How to make autistic child sleep
Better sleep for autistic children: tips
About good sleep for autistic children
Good sleep is about getting to sleep, staying asleep and getting enough good-quality sleep. All children, including autistic children, need enough good-quality sleep for growth, development and learning.
How long it takes children to get to sleep and settle back to sleep when they wake in the night can depend on things like:
- what they do before they go to bed
- what time they go to bed
- what they need to get to sleep
- where they go to sleep
- what they do during the day.
How to sleep better for autistic children: tips
The tips below can help all children, including autistic children, sleep better. They help children develop healthy daytime and bedtime habits that promote sleep.
If your autistic child has particular problems with falling asleep and waking in the night and these tips don’t seem to be working after 2-4 weeks, it’s a good idea to seek help. Talk with your doctor or another health professional about the best strategies for your situation.
1. Set up a bedtime routine
A regular bedtime routine starting around the same time each night encourages good sleep patterns. A bedtime routine of bath, story and bed can help younger children feel ready for sleep. For older children, the routine might include a quiet chat with you about the day then some time alone relaxing before lights out.
Autistic children might need some extra support to get used to a bedtime routine. Here are some ideas:
- Give your child clear and consistent cues when it’s nearly bedtime. For example, 30 minutes before bedtime, start some quiet activities like reading or drawing in the family room. Then 15 minutes before bedtime, get your child to clean their teeth and go to the toilet.
- Use a visual support with pictures showing your child’s bedtime routine, so your child understands the steps. For example, put on pyjamas, clean teeth, go to the toilet, get into bed, have a bedtime story, turn out light.
- Put stickers on the visual support to show when your child completes a step correctly.
- Praise your child for successfully completing steps in the routine. For younger children, you could use a reward chart.
- If your child gets upset or wakes during the night, quietly and calmly put your child back to bed. Settle them and remind them of the sleep routine using words or pictures. You might need to do this many times.
Once your child has a positive bedtime routine, you might find that your child settles well when they can follow that routine, but has problems if the routine changes. You might be able to handle this issue by planning and preparing for changes to your child's routine.
2. Set regular and appropriate bedtimes
Regular and appropriate bedtimes can help your autistic child get the sleep they need.
The first thing is to work out the best time for your child to go to bed. You can do this by looking at when your child needs to get up, and how much sleep your child needs to be well and alert during the day.
For example, you might notice your child generally needs 11 hours of sleep. You also know you won’t make it to school on time unless your child is up by 7 am. This means that 8 pm is the ideal bedtime for your child. Your evening activities – dinner time, pre-bedtime and bedtime routines – need to take this ideal bedtime into account.
The next step is to move your child’s sleepy time towards their ideal bedtime. To start with, put your child to bed when they’re sleepy. This might mean that your child stays up later and starts their bedtime routine a bit later initially.
Once your child is falling asleep quickly, move the start time for the routine back by 15 minutes every two days. It might take a few weeks, but your child should start to feel sleepy earlier until they’re going to bed at the desired time.
Until your child is good at settling to sleep, try to keep the same bedtime at weekends and holidays.
It’s best to introduce new bedtimes, bedtime routines and sleep habits gradually. It’s also important to encourage, praise and reward your child as you make any changes.
It’s also important to encourage, praise and reward your child as you make any changes.
3. Set up healthy sleep associations
Sleep associations and habits are the things that children (and adults) need to settle for sleep. When children wake at night, they need the same things to go back to sleep.
For autistic children, sleep associations and habits can be very strong. They might include falling asleep next to a parent, while watching TV or after using an electronic device.
If you’d prefer your child to fall asleep by themselves in their own bed, you might want to help your child develop some healthy sleep associations. Here are some ideas:
- Use pictures of your child sleeping in their own bed as part of a visual support.
- Give your child a reward for staying in their own bed.
If your child can fall asleep only when you’re next to them, you could try sitting on the edge of the bed or on a chair next to the bed. Gradually move away from your child each night as your child gets better at falling asleep alone.
4. Set up a safe, comfortable sleep environment
Some sleep environments can make it harder for children to get to sleep. Check that your child’s sleep space is quiet, dimly lit, and neither too hot nor too cold.
Gradually remove objects that might stop your child from sleeping comfortably. For example, a favourite soft toy in the bed might be OK. But if your child has a whole collection of toy cars in their bed, it might make it hard for your child to get comfortable in bed. You could encourage your child to put one or two cars per night into a box next to their bed.
Rewards can help your child make this change.
5. Avoid caffeine, screens and excitement before bed
Caffeine is in energy drinks, coffee, tea, chocolate and cola. Make sure your child avoids these foods and drinks, especially in the late afternoon or evening.
Your child might be more likely to relax and settle for sleep if they also avoid excitement, TV and screens in the hour before bed.
6. Eat the right amount at the right time during the day
What and when your child eats and drinks can affect their ability to settle down at night.
In the morning, a healthy breakfast helps to kick-start your child’s body clock at the right time. And in the evening, plan dinner so that your child is satisfied but not too full when they go to bed.
7. Get enough physical activity during the day
It’s a good idea to encourage your child to be more active during the day – for example, even a family walk before dinner can make a difference. And it’s great if your child can be active outside, because plenty of natural light during the day also helps with sleep.
