches can occur from excessive consumption of caffeine. Usually caffeine enters the body with coffee, tea or cola, but it can also be contained in headache pills (combined analgesics).
These drugs include triptans and, to a greater extent, ergotamine. Similar headaches can occur from excessive consumption of caffeine. Usually caffeine enters the body with coffee, tea or cola, but it can also be contained in headache pills (combined analgesics).
Patients with AH usually have a migraine or tension-type headache at the onset. For various reasons, headache attacks are becoming more and more frequent. This may occur against the background of emotional stress, due to the addition of another type of headache, may be due to muscle tension. An increase in the frequency of pain attacks leads to an increase in the use of painkillers, which, in the end, leads to daily and repeated use of drugs. nine0005
Many people in this situation realize that they are abusing drugs and try to stop taking them. This leads to the development of a withdrawal syndrome and an increase in headache, which again requires the use of an analgesic. A vicious circle arises that is very difficult to break: pain - taking painkiller - pain relief - the effect of the drug is over - pain intensification - taking painkiller - pain relief - the effect of the drug is over - pain intensification, etc.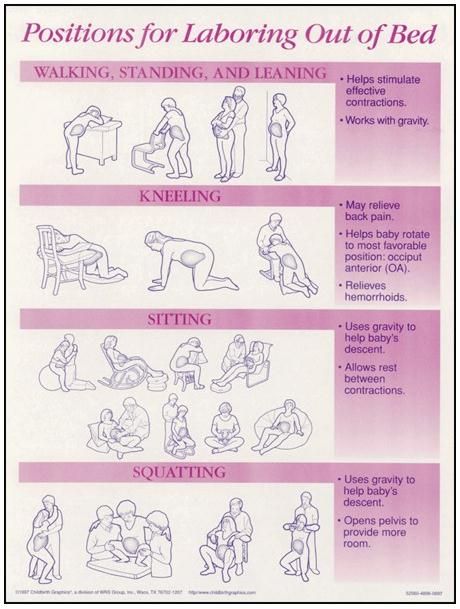
Read more
Specialists
Samorukova
Ekaterina Mikhailovna
Neurologist, Tsephalgologist, Botulinotherapist
Toropova
Neurologist, Botulinotherapist
, initial appointment
from 2 000 ₽
Neurologist, repeated appointment
1 950 ₽ 1 700 ₽
Online consultation of a neurologist
2 200 ₽
Cephologist, advanced consultation (90 min.)
4 200 ₽
All prices
Are additional examinations needed?
There are no methods of examination confirming the diagnosis of AHD. Diagnosis is based on the patient's description of their headache and an analysis of the frequency and amount of pain medication taken for headache. It is mandatory that there are no abnormalities during the medical examination.
Additional research methods, including brain scanning, have no diagnostic value in CEHD, since they do not reveal any specific changes. If the doctor is not sure of the correctness of the diagnosis, he may prescribe additional examination methods to exclude other causes of headache. If the doctor has not ordered additional studies, this means that he is confident in the diagnosis and conducting examinations will in no way facilitate the appointment of treatment.
If the doctor is not sure of the correctness of the diagnosis, he may prescribe additional examination methods to exclude other causes of headache. If the doctor has not ordered additional studies, this means that he is confident in the diagnosis and conducting examinations will in no way facilitate the appointment of treatment.
What can you do to help yourself?
The only way to get rid of drug-induced headache is to stop the addictive drug; clinical studies have shown that the abolition of the "guilty" drug significantly improves well-being. However, it may take up to three months for you to feel the final improvement. Even if the headaches persist despite discontinuation of the drug, they become milder and more responsive to the right treatment. nine0005
You can stop the drug at once, or do it gradually, reducing the dose over 2-3 weeks. In any case, during the period of withdrawal, you need to drink more fluids (but not caffeinated drinks). With the simultaneous cancellation of the "guilty" drug within 48 hours, withdrawal symptoms may occur: increased headache, nausea or vomiting, anxiety, sleep disturbances. These symptoms may persist for a maximum of two weeks. Don't start canceling before important events: warn co-workers that you may be out of work for a few days. nine0005
These symptoms may persist for a maximum of two weeks. Don't start canceling before important events: warn co-workers that you may be out of work for a few days. nine0005
What happens if you leave everything as it is?
