How soon can you feel braxton hicks
Braxton Hicks contractions | Pregnancy Birth and Baby
Braxton Hicks contractions | Pregnancy Birth and Baby beginning of content4-minute read
Listen
If you feel tightening or cramping in your abdomen during your pregnancy, you may be having Braxton Hicks contractions. This is normal and not a sign that you’re ready to give birth.
Braxton Hicks contractions are sometimes called ‘false’ or ‘practice’ contractions.
What are Braxton Hicks contractions?
Braxton Hicks contractions are a tightening in your abdomen that comes and goes. They are contractions of your uterus in preparation for giving birth. They tone the muscles in your uterus and may also help prepare the cervix for birth.
Braxton Hicks contractions don’t cause labour and aren’t a sign that labour is beginning.
If you’re not sure whether what you’re experiencing is Braxton Hicks contractions or actual labour, contact your doctor or midwife. They will be able to tell by doing a vaginal examination — if there are no signs that your cervix is changing, it is not labour.
What do they feel like?
Braxton Hicks contractions feel like muscles tightening across your belly, and if you put your hands on your belly when the contractions happen, you can probably feel your uterus becoming hard.
The contractions come irregularly and usually last for about 30 seconds. While they can be uncomfortable, they usually aren’t painful.
If the pain or discomfort of your contractions eases off, they’re probably Braxton Hicks contractions.
When do you get them?
Braxton Hicks contractions occur from early in your pregnancy but you may not feel them until the second trimester. If this is your first pregnancy, you might start to feel them from about 16 weeks. In later pregnancies, you may feel Braxton Hicks contractions more often, or earlier. Some women won’t feel them at all.
Some women won’t feel them at all.
In late pregnancy, you may experience Braxton Hicks contractions more often — perhaps as much as every 10 to 20 minutes. This is a sign that you are preparing for labour — known as prelabour.
How are Braxton Hicks contractions different from labour pain?
There are some differences between Braxton Hicks contractions and true labour contractions that will help your doctor or midwife decide whether you are in labour:
Braxton Hicks contractions:
- don’t result in your cervix thinning and opening
- usually last for about 30 seconds
- can be uncomfortable, but usually aren’t painful
- come and go at irregular times
- usually occur no more than once or twice an hour (until late in the pregnancy), a few times a day
- usually stop if you change position or activity or go for a walk
- usually go if you have a warm bath or shower
Real labour contractions:
- result in your cervix thinning and opening
- last 30 to 70 seconds
- become very regular
- get closer together
- last longer as time goes by
- get stronger or come more often when you walk
- get stronger over time
Should I call my doctor or midwife?
If you are less than 37 weeks pregnant, contractions can be a sign of premature labour. Contact your doctor or midwife immediately if:
Contact your doctor or midwife immediately if:
- you feel pain, pressure or discomfort in your pelvis, abdomen or lower back
- the contractions become stronger, closer together and more regular
- there is fluid leaking or gushing from your vagina
If you are full-term, you may choose to wait until a bit later in your labour, depending on what you have arranged with your doctor or midwife. If your waters break, or your contractions are strong and 5 minutes apart, it’s time to go to the hospital.
As any stage of pregnancy, you should contact your doctor or midwife immediately if you:
- you have persistent pain in your abdomen
- you have vaginal bleeding
- you notice your baby’s movements have slowed or stopped
- you feel very unwell
If you are in doubt, don’t hesitate to call your doctor or midwife for advice.
How can I ease the discomfort?
Braxton Hicks contractions are normal and don’t need treatment. But if you feel uncomfortable, you can try:
But if you feel uncomfortable, you can try:
- lying down
- taking a walk
- relaxing in a warm bath
- having a massage
It may help to practise your breathing exercises during your Braxton Hicks contractions.
Sources:
Raising Children Network (23 weeks pregnant), RANZCOG (Labour and birth), Elsevier Patient Education (Braxton Hicks Contractions)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Giving birth - stages of labour
- Health professionals involved in your pregnancy
- Signs of premature labour
Need more information?