Australian guidelines recommend that:
- preschoolers should be physically active for at least three hours a day, including at least an hour of energetic play, like running and jumping
- school-age children should be physically active for several hours a day, including at least an hour of moderate to vigorous physical activity.

8. Keep older children’s naps early and short
If your child over five years is still napping during the day, try to keep the nap to no longer than 20 minutes and no later than early afternoon. Longer and later naps can make it harder for children to get to sleep at night.
Autism and Sleep. Ten possible strategies.
The article below adresses the issues of autism and sleep in children and offers ten possible strategies.
You know that your child with an Autism Spectrum Disorder (ASD) experiences sleep difficulties. You also know that your child’s difficulties create sleep challenges for you too. But what you may not know is how common the challenges you face are for families affected by ASD.
In a report published in 1999, psychologist Amanda Richdale estimated that 44-83% of children on the autism spectrum experience sleep challenges, the most common of which are difficulty falling asleep, frequent wakings during the night, and early morning waking. Other difficulties include:
Other difficulties include:
- Insomnia
- Sleep apnea
- Bedtime resistance
- Parasomnias, such as sleepwalking, restless leg syndrome, nightmares, and night terrors
Sound familiar?
The good news is that the struggles you have getting your child to fall asleep and stay asleep are not unique to your family. In fact, the prevalence of sleep difficulties among children with autism means there has been ample opportunity for researchers to study the causes of the problem and develop effective strategies to help children and their parents get the sleep they need.
10 ways you can help your child with ASD sleep better
While these aren’t 100% effective all the time, practicing these habits may help improve your nighttime (and early morning) struggles.
1. Eliminate household noisesMost typically developing (TD) kids can easily block out ambient noise, especially when they are tired. For kids on the spectrum, household noises like the TV, music, the dishwasher, etc. can be over-stimulating or otherwise disturbing, making it impossible for them to fall asleep or even feel tired. As much as possible, try to limit your child’s exposure to household noises once they have gone to bed.
can be over-stimulating or otherwise disturbing, making it impossible for them to fall asleep or even feel tired. As much as possible, try to limit your child’s exposure to household noises once they have gone to bed.
Visual stimuli can disturb your child and make it difficult to fall asleep. Keeping their bedroom dark will help limit visual stimulation and encourage the production of melatonin, a neurohormone that promotes sleep. Switch to black-out curtains if there are streetlights, traffic lights, or other outdoor light sources near your child’s bedroom windows.
3. Keep the bedroom coolYour child may not be able to tell you if they feel too cool or too warm, but sleep experts indicate that a cool bedroom promotes sound sleep. Optimal bedroom temperatures range from 65° – 67° F. If your child cannot tolerate bed clothes or covers, you will want to raise the heat a bit but no higher than around 75° F.
Many children with ASD find certain fabrics and clothing features to be extremely irritating. Make sure that your child’s PJs and bed linens are made of fabrics that at least do not cause discomfort and at best are soothing to your child. Be aware that seams, zippers, and buttons can also be irritating. If your child is non-verbal, you may need to do some investigative research with them using trial and error.
5. Establish a bedtime routine and create visual cuesWork with your child to develop a soothing bedtime routine that you can stick to every night. Keep it simple, calming, and free from electronic screens. Create visual support for your child’s bedtime routine. (For more information about visual tools for children with autism and examples, see The National Autistic Society.) A bedtime routine might look like this:
- Take a bath
- Put on pajamas
- Use the bathroom
- Wash hands
- Brush teeth
- Read a book
- Go to sleep
 Use a bedtime social story
Use a bedtime social storyCreate a social story explaining the importance of sleep and the cues people use to know when it’s time for sleep. Be sure to include pictures to support your story.
7. Try a weighted blanketWhile a recent study suggests that weighted blankets do not increase sleep time or decrease time spent falling asleep, the deep pressure touch provided by the weighted blanket can help to soothe your child and make the bedtime routine more appealing.
8. Use relaxation trainingIf you suspect anxiety is the cause of your child’s sleep difficulties, incorporate some relaxation activities into the bedtime routine. These include:
- Deep breathing
- Muscle relaxation techniques
- Warm bath
- Soft music
- Audiobooks/stories
Research has shown that children with ASD improved their sleep when given melatonin in combination with oral instructions for parents on strategies to promote sleep. Look for a new melatonin mini-pill to be available in Europe in October 2018 and in the U.S. after that. It is a slow-release pill that is easy for kids to swallow and has been shown to decrease the time spent falling asleep as well increase total sleep time.
Look for a new melatonin mini-pill to be available in Europe in October 2018 and in the U.S. after that. It is a slow-release pill that is easy for kids to swallow and has been shown to decrease the time spent falling asleep as well increase total sleep time.
Many parents of children with autism fall into the habit of lying down with their kids to get them to sleep. While this can be a precious time to connect with your child, it reinforces their perceived need to have you near them in order to sleep. That means you are indispensable at bedtime as well as when your child awakens in the middle of the night. And that’s not good for either of you.
Tips for children who can’t go back to sleep on their own
Everyone naturally wakes up several times a night. For most people, these wakings go unnoticed because we go back to sleep right way.