If the cause of your headache is the abuse of analgesics, then letting things take their course is not the way out. Headaches will continue to become more frequent, will finally cease to be relieved by analgesics and will not respond to preventive treatment. Over time, liver or kidney dysfunction may develop.
What other treatments are available?
Your doctor may prescribe certain drugs for you to take every day to help you stop taking painkillers. But these drugs will only work if you stop taking all pain medications. With severe drug abuse, there are methods of active detoxification, which is carried out in a hospital. nine0005
Can you be sure that the headache will never come back?
As a rule, after discontinuation of the “guilty” drug and against the background of prophylactic treatment, ATH begins to recede, and patients return to their original type of headache: episodic migraine or TTH. Then, if necessary, you can carefully resume taking painkillers no earlier than after a few weeks. One should always be aware of the risk of re-development of the same condition. To prevent this from happening, avoid taking painkillers more than three days in a row or on a regular basis more than three times a week. nine0005
Then, if necessary, you can carefully resume taking painkillers no earlier than after a few weeks. One should always be aware of the risk of re-development of the same condition. To prevent this from happening, avoid taking painkillers more than three days in a row or on a regular basis more than three times a week. nine0005
- All clinics and centers
- multidisciplinary clinics
- Medicine Medicine Center
- Rage Diagnostic Center
- Clinic of Treatment of Pain Cardiocenters
- Clinic of Aesthetic Medicine 00 SAM, Multi-Prophetic Clinic, Multi-Prophetic Clinic, Multi-Prophetic Clinic, Multi-Prophetic Clinic St. Petersburg Research Cardiology Center Medica
- All clinics and centers
- Multidisciplinary clinics
- Fetal medicine centers
- Radiology center
- Pain treatment clinic
- Cardiac center network
- Aesthetic medicine clinic 9090
- Multidisciplinary clinic, branch on Komendantsky pr.
 Petrozavodskaya d. 13
Petrozavodskaya d. 13
Address:
st. Petrozavodskaya, 13
Petrozavodskaya, 13
Petrogradskaya
Sports
Chkalovskaya
Opening hours:
Mon-VC 8.00-21.00
On holidays, the work schedule was changed
+7 (812) 458-00-00 +7 (999 (999 )063-15-77
About the branch
Available at the branch:
Network of cardio centers
Multidisciplinary clinic on Gzhatskaya
Address:
Gzhatskaya, 22 k.4, lit. A
Academic
Operating mode:
Mon-Fri from 8:00 to 21:00
Sat, Sun from 9:00 to 21:00
On public holidays the work schedule is changed
Phone:
For appointment: +7 (812) 458- 00-00 For inquiries: +7 (921) 992-22-79
th line of Vasilyevsky Island, 7
Vasileostrovskaya
Working hours:
Mon-Sun from 9:00 to 21:00
On holidays, the work schedule is changed
Phone:
For appointment: +7 (812) 458-00-00 For inquiries: +7 (921) 956-70-16
About the branch
Available at the branch:
Fetal Medicine Centers
Fetal Medicine Center on Myasnitskaya (Moscow)
Address:
Moscow, st. Myasnitskaya, 32, building 1
Myasnitskaya, 32, building 1
Chistye Prudy
Sretensky Boulevard
Turgenevskaya
Working hours:
Mon-Sun from 9:00 to 21:00
On holidays, the work schedule is changed
Phone:
For appointment: +7 (495) 215-12-15 For inquiries : +7 (495) 215-12-15
Email:
Vyborg, Leningradsky prospect, 10
Working hours:
Mon-Sun from 9:00 a.m. to 8:00 p.m. (921) 301-21-00
About the branch
Available at the branch:
Fetal Medicine Centers
Fetal Medicine Center at Siqueiros
Address:
st. Siqueirosa, 10, building 2
Ozerki
Working hours:
Mon-Sun from 9:00 to 20:00
On holidays, the work schedule is changed
Phone:
For appointment: +7 (812) 458-00-00 For inquiries: +7 (921) 908-35-55
About the branch
Available at the branch:
Fetal Medicine Centers
Fetal Medicine Center on Leni Golikova
Address:
st. Leni Golikova, d.0008 Phone:
Leni Golikova, d.0008 Phone:
For appointment: +7 (812) 458-00-00 +7 (921) 919-74-07
Comensdantsky pr.
