How to spot a child abuser
Child abuse - Symptoms and causes
Overview
Mayo Clinic Center for Safe and Healthy Children and Adolescents
Any intentional harm or mistreatment to a child under 18 years old is considered child abuse. Child abuse takes many forms, which often occur at the same time.
- Physical abuse. Physical child abuse occurs when a child is purposely physically injured or put at risk of harm by another person.
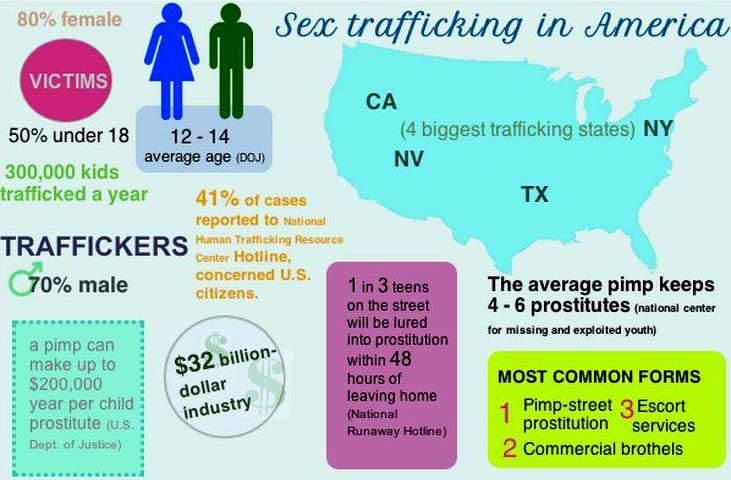
- Sexual abuse. Child sexual abuse is any sexual activity with a child. This can involve sexual contact, such as intentional sexual touching, oral-genital contact or intercourse. This can also involve noncontact sexual abuse of a child, such as exposing a child to sexual activity or pornography; observing or filming a child in a sexual manner; sexual harassment of a child; or prostitution of a child, including sex trafficking.
- Emotional abuse.
Emotional child abuse means injuring a child's self-esteem or emotional well-being. It includes verbal and emotional assault — such as continually belittling or berating a child — as well as isolating, ignoring or rejecting a child.
- Medical abuse. Medical child abuse occurs when someone gives false information about illness in a child that requires medical attention, putting the child at risk of injury and unnecessary medical care.
- Neglect. Child neglect is failure to provide adequate food, clothing, shelter, clean living conditions, affection, supervision, education, or dental or medical care.
In many cases, child abuse is done by someone the child knows and trusts — often a parent or other relative. If you suspect child abuse, report the abuse to the proper authorities.
Products & Services
- Book: Mayo Clinic Guide to Raising a Healthy Child
Symptoms
A child who's being abused may feel guilty, ashamed or confused. The child may be afraid to tell anyone about the abuse, especially if the abuser is a parent, other relative or family friend. That's why it's vital to watch for red flags, such as:
The child may be afraid to tell anyone about the abuse, especially if the abuser is a parent, other relative or family friend. That's why it's vital to watch for red flags, such as:
- Withdrawal from friends or usual activities
- Changes in behavior — such as aggression, anger, hostility or hyperactivity — or changes in school performance
- Depression, anxiety or unusual fears, or a sudden loss of self-confidence
- Sleep problems and nightmares
- An apparent lack of supervision
- Frequent absences from school
- Rebellious or defiant behavior
- Self-harm or attempts at suicide
Specific signs and symptoms depend on the type of abuse and can vary. Keep in mind that warning signs are just that — warning signs. The presence of warning signs doesn't necessarily mean that a child is being abused.
Physical abuse signs and symptoms
- Unexplained injuries, such as bruises, broken bones (fractures) or burns
- Injuries that don't match the given explanation
- Injuries that aren't compatible with the child's developmental ability
Sexual abuse signs and symptoms
- Sexual behavior or knowledge that's inappropriate for the child's age
- Pregnancy or a sexually transmitted infection
- Genital or anal pain, bleeding, or injury
- Statements by the child that he or she was sexually abused
- Inappropriate sexual behavior with other children
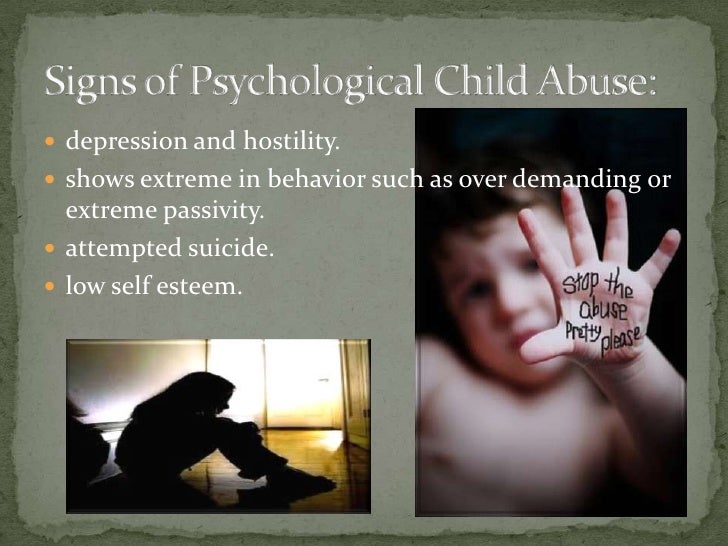
Emotional abuse signs and symptoms
- Delayed or inappropriate emotional development
- Loss of self-confidence or self-esteem
- Social withdrawal or a loss of interest or enthusiasm