For children who cannot go back to sleep by themselves, these natural wakings can wreak havoc on their night’s sleep and yours. That’s why it’s important for your child to learn to fall asleep alone at bedtime as well as during the night.
That’s why it’s important for your child to learn to fall asleep alone at bedtime as well as during the night.
Training your child to fall asleep alone should be done gradually over the course of a few weeks. Gradually distance yourself from your child once they have gotten into bed, then keep your visits back to their room brief. Gradually decrease the amount of attention you direct toward your child such as talking, eye contact, facial expressions, etc. while you are increasing your distance away from them.
SAMPLE DISTANCING SCHEDULE| Nights 1, 2, and 3 | Nights 4, 5, and 6 | Nights 7, 8, and 9 | Nights 10, 11, and 12 |
| Sit on the bed with your child as they lie down for sleep. Read them a soothing, short story. | Sit on a chair beside the bed. Keep an eye on them but make a game out of both of you staying quiet. | Move your chair further from the bed as your child tries to sleep. Try to make no contact with your child. | Wait outside your child’s bedroom after tucking them in and see if they can fall asleep alone. If not, go back into their room briefly, just long enough to remind them that it’s time for sleep, they are OK, and wish them “good night.” |
If you need to return to their room because they still haven’t fallen asleep, wait a little longer each time and keep your visits brief and uneventful. You can use this same method for middle-of-the-night wakings.
ASD teens and sleep
The teen years are a time of enormous physical, intellectual, and emotional change. These changes can disrupt sleep even if your child has been a good sleeper in the past. Alternatively, if you have tried some of these strategies in the past with no effect, it is worth trying them again with your teenage child.
Keep in mind that all teenagers experience a shift in their sleep and wake rhythms when they hit puberty. The time that they become sleepy gets later and their wake time is also pushed back. This shift often conflicts with school and work schedules. If there is flexibility in your teen’s schedule, help them shift to a later bedtime gradually by pushing bedtime back 30 minutes every few days.
The time that they become sleepy gets later and their wake time is also pushed back. This shift often conflicts with school and work schedules. If there is flexibility in your teen’s schedule, help them shift to a later bedtime gradually by pushing bedtime back 30 minutes every few days.
Allow them to sleep a little later as their schedule allows. Just make sure they have the recommended nine hours devoted to sleep each night. And reward them for sticking to their weekday sleep and wake schedule on the weekends.
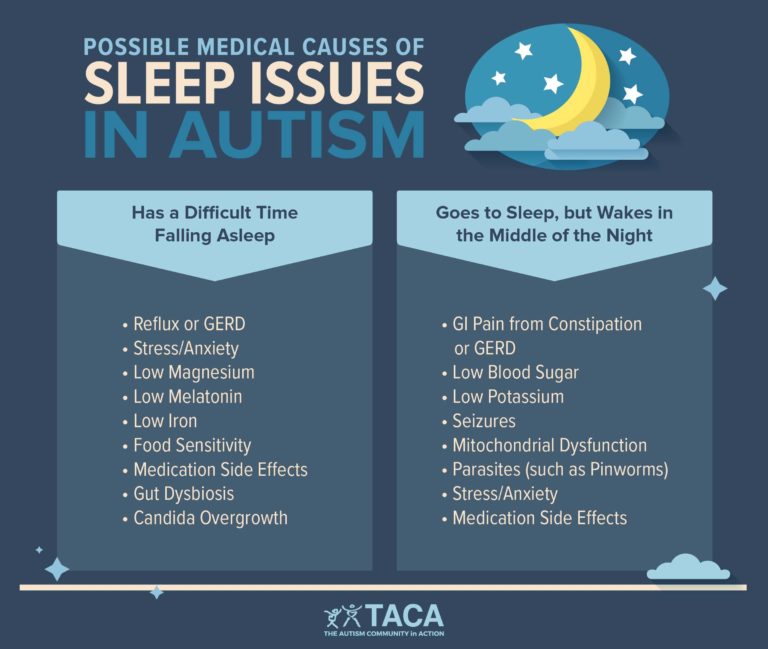
Causes of sleep challenges for children with ASD
Researchers do not agree on why sleep challenges are so prevalent among children with autism. But there are several theories circulating in the autism research community that can lead to better therapies or treatments.
- Missed signals. Children with ASD may find it difficult to learn normal sleep associations (such as bedtime routines that signal time for sleep).
- Adjusting to changes.
 Children with autism usually have a hard time adjusting to changes in routine or environment. Trips to Grandma’s or family vacations can wreak havoc on their sleep schedules. Adjusting to Daylight Saving Time and then back to Standard Time presents another challenge.
Children with autism usually have a hard time adjusting to changes in routine or environment. Trips to Grandma’s or family vacations can wreak havoc on their sleep schedules. Adjusting to Daylight Saving Time and then back to Standard Time presents another challenge. - Circadian rhythm sleep disorders. Children with ASD may not respond to the social cues that help to regulate the circadian rhythms in TD children and adults such as mealtimes, bath times, dressing for bed, brushing teeth, etc. A study conducted by a team of researchers in Japan, found that people with autism are about twice as likely to carry mutations in the genes that regulate the body’s sleep/wake cycle or circadian rhythms, which may be one reason so many children with ASD experience sleep difficulties.