Address:
Comenstatsky pr., 10, building 1
Pioneer
Old village
Comenskitan Prospekt
Opening hours:
Mon-AVS 9.00-21.00
On holidays. work changed
Phone:
For appointment: +7 (812) 458-00-00 For inquiries: +7 (921) 965-78-28
ave. Fetal Medicine Centers Multidisciplinary Clinics
Center for Radiation Diagnostics
Address:
Torez, d.0005
On holidays, the work schedule is changed
Phone:
For appointment: +7 (812) 458-00-00
Degtyarnoy
Address:
st. Degtyarnaya, 23
Ploshchad Vosstaniya
Opening hours:
Mon-Sun from 9:00 to 21:00
On holidays, the work schedule is changed
Phone:
For appointment: +7 (812) 458-00-00 For inquiries: +7 (921) 909-01-09
Multidisciplinary clinic on Bogatyrsky
Address:
Bogatyrsky pr. 0008 Phone:
0008 Phone:
For appointment: +7 (812) 458-00-00
About the branch
Available at the branch:
49
Prospekt Prosveshcheniya
Ozerki
Opening hours:
Mon-Sun 8.00-20.00
Opening hours changed on holidays
Phone:
For appointment:
inquiries: +7 (921) 952-52-20
About the branch
Available at the branch:
Pain treatment clinic
Badaeva, 6, building 1
Bolshevikov
Working hours:
Mon-Fri from 8:00 to 21:00
Sat-Sun from 9:00 to 21:00
Opening hours on holidays changed
Phone:
For appointment: +7 (812) 458-00-00 For inquiries: +7 (921) 952-52-20
About branch
Available at the branch:
Multidisciplinary Clinics Network of Cardiocenters Fetal Medicine Centers Aesthetic Medicine Clinic
Pulkovskaya, 8, building 1
Zvezdnaya
Working hours:
Mon-Fri from 8:00 to 21:00
Sat-Sun from 9:00 to 21:00
Opening hours on public holidays changed
Phone:
For appointment: +7 (812) 458-00-00 For inquiries: +7 (921) 965-78-28
About the branch
Available at the branch:
Multidisciplinary clinics Network of cardiac centers Fetal medicine centers Aesthetic medicine clinic
Make an appointment
Thank you for contacting us! We will contact you shortly.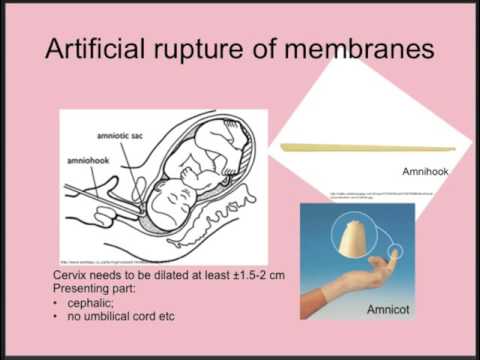
Leave a comment
Thank you, your feedback is very important to us
Apply for a job
Thank you for contacting us! We will contact you shortly.
Enroll in course
Thank you, your application has been sent successfully
Registration for the conference
Thank you, your application has been successfully sent
Ask a question
Thank you, we have submitted your question Petersburg [MEDICA]
What is chronic daily headache?
Chronic daily headache (CDH) is not a diagnosis. This is a term that includes headaches that occur 15 or more days a month for more than 3 months. nine0005
What are the types of chronic daily headache?
There are several types of HEGB and they differ in cause. The most common are chronic tension-type headache and headache associated with excessive use of drugs (painkillers) drugs (overuse headache). If you would like more information, there is an information leaflet on tension headache. Abusive headache can develop from migraine and tension headache. nine0005
Abusive headache can develop from migraine and tension headache. nine0005
Who gets HEGB?