- Depression
- Avoidance of certain situations, such as refusing to go to school or ride the bus
- Appears to desperately seek affection
- A decrease in school performance or loss of interest in school
- Loss of previously acquired developmental skills
Neglect signs and symptoms
- Poor growth
- Excessive weight with medical complications that are not being adequately addressed
- Poor personal cleanliness
- Lack of clothing or supplies to meet physical needs
- Hoarding or stealing food
- Poor record of school attendance
- Lack of appropriate attention for medical, dental or psychological problems or lack of necessary follow-up care
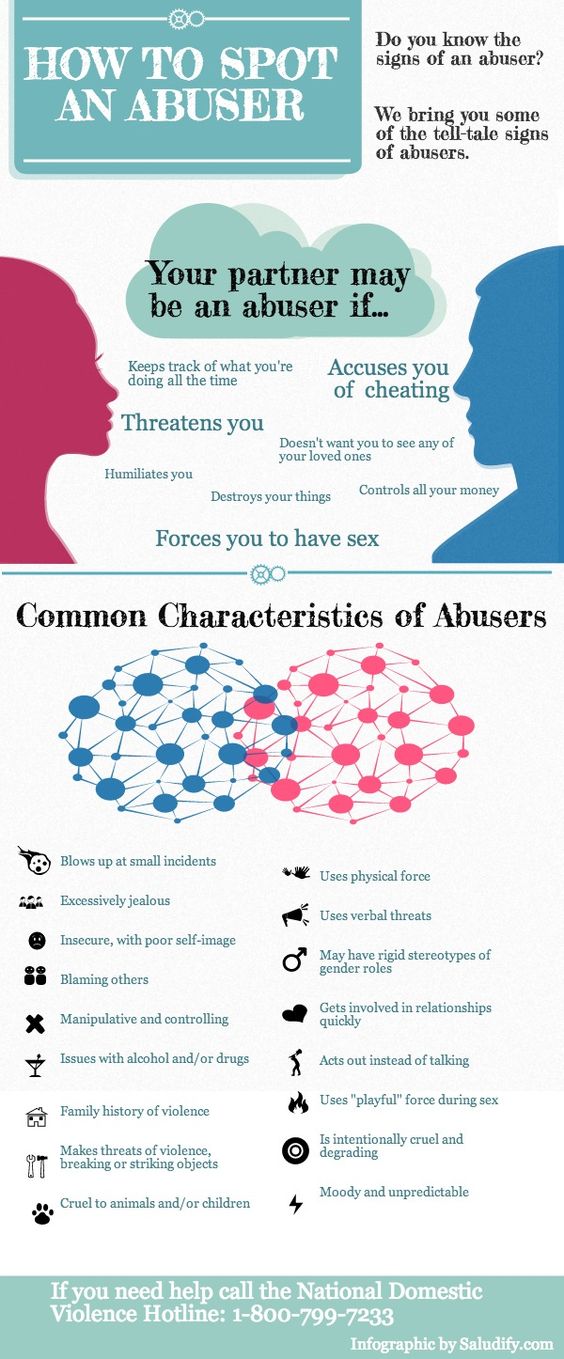
Parental behavior
Sometimes a parent's demeanor or behavior sends red flags about child abuse.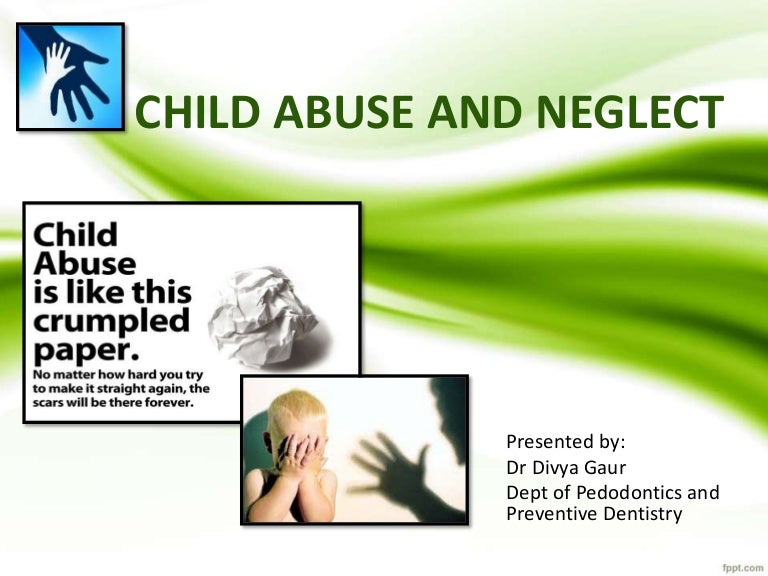 Warning signs include a parent who:
Warning signs include a parent who:
- Shows little concern for the child
- Appears unable to recognize physical or emotional distress in the child
- Blames the child for the problems
- Consistently belittles or berates the child, and describes the child with negative terms, such as "worthless" or "evil"
- Expects the child to provide attention and care to the parent and seems jealous of other family members getting attention from the child
- Uses harsh physical discipline
- Demands an inappropriate level of physical or academic performance
- Severely limits the child's contact with others
- Offers conflicting or unconvincing explanations for a child's injuries or no explanation at all
- Repeatedly brings the child for medical evaluations or requests medical tests, such as X-rays and lab tests, for concerns not seen during the health care provider's examination
Physical punishment
Child health experts condemn the use of violence in any form, but some people still use physical punishment, such as spanking, to discipline their children. While parents and caregivers often use physical punishment with the intention of helping their children or making their behavior better, research shows that spanking is linked with worse, not better, behavior. It's also linked to mental health problems, difficult relationships with parents, lower self-esteem and lower academic performance.
While parents and caregivers often use physical punishment with the intention of helping their children or making their behavior better, research shows that spanking is linked with worse, not better, behavior. It's also linked to mental health problems, difficult relationships with parents, lower self-esteem and lower academic performance.
Any physical punishment may leave emotional scars. Parental behaviors that cause pain, physical injury or emotional trauma — even when done in the name of discipline — could be child abuse.
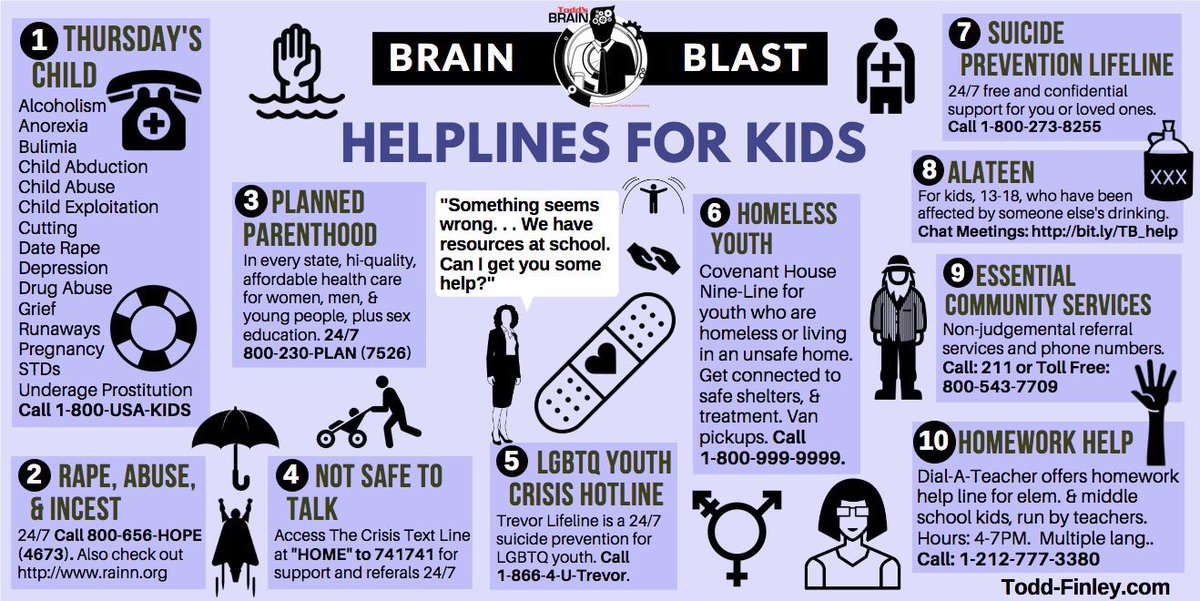
When to see a doctor
If you're concerned that your child or another child has been abused, seek help immediately. Depending on the situation, contact the child's health care provider, a local child welfare agency, the police department or a 24-hour hotline for advice. In the United States, you can get information and assistance by calling or texting the Childhelp National Child Abuse Hotline at 1-800-422-4453.
If the child needs immediate medical attention, call 911 or your local emergency number.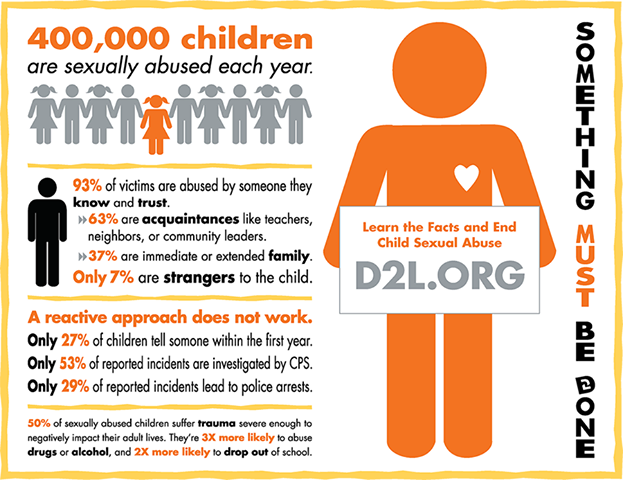
In the United States, keep in mind that health care professionals and many other people, such as teachers and social workers, are legally required to report all suspected cases of child abuse to the appropriate local child welfare agency.