Pregnancy at week 22
By week 22, some parts of your baby’s body are fully formed, while some women experience Braxton Hicks contractions about now.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 35
You'll probably be having lots of Braxton Hicks contractions by now. It's your body's way of preparing for the birth. They should stop if you move position.
Read more on Pregnancy, Birth & Baby website
Giving birth - contractions
Contractions are when the muscles in your uterus tighten and then relax. They occur throughout the later stages of your pregnancy.
Read more on Pregnancy, Birth & Baby website
What happens to your body in childbirth
During childbirth, the body’s hormones and muscles, as well as the shape of the pelvis, all work together to bring the baby safely into the world.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth - uterus
The uterus is your growing baby’s home during pregnancy. Learn how the uterus works, nurtures your baby and how it changes while you are pregnant.
Read more on Pregnancy, Birth & Baby website
Preterm labour - MyDr.com.au
Going into labour before your 37th week of pregnancy is called preterm labour, or premature labour. Find out what it means for you and your baby.
Read more on myDr website
38 weeks pregnant | Raising Children Network
38 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.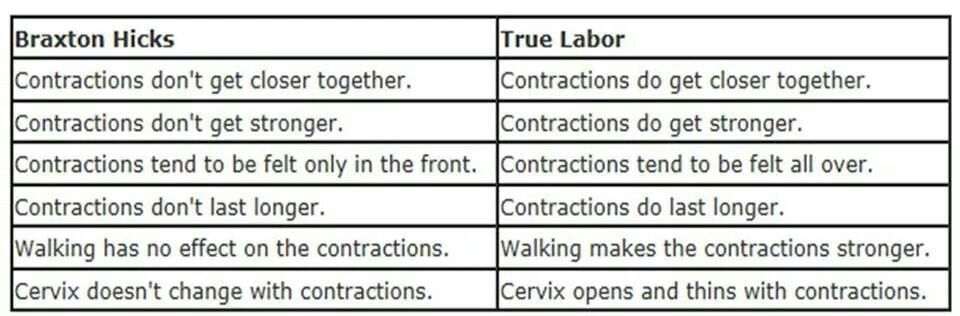
Read more on raisingchildren.net.au website
26 weeks pregnant | Raising Children Network
26 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.
Read more on raisingchildren.net.au website
Giving birth - early signs of labour
You can know the early signs of labour, even if you cannot predict when your labour will begin. Find out also what to do if something appears to be wrong.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth
From conception to giving birth, a woman's body goes through many physical changes.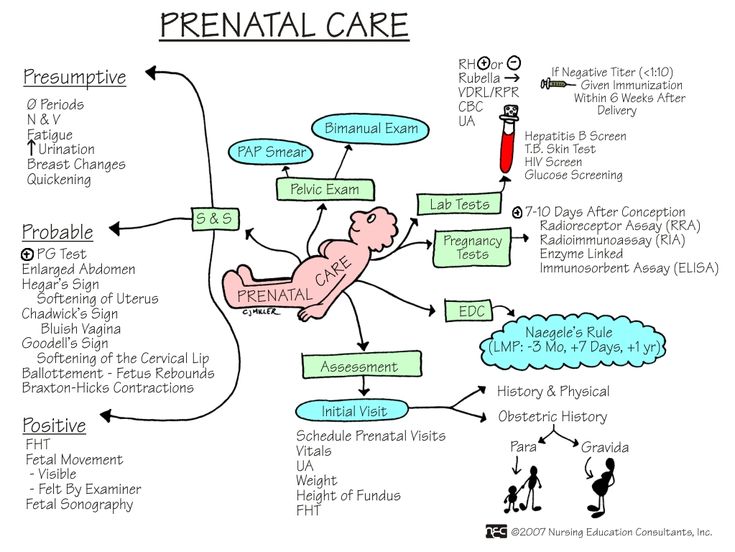 Learn what happens to your body during pregnancy and labour.