- Anxiety is a common problem for children with autism and may lead to insomnia and other sleep difficulties.
- Medical issues. Sleep apnea, epilepsy, and acid reflux are more common in children with ASD and can disrupt sleep.

- Lower levels of melatonin. Children with autism have been shown to produce lower levels of melatonin, a neurohormone that regulates the sleep/wake cycle. In a study conducted at Vanderbilt University, children on the autism spectrum with lower melatonin levels were found to spend less time in deep sleep stages and exhibited more daytime sleepiness.
You and your child don’t have to live this way
You and your child already deal with so many challenges resulting from ASD that you may think sleep deprivation is just another one on a long list. But your child’s sleep difficulties should not be ignored because they can have serious consequences for your child as well as the entire family.
- Poor sleep exacerbates some of the classic difficulties for children with autism such as weak emotional control, repetitive behaviors, difficulty with social situations and communication, and attention deficits.
- Recent studies indicate that children with ASD may get less rapid eye movement (REM) sleep than their neurotypical peers.
 This deficit can have significant consequences for their intellectual development since memory and learning is solidified during this phase of sleep. REM sleep is also the time when brains process fear and emotions. Insufficient REM sleep can lead to increased anxiety and stress.
This deficit can have significant consequences for their intellectual development since memory and learning is solidified during this phase of sleep. REM sleep is also the time when brains process fear and emotions. Insufficient REM sleep can lead to increased anxiety and stress. - The nightly struggle to get your child to bed and to fall asleep makes bedtime stressful for everyone in the family. If you have more than one child, you may have less time and energy to attend to your other children because you are consumed by the needs of your child with ASD.
- Your evenings turn into a race against the clock to get your child to sleep. Disruptions during the night may interfere with your time with your spouse. The chronic lack of sleep can make you less of the kind of parent and spouse you’d like to be.
That’s why it’s important to take steps to help your child sleep as soon as it becomes a problem.
HOW MUCH SLEEP DO KIDS NEED?| Age | Recommended Sleep Duration | Not Recommended |
| Toddlers (1-2 years) | 11 to 14 hours | Less than 9 hours; More than 16 hours |
| Preschoolers (3-5 years) | 10 to 13 hours | Less than 8 hours; More than 14 hours |
| School-aged children (6-13 years) | 9 to 11 hours | Less than 7 hours; More than 12 hours |
| Teenagers (14-17 years) | 8 to 10 hours | Less than 7 hours; More than 11 hours |
| Young adults (18-25 years) | 7 to 9 hours | Less than 6 hours; More than 11 hours |
Recommendations courtesy of the National Sleep Foundation
This article has been kindly donated by Mattress Advisor. Click the logo below to go to the website.
Click the logo below to go to the website.
If you need help looking for services for an individual with an autism spectrum condition, we can help. Click below for the Autism Placement Support Service.
How to help a child with autism regulate sleep?
04/26/15
Description of behavioral techniques for correcting sleep violations for Autism
Source: Association for Science in Autism Treatment
9000 I am a home program and work with the Working program with the Shelves. diagnosed with autism. His parents are concerned that he has trouble getting to bed and he often wakes up in the middle of the night and visits them. Parents would like the child to continue sleeping in bed all night, and they have already tried everything. What can I offer them to treat their child's sleep behavior?
Answered by Lauren Schnell, Certified Behavior Analyst, Children's Specialty Hospital.
Sleep disturbances in children with autism are a concern for many parents. It is estimated that approximately 25% of normal children aged one to four often wake up during the night (Lozoff, Wolf, & Davis, 1985). Among children with special needs, up to 80% have some type of sleep problem (Lamberg, 1994). Most children who often wake up at night end up sleeping in their parents' bed, and sleep problems persist for a long time.
The good news is that there are several behavioral approaches that have been shown to be effective for sleep disorders in children with autism. These approaches are based on the assumption that disturbed sleep patterns are learned and therefore can be relearned.
Before implementing a behavioral program to regulate sleep, possible medical causes of sleep disturbances, such as physical discomfort caused by illness, must be ruled out. It is necessary to discuss with the pediatrician whether sleep difficulties may be due to a medical problem, as well as conduct an appropriate medical examination.
If it can be assumed that sleep problems are behavioral, the first step is to keep a sleep diary to determine the extent of the problem and possible environmental factors that may be having an undesirable effect on the child's sleep. The sleep diary records what time the child is put to bed, what time he falls asleep, how often he wakes up at night and how long he stays awake on these occasions.
Additional information can also be collected on behaviors that can be observed at bedtime, such as protests during bedtime or unwanted behaviors during the night. Baseline data collection should continue until patterns (or lack thereof) of sleep and unwanted behaviors are identified.
Here are some questions that can help parents keep a sleep diary:
- What time does the child go to bed?
— What does the child do before going to bed?
— What happens at home that can affect a child's sleep after he has been put to bed?
— What does the child do before falling asleep?
— What time does the child wake up at night and in the morning?
Does the child sleep during the day?
Based on the basic data collected in the sleep diary, you can choose from several approaches. The following are examples of approaches that can improve sleep behavior in a child with autism.
The following are examples of approaches that can improve sleep behavior in a child with autism.