Request an Appointment at Mayo Clinic
Risk factors
Factors that may increase a person's risk of becoming abusive include:
- A history of being abused or neglected as a child
- Physical or mental illness, such as depression or post-traumatic stress disorder (PTSD)
- Family crisis or stress, including domestic violence and other marital conflicts, or single parenting
- A child in the family who is developmentally or physically disabled
- Financial stress, unemployment or poverty
- Social or extended family isolation
- Poor understanding of child development and parenting skills
- Alcohol, drugs or other substance abuse
Complications
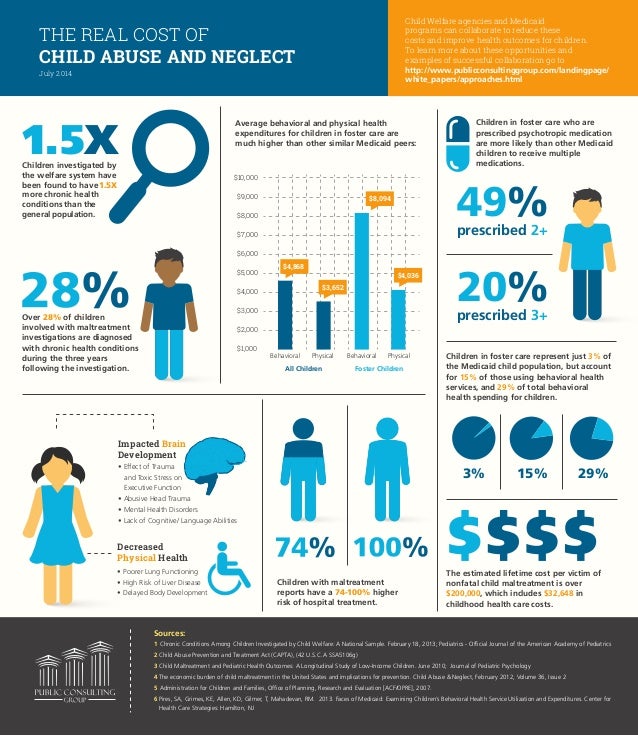
Some children overcome the physical and psychological effects of child abuse, particularly those with strong social support and resiliency skills who can adapt and cope with bad experiences.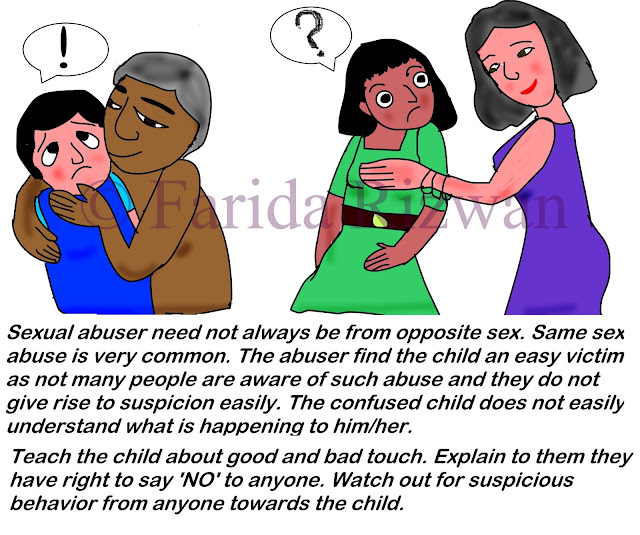 For many others, however, child abuse may result in physical, behavioral, emotional or mental health issues — even years later.
For many others, however, child abuse may result in physical, behavioral, emotional or mental health issues — even years later.
Here are some examples.
Physical issues
- Premature death
- Physical disabilities
- Learning disabilities
- Substance abuse
- Health problems, such as heart disease, diabetes, chronic lung disease and cancer
Behavioral issues
- Illegal or violent behavior
- Abuse of others
- Withdrawal
- Suicide attempts or self-injury
- High-risk sexual behaviors or teen pregnancy
- Problems in school or not finishing high school
- Limited social and relationship skills
- Problems with work or staying employed
Emotional issues
- Low self-esteem
- Difficulty establishing or maintaining relationships
- Challenges with intimacy and trust
- An unhealthy view of parenthood
- Inability to cope with stress and frustrations
- An acceptance that violence is a normal part of relationships
Mental health disorders
- Eating disorders
- Personality disorders
- Behavior disorders
- Depression
- Anxiety disorders
- Post-traumatic stress disorder (PTSD)
- Trouble sleeping (insomnia) and nightmares
- Attachment disorders
Prevention
You can take important steps to protect your child from exploitation and child abuse, as well as prevent child abuse in your neighborhood or community. The goal is to provide safe, stable, nurturing relationships for children.
The goal is to provide safe, stable, nurturing relationships for children.
Here's how you can help keep children safe:
- Offer your child love and attention. Nurture and listen to your child and be involved in your child's life to develop trust and good communication. Encourage your child to tell you if there's a problem. A supportive family environment and social networks can help improve your child's feelings of self-esteem and self-worth.
- Don't respond in anger. If you feel overwhelmed or out of control, take a break. Don't take out your anger on your child. Talk with your health care provider or a therapist about ways you can learn to cope with stress and better interact with your child.
- Think supervision. Don't leave a young child home alone. In public, keep a close eye on your child. Volunteer at school and for activities to get to know the adults who spend time with your child. When old enough to go out without supervision, encourage your child to stay away from strangers and to hang out with friends rather than be alone.
 Make it a rule that your child tells you where he or she is at all times. Find out who's supervising your child — for example, at a sleepover.
Make it a rule that your child tells you where he or she is at all times. Find out who's supervising your child — for example, at a sleepover. - Know your child's caregivers. Check references for babysitters and other caregivers. Make irregular, but frequent, unannounced visits to observe what's happening. Don't allow substitutes for your usual child care provider if you don't know the substitute.
- Emphasize when to say no. Make sure your child understands that he or she doesn't have to do anything that seems scary or uncomfortable. Encourage your child to leave a threatening or frightening situation immediately and seek help from a trusted adult. If something happens, encourage your child to talk to you or another trusted adult about what happened. Assure your child that it's OK to talk and that he or she won't get in trouble.
-
Teach your child how to stay safe online. Put the computer in a common area of your home, not the child's bedroom.
 Use the parental controls to restrict the types of websites your child can visit. Check your child's privacy settings on social networking sites. Consider it a red flag if your child is secretive about online activities.
Use the parental controls to restrict the types of websites your child can visit. Check your child's privacy settings on social networking sites. Consider it a red flag if your child is secretive about online activities.Cover online ground rules, such as not sharing personal information; not responding to inappropriate, hurtful or frightening messages; and not arranging to meet an online contact in person without your permission. Tell your child to let you know if an unknown person makes contact through a social networking site. Report online harassment or inappropriate senders to your service provider and local authorities, if necessary.
- Reach out. Meet the families in your neighborhood, including parents and children. Develop a network of supportive family and friends. If a friend or neighbor seems to be struggling, offer to babysit or help in another way. Consider joining a parent support group so that you have an appropriate place to vent your frustrations.

If you worry that you might abuse your child
If you're concerned that you might abuse your child, seek help immediately. In the United States, you can get information and assistance by calling or texting the Childhelp National Child Abuse Hotline: 1-800-4-A-CHILD (1-800-422-4453).
Or you can start by talking with your family health care provider. Your provider may offer a referral to a parent education class, counseling or a support group for parents to help you learn appropriate ways to deal with your anger. If you're misusing alcohol or drugs, ask your health care provider about treatment options.
If you were abused as a child, get counseling to ensure you don't continue the abuse cycle or teach those destructive behaviors to your child.
Remember, child abuse is preventable — and often a symptom of a problem that may be treatable. Ask for help today.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Recognizing Signs of Child Abuse and Neglect
AddictionAllergies & AsthmaAmbulatoryAudiologyAutismAwardsBC4TeensBehavioral HealthBehind the ScenesBurn CenterCancerCardiologyCenter for Healthy Weight and NutritionCenter for Injury Research and PolicyChild BehaviorChild DevelopmentColorectal and Pelvic ReconstructionCommunity EducationCommunity ResourcesCoronavirusDentistryDermatologyDiseases & ConditionsDiversity and InclusionEndocrinologyENTEpilepsyEverything MattersFertility and Reproductive Health ProgramFundraising EventsGastroenterologyGeneticsGynecologyHematologyHomecareHospiceHospital NewsInfants & NewbornsInfectious DiseaseKids & TeensLaboratory ServicesMake Safe HappenMarathonNeonatologyNephrologyNeurologyNeurosurgeryNew HospitalNICUNutrition & FitnessOccupational TherapyOphthalmologyOrthopedicsOur PatientsOur staffPalliative CareParentingPediatric NewsPharmacyPhysical Therapy - Sports and OrthopedicPlastic SurgeryPopulation HealthPregnancyPrimary CarePsychologyPulmonaryRadiologyReach Out and ReadRehabilitationResearchRheumatologySafety & PreventionSports MedicineSurgical ServicesThe Center for Family Safety and HealingTherapeutic RecreationTherapyTHRIVE ProgramToddlers & PreschoolersUrgent CareUrology
Aaron Barber, AT, ATC, PESAbbie Roth, MWCAbby Orkis, MSW, LSWAdam Ostendorf, MDAdriane Baylis, PhD, CCC-SLPAdrienne M. Flood, CPNP-ACAdvanced Healthcare Provider CouncilAila Co, MDAlaina White, AT, ATCAlana Milton, MDAlana Milton, MDAlecia Jayne, AuDAlena SchuckmannAlessandra Gasior, DOAlex Kemper, MDAlexandra Funk, PharmD, DABATAlexandra Sankovic, MDAlexis Klenke, RD, LDAlice Bass, CPNP-PCAlison PeggAllie DePoyAllison Rowland, AT, ATCAllison Strouse, MS, AT, ATCAmanda E. Graf, MDAmanda GoetzAmanda Smith, RN, BSN, CPNAmanda Sonk, LMTAmanda Whitaker, MDAmber Patterson, MDAmberle Prater, PhD, LPCCAmy Brown Schlegel, MDAmy Coleman, LISWAmy Dunn, MDAmy E. Valasek, MD, MScAmy Fanning, PT, DPTAmy Garee, CPNP-PCAmy Hahn, PhDAmy HessAmy Leber, PhDAmy LeRoy, CCLSAmy Moffett, CPNP-PCAmy Randall-McSorley, MMC, EdD CandidateAmy Thomas, BSN, RN, IBCLCAmy Wahl, APNAnastasia Fischer, MD, FACSMAndala HardyAndrea Brun, CPNP-PCAndrea M. Boerger, MEd, CCC-SLPAndrea Sattler, MDAndrea ShellowAndrew AxelsonAndrew Kroger, MD, MPHAndrew SchwadererAndria Haynes, RNAngela AbenaimAngela Billingslea, LISW-SAnn Pakalnis, MDAnna Lillis, MD, PhDAnnette Haban-BartzAnnie Drapeau, MDAnnie Temple, MS, CCC-SLP, CLCAnnie Truelove, MPHAnthony Audino, MDAnup D.
Flood, CPNP-ACAdvanced Healthcare Provider CouncilAila Co, MDAlaina White, AT, ATCAlana Milton, MDAlana Milton, MDAlecia Jayne, AuDAlena SchuckmannAlessandra Gasior, DOAlex Kemper, MDAlexandra Funk, PharmD, DABATAlexandra Sankovic, MDAlexis Klenke, RD, LDAlice Bass, CPNP-PCAlison PeggAllie DePoyAllison Rowland, AT, ATCAllison Strouse, MS, AT, ATCAmanda E. Graf, MDAmanda GoetzAmanda Smith, RN, BSN, CPNAmanda Sonk, LMTAmanda Whitaker, MDAmber Patterson, MDAmberle Prater, PhD, LPCCAmy Brown Schlegel, MDAmy Coleman, LISWAmy Dunn, MDAmy E. Valasek, MD, MScAmy Fanning, PT, DPTAmy Garee, CPNP-PCAmy Hahn, PhDAmy HessAmy Leber, PhDAmy LeRoy, CCLSAmy Moffett, CPNP-PCAmy Randall-McSorley, MMC, EdD CandidateAmy Thomas, BSN, RN, IBCLCAmy Wahl, APNAnastasia Fischer, MD, FACSMAndala HardyAndrea Brun, CPNP-PCAndrea M. Boerger, MEd, CCC-SLPAndrea Sattler, MDAndrea ShellowAndrew AxelsonAndrew Kroger, MD, MPHAndrew SchwadererAndria Haynes, RNAngela AbenaimAngela Billingslea, LISW-SAnn Pakalnis, MDAnna Lillis, MD, PhDAnnette Haban-BartzAnnie Drapeau, MDAnnie Temple, MS, CCC-SLP, CLCAnnie Truelove, MPHAnthony Audino, MDAnup D.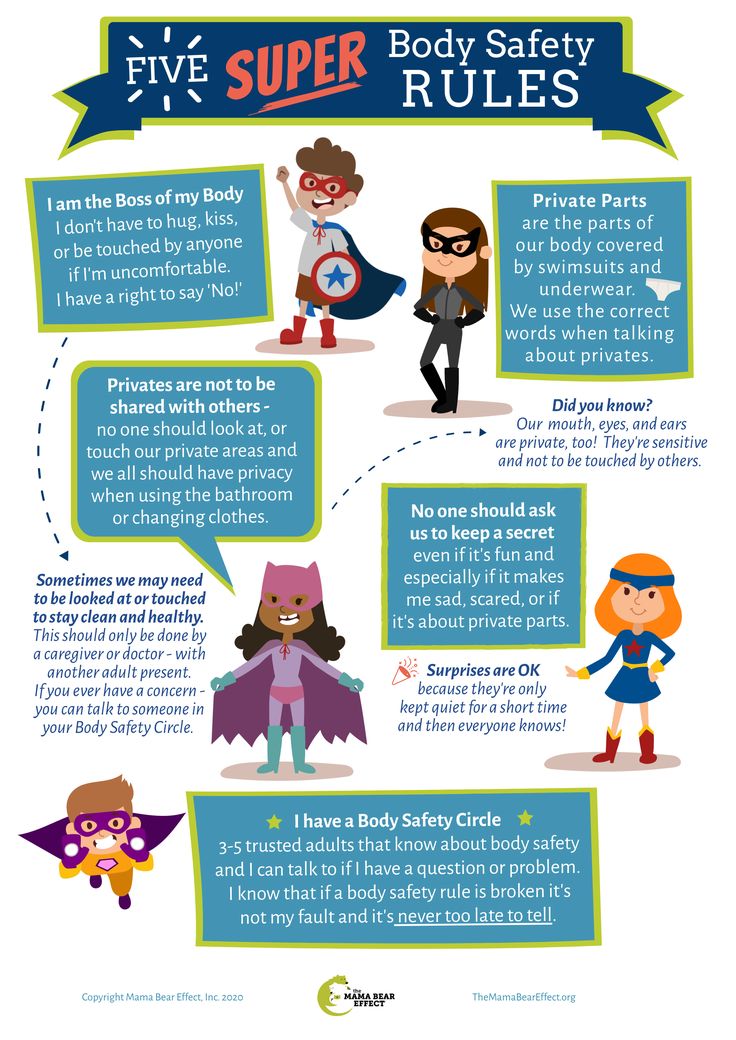 Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H.
Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H.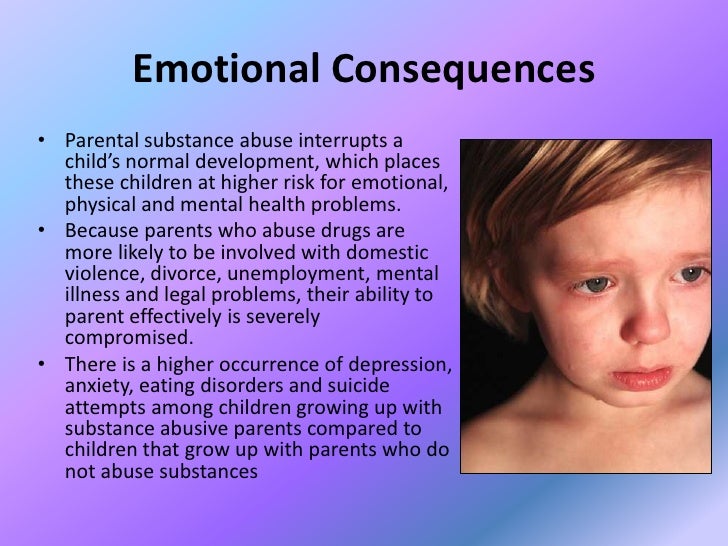 Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarneshia EdwardsCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsea Kebodeaux, MDChelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R.
Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarneshia EdwardsCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsea Kebodeaux, MDChelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R. Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin McKnight, MD, MPHErin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHeather Battles, MDHeather ClarkHeather L. Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHilary Michel, MDHiren Patel, MDHolly Deckling, MSSW, LISWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D.
Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin McKnight, MD, MPHErin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHeather Battles, MDHeather ClarkHeather L. Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHilary Michel, MDHiren Patel, MDHolly Deckling, MSSW, LISWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D. Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R. Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M.
Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R. Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M. Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatherine Deans, MDKatherine McCracken, MD FACOGKathleen (Katie) RoushKathryn Blocher, CPNP-PCKathryn J. Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N.
Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatherine Deans, MDKatherine McCracken, MD FACOGKathleen (Katie) RoushKathryn Blocher, CPNP-PCKathryn J. Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N.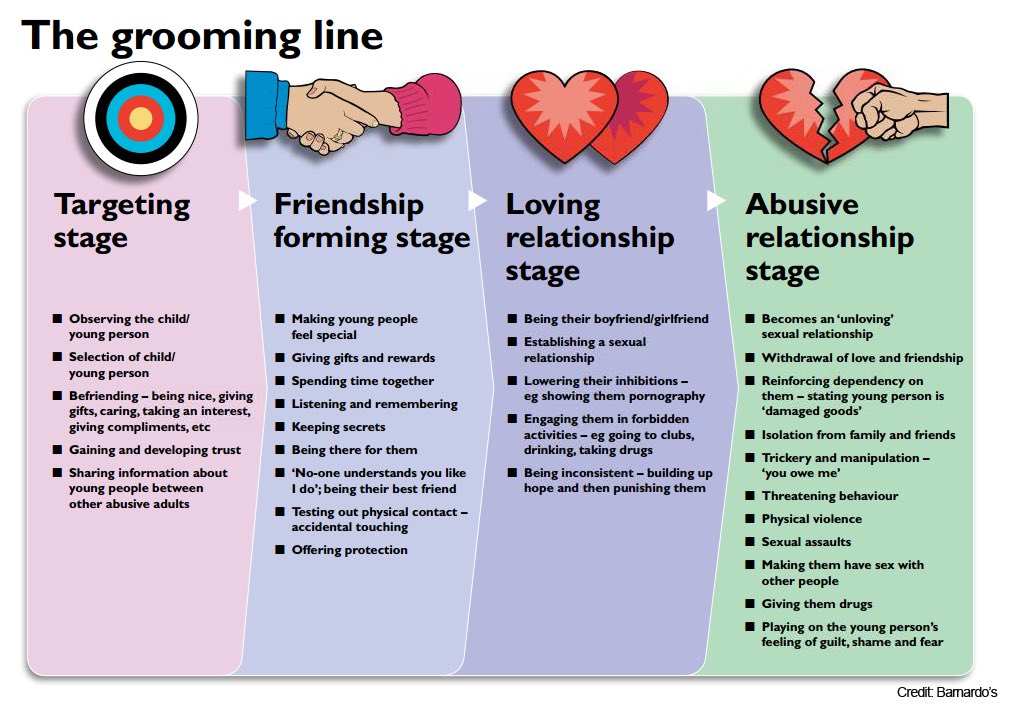 Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M. Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc P.
Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M. Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc P. Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I.
Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I. Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDPriyal Patel, DORachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A. Kowatch, MD, Ph.
Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDPriyal Patel, DORachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A. Kowatch, MD, Ph.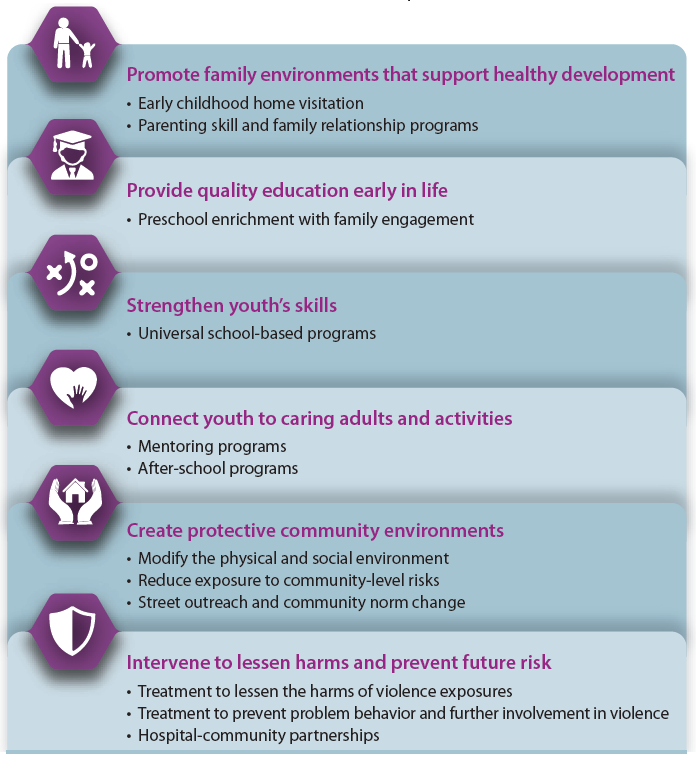 D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C. Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDSini James, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C.
D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C. Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDSini James, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C.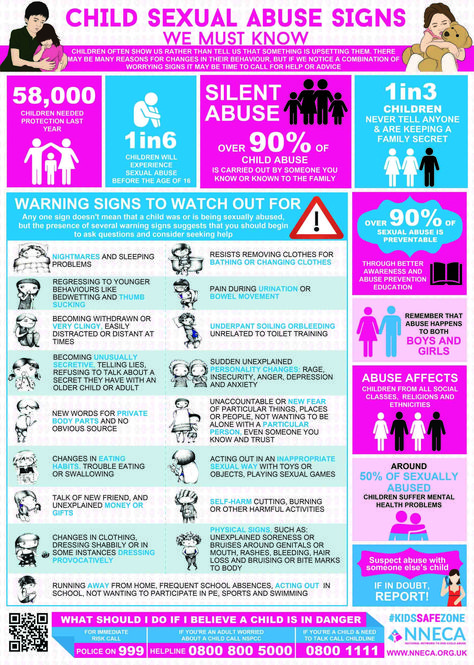 Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTenelle JonesTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L. Sisk, RN, BSN, MHATracie Steinke RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W.
Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTenelle JonesTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L. Sisk, RN, BSN, MHATracie Steinke RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W. Long, MD
Long, MD
Article | How to recognize violence
Violence is not always easy to spot. Especially if not your own child is injured, but a friend or, say, a neighbor. But help is needed anyway. Elena Gorinova, the leading trainer of the Federal Scientific and Methodological Center in the field of psychology and pedagogy of tolerance, talks about the dangers of physical or psychological violence and how to save a child from the “victim complex”.
Types of violence
Violence is different. And it's not necessarily bruises or abrasions. It can manifest itself in various ways.
- Physical: beating, injury, bodily injury.
- Emotional: bullying, parental actions that, at first glance, do not look like violence (insults, ignoring, depreciation, overprotection).
- Sexy.
- Hypoguardianship: inaction, non-compliance with duties by parents or guardians. Failure to provide care, neglect of the rules of hygiene, failure to provide the child with comfort, nutrition, etc.
It is widely believed that violence can only exist in a dysfunctional family of asocial, marginalized people. Many people think that violent actions occur in disadvantaged areas. In reality, violence against children does not depend on the well-being, level of cultural development, nationality, education and income of adult family members. It happens not only in shelters, but also in ordinary families.
Post-traumatic stress disorder
An abused person may suffer from post-traumatic stress disorder (PTSD) for years.
Initially, PTSD was thought to be a psychological disorder that affects people who have experienced catastrophes, natural disasters, and military operations. Now this mental disorder is recorded in people who have been subjected to domestic and social violence. It is observed in children, and the figures are disappointing - from 5 to 98%.
Natural disaster - an isolated case. Bullying, trolling or abuse of a child occurs systematically and leads to the formation of a victim complex .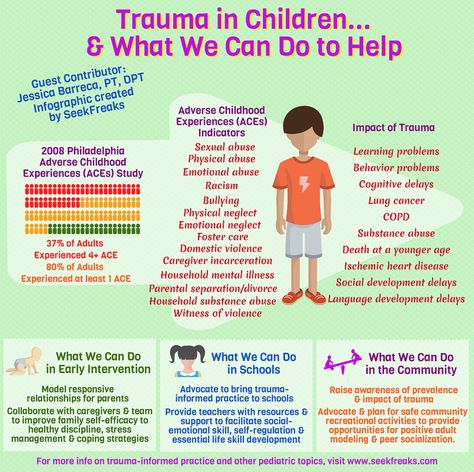 In such cases, the child is forced and constantly exposed to violence, and the consequences of these actions have a long-term and delayed effect.
In such cases, the child is forced and constantly exposed to violence, and the consequences of these actions have a long-term and delayed effect.
A victim of a natural disaster is exposed to a single impact, but a child with a victim complex develops a guilt complex. He thinks that he is to blame, and does not even try to seek support. The child may try to run away, close in on himself and not involve anyone to fight the aggressor. No one may be aware that a boy or girl in class or in the neighborhood is the victim of physical or emotional abuse.
Manifestations of PTSD
- Increased anxiety: constant anxiety, sleep disturbance, fright from sudden gestures.
- Insomnia, nightmares or, conversely, excessive sleepiness.
- Eating disorders: lack of appetite, which can lead to anorexia, or the opposite - gluttony, bulimia.
- Apathy, loss of interest in what used to worry.
- Problems with learning, fading of cognitive abilities and motivation.

- Speech disorders: unmotivated mutism, stuttering, situational muteness.
- Reproduction of traumatic events in repetitive games or drawings (in preschool children).
- Preference for violent computer games dominated by murder and violence. Perhaps this is how he tries to take out PTSD on the characters in the game.
- Depressive moods and pessimism (in adolescents).
- Aggression towards others.
- Auto-aggression: self-harm, cutting.
- Deviant behavior or suicidal tendencies that can be seen in social networks.
- Extreme behavior: catching, roofing, etc.
- Addiction to alcohol and other substances.
Why don't the children tell anything?
If a child has already formed a victim complex, then he will perceive what is happening as the norm. He will be silent so as not to harm loved ones. The child is afraid of the consequences: the main thing is that it does not get worse.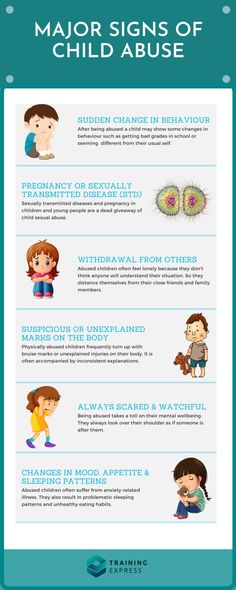 When the abuser is a close adult for whom the child feels love and affection, he will protect him. The child will hide from outsiders some facts that may negatively affect the parents. He will not tell that his mother does not care about him and does not love him.
When the abuser is a close adult for whom the child feels love and affection, he will protect him. The child will hide from outsiders some facts that may negatively affect the parents. He will not tell that his mother does not care about him and does not love him.
Guilt makes the child feel responsible for everything that happens. He is ashamed to be a victim. He is afraid that he will be despised for being bad. Therefore, he prefers to remain silent. This is due to the work of protective mental mechanisms. Trying to move away from traumatic pain, the child convinces himself that nothing terrible has happened and he is safe.
All this destroys trust in adults. A traumatized child does not know what a trusting relationship is, he does not expect anything good from adults. And to whom to turn for help and support, he does not understand. In addition, the victim complex makes the child feel powerless and helpless.
It seems that the victims of violence or aggression are certain people who behave somehow differently, look strange and have some peculiarities.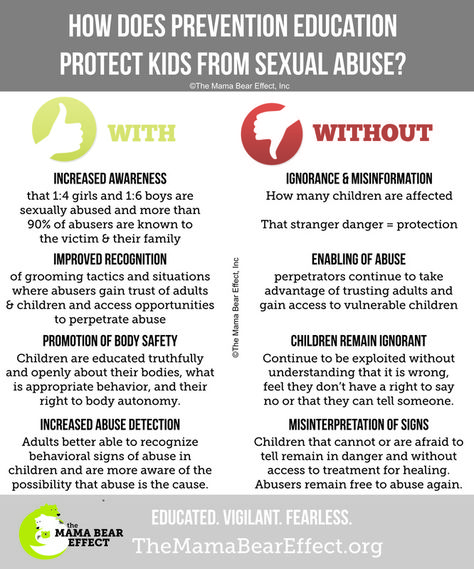 But in fact, absolutely anyone can become a victim of violence and aggression.
But in fact, absolutely anyone can become a victim of violence and aggression.
Negative consequences
As a rule, adults prefer not to notice warning signs in a child's behavior, thinking that these are signs of age and everything will pass. But this only exacerbates the situation. It happens that parents only increase the requirements: “Do you want to study? Got two again! Stay at home now! Until you learn everything, you will not go anywhere!”
What should alert
- Untidy and untidy.
- Stop in physical development.
- Inappropriate clothing.
- The child is hungry all the time.
- Painful appearance and neglect of medical care.
- The child is constantly alone.
- Systematic tardiness for lessons, absenteeism.
Why don't adults do anything?
- Many adults are captivated by a certain "cultural norm": "We were beaten, and nothing, they grew up to be good people.
 "
" - Bullying is perceived as a lesson and experience for "hardening character".
- Stereotypical thinking: "Everyone goes through this."
- Shielding a family member. For example, a mother justifies a father who beats a child, because "the father knows how to do it."
- Avoidance of problems and unwillingness to resolve the situation. Impotence. Justification of the aggressor.
- Lack of parental competence and an adult's focus only on the material support of the family.
- Adults are not always ready to think and speak on "forbidden" topics. A child cannot tell, and adults are not ready to listen, that someone has performed inappropriate actions towards him.
- Distrust of specialists, neglect of psychological help.
- Unwillingness to interfere in the affairs of others (“they will figure it out themselves”, etc.).
- Ignorance of the characteristics of adolescence.
In case of suspicion
If there is information about violent actions against a child, in no case should you be angry and angry with him. You need to talk to him gently and gently. So to encourage him to tell what happened.
You need to talk to him gently and gently. So to encourage him to tell what happened.
It is unacceptable to show horror. This will only exacerbate the guilt complex. The teenager will definitely transfer it to himself. It is necessary to do everything possible so that the teenager does not feel disgust. After all, it will make the child feel that it is he who is to blame for what happened.
In this case, it is necessary to calm and encourage the child so that he understands that you are not accusing him of anything. You need to give soft feedback: emphasize that this could happen to anyone, and provide moral support. It is necessary to explain that experiencing such feelings is a normal reaction of the psyche.
It is important to give the teenager a chance to speak, not to interrupt or rush him. You should share your intentions with the child: contact a psychologist, social pedagogue or law enforcement agencies. He must know about it.
Responsibility
Incidents of domestic violence - established and those that only require proof - cannot be ignored. Offenders and domestic tyrants must be punished. There is no article specifically for domestic violence in the Criminal Code of the Russian Federation. But depending on the harm done to the victim, the crime can be qualified under articles 111, 112, 115, 119 and 132 of the Criminal Code of the Russian Federation.
Offenders and domestic tyrants must be punished. There is no article specifically for domestic violence in the Criminal Code of the Russian Federation. But depending on the harm done to the victim, the crime can be qualified under articles 111, 112, 115, 119 and 132 of the Criminal Code of the Russian Federation.
Responsibility for domestic violence will depend on the method of implementation and the consequences caused by violent acts. The abuser may be subject to a fine, forced labor, or corrective labor. Restriction of freedom for up to 2 years or a prison sentence for the same term is also possible. The most severe punishment for moderate injuries is imprisonment or restriction of liberty for up to 3 years, as well as arrest for up to 6 months. If domestic violence has serious consequences, the perpetrator faces imprisonment for up to 8 years.
Even doubts and suspicions about domestic violence should not be ignored. The impunity and patience of the victim encourage the tyrant to continue his actions. The main thing is not to be silent!
The main thing is not to be silent!
what is dangerous and how to deal with it
Photos: Depositphotos / Illustration: Julia Zamzhitskaya
Resentment is a normal part of communication, if they are temporary. But there are times when resentment becomes chronic. This hinders the development of relationships between children and leaves a painful imprint on adult life: the psyche retains the entire spectrum of old experiences, forcing a person to return to them again and again. Gayane Yeribekyan, a primary school teacher and psychologist with 15 years of experience, tells how to protect a child from this child and help touchy adults.
How to determine the "level of touchiness" in a child
A touchy child reacts to events too sharply, even inadequately. He is hurt by someone else's success: it seems to devalue his own achievements. Such children are often aggressive: they not only give back to the offenders, but also think over a plan of revenge.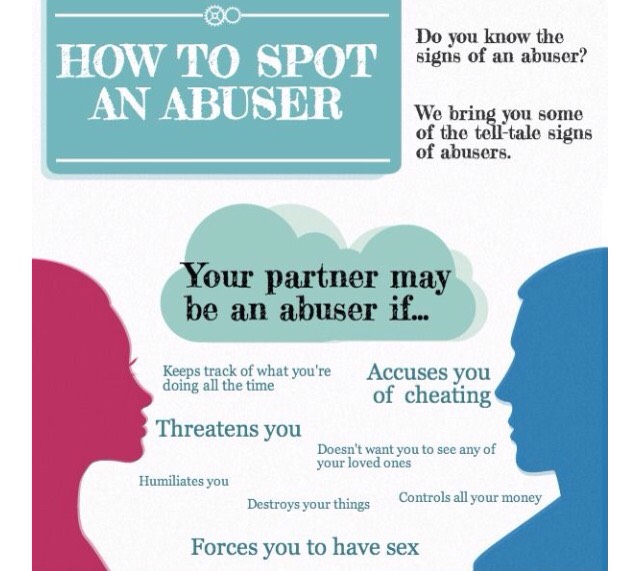
All this forms in the child suspicion and distrust of others, a tendency to manipulation. And gradually these properties become character traits.
To understand whether touchiness has become a problem for a child, use a small test. Are the following statements true?
- The child often needs praise to be confident in his actions.
- Talking about his friend, the child talks more about what this friend does for him.
- The child, by his behavior, initiates situations in which he can be offended.
- The child seems to be deliberately offended.
- The child has a hard time with the success of other children.
- Hearing praise for other children, the child cries and refuses to do anything else with them.
- The child reacts sharply to criticism.
- The child remembers grievances for a long time, can remember and talk about them months and years later, as if reliving anew.
- The child uses his resentment as a way to achieve what he wants.
If at least five statements turned out to be true in your case, this means that touchiness has grown into a problem and it's time to fight it.
Get the profession of a teacher-organizer with the additional qualification "Social teacher" at the Training Center of the Teachers' Council.
What's in the program?
— Practice-oriented methods of work of a social pedagogue and an organizing teacher.
— Methods of social and pedagogical work with children left without parental care and dysfunctional families.
— Support for curators and feedback from teachers.
And what is the result?
A new profession and a diploma of professional retraining of the established sample.
Installment available.
Learn more
Resentment is a feeling formed by anger and helplessness. Most often it is associated with a violation of the psychological boundary in childhood. Many parents, noticing anger in a child, try to suppress this feeling in him instead of teaching him how to cope with it. So the baby has a state of helplessness, inability to resist. In most cases, touchy children react to a traumatic situation in the same way: they simply do not know how to do it differently. Therefore, the task of an adult is to show the baby other ways of behavior:
Many parents, noticing anger in a child, try to suppress this feeling in him instead of teaching him how to cope with it. So the baby has a state of helplessness, inability to resist. In most cases, touchy children react to a traumatic situation in the same way: they simply do not know how to do it differently. Therefore, the task of an adult is to show the baby other ways of behavior:
- Do not generalize.
The child is used to saying in a general way: "I was offended." Here it is important to achieve a specific answer: who exactly offended?
You can help your child by listing the names of potential offenders. And the first to name those who, most likely, have nothing to do with it. So the child will understand that not everyone offends. And if so, then you can not run away and hide, but start a fight with the offender.
- Talk directly about your feelings.
The child should tell the bully how he feels when he is bullied.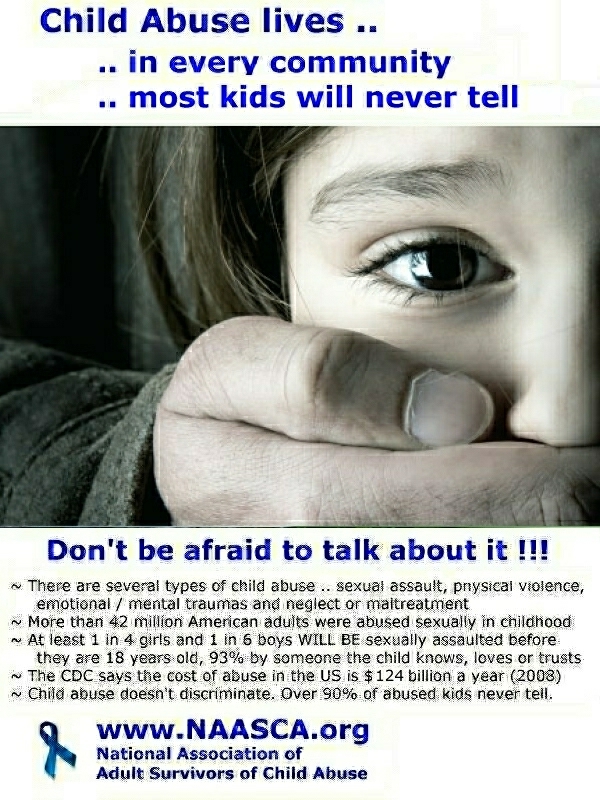 “I don’t like it”, “Please don’t say it, don’t do it” and so on. After these words, the child must pause so that the offender has the opportunity to understand what actions or words are being discussed.
“I don’t like it”, “Please don’t say it, don’t do it” and so on. After these words, the child must pause so that the offender has the opportunity to understand what actions or words are being discussed.
- Ignore the offender.
It is not always possible to defend yourself against attacks by directly addressing the offender. Sometimes it is more useful to ignore it: the child needs to imagine that the opponent is simply not in the room. But this technique is not for all children. If the child is impulsive and emotional, most likely, he will not be able to restrain himself and, in the end, will react violently to ridicule and offensive words.
- Use the three step method.
First step: a calm but firm statement: "Don't do it, don't say it...", "I don't like it." It is very important to say this in a firm and confident tone. If the bully continues to insult or ridicule, you need to go to the second step: warn that if the attacks do not stop, the bully will get hit (this method is not applicable to girls).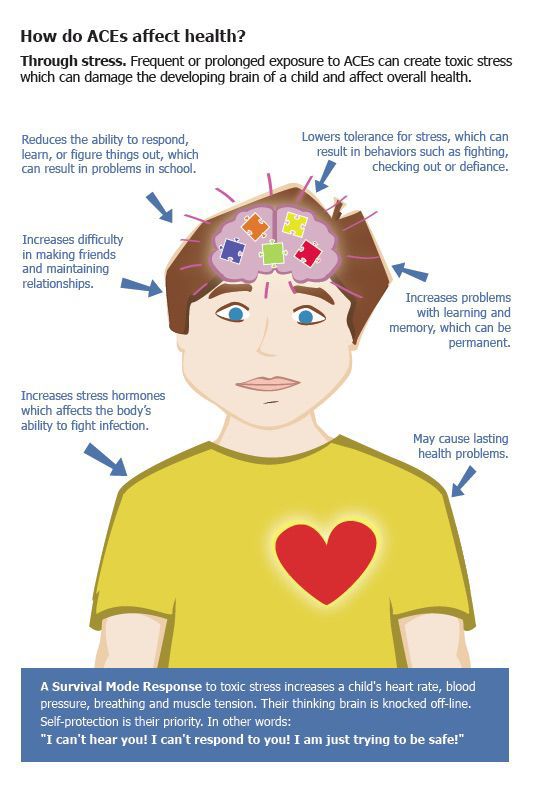 Finally, the third step is a blow (if the offender has not stopped his actions).
Finally, the third step is a blow (if the offender has not stopped his actions).
In this way, the child learns to remain calm in traumatic situations and to stop aggression from other children.
- Show interest in other children.
Resentful children are overly focused on themselves and their experiences. They do not imagine that you can communicate and be friends with other children if you find out about their interests. In order for the child to find out more about peers, you can ask him to create a “portrait” of one of the children. So he finds out what other guys are interested in, what books, cartoons, games they like. This will help to find common interests and make friends, and there will be no place for resentment.
- Build internal supports.
Touchy children are very dependent on other people's opinions. It is important for them to receive praise, and negative evaluations or indifference hurt them.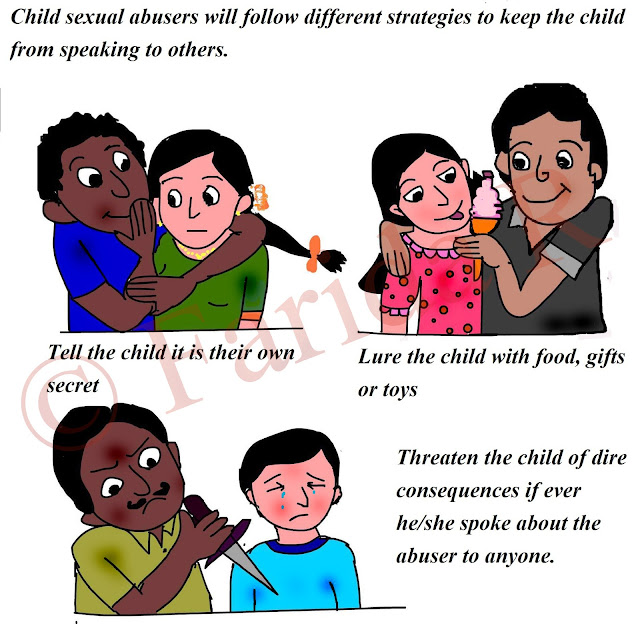 Therefore, you need to teach your child to notice and appreciate their own achievements.
Therefore, you need to teach your child to notice and appreciate their own achievements.
For example, when writing, let the child find and highlight the letters that worked out especially well for him. Having praised the child for a report or well-designed work, it should be said that he can be proud of himself. It is important that the child learns to feel pride in the work done. Such an attitude towards oneself and one's achievements forms the psychological foundations on which self-esteem and self-confidence are based.
What resentments become chronic
There is a certain kind of resentment that leaves the deepest imprint on the psyche and continues to affect a person even in adulthood. As a rule, their child is inflicted by the most significant people in his life - parents. The feeling of resentment can grow over the years, crowding out other emotions, depriving a person of the desire to live and enjoy life.
Resentment against my mother: I am unloved and nobody needs me
Often adults who seem self-sufficient and self-confident actually feel inner emptiness and a sense of their own uselessness. They have a gloomy attitude and a pessimistic attitude towards life.
They have a gloomy attitude and a pessimistic attitude towards life.
The origins of this psychological problem, as a rule, lie in deep childhood, in the peculiarities of the relationship with the mother. In the memories, she remained indifferent or critical, always busy with work and tired. Or maybe she demanded obedience all the time or looked for the right methods of education from the "authorities", although it would be better to trust her own maternal instincts.
Such traumatic memories are familiar to almost all people: almost everyone at least once had the thought that his mother “didn't like him” creep into his head.
Resentment against the father: seeking someone else's approval
Many "chronic" resentments in adult life are associated with the relationship between the child and the father. It is important for children that their father recognizes their talents and abilities. And constant criticism, devaluation and indifference, on the contrary, form low self-esteem.
Even having achieved great success in life, such a person continues to look for "significant" people who would appreciate his talents and achievements. This search brings only disappointment. First of all, the “seeker” himself should accept the value and significance of his achievements.
Resentment against sisters and brothers: whom parents loved more
Caring for younger sisters and brothers, which parents entrust to older children, often turns out to be a heavy burden for them. After all, caring for the younger ones, the older ones partly take on the role of adults and lose their own childhood. The child believes that a little sister or brother is loved more, and he gets only demands and claims. Such resentment accumulates and often persists into adulthood, continuing to influence family relationships.
Often, younger children also have a reason for resentment: older children take out their anger on them for parental injustice.
How to overcome chronic resentment
The “letter to the offender” technique helps to overcome resentment.