Learn what happens to your body during pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Braxton Hicks Contractions | American Pregnancy Association
You might have heard this funny phrase before you were pregnant, but now you want to know what it means. The term originated in 1872 when an English doctor named John Braxton Hicks described the contractions that occur before real labor. Imagine constantly thinking, “This must be it,” only to find out that it wasn’t. Doctors and pregnant women have Dr. Hicks to thank for eliminating the confusion. The following information should be helpful in determining the difference between true labor and Braxton Hicks contractions.
Doctors and pregnant women have Dr. Hicks to thank for eliminating the confusion. The following information should be helpful in determining the difference between true labor and Braxton Hicks contractions.
Braxton Hicks contractions can begin as early as the second trimester. However, they are most commonly experienced in the third trimester. When this happens, the muscles of the uterus tighten for approximately 30 to 60 seconds, and sometimes as long as two minutes.
Braxton Hicks are also called “practice contractions” because they are a preparation for the real event and allow the opportunity to practice the breathing exercises taught in childbirth classes.
What do Braxton Hicks contractions feel like?
Braxton Hicks contractions start as an uncomfortable but painless tightening that begins at the top of your uterine muscles and spreads downwards. They cause your abdomen to become very hard and strangely contorted (almost pointy). Once you get closer to your estimated due date, they will become more frequent and intense.
Once you get closer to your estimated due date, they will become more frequent and intense.
They are described as:
- Irregular in intensity and usually last about 15 to 30 seconds, but sometimes as long as two minutes
- Infrequent
- Unpredictable
- Non-rhythmic
- More uncomfortable than painful (although for some women Braxton Hicks can feel painful)
- They do not increase in intensity or frequency
- They taper off and then disappear altogether
If your contractions are easing up in any way, they are most likely Braxton Hicks.
What causes them?
There are possible causes of these contractions. Some physicians and midwives believe that they play a part in toning the uterine muscle and promoting the flow of blood to the placenta. They are not thought to have a role in dilating the cervix but might have some impact on the softening of the cervix.
However, as Braxton Hicks contractions intensify nearer the time of delivery, the contractions are often referred to as false labor. When this occurs, it can help the dilation and effacement process.
When this occurs, it can help the dilation and effacement process.
What triggers them?
The following are triggers of Braxton Hicks:
- When the mother or the baby is very active
- If someone touches the mother’s belly
- When the bladder is full
- After sex
- Dehydration
What can I do to alleviate Braxton Hicks contractions?
- Change positions. You can lie down if you have been standing or go for a walk if you have been sitting or laying
- Take a warm bath for 30 minutes or less
- Because contractions may be brought on by dehydration, drink a couple of glasses of water
- Drink a warm cup of herbal tea or milk
If none of these steps work, you should contact your health care provider.
Want to Know More?
- Signs of Labor
- Pregnancy Pains
- Stages of Labor: Stage 1
Compiled using information from the following sources:
1. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 17.
William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 17.
2. Mayo Clinic Guide To A Healthy Pregnancy Harms, Roger W., M.D., et al, Ch. 11.
Braxton Hicks contractions for how long - 25 recommendations on Babyblog.ru
For fifteen years now we have been living not just in the new century, but in the new millennium. For twenty years we have been using computers and the Internet everywhere. It would seem that with the progress of technology, people have enormous opportunities for the exchange of progressive information, knowledge and best practices. But the real picture is almost the opposite: false, untruthful information, often presented under the “sauce” of intimidation and deceit, is spread and accepted by people faster and easier than truthful and useful information.
The worst thing that is now observed in medicine is the filing of many conditions, including quite normal ones, and some diagnoses as something terrible and dangerous, threatening a person’s life, requiring aggressive and extensive treatment immediately. Obstetrics is no exception. On the contrary, in recent years this branch of medicine has grown in a number of countries into a kind of machine of deliberate harm to a pregnant woman and her unborn child.
Obstetrics is no exception. On the contrary, in recent years this branch of medicine has grown in a number of countries into a kind of machine of deliberate harm to a pregnant woman and her unborn child.