Oddly enough, this condition is very common. Approximately one patient out of 20 develops this problem at some time in their life. HEGB is more common in women than in men; it can also develop in children.
What are the symptoms of CEHD?
The main manifestation is very frequent headaches. The pain can have different intensity, its character is usually dull. In addition to pain, there is often a feeling of fatigue, lightheadedness, irritability, and sleep disturbances. Sometimes a headache can be unbearable, although its severity may vary throughout the day. The intensity of the headache associated with excessive use of drugs, as a rule, is greatest in the morning. nine0005
Can HEGB pass?
The treatment of CEHD depends on the diagnosis and its cause. The selection of the right therapy is very important, so a doctor's supervision is necessary.
In all types of CEHD, pain medications and anti-migraine drugs can provide temporary relief, but in many cases the effect is only partial and passes quickly. Such treatment may worsen the condition.
Such treatment may worsen the condition.
If the headache is already caused by overuse of pain medications, these medications should be discontinued. Discontinuation of the "guilty" drug helps to reduce the frequency of headaches. nine0005
Do you need additional examinations?
Regardless of the current cause of chronic daily headache, there are no tests that confirm this diagnosis. Diagnosis is based on your description of the characteristics of the headache and accompanying symptoms, and the absence of any abnormalities on physical examination is mandatory. Try to describe your headache to the doctor in as much detail as possible. It is very important to let your doctor know how often and how much you are taking painkillers or other medications for your headache. nine0005
Your doctor will most likely tell you that you have nothing serious, that you just have a chronic daily headache. If the nature of your pain suddenly changes, or if the doctor is in doubt about the correctness of the diagnosis, he may prescribe additional tests for you, including neuroimaging (computed tomography or magnetic resonance imaging), to rule out other causes of headache.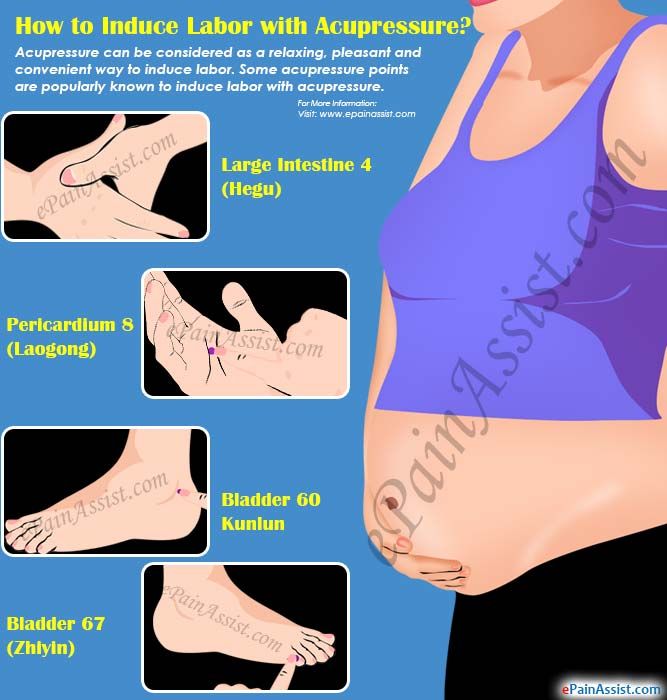 As a rule, this is not often necessary. If the doctor has not ordered additional studies, this means that he is confident in the diagnosis and conducting examinations will in no way facilitate the appointment of treatment. nine0005
As a rule, this is not often necessary. If the doctor has not ordered additional studies, this means that he is confident in the diagnosis and conducting examinations will in no way facilitate the appointment of treatment. nine0005
Read more
Samorukova
Ekaterina Mikhailovna
Neurologist, Tsephalgologist, Botulinotherapist
Toropova
Anna Albertovna
9000 9000 9000 9000 9000 9000 9000 9000
Neurologist, initial appointment
from 2,000 ₽
Neurologist, follow-up appointment
1,950 ₽ 1,700 ₽
Online consultation with a neurologist
2 200 ₽
Headache, extended consultation (90 min.)
