How many epipens should a child have
How Many Epinephrine Auto-injectors Should Your Child Have On Hand?
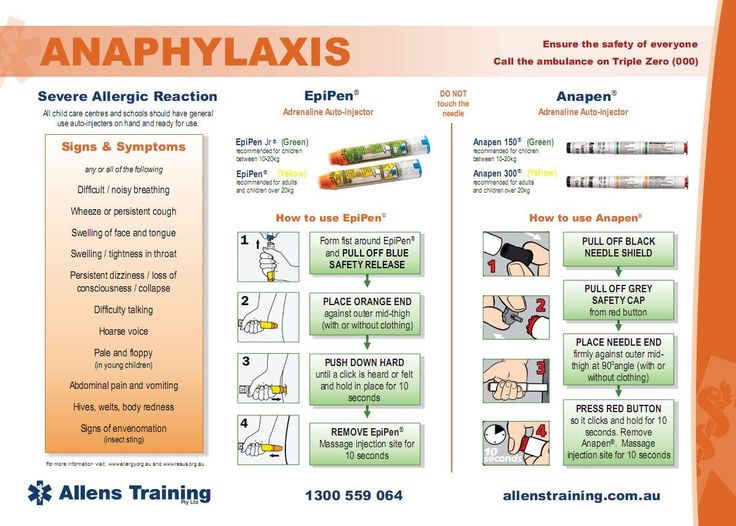
While we usually write about common food allergy symptoms, such as diarrhea or eczema, more severe reactions like anaphylaxis are possible for many children and adults with allergies. Allergens that cause anaphylaxis include food, insect stings, drugs, latex, and even exercise. When anaphylaxis happens as a result of contact with an allergen, a rapid immune reaction occurs that can quickly make breathing very difficult. For those patients an immediate injection of epinephrine can prevent very serious complications. Sometimes even the few minutes it takes emergency medical care to arrive is too long, and a personal device with automated injectable epinephrine, an auto-injector, is essential.
The EpiPen®, made by Mylan, delivers a quick shot of epinephrine to the thigh. Other similar devices are available, such as the Adrenaclick® by Amedra Pharmaceuticals.
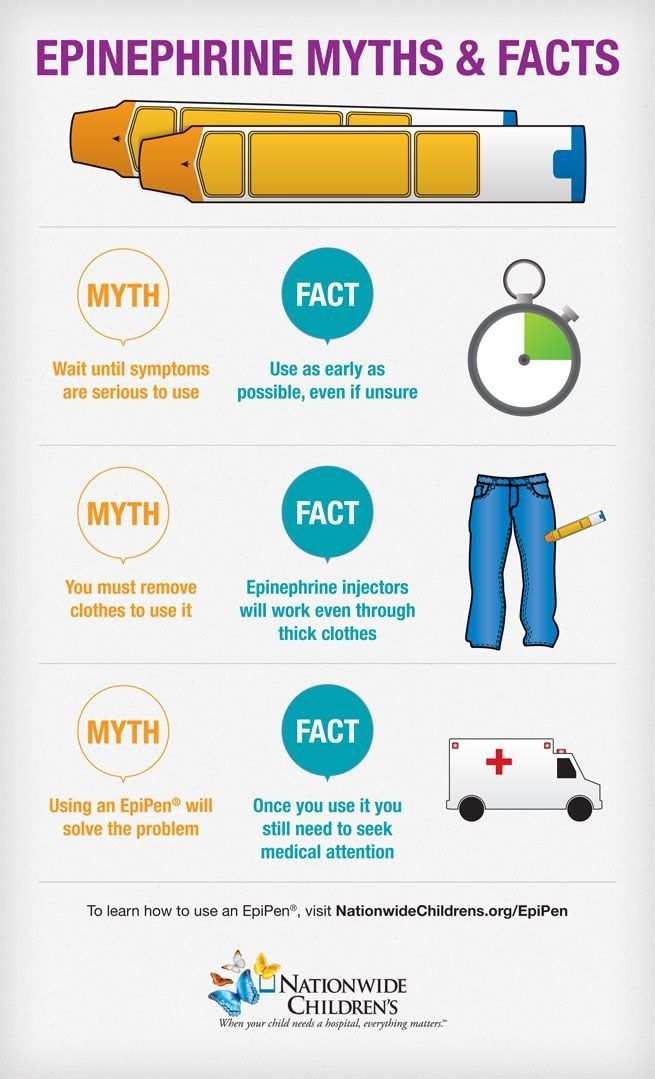
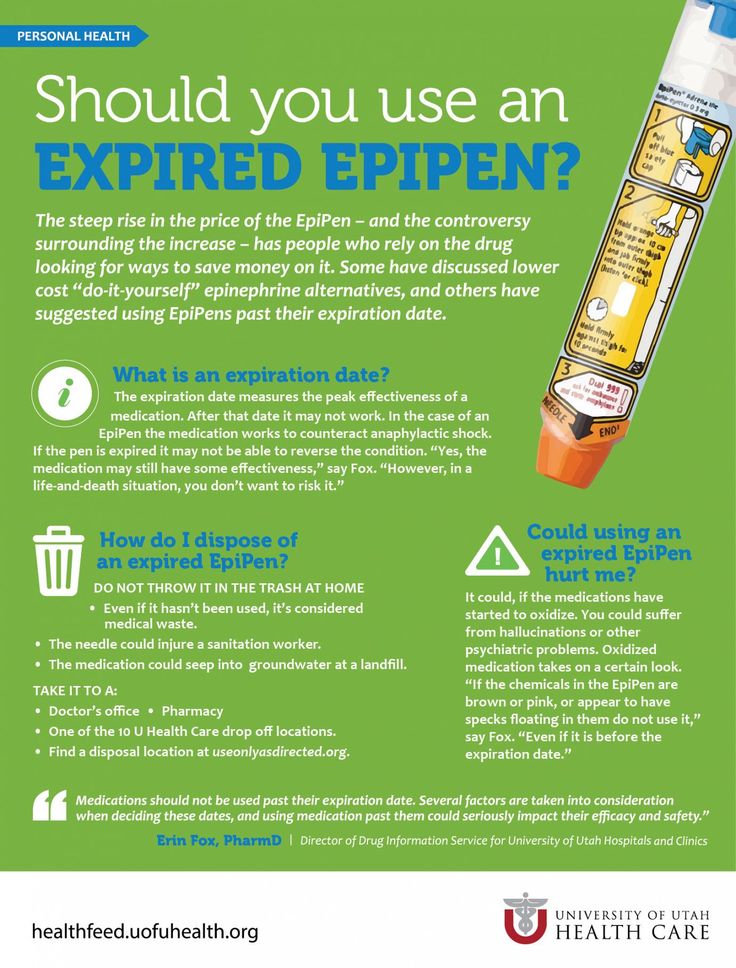
Epinephrine helps the body to keep the airway open so that breathing does not become as difficult, allowing time for emergency medical care to arrive. But many parents worry that one auto-injector might not be enough or that something might go wrong that could require additional auto-injectors. For instance, someone nearby might experience a severe allergic reaction and need to use your child’s auto-injector. Or what if your child’s only auto-injector was unknowingly broken? What if the auto-injector were accidentally put in the fridge or left in the sun? What if the contents were cloudy? Or if it had expired? So many scary possibilities!
So, what is the right number of auto-injectors? The answer to that question depends on a number of factors.
How Many to Carry?On their website, Mylan recommends that patients at risk for allergic emergencies carry two doses of epinephrine. This is because up to 20% of patients who have an allergic emergency requiring epinephrine will require a second dose. At all times the injector should be kept close to room temperature, out of sunlight, and replaced by the expiration date. It’s a good idea to occasionally check the solution in the auto-injector to make sure it hasn’t discolored, which can be a sign of a possible loss of effectiveness.
It’s a good idea to occasionally check the solution in the auto-injector to make sure it hasn’t discolored, which can be a sign of a possible loss of effectiveness.
If a long trip is planned, especially one overseas where similar products may not be readily available in pharmacies; two auto-injectors (or one that contains two doses) may not be enough.
Should you or your child carry more than two auto-injectors? Not necessarily. Additional backups would likely be for peace of mind. A second dose of epinephrine may be needed in an emergency, but more than two doses during an emergency should only be given with medical supervision. Some caregivers choose to carry two auto-injectors from different lots for added precaution.