The concept of "commercial diagnosis", introduced by me ten years ago, is no longer denied by many people and is even used by them in everyday life, conversations and discussions of the situation in the healthcare system. Both doctors and people of other specialties began to talk and write about obstetric aggression. Nevertheless, the number of fictitious diagnoses that do not exist in most countries of the world is striking not only by their backwardness, but also by the lack of a logical analysis of the situation, signs, and examination results when they are made (more precisely, invented).
INCOMPATIBILITY OF THE SPOUSES
Usually such a diagnosis sounds when:
- unsuccessful planning of pregnancy and infertility;
- loss of pregnancy, even the first or one;
- spontaneous habitual miscarriages;
- in exceptionally "striking cases" in the presence of one child or several healthy children.
If we talk about some kind of "incompatibility of spouses", then we can only talk about incompatibility of psychological or sexual temperaments, but no other "incompatibility" exists.
Allergic reaction to semen is extremely rare in humans, but the diagnosis would be allergy, not incompatibility.
If a married couple cannot conceive, it may be infertility, which requires proper diagnosis. There are different types of infertility or infertility factors, which means that there will be a different approach to the examination of a married couple and treatment.
Very fashionable commercial HLA (human leukocyte antigen) testing in the world of progressive medicine is used in organ and tissue transplantation, to diagnose a number of autoimmune diseases, confirm paternity and monitor the effectiveness of the treatment of a number of diseases, but has nothing to do with conceiving children, carrying a pregnancy , and even more so with the "incompatibility of the spouses. " "Genetic incompatibility of partners" is another invention for imposing an expensive examination and treatment.
" "Genetic incompatibility of partners" is another invention for imposing an expensive examination and treatment.
If one of the partners has affected genes, that is, there are changes in the form of mutations, then such changes may be associated with problems in conceiving and bearing offspring, but this is not incompatibility. This may be a specific diagnosis (disease, syndrome) on the part of one or both partners. And the recommendations of some doctors to carry out IVF in such cases using the same sexual material, or to find a sexual partner outside of marital relations in order to conceive a child, do not always sound professional.
TOXICOSIS
The concept of "toxicosis" appeared in Soviet obstetrics in the early 1990s, when everyone in the world of progressive medicine had already completely abandoned this concept. Toxicosis means “a state of poisoning” (toxins are poison), and the logical conclusion is that this is pregnancy poisoning, that is, the embryo / fetus poisons the body, and therefore the life of the expectant mother. But doesn’t a mother poison her unborn child with poor-quality food, water, medication, smoking, and even drinking alcohol?
But doesn’t a mother poison her unborn child with poor-quality food, water, medication, smoking, and even drinking alcohol?
In the West, they quickly realized the absurdity of such a “diagnosis” and tried to switch to the concept of “preeclampsia”, that is, a condition associated with gestation (pregnancy). However, this definition was also abandoned very quickly, because the more science and medicine developed, the faster the exchange of advanced information and experience took place, the faster doctors began to understand that many “strange” phenomena during pregnancy are not diseases, but variants of the norm. and vice versa - all complications of pregnancy have specific specific names, which should appear as diagnoses.
In post-Soviet medicine, a completely normal phenomenon - nausea and vomiting at the beginning of pregnancy - is still called early toxicosis (in the rest of the world these are just unpleasant symptoms of this condition), and edema, which for the vast majority of women are normal, hypertension in pregnancy, preeclampsia, eclampsia, and about ten other complications of pregnancy, which are independent diagnoses, and not a comprehensive mythical toxicosis.
Remember: there is no such diagnosis - toxicosis!
UTERINE TONE / HYPERTONE
For the first time, normal uterine contractions from the beginning of pregnancy to the end of childbirth were described by the English physician John Braxton Hicks in 1872. Mistakenly, such contractions are called "training bouts", which is not true. In the publication of this doctor, it was about normal uterine contractions throughout pregnancy, and not before childbirth.
