How to tell if your child has rsv
RSV: When It's More Than Just a Cold
By: Andrea Jones, MD, FAAP
Almost all children get RSV at least once before they are 2 years old. For most healthy children, RSV is like a cold. But, some children get very sick with RSV.
What is RSV?
RSV (or respiratory syncytial virus) is one of the many viruses that cause respiratory illness―illnesses of the nose, throat and lungs. This virus usually occurs in the late fall through early spring months, but can vary in different parts of the country.
With mask-wearing and physical distancing for COVID-19, there were fewer cases of RSV in 2020. However, once safety measures relaxed with the arrival of COVID-19 vaccines, a rise in RSV cases began in spring 2021. The spread of RSV and other seasonal
respiratory illnesses like influenza (flu) has also started earlier than usual this year.
RSV symptoms in babies
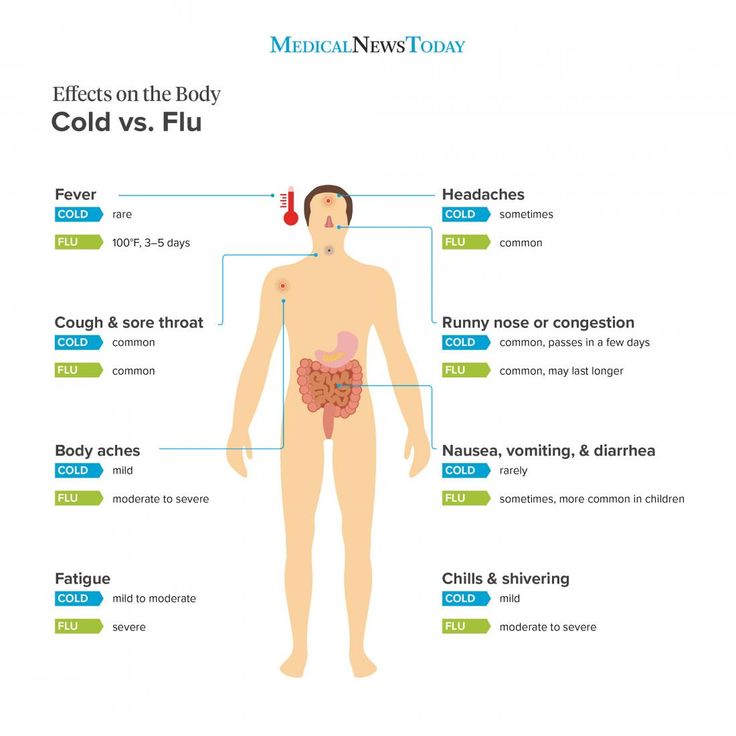
Typically, RSV causes a
cold, which may be followed by
bronchiolitis or pneumonia. Symptoms generally last an average of 5-7 days.
Cold symptoms may include: | May include
cold symptoms, plus:
|
Chest wall retractions happen when a baby must use muscles between the ribs or in the neck to breathe. It is a sign that your baby is having to work harder than normal to breathe.
Watch your child's rib cage as they inhale. If you see it "caving in" and forming an upside-down "V" shape under the neck, then they are working too hard. |
Is your baby or young child at a greater risk of this respiratory illness?
Infants with a higher risk for severe RSV infection include:
12 weeks old or younger at the start of RSV season
Premature or low birth weight infants (especially those born before 29 weeks gestation)
Chronic lung disease of prematurity
Babies with certain types of heart defects
Those with weak immune systems due to illness or treatments
Additional risk factors for severe RSV infections include low birth weight, having siblings, a mother's smoking during pregnancy, exposure to secondhand smoke in the home, history of allergies and eczema, not breastfeeding, and being around children in a child care setting or living in crowded living conditions.
When should you call the doctor?
RSV symptoms are typically at their worst on days 3 through 5 of illness. Fortunately, almost all children recover from an RSV infection on their own.
Call your pediatrician right away if your child has any:
Symptoms of bronchiolitis (listed above)
Symptoms of dehydration (fewer than 1 wet diaper every 8 hours)
Pauses or difficulty breathing
Gray or blue color to tongue, lips or skin
Significantly decreased activity and alertness
Some children with RSV may be at increased risk of developing a bacterial infection, such as an
ear infection. Call your doctor if your child has:
Symptoms that worsen or do not start to improve after 7 days
A fever (with a rectal temperature of 100.
 4°F or higher) and they are younger than 3 months of age (12 weeks).