Bedtime routine
A bedtime routine can help a child because it creates predictability and consistency that leads to bedtime. It is best to make a written or visual schedule for such a routine to ensure that the child follows it clearly. The schedule should list all the activities that precede going to bed, such as brushing your teeth, putting on pajamas, saying goodnight to loved ones, listening to a bedtime story.
The bedtime routine should begin at least 30-60 minutes before going to bed. It is also recommended that parents cut out all caffeinated foods and drinks at least six hours before bedtime, and try to avoid being too active in the evening.
At first, the child may need very high levels of positive reinforcement for following a bedtime routine. Subsequently, parents can provide positive reinforcement to the child the following morning for completing the entire bedtime routine and staying in bed all night. Such reinforcement may include a favorite breakfast cereal, a toy, or a sticker that is placed on a board after waking up (Mindell & Durand, 1993).
Such reinforcement may include a favorite breakfast cereal, a toy, or a sticker that is placed on a board after waking up (Mindell & Durand, 1993).
Extinction procedure for sleep avoidance
Changes in pre-sleep routine are not always sufficient to successfully treat sleep disorders, and other interventions may be required. The choice of procedure depends to a large extent on when the sleep disturbance occurs. In a situation where the child has difficulty falling asleep or wakes up many times during the night, the extinction procedure can be used to avoid sleep. Extinction to avoidance is a common procedure where the reward that supported the behavior is prevented or eliminated. During this procedure, the parents go through a bedtime routine, at the end of which the child is put to bed and left the room. Every time the child wakes up and tries to leave the room, the parents direct the child back to bed without any conversation or interaction with the child. This procedure is repeated until the child begins to stay in bed until he falls asleep (Rickert & Johnson, 1988; France, Blampied, & Wilkinson, 1991).
When implementing sleep avoidance extinction protocols, it is important to ensure that the child is completely safe. For example, if a child has severe behavioral problems, such as hurting himself or climbing on furniture, a modified extinction program can be implemented. In such a program, one of the parents stays in the room and monitors the safety of the child with minimal interaction with him. In addition, parents can install a video surveillance system to monitor the child's safety from another room.
Sleep avoidance extinction procedure
If it is not possible to use the sleep avoidance extinction procedure, parents can use the sleep avoidance extinction procedure. This therapeutic procedure can be used when the child has difficulty falling asleep, wakes up frequently during the night and exhibits protest behavior at night. In gradual extinction, the procedure also begins with putting the child to bed and leaving the room (Durand, 1998).
If the child starts crying or protesting, then the parents wait a predetermined period of time and only then go to the child. This pre-response pause will systematically increase until the child falls asleep before the parents arrive (Durand & Mindell, 1990).
This pre-response pause will systematically increase until the child falls asleep before the parents arrive (Durand & Mindell, 1990).
Pay per response sleep time reduction
Another option is the pay per response sleep time reduction procedure (Piazza & Fisher, 1991). First, it is necessary to determine how long after going to bed the child actually falls asleep (according to the sleep diary). By this time, 30 minutes are added, this will be the new time for putting the child to bed. For example, if a child is put to bed at eight in the evening, and he falls asleep at half past nine, then he will need to be put to bed at nine in the evening. Once the new time is set, it is very important that the child is awake until 9 p.m. to increase the likelihood that he will be quite tired by this time. If the child falls asleep within 15 minutes after being laid down, then the time gradually decreases to the previous 30 minutes per day (that is, the next day the child should be put to bed not at nine in the evening, but at half past eight). If the child does not fall asleep within 15 minutes after going to bed, then he must be raised from the bed for about 15 minutes. During this time, the child is not encouraged to fall asleep, but is not offered any exciting activities. The goal is to increase the child's motivation to fall asleep. At the end of the 15-minute interval, the child is put back into bed. This procedure is repeated until the child falls asleep. In this case, the next day, the time for going to bed is shifted 30 minutes later (the child is put to bed not at nine in the evening, but at half past ten). A similar cycle is repeated until the child falls asleep at the time that was originally determined by his parents.
If the child does not fall asleep within 15 minutes after going to bed, then he must be raised from the bed for about 15 minutes. During this time, the child is not encouraged to fall asleep, but is not offered any exciting activities. The goal is to increase the child's motivation to fall asleep. At the end of the 15-minute interval, the child is put back into bed. This procedure is repeated until the child falls asleep. In this case, the next day, the time for going to bed is shifted 30 minutes later (the child is put to bed not at nine in the evening, but at half past ten). A similar cycle is repeated until the child falls asleep at the time that was originally determined by his parents.
Scheduled awakenings
If your child has difficulty staying asleep and wakes up during the night, a procedure called scheduled awakenings can help. Using sleep diary data, parents determine when the child most often wakes up during the night and wake the child up about 30 minutes before that time by gently touching and talking to the child. As soon as the child wakes up, the parents let him fall asleep again. The plan continues until the child sleeps through the night without waking up on his own for 5-7 days in a row. Once this criterion is reached, scheduled awakenings can be skipped one per week until the child can sleep through the night on his own (Rickert & Johnson, 1988).
As soon as the child wakes up, the parents let him fall asleep again. The plan continues until the child sleeps through the night without waking up on his own for 5-7 days in a row. Once this criterion is reached, scheduled awakenings can be skipped one per week until the child can sleep through the night on his own (Rickert & Johnson, 1988).