The uterus is a muscular organ, therefore, just like any muscle, it has its own mode of contraction, which depends on many factors and can be observed both outside of pregnancy and during pregnancy.
The diagnosis "tonus" or "hypertonicity" was invented by post-Soviet ultrasound doctors and the rest of the world does not exist in obstetrics, therefore it does not require treatment, and even more so inpatient, with the use of a large number of drugs that have also not been used in modern obstetrics for a long time ("Papaverine" , "No-shpa", "Viburkol", vitamin E, magnesia, etc. )
)
THREAT OF LOSS OF PREGNANCY
I have already raised the topic of "threat of abortion" more than once, especially since it is consonant with the topic of "preservation of pregnancy". In reality, the threat to a pregnant woman comes more from the medical staff than really from someone else or something (nature), because it is people who intimidate, put pressure on the psyche with negative scenarios, escalate the situation, harm with unsafe treatment.
The only diagnosis in obstetrics that has a word root consonant with “threat” is “threatened abortion”. This diagnosis is made according to strict criteria, and not because of “tone / hypertonicity of the uterus”, it does not require treatment, because there is no cure.
All other types of threats are fictitious diagnoses. In obstetrics, it is customary to talk about risk factors and determine the group or degree of risk for the development of one or another pregnancy complication (low risk, high risk). Against the background of the presence of various risk factors, pregnancy can proceed quite normally and end safely.
RH AND GROUP CONFLICT
In modern obstetrics there is no such concept or diagnosis as "Rh conflict" or "group conflict". Worst of all, such a “diagnosis” intimidates a married couple to such an extent that she refuses to conceive children: since it is absolutely impossible to get pregnant, then we are not trying. The presence of different blood types, as well as different Rh factors, is a normal phenomenon in human life and is not considered any conflict.
In modern obstetrics, there are more than 50 blood markers (antigens) for which antibodies (immunoglobulins) can be produced, and this condition is called alloimmunization, or sensitization.
During pregnancy, antibodies can be produced in the mother's body against fetal antigens, cross the placenta and destroy the fetal red blood cells, leading to anemia and fetal hemolytic disease. If hemolytic disease of the fetus occurs, then it will end either with the death of the fetus, or the birth of a child with hemolytic disease of the newborn. Unfortunately, many doctors do not understand the types of jaundice, do not know the current norm of bilirubin levels, so the diagnosis of "hemolytic disease of the newborn" in most cases turns out to be false, which means that aggressive treatment of such children is absolutely inappropriate.
Unfortunately, many doctors do not understand the types of jaundice, do not know the current norm of bilirubin levels, so the diagnosis of "hemolytic disease of the newborn" in most cases turns out to be false, which means that aggressive treatment of such children is absolutely inappropriate.
If we talk about really rare "blood conflicts", then they arise not between a man and a woman, but between a mother and a fetus. Therefore, the enthusiasm of some doctors for the search for antibodies in the blood of a man is so surprising. Also depressing is the fact of searching for antibodies in the mother's blood after childbirth in order to make a diagnosis of "hemolytic disease of the newborn." And the use of such a dangerous procedure as plasmapheresis, supposedly to “cleanse the blood” of antibodies, is shocking. This procedure has passed into the category of commercial ones, because it is expensive and brings considerable income to those who carry it out.
For the prevention of Rh sensitization in the mother, vaccination with immunoglobulins (D-antibodies) has long been used, which is carried out in the absence of a woman's own antibodies during pregnancy, after childbirth, abortion, and a number of procedures. This prophylaxis does not protect the current pregnancy, but it does prevent hemolytic disease of the fetus and newborn in subsequent pregnancies. However, it is ineffective in preventing sensitization for all other blood markers.
This prophylaxis does not protect the current pregnancy, but it does prevent hemolytic disease of the fetus and newborn in subsequent pregnancies. However, it is ineffective in preventing sensitization for all other blood markers.