4 200 ₽
All prices
What is headache associated with overuse of drugs (painkillers) (overuse headache)?
Any medication you take for headaches can cause overuse headache if taken very often over a long period of time.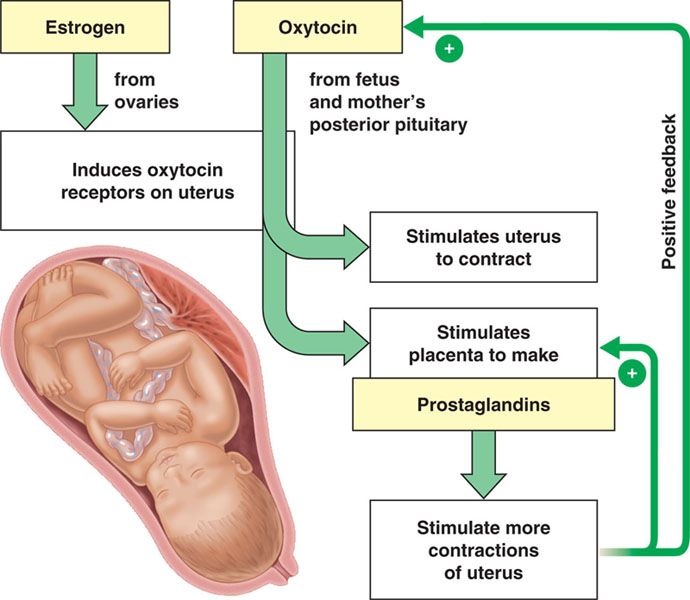 Aspirin, paracetamol, ibuprofen, codeine - virtually all overused analgesics can lead to this problem. However, it can be not only analgesics. Drugs intended for the specific treatment of a migraine attack, if abused, can also cause overuse headache. These drugs include triptans and, to a greater extent, ergotamine. nine0005
Aspirin, paracetamol, ibuprofen, codeine - virtually all overused analgesics can lead to this problem. However, it can be not only analgesics. Drugs intended for the specific treatment of a migraine attack, if abused, can also cause overuse headache. These drugs include triptans and, to a greater extent, ergotamine. nine0005
Similar headaches (although not exactly drug-induced headaches) can result from excessive caffeine intake. Usually caffeine enters the body with coffee, tea or cola, but it can also be contained in headache pills (combined analgesics).
The mechanism of development of drug-induced headache is not fully understood and may vary depending on the drug that caused this headache. Triptans or ergotamine preparations can cause withdrawal headaches: the pain returns after the drug wears off. It is assumed that analgesics cause changes in the brain systems that conduct pain impulses over time. Thus, drugs are beginning to be used to treat abuse headaches, and you need more and more pain pills. nine0005
nine0005
For most people with occasional headaches, analgesics are safe and effective. However, drug-induced headache can develop in anyone who takes analgesics more than 3 days a week. Patients with overbusy headache usually start with tension headache or, more commonly, migraine at the onset. For various reasons, headache attacks are becoming more and more frequent. This may be the natural course of the disease or due to the addition of another type of headache, possibly associated with stress or muscle tension. An increase in the frequency of pain attacks leads to an increase in medication to reduce existing symptoms, which, in the end, leads to daily and repeated use of drugs. nine0005 Many people in this situation realize that they are abusing drugs and try to stop taking them. This leads to the development of a withdrawal syndrome and an increase in headache, which again requires the use of an analgesic. It is easy to guess that there is a vicious circle that is very difficult to break. The only way to get rid of drug-induced headache is to stop the addictive drug; clinical studies have shown that the abolition of the "guilty" drug significantly improves well-being. However, it may take up to three months for you to feel the final improvement. Even if the headaches persist despite discontinuation of the drug, they become milder and more responsive to the right treatment. nine0005 You can stop the drug at once, or do it gradually, reducing the dose over 2-3 weeks. Whichever route you choose, drink plenty of fluids during this time (but avoid caffeinated drinks). When deciding to stop a drug, do not do so before a major event. Warn co-workers that you may not be at work for several days. If overuse of analgesics is the cause of your headache, then letting things take their course is not the answer. You will develop more frequent headaches that will no longer be relieved by analgesics and will not respond to preventive treatment. Over time, you can harm your body, such as damage your liver or kidneys. nine0005 Your doctor may prescribe certain drugs for you to take every day to help you stop taking painkillers. Drug-induced headache significantly alters the course of the primary headache (migraine or tension-type headache) for which you started taking pain medication. This means that after your abuse headache subsides after stopping the “guilty” drug, you will return to your original type of headache again. There are separate leaflets containing information about migraine and tension headache. nine0005 If necessary, you can safely start taking pain medication again as soon as the headache pattern improves, but not until a few weeks later. Be careful as there is a risk of the same condition developing again. To prevent this from happening, avoid taking painkillers more than three days in a row or on a regular basis more than three times a week. Do not forget to read the information on the packaging of the medicine and the instructions for using the drug. If the headache persists or comes back, do not take any medication yourself without consulting a doctor. Keeping a headache diary will help you gather important information about your headache: how often your headache occurs, when it occurs and how long it lasts, and what symptoms accompany it. This information is very valuable for making a correct diagnosis, identifying factors that provoke headaches and evaluating the effectiveness of treatment. nine0005 For people at high risk of drug-induced headache, keeping a diary is especially important as it gives an idea of how often and how much medication is taken.  It's not how much medication you take that matters: if you only use a full dose of an analgesic 1-2 days a week, you're unlikely to develop an overuse headache. But if you take only 2 tablets of an analgesic, but most of the time, then the likelihood of developing a drug-induced headache will increase significantly. Thus, the problem is the frequent use of drugs for a long time. nine0005
It's not how much medication you take that matters: if you only use a full dose of an analgesic 1-2 days a week, you're unlikely to develop an overuse headache. But if you take only 2 tablets of an analgesic, but most of the time, then the likelihood of developing a drug-induced headache will increase significantly. Thus, the problem is the frequent use of drugs for a long time. nine0005 What can you do to help yourself?
 If you stop the drug at the same time, read for sure, you will experience withdrawal symptoms: increased headache, nausea, possibly vomiting, anxiety, sleep disturbances. These symptoms occur within 48 hours of withdrawal and persist for a maximum of two weeks. However, patients who attempt to slowly withdraw the drug are more likely to experience failure, possibly because it takes longer. nine0005
If you stop the drug at the same time, read for sure, you will experience withdrawal symptoms: increased headache, nausea, possibly vomiting, anxiety, sleep disturbances. These symptoms occur within 48 hours of withdrawal and persist for a maximum of two weeks. However, patients who attempt to slowly withdraw the drug are more likely to experience failure, possibly because it takes longer. nine0005 What happens if you leave everything as it is?
What other treatments are available?
 But these drugs will only work if you stop taking all pain medications.
But these drugs will only work if you stop taking all pain medications. Can you be sure that the headache will never come back?
 nine0005
nine0005 Keeping a headache diary
Petrogradskaya
Sports
Chkalovskaya
Opening hours:
Mon-VC 8.00-21.00
On holidays, the work schedule changed
phone:
+7 (812) 458-00-00-00-00-00-00-00-00-00-00-00-00-00-00-00-00-00-00 +7(999)063-15-77
About the branch
Available at the branch:
Network of cardio centers
Multidisciplinary clinic on Gzhatskaya
Address:
Gzhatskaya, 22 k.4, lit. A
Academic
Opening hours:
Mon-Fri from 8:00 to 21:00
Sat, Sun from 9:00 to 21:00
Opening hours on public holidays are changed
Phone:
records: +7 (812) 458-00-00 For inquiries: +7 (921) 992-22-79
About the branch
Available in the branch:
Multidisciplinary clinics Network of cardiac centers Fetal medicine centers
Center for fetal medicine on Vasilevsky Island
Address:
14th line of Vasilevsky Island, 7
Vasileostrovskaya
Mon-Fri
until 21:00
On holidays, the work schedule is changed
Phone:
For appointments: +7 (812) 458-00-00 For inquiries: +7 (921) 956-70-16
About the branch
Available at the branch:
Fetal Medicine Centers
Fetal Medicine Center on Myasnitskaya (Moscow)
Address:
Moscow, st. Myasnitskaya, 32, bldg. 1
Myasnitskaya, 32, bldg. 1
Chistye Prudy
Sretensky Boulevard
Turgenevskaya
Working hours:
Mon-Sun from 9:00 to 21:00
work schedule is changed on public holidays
For appointment: +7 (495) 215-12-15 For inquiries: +7 (495) 215-12-15
Email:
About the branch
Available at the branch:
Fetal Medicine Centers
Fetal Medicine Center in Vyborg
Address:
Vyborg, Leningradsky Prospekt, 10
Working hours:
Mon-Sun
until 20:00
On holidays, the work schedule is changed
Phone:
For appointments: +7 (812) 458-00-00 For inquiries: +7 (921) 301-21-00
About the branch
Available at the branch:
Fetal Medicine Centers
Center for Fetal Medicine at Siqueiros
Address:
st. Siqueirosa, d. 10, k. 2
Siqueirosa, d. 10, k. 2
Ozerki
Working hours:
Mon-Sun from 9:00 to 20:00
On holidays, the work schedule is changed
Phone:
For appointment: +7 ( 812) 458-00-00 For inquiries: +7 (921) 908-35-55
About the branch
Available at the branch:
Fetal Medicine Centers
Fetal Medicine Center on Leni Golikova
Address:
St. Leni Golikova, d. 812) 458-00-00 +7 (921) 919-74-07
., d. 10, k. 1
Pioneer
Old village
Komendantsky Prospekt
Opening hours:
Mon-SS 9.00-21.00
Work schedule changed
phone:
for recording: +7 (812) 458-00-00-00 For inquiries: +7 (921) 965-78-28
About the branch
Available at the branch:
0005
Address:
Ave. Toreza, 72
Specific
Courage area
Opening hours:
Mon-PT 8. 00-21.00
00-21.00
SB-Sun 8.00-20.00
On holidays, the work schedule was changed
for recording: +7 (812) 458-00-00
About the branch
Available in the branch:
Network of Cardiocenters Center for Radiation Diagnostics
Aesthetic Medicine Clinic on Degtyarnaya
Address:
st. Degtyarnaya, d. -00-00 For inquiries: +7 (921) 909-01-09
d.64 k.1
Komendantsky Prospekt
Old village
Cunning
Opening hours:
On holidays, the work schedule changed
phone:
for recording: +7 (812) 458-00-00
About the branch
V. branch available:
Multidisciplinary clinics
Clinic for the treatment of pain on Lunacharskogo
Address:
Lunacharskogo Ave., 49
0005
Mon-Sun 8.00-20.00
Opening hours changed on holidays
Phone:
For appointments: +7 (812) 458-00-00 For inquiries: +7 (921) 952-52-20
About the branch
Available in the branch:
Pain treatment clinic
Badaeva, 6, building 1
Bolshevikov
Working hours:
Mon-Fri from 8:00 to 21:00
Sat-Sun from 9:00 to 21:00
On holidays, the work schedule is changed
Phone:
For appointment: +7 (812) 458-00-00 For inquiries: +7 (921) 952-52-20
About the branch
Available at the branch:
Multidisciplinary clinics Network of cardio centers Fetal medicine centers Aesthetic medicine clinic
Multidisciplinary clinic at Pulkovskoy
Pulkovskaya, 8, building 1
Zvezdnaya
Working hours:
Mon-Fri from 8:00 to 21:00
Sat-Sun from 9:00 to 21:00
On holidays, the work schedule is changed
Phone:
For appointments: +7 (812) 458-00-00 For inquiries: +7 (921) 965- 78-28
About the branch
Available at the branch:
Multidisciplinary clinics Network of cardiac centers Fetal medicine centers Aesthetic medicine clinic
Make an appointment
Thank you for contacting us! We will contact you shortly.