Pass out of bed
Very often the child resists attempts to put him to bed, calls his parents or gets out of bed to find them. One possible intervention to correct this behavior is skipping out of bed. Parents give the child a "pass" that can be exchanged for the ability to get out of bed for a short period of time. Such a pass can be a small business card with the name of the child. Such a rise should be short and related to a specific goal, for example, to drink, go to the toilet, hug your mother. As soon as the pass is used, the child gives it to the parent until the next evening. Depending on how often the child gets up or calls for parents (as shown in the sleep diary), additional passes can be given to the child. If the child exhibits problematic sleep-related behaviors after using the gaps, then the parents should use the sleep avoidance extinction procedure discussed above.
If the child exhibits problematic sleep-related behaviors after using the gaps, then the parents should use the sleep avoidance extinction procedure discussed above.
Sleep disorders are a very common problem faced by families of children with disabilities. Because sleep management often involves sleep interruption for those working on this plan, it's important to discuss the plan with the parents and see if they can follow it. As a rule, such plans need to be modified to better suit the lifestyle of a particular family. As with any other type of treatment, it is very important that all family members behave consistently according to the plan. Even sibling play can play an important role in correcting sleep problems, as they can demonstrate to the child how to behave properly at bedtime and stay in bed all night. Applying research-based approaches and a great deal of patience and perseverance can save many families of children with autism from chronic sleep deprivation.
Ref.

Durand, V. M. (1998). Sleep better! A guide to improving sleep for children with special needs. Baltimore, MD: Paul H. Brookes Publishing.
Durand, V. M. & Mindell, J. A. (1990). Behavioral treatment of multiple childhood sleep disorders. Behavior Modification, 14, 37-49.
France, K. G., Blampied, N. M., & Wilkinson, P. (1991). Treatment of infant sleep disturbance by trimeprazine in combination with extinction. Journal of Developmental Behavior and Pediatrics, 12, 308-314.
Friman, P., Hoff, K. E., Schnoes, C., Freeman, K. A., Woods, D. W., Blum, N. (1999). The bedtime pass: An approach to bedtime crying and leaving the room. Archives of Pediatric and Adolescent Medicine, 153, 1027-1029.
Lamberg, L. (1994). Bodyrhythms: Chronobiology and peak performance. New York: William Morrow & Company.
Lozoff, B., Wolf, A. W., & Davis, N. C. (1985). Sleep problems seen in pediatric practice. Pediatrics, 75, 477-483.
Mindell, J. A., & Durand, V.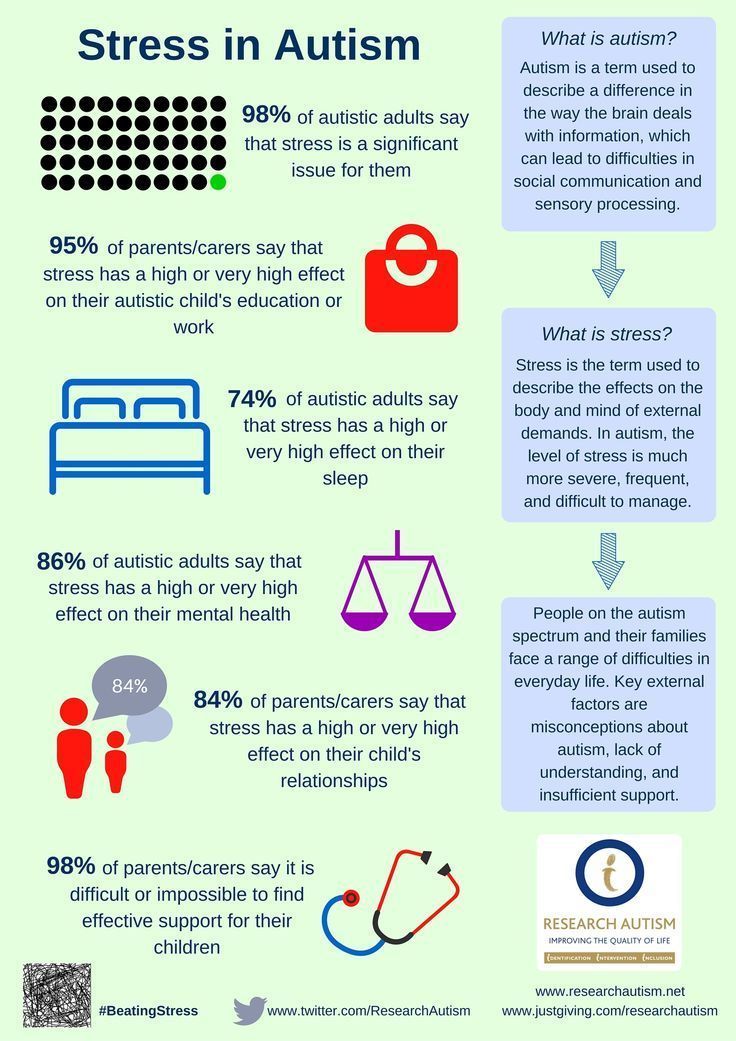 M. (1993). Treatment of childhood sleep disorders: Generalization across disorders and effects on family members. Journal of Pediatric Psychology, 18, 731-750.