4°F or higher) and they are younger than 3 months of age (12 weeks). A fever that rises above 104°F repeatedly for a child of any age.
Poor sleep or fussiness, chest pain, ear tugging or ear drainage
How do doctors diagnose RSV?
Pediatricians diagnose children with a cold or bronchiolitis by asking about their symptoms and by doing a physical exam. Your pediatrician may do a nasal swab test to determine if your child has RSV or another virus. A chest x-ray and/or oxygen saturation test may also be done to check for lung congestion. Because most children recover without difficulty and because there is no treatment for RSV, these tests usually are not necessary.
Is RSV contagious?
Yes. RSV spreads just like a common-cold virus―from one person to another. It enters the body through the nose or eyes or, usually from:
Direct person-to-person contact with saliva, mucus, or nasal discharge.
Unclean hands (RSV can survive 30 minutes or more on unwashed hands).
Unclean objects or surfaces (RSV can survive up to 6 hours on surfaces, toys, keyboards, door knobs, etc).
Symptoms can appear 2 to 8 days after contact with RSV. According to the U.S. Centers for Disease Control and Prevention (CDC), people infected with RSV are usually contagious for 3 to 8 days. However, some infants and people with weakened immune systems can be contagious for as long as four weeks―even if they are not showing symptoms.
Keep in mind, children and adults can get RSV multiple times–even during a single season. Often, however, repeat infections are less severe than the first one.
What can you do to help your child feel better?
There is no cure for RSV and medications, like steroids and antibiotics, do not help with RSV.
To help your child feel more comfortable, begin by doing what you would for any bad cold:
Nasal saline with gentle suctioning to allow easier breathing and feeding.
Cool-mist humidifier to help break up mucus and allow easier breathing.
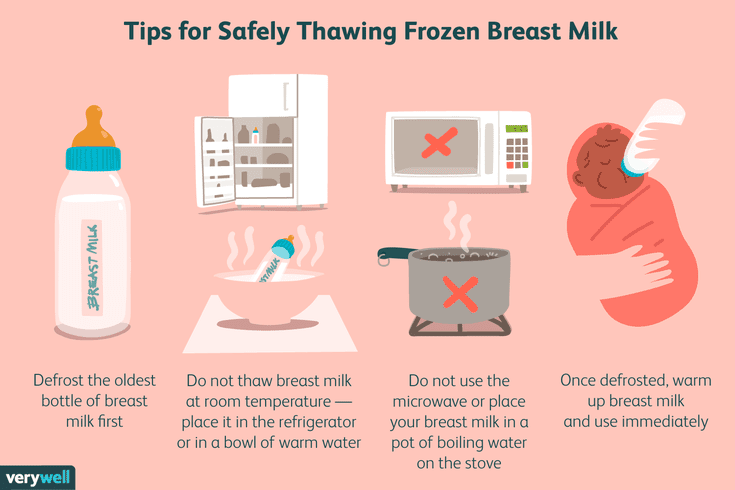
Fluids & frequent feedings. Make sure your child is staying hydrated. Infants with a common cold may feed more slowly or not feel like eating because they are having trouble breathing. Try to section baby's nose before trying to breast or bottle-feed. Supplementing with water or formula is unnecessary for breastfed babies. If difficult for the baby to feed at the breast, expressing breastmilk into a cup or bottle may be an option.
Acetaminophen or ibuprofen (if older than 6 months) to help with low-grade fevers. Always avoid aspirin and cough and cold medications.
Do babies with RSV need to be hospitalized?
Only
1% to 2% of children younger than 6 months of age with RSV infection may require a
hospital stay. Those babies may need
oxygen to help with breathing or an (intravenous) IV line for fluids. Most of these children can go home after 2 or 3 days. Rarely, a child may need care in a pediatric intensive care unit (PICU).
Most of these children can go home after 2 or 3 days. Rarely, a child may need care in a pediatric intensive care unit (PICU).
How can you protect your children from RSV?
Wash your hands! Just as you would to prevent germs at any time, use soap and water and scrub for at least 20 seconds. Remind children to practice good hand hygiene all through the year.
Other ways to help prevent RSV
Vaccinate. Keep your children up to date on their immunizations and get the whole family annual flu shots. Getting vaccinated with Tdap―to protect against whooping cough is especially important for adults who are around infant—new parents, grandparents, babysitters, nannies, etc. Your child should also be immunized against COVID-19.