HEREDITARY (GENETIC) THROMBOPHILIA
In post-Soviet obstetrics, over the past decade, there have been an extremely large number of positions of geneticists who do not understand prenatal genetic screenings and genetics in general, and hematologists (they are fashionably called hemostesiologists, hemastesologists), who do not understand blood and know absolutely nothing about normal changes in the composition of the blood, especially the blood coagulation system in pregnant women.
During pregnancy, blood viscosity increases despite an increase in blood (plasma) volume and a decrease in the concentration of many substances. Therefore, from the very first weeks, pregnancy is accompanied by a hypercoagulable state. It can persist for several weeks, not only after childbirth, but also after abortions and missed pregnancies. This is not a pathological condition, but normal physiological changes.
This is not a pathological condition, but normal physiological changes.
D-dimer, according to the level of which heparin is prescribed to all pregnant women in a row, is a derivative of fibrinogen. Both of these indicators increase from the first weeks of pregnancy, which is absolutely normal.
Commercially profitable genetic testing leads to the diagnosis of thrombophilia being overused, although several dozen diseases are known to be associated with disorders of the blood clotting process. There are several types of hereditary thrombophilia that have a clear name, and not just "genetic thrombophilia". There are also acquired thrombophilias, which often turn out to be not a separate diagnosis, but a laboratory and clinical symptom of other diseases.
The presence of genes and their combinations does not mean that a person has thrombophilia (and many other diseases). This may indicate a hereditary predisposition, but without clinical and laboratory confirmation, and even more so outside the state of pregnancy, such diagnoses are not made and blood thinning drugs are not prescribed.
Bed rest in hospitals, where pregnant women are kept for weeks and even months, is recognized as the most dangerous factor in the formation of blood clots. It is also surprising that before pregnancy, many women had no idea about their "genetic disease", they took hormonal contraceptives that are incompatible with thrombophilia, and then after giving birth they continue to take them, forgetting about the terrible diagnosis. However, doctors quickly forget about him too.
OLD PLACENTA
The diagnosis of "old placenta", which often sounds in conjunction with the diagnosis of "uteroplacental insufficiency", was born by the same ultrasound specialists.
The placenta is a dynamic organ that undergoes regular changes as pregnancy progresses. Therefore, we can safely say that not only the placenta is aging, but also the fetus itself. The woman also gets older by 9 months!
Placenta insufficiency can be spoken of only when it does not fulfill its function. Just as there is heart or liver failure, placental failure can also exist. But its presence can only be determined by the state of the fetus. If the fetus develops normally and does not lag behind in growth (for this, growth charts must be kept and the exact gestational age must be known), then what kind of placental insufficiency can we talk about?
But its presence can only be determined by the state of the fetus. If the fetus develops normally and does not lag behind in growth (for this, growth charts must be kept and the exact gestational age must be known), then what kind of placental insufficiency can we talk about?
But what is depressing in all these stories with placentas is that a woman is offered different schemes for "rejuvenation" of the placenta, which necessarily include two fuflomycins - "Kurantil" and "Actovegin". Remember: the placenta cannot be rejuvenated!
In addition, the diagnosis "placentitis" suddenly became fashionable, which was indeed used in veterinary medicine for a very long time, but never in obstetrics! Turning pregnant women into female animals?
oligohydramnios/polyhydramnios tendencies
When I hear or read about the diagnosis of oligohydramnios/polyhydramnios tendency, I want to respond with a great sense of humor: “You know, we all have a lot of tendencies. For example, there is a real tendency with age to get senile dementia. You can buy a lottery ticket - there will be a tendency to enrich. We sit in a car, drive along a highway - we tend to get into a traffic accident and even die. That's right, life tends to end. This means that pregnancy tends to end in term birth and the birth of a healthy baby.
You can buy a lottery ticket - there will be a tendency to enrich. We sit in a car, drive along a highway - we tend to get into a traffic accident and even die. That's right, life tends to end. This means that pregnancy tends to end in term birth and the birth of a healthy baby.