M. (1993). Treatment of childhood sleep disorders: Generalization across disorders and effects on family members. Journal of Pediatric Psychology, 18, 731-750.
Piazza, C. C., & Fisher, W. (1991). A faded bedtime with response cost protocol for treatment of multiple sleep problems in children. Journal of Applied Behavior Analysis, 24, 129-140.
Rickert, V., & Johnson, M. (1998). Reducing nocturnal awakening and crying episodes in infants and young children: A comparison between scheduled awakenings and systematic ignoring. Pediatrics, 81, 203-212.
We hope that the information on our website will be useful or interesting for you. You can support people with autism in Russia and contribute to the work of the Foundation by clicking on the "Help" button.
ABA Therapy and Behavior, Comorbidities
Autism in Children: How to Improve Sleep
06/03/13
Sleep disturbances are a common problem in autism that affects the child's behavior throughout the day
9002
Most parents have had negative experiences with a child who never gets to sleep, often wakes up in the middle of the night and/or sleeps only a couple of hours each night. Temporary sleep difficulties are "expected" at a certain stage of a child's development. Sleep disturbances that persist and do not improve over time adversely affect the child, parents, and all family members. It appears that these sleep disturbances are much more common and more intense in children with autism spectrum disorders than in children with typical development.
Temporary sleep difficulties are "expected" at a certain stage of a child's development. Sleep disturbances that persist and do not improve over time adversely affect the child, parents, and all family members. It appears that these sleep disturbances are much more common and more intense in children with autism spectrum disorders than in children with typical development.
There are several factors that need to be taken into account in order to maintain a normal sleep pattern. First, the child should be tested for hidden medical problems that may be affecting sleep. Consider testing for allergies or intolerances to various foods and environmental substances, digestive disorders, and epilepsy. All of these problems are common in people with autism. Also, sleep disturbances can be a side effect of medications that the child is taking, and this option must also be considered.
Sleep disorders
Sleep disorders that are common in the general population should be excluded from your child. Sleep apnea is a disorder that can affect anyone at any age. In this disorder, a person stops breathing for a few seconds due to airway obstruction during sleep. The most common cause of sleep apnea is enlarged tonsils or adenoids. Upper respiratory illnesses and/or allergies can also contribute to sleep apnea. In addition to holding the breath, the symptoms of sleep apnea in children include: snoring, mouth breathing, restless sleep, sweating, waking at night, and/or frequent coughing or difficulty breathing during sleep.
Sleep apnea is a disorder that can affect anyone at any age. In this disorder, a person stops breathing for a few seconds due to airway obstruction during sleep. The most common cause of sleep apnea is enlarged tonsils or adenoids. Upper respiratory illnesses and/or allergies can also contribute to sleep apnea. In addition to holding the breath, the symptoms of sleep apnea in children include: snoring, mouth breathing, restless sleep, sweating, waking at night, and/or frequent coughing or difficulty breathing during sleep.
The child should be evaluated for other sleep disturbances, if appropriate, including night terrors (waking in deep sleep in a state of extreme fear and confusion) and incomplete awakenings. These disorders are often referred to as parasomnias. Parasomnia is a disorder caused by "partial awakenings" that causes unusual behavior during sleep. Children with sensory impairments often have difficulty falling asleep and waking up at night. Consultation and evaluation with a sensory integrator can help identify relaxation and arousal problems in the nervous system and develop strategies to address these problems.
Having ruled out medical problems, we need to consider other factors that affect sleep and develop strategies that affect them. These factors include: environmental factors, bedtime schedules, and consistent bedtime training. Each of these approaches is discussed below.
Environmental factors
After analyzing your child's sleep environment, you may decide to make some adaptations and modifications to help your child relax more during sleep.
Consider whether the child might be too hot or too cold. Monitor the air temperature, evaluate the baby's blanket and sleepwear, and decide which combination is best for him. Be aware that your child may perceive temperature in a completely different way than you. Try to determine what temperature the child prefers and at what temperature he is most comfortable during the day, and based on this make decisions about the optimal temperature at night.
Consider whether tactile sensitivity might affect your child's ability to sleep. Some types of fabric can relax or tone the baby. Pay attention to the fabric of bed linen and pajamas. The child may or may not like to have their feet covered in pajamas or socks. Some children have problems with how close the clothes are to the body, or how stretchy they are. In addition, for a child with autism, it may be important that the blanket is optimally pressed against the skin.
Some types of fabric can relax or tone the baby. Pay attention to the fabric of bed linen and pajamas. The child may or may not like to have their feet covered in pajamas or socks. Some children have problems with how close the clothes are to the body, or how stretchy they are. In addition, for a child with autism, it may be important that the blanket is optimally pressed against the skin.
Think about environmental noise and how it affects your child. When your child is trying to relax and sleep, the little noises he hears can be unbearable because the child cannot distract himself from them. Noises such as tap water or a dog scratching may not affect you or other family members in any way, but they can make it difficult for a child with autism spectrum disorder to fall asleep. Could any sounds in the house be related to your child's sleep? Sometimes in such cases, it is easier for a child to fall asleep to constant and soothing noise that drowns out other sounds in the room - an air freshener, a fan, a TV or quiet music.