Limit your baby's exposure to crowds, other children, and anyone with colds. Keep them home from school or child care when they are sick and teach them to cover their coughs and sneezes.
Go germ-free. Disinfect objects and surfaces in your home regularly and avoid exposing your child to smoke from tobacco or other substances.
Feed your baby breastmilk. It has unique antibodies to prevent and fight infections.
Monoclonal antibody injections for high-risk infants
There is a monoclonal antibody treatment that may reduce the risk of severe RSV infection in some high-risk infants. Your pediatrician will let you know if your baby is a candidate.
Hope on the horizon for RSV
Medicine is always advancing! Scientists are currently studying vaccines to prevent and medications to treat RSV. We may have more options in the future. In the meantime, rest assured that most children recover well from RSV and grow to be healthy adults.
More information
-
COVID, Flu & RSV: How Are These Respiratory Illnesses Different?
- Treating Bronchiolitis in Infants
-
HealthyChildren.
 org Parent Webinar on RSV
org Parent Webinar on RSV -
RSV in Infants and Young Children (CDC)
About Dr. Jones:
Andrea N. Jones, MD, FAAP, is a board-certified general pediatrician. She is an Assistant Professor in the Department of Pediatrics at the University of Wisconsin School of Medicine and Public Health. Dr. Jones is a member of the Wisconsin Chapter of the American Academy of Pediatrics.
|
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Breastfeeding Benefits Your Baby’s Immune System
Log in | Register
Ages & Stages
Ages & Stages
By: Claire McCarthy, MD, FAAP
Breast milk is the food naturally designed to best meet the needs of human babies. It has all the necessary nutrients, in just the right amounts, and is easy to digest. Beyond the nutritional benefits, here's a great bonus: Breast milk also helps build and support your baby's immune system. Read on to learn how.
It has all the necessary nutrients, in just the right amounts, and is easy to digest. Beyond the nutritional benefits, here's a great bonus: Breast milk also helps build and support your baby's immune system. Read on to learn how.
Breast milk: food & infection fighter
Breast milk contains antibodies that can fight infection. Those antibodies are present in high amounts in colostrum, the first milk that comes out of the breasts after birth. However, there are antibodies in breastmilk the entire time a mother continues to nurse. Through these antibodies, the mother can pass on some protection from infectious illness she had in the past, and those she gets while breastfeeding. Breast milk can literally give babies a head start in preventing and fighting infections.
Breast milk also is made up of other proteins, fats, sugars and even white blood cells that work to fight infection in many different ways. They are especially helpful in fighting gastrointestinal infections, since breast milk heads right to the stomach and intestine when your baby eats. The different factors in breast milk work directly within the intestine before being absorbed and reaching the entire body. This also sets the stage for a protective and balanced immune system that helps recognize and fight infections and other diseases even after breastfeeding ends.
The different factors in breast milk work directly within the intestine before being absorbed and reaching the entire body. This also sets the stage for a protective and balanced immune system that helps recognize and fight infections and other diseases even after breastfeeding ends.
Other factors in breast milk directly stimulate and support the immune system. These include lactoferrin and interleukin-6, -8 and -10. These proteins help to balance the immune system inflammatory response, which is needed for immune function but can be damaging in excess.
There's even evidence that nursing mothers who are vaccinated against COVID-19 can pass along antibodies to the virus through breast milk. Although it's not proven, these antibodies may help protect babies too young for the vaccine. (See Breastfeeding During the COVID-19 Pandemic.")
Is breastmilk probiotic?
Breast milk has "probiotic" factors, too. Some support the immune system and others serve as a nutrient source for healthy bacteria in the body, called the human microbiome. The healthy microbiome can play a lifelong role in not only preventing infection, but also in decreasing the risk of
allergies, asthma,
obesity and other chronic diseases.
The healthy microbiome can play a lifelong role in not only preventing infection, but also in decreasing the risk of
allergies, asthma,
obesity and other chronic diseases.
With all these immunity-boosting factors in breast milk, it is not surprising that breastfed babies are less likely to suffer from ear infections, vomiting, diarrhea, pneumonia, urinary tract infections, and certain types of meningitis. Research also shows that children who nurse for more than six months are less likely to develop childhood leukemia and lymphoma than those who receive formula. This may be in part because these types of cancer are affected by disruptions to the immune system.