The extremely common diagnosis of "trends" is often the product of ultrasound specialists who somehow do not use the logical thinking of obstetrician-gynecologists to ask a simple question: what kind of nonsense is this?
The state of amniotic fluid is only in the form of a norm, polyhydramnios and oligohydramnios, but there are no trends. These conditions are determined by measuring one pocket (column) of amniotic fluid in centimeters, but most often by the sum of four (namely four, not two or three) pockets, that is, by determining the amniotic index of amniotic fluid (AIF). After 20 weeks, the normal AIH ranges from 8 to 24 cm, of course, adjusted for the condition of the fetus and other ultrasound findings.
Oligohydramnios and polyhydramnios are practically not treated, therefore, volumetric regimens of antibiotics and fuflomycins, the same "Kurantil", "Actovegin", "Khofitol", "Viferon", "Tivorin" and other similar drugs, and with the obligatory presence of a pregnant woman in a hospital , is a manifestation of medical illiteracy.
fetal asphyxia
Most often, the diagnosis of fetal asphyxia appears in the conclusions of pathologists after pregnancy loss, as well as in stillbirth. Surprisingly, it is specialists who do not see the difference between hypoxia and asphyxia, who are just obliged to find out the cause of abortion and fetal death.
The baby is not breathing inside the uterus. His lungs don't work. Everything he receives from his mother in the form of nutrients and oxygen comes through the umbilical cord. The concept of hypoxia implies a violation of blood flow in the vessels of the fetus (impaired hemodynamics) due to the presence of usually two parallel conditions - anemia (anemia) and acidosis (increased acidity) due to oxygen starvation of tissues.
Asphyxia is understood as suffocation, which is associated with a decrease and even cessation of oxygen supply through the respiratory system. At the same time, the oxygen content in the blood drops sharply, which leads to brain death and death. Since the fetus is not breathing, it cannot have asphyxia.
Asphyxia of a newborn is said when a foreign body (amniotic fluid, mucus, meconium, blood, etc.) enters the child's respiratory tract after birth with the first or subsequent breaths. Therefore, the diagnosis of "fetal asphyxia" simply does not exist, and if it is present in the conclusions of the pathoanatomical examination (autopsy), this indicates the unprofessionalism of the doctor.
Braxton-Hicks contractions. How to distinguish between false and real contractions?
Braxton-Hicks contractions or false labor contractions are irregular contractions and relaxation of the muscles of the uterus as a way of preparing for true labor. They are thought to start around 6 weeks of gestation but are not usually felt until the 2nd or 3rd trimester.
False contractions are a normal part of pregnancy. They may be uncomfortable, but not painful. Women describe them as a feeling that feels like mild menstrual cramps or tightness in a specific area of the abdomen that quickly resolves.
They are also irregular in duration and intensity, occur infrequently, are unpredictable and not rhythmic, and are more uncomfortable than painful.
Braxton Hicks contractions tend to increase in frequency and intensity towards the end of pregnancy. Women often mistake Braxton Hicks contractions for real labor. However, unlike real contractions, they do not dilate the cervix and result in the birth of a baby.
Braxton Hicks contractions occur when the muscle fibers of the uterus contract and relax. The exact etiology of Braxton Hicks contractions is unknown. However, there are circumstances that can cause them:
- when the woman is very active,
- when the bladder is full,
- after sexual activity,
- when a woman is dehydrated.

Common among all these circumstances is the potential stress on the fetus and the need for increased blood flow to the placenta to provide oxygen to the fetus.
- Change position or activity level: if you were very active, lie down; if you have been sitting for a long time, go for a walk.
- Relax: take a warm bath, massage, read a book, listen to music or take a nap.
If you have Braxton Hicks contractions or if they continue and become more frequent and intense, you should see your doctor.
When assessing for Braxton Hicks contractions, there are a few key questions to ask yourself. We have prepared a table for you with questions, the answers to which will help you understand what kind of contractions you have:
| Braxton Higgs contractions | Real labor pains | |
|---|---|---|
| How often do contractions occur? | Irregular and do not increase over time. |