In addition, the child may be disturbed by visual stimuli. Is the child afraid of the dark? Some children with autism prefer dark places during the day, but things may be different on a bed in a dark room. Street lights, the moon, or car headlights shining into the room at random intervals can interfere with a child's sleep. It is very important that the child sleeps in a room that is equally dark or light at all times, depending on your child's needs.
Bedtime schedules and autism
Bedtime schedules and rituals are important for almost any child's sleep, but they become extremely important for children with autism. It is very important for your child to always go to bed at the same time. Pick a reasonable bedtime that you can insist on under any circumstances.
It is important for children with autism to know what is happening and what will happen next. Create a bedtime schedule that can keep them predictable, comfortable, and familiar. This understanding and structure can provide a visual timetable for bedtime. A visual schedule can also serve as a reminder and provide stability for all other family members.
This understanding and structure can provide a visual timetable for bedtime. A visual schedule can also serve as a reminder and provide stability for all other family members.
A good bedtime schedule should include only activities that help the child relax, calm down and prepare for sleep. For example, washing in the bathroom may be associated with very strong sensory stimulation or frighten the child. In this case, you do not need to include a bath in the schedule for the evening, it is better to wash the child at another time. On the other hand, if there are sensory integration exercises that relax your child, then you should schedule them as part of your bedtime schedule.
The bedtime schedule should remain the same each day, and should include activities that are enjoyable and relaxing that suit your child's individual needs and interests. A realistic bedtime schedule should consist of 4-6 items, and should not take up the entire evening.
Activities that could be an evening ritual and part of a visual schedule before bed could include: reading aloud or looking at the same book or story every night, saying goodnight to your favorite toys or objects, washing your face, taking a bath, putting on pajamas , brushing your teeth, drinking a glass of water, singing your favorite song, praying, listening to your favorite and soothing music, hugging and kissing family members, and/or doing sensory integration relaxation exercises.
On days when you are away from home or come home very late, it is still very important to follow a schedule and bedtime rituals. You can shorten each step, but following a schedule is important to reduce your child's frustration with the change. Even in a completely new environment, a familiar routine can have a calming effect. Once you get home, the bedtime schedule will continue to be effective, although changes in environment may require one evening or more of adjustment, depending on how long the child has been away from home.
Sleep training and autism
Once you've dealt with possible medical issues, environmental factors, and bedtime schedules, the hardest part of getting a good night's sleep remains: getting your child to sleep through the night. There are different versions of sleep training that you may have read about. The easiest way is after you've completed your bedtime schedule and your baby is in bed, leave the room without saying anything and don't try to touch the baby.
If the child is upset or obviously awake, wait a few minutes and then return to the room to check on how he is. Checking means you briefly enter the room (no longer than a minute, less is better), touch, massage, maybe say high five or hug the child if he responds well to such actions. Then say softly but firmly, "It's okay, it's time for bed, you're fine," or something similar, and then leave the room until the next check or until the child falls asleep.
Consistent application of this technique is harder on the parent than on the child. The first few evenings it can take up to two hours. It is very important to know that in the early days the child's behavior may worsen before it gets better. This is a normal way for the child to test the new order and try to return to a more familiar routine. For older children, who may not really be tired when it's time for bed, just being in bed or in a quiet room can become a routine. In these situations, sleep training methods may still work. You can use a gate or other barrier on the bedroom door to remind your child that it's bedtime and they should stay in their room.
You can use a gate or other barrier on the bedroom door to remind your child that it's bedtime and they should stay in their room.
If your older child never sleeps through the night, you yourself may be suffering from severe sleep deprivation. Seek help from a doctor or psychologist. You can ask other parents if they know of a good specialist who can help. In addition, if your child's sleep patterns are regressing, specialist advice may be needed. Again, it is best to start with a medical examination. Sometimes, if other medical problems have been ruled out, sleep problems can be treated with temporary medication. When taking medication, it is very important to simultaneously work on a bedtime schedule and rituals that are appropriate for your child.
Melatonin, sleep and autism
Some autism scientists have conducted preliminary studies on the short-term use of the over-the-counter nutritional supplement melatonin. This drug helps stabilize sleep patterns and promotes normal sleep in some children by helping them fall asleep faster. The few studies that exist at the moment, however, warn that sometimes melatonin stops working, and it usually does not help those who wake up frequently during the night. In addition, the effects of long-term use of melatonin are still unknown. Some parents also find that vitamin supplements help their children sleep better.
The few studies that exist at the moment, however, warn that sometimes melatonin stops working, and it usually does not help those who wake up frequently during the night. In addition, the effects of long-term use of melatonin are still unknown. Some parents also find that vitamin supplements help their children sleep better.
Children with autism often have difficulty falling asleep, sleeping only a couple of hours, or waking up frequently during the night. These sleep patterns are easy to come by, but very difficult to change. One of the problems that has not yet been discussed in this article is the habit of sleeping with the child. This habit can develop when a child's sleep disturbance affects not only the child, but also the parents and the rest of the family.
If the child is accustomed to sleeping with parents and/or in the parent's bed, the same steps are needed as described above, but additional support will be needed in assessing environmental factors and developing a bedtime schedule.