Multiple LocationsSome patients who use auto-injectors prefer to carry the standard two with them and also keep backup injectors in one or more strategic locations. These might include an extra one or two at work, school, daycare, and/or a relative’s house.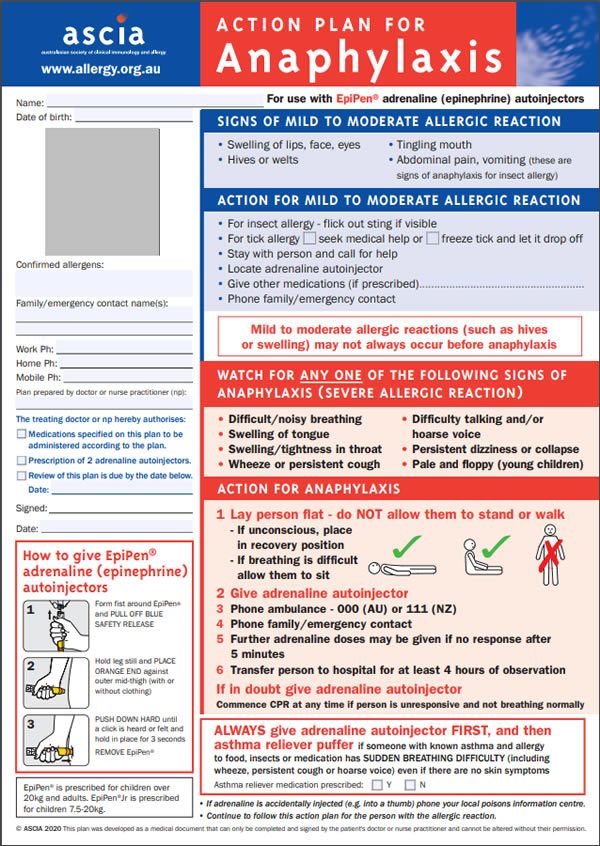 These are great because they can serve as backup in case someone forgets their daily go-everywhere auto-injectors. Just make sure you follow the recommended storage instructions everywhere you keep an auto-injector and check your backups for discoloration and expiration dates. Knowing that you have extra auto-injectors in places like this, in addition to the daily carry-with auto-injectors you have, may bring you more comfort.
These are great because they can serve as backup in case someone forgets their daily go-everywhere auto-injectors. Just make sure you follow the recommended storage instructions everywhere you keep an auto-injector and check your backups for discoloration and expiration dates. Knowing that you have extra auto-injectors in places like this, in addition to the daily carry-with auto-injectors you have, may bring you more comfort.
How about you? How many auto-injectors does your family keep on hand, and where? Please share your thoughts in the comment section of this blog post.
– Rob McCandlish, RDN
Published: 06/28/2011
When To Give An EpiPen To Your Child
Epinephrine is the only way to stop a severe food allergic reaction. Learn when and how to give epinephrine to your food allergic child.
Epinephrine is a vital medicine for children with food allergies. It is the only way to stop a severe allergic reaction. Here’s what your family needs to know about epinephrine, including when and how to give it to your food allergic child.
**If you need to give epinephrine immediately, scroll down to the video and skip to 2:52.
What is epinephrine?
Epinephrine is also known as adrenaline. It is actually a hormone that the body produces naturally, but it can also be used as a medicine.
Epinephrine is used as a medicine for people with food allergies, to stop severe allergic reactions. In fact, it is the only medicine that can stop severe allergic reactions, including life-threatening anaphylaxis.
For people with food allergies, epinephrine comes in an auto-injector, designed to be injected into a person’s thigh in case of an allergy emergency. Common brands of auto-injector include the EpiPen, the Auvi-Q, and the Adenaclick.
When the epinephrine is injected, it causes the blood vessels to narrow, blood pressure to raise if it has dropped, and breathing to improve. It also helps stop widespread hives and serious swelling anywhere on the body. These effects act quickly to help reverse the symptoms of a severe allergic reaction. Epinephrine is life-saving!
Epinephrine is life-saving!
Epinephrine vs. antihistamines
Antihistamines like Benadryl and Zyrtec cannot stop anaphylaxis. Only epinephrine can stop anaphylaxis (and stop any severe allergic reaction). So, never use any other medicine in place of epinephrine.
The American College of Allergy, Asthma, and Immunology (ACAAI) reports that antihistamines like Benadryl and Zyrtec “are not adequate substitutes” for epinephrine during a severe reaction, “as they do not reverse swelling of the airways or raise low blood pressure.” Only epinephrine is life-saving during a severe allergic reaction.
As food allergy activist The Grateful Foodie explains, trying to treat a severe allergic reaction with antihistamine is like tossing a cup of water on a burning building. It just won't work. Rather, you need the proper treatment --- the epinephrine injection. Epinephrine is like using the firefighters’ hose on a burning building, as it’s the only way to stop the “fire” of the reaction at