Remember
To help keep babies healthy, communities can take steps to support mothers who choose to breastfeed their babies. This can include offering paid leave and giving employees places and time to pump breast milk. If you're breastfeeding your baby or have any questions, never hesitate to talk with your pediatrician. If you can't breastfeed, or for personal reasons choose not to, talk to your pediatrician about the many other ways to support your baby's health.
If you can't breastfeed, or for personal reasons choose not to, talk to your pediatrician about the many other ways to support your baby's health.
More information
- Breastfeeding: AAP Policy Explained
- Breastfeeding During the COVID-19 Pandemic
About Dr. McCarthy
Claire McCarthy, MD, FAAP is a primary care pediatrician at Boston Children's Hospital, an Assistant Professor of Pediatrics at Harvard Medical School, a senior editor for Harvard Health Publications, and an official spokesperson for the American Academy of Pediatrics. She writes about health and parenting for the Harvard Health Blog, Huffington Post and many other online and print publications.
- Last Updated
- 7/19/2022
- Source
- American Academy of Pediatrics (Copyright © 2020)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Updated calculation of insurance premiums - 2022 - SKB Kontur
April 18, 2022 118,070
What is the procedure for submitting an updated calculation when the base for calculating insurance premiums for previous reporting periods is reduced? What to do with negative values and what to do if an error is made in the personal data of the insured, they forgot to include an employee in the calculation or included an extra one?
When it is necessary to submit an updated calculation
The payer is obliged to make the necessary changes and submit an updated calculation to the tax authority in the manner prescribed by Art. 81 of the Tax Code of the Russian Federation, if the following facts are found in the calculation submitted by him (clause 1.2 of the Procedure for filling out the calculation of insurance premiums, approved by Order of the Federal Tax Service of Russia dated 06. 10.2021 N ED-7-11/875@, hereinafter referred to as the Procedure):
10.2021 N ED-7-11/875@, hereinafter referred to as the Procedure):
- failure to reflect or incomplete reflection of information;
- errors that lead to an underestimation of the amount of insurance premiums payable;
- as well as downward recalculation of the base for the previous period, such explanations are given by the Federal Tax Service in a letter dated 08.24.2017 No. BS-4-11/16793@.
Contents of the revised calculation
The revised calculation includes those sections and annexes to them that were presented earlier, except for Section 3, taking into account the changes made. Other sections and appendices may be included if changes have been made to them. nine0005
Section 3 "Personalized information about insured persons" is included only in relation to those individuals for whom changes have occurred (clause 1.2 of the Procedure).
Fill out, check and submit RSV free of charge via the Internet
Try
How to act in case of incomplete reflection of information
on insurance premiums. In this case, it is necessary to accrue and pay contributions at the appropriate rate (4%), and then make the necessary changes and submit an updated calculation to the tax authority. nine0005
In this case, it is necessary to accrue and pay contributions at the appropriate rate (4%), and then make the necessary changes and submit an updated calculation to the tax authority. nine0005
Include section 1 with the same appendices and subsections that were originally submitted for the 1st quarter in the revised calculation, completing lines 060-073 in section 1, and supplement Annex 1 with subsection 1.3.2.
A section 3 of the employee shall be supplemented with subsection 3.2.2 - information on the base for calculating contributions at an additional rate.
How to proceed with downward recalculation
In case of adjustment of the base for calculating insurance premiums for previous reporting periods, an updated calculation for this period is submitted. In the calculation for the current reporting period, the amount of the recalculation made for the previous period is not reflected. When filling in the indicators of the calculation lines, negative values are not provided (clause 1. 13 of the Procedure). nine0005
13 of the Procedure). nine0005
Files containing negative amounts are considered out of format. Such requirements of the Federal Tax Service are included in the schema of the xml file.
Let's say that in July they recalculated the vacation pay accrued in June to a retired employee. The result was a negative base and assessed contributions. It is necessary to submit to the Federal Tax Service an updated calculation for half a year with reduced amounts, and in the calculation for 9 months, take this into account in the columns “Total from the beginning of the billing period”.
Let's go back to the above example. In this case, when filling out the revised calculation, the indicators of the previously submitted calculation for the six months are adjusted. Section 3 is included in it, containing information regarding the person to whom the recalculation was made, with correct indicators (reduced amounts) in subsection 3.2:
- in line 140 for month 3 (June) the amount of payments reduced by the difference received as a result of recalculation of vacation pay;
- in line 150 the reduced amount of the base for calculating contributions;
- in line 170 is the reduced amount of contributions.
In section 1, in appendices 1 and 2, indicate the reduced values in the columns relating to the 3rd month and in the columns "Total since the beginning of the billing period".
How contribution reporting will change in 2023
Read article
What to do if you forgot to include an employee in the calculation
For example, when submitting a calculation for half a year, they did not include information about the remuneration to an individual who provided services under a GPC agreement in May. In this case, when filling out the revised calculation, the indicators of the previously submitted calculation for the six months are adjusted. Section 3 is included in it, containing information regarding the person who was forgotten to be included in the initial calculation. In subsection 3.2.1 indicate:
- in line 120 is the serial number of the month "2";
- in line 140 the amount of remuneration;
- in line 150 the amount of the base for calculating contributions;
- in line 160 the amount of the base, including under the GPC agreement;
- in line 170 the amount of contributions.
In section 1, in appendices 1 and 2, the increased values are indicated in the columns relating to the 2nd month and in the columns "Total since the beginning of the billing period".
Report for employees through Kontur.Extern. Loading data into RSV from SZV-M. Zero RSV in no time. nine0005
Register
What to do if you made a mistake in the employee’s personal data
If you find inaccurate information or errors in the calculation submitted to the tax authority that do not lead to an underestimation of the amount of insurance premiums payable, the payer has the right (but is not obliged) to make the necessary changes in the calculation and submit to the tax authority an updated calculation (clause 1.2 of the Procedure).
Such errors include inaccurate personal data of insured persons specified in subsection 3.1, with the exception of SNILS and full name ). nine0005
If the calculation accepted by the Federal Tax Service indicated incorrect TIN, date of birth, citizenship or passport data, then include section 3 of the employee whose information was incorrect in the revised calculation. In lines 020, 070 -110, indicate the correct values (do not indicate the cancellation flag in line 010). The amounts in subsection 3.2, in section 1 and annexes to section 1 are left unchanged.
In lines 020, 070 -110, indicate the correct values (do not indicate the cancellation flag in line 010). The amounts in subsection 3.2, in section 1 and annexes to section 1 are left unchanged.
Extern
Submission of any type of reporting to all regulatory authorities: Federal Tax Service, Pension Fund of the Russian Federation, FSS, Rosstat, RAR, RPN
Learn more
External
Submission of any type of reporting to all regulatory authorities: Federal Tax Service, Pension Fund of the Russian Federation, FSS, Rosstat, RAR, RPN
Learn more
RS-virus hos barn - RSV in children
RS-virus hos barn - ryska
Infectioner med RS-virus är mycket vanliga. De flesta barn blir sjuka som vid en förkylning. En del barn kan bli mycket sjuka och behöva få vård på sjukhus.
Här kan du läsa den här texten på svenska.
RSV is most common in autumn and winter. nine0005
nine0005
Symptoms
RSV may resemble the common cold. However, children under six months of age can have a hard time with the disease. Recovery often takes several weeks.
First symptoms of RSV:
- The child develops a runny nose and stuffy nose.
- The temperature is rising.
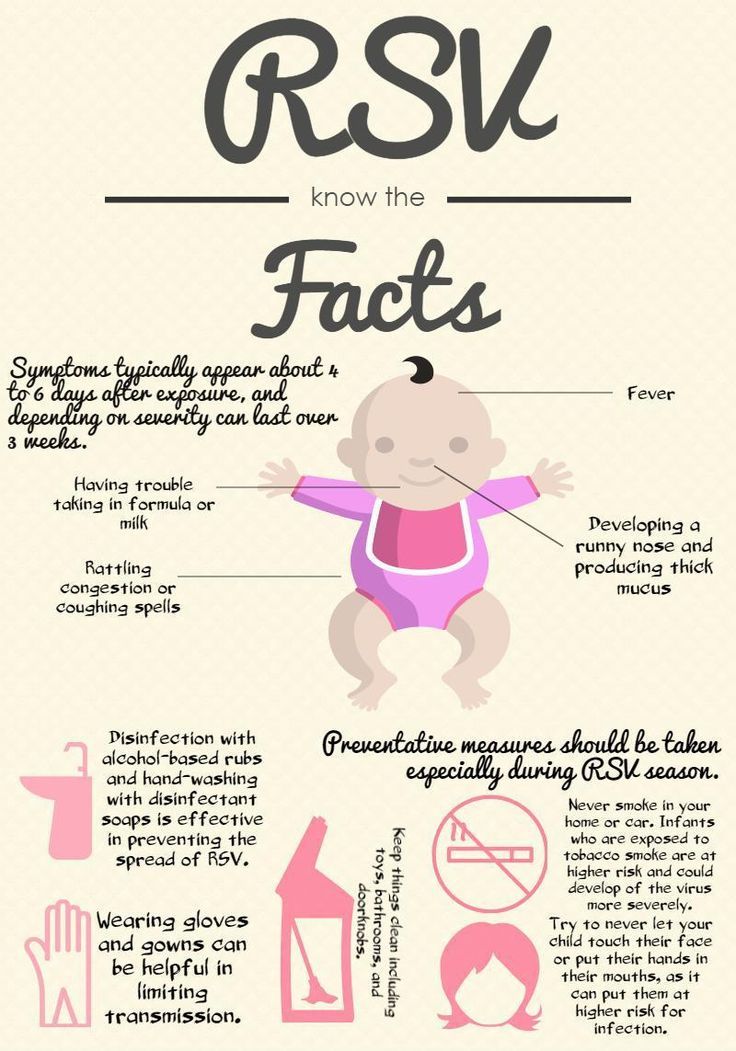
- Baby has difficulty breastfeeding, eating or drinking. The child is tired.
In the first few days, the child's symptoms can be very severe. Breathing problems may occur. This may manifest itself in the following ways:
- The child has rapid breathing.
- When breathing, the abdomen expands and falls.
- The child seems to have difficulty breathing.
Some children may experience pauses in breathing. In this case, the child completely stops breathing for a short time.
In this case, the child completely stops breathing for a short time.
Severe cough
RSV may cause severe cough. It may begin a few days after the child has the first symptoms. The child may cough heavily for several weeks. nine0005
When and where to seek medical help?
Most people with RSV do not require medical attention. The disease usually goes away on its own.
In the following cases, urgently need to contact the medical center:
- The child is less than 3 months old and has a fever.
- The child has difficulty breathing.
- The baby cannot breastfeed, drink or eat.
If the health center is closed or unable to see you, go to the emergency room. nine0005
Emergency
Call 112 immediately if your child is short of breath.
Advice on
If you don't know what to do, call 1177 for advice. The nurse will answer you. If necessary, she can tell you where to go for medical help.
The nurses speak Swedish and English. Sometimes it is possible to get help in other languages. nine0005
If you are calling from a foreign number, dial 00 46 771 11 77 00.
How can I help my child at home?
Here are some tips:
- Use saline spray or drops. This helps if the child has a stuffy nose.
- Use a special suction to remove nasal mucus.
 It can be purchased at a pharmacy.
It can be purchased at a pharmacy.
- To sleep, lay the child so that the head is higher than the body. You can add extra pillows to the bed. nine0015
- Give your child to drink frequently.
 For example, breastfeed or give formula milk more often than usual.
For example, breastfeed or give formula milk more often than usual. - If the child eats little at one meal, feed him more often.
- If the child is very unwell with a fever, give him antipyretic drugs.
 Check with pharmacy staff. If the child is less than six months old, consult a doctor.
Check with pharmacy staff. If the child is less than six months old, consult a doctor.
How is RSV transmitted?
RSV can be transmitted when an infected person sneezes or coughs and small droplets of liquid containing the virus enter the atmosphere. If these droplets enter your body, you can become infected. nine0005
RSV can also be spread when you touch someone who is sick, such as holding hands. The virus can get into your mouth or nose if you touch your face with your hands.
You can reduce your risk of getting RSV
Here's how you can reduce your risk of getting RSV:
- Wash your hands frequently.

- Keep your distance from other people, especially indoors.
- Avoid contact with people with a cold.
- Prioritize outdoor activities.
 nine0015
nine0015
Sometimes the course of the disease in children can be severe
The risk of a severe course of the disease is increased if:
- The child is less than three months old.
- The baby is less than a year old and was born more than five weeks prematurely.

- The child has a heart, lung or nervous system disorder.
It is especially important to protect children at risk.
Treatment
Children who are severely ill may need to be hospitalized. In the hospital, the child is helped to receive fluids and nutrition. nine0005
If the child is having difficulty breathing, he or she will receive appropriate help.
Antivirals
There are medicines that prevent a child from getting sick. They are administered in a hospital. Children at risk of a severe course may need to be treated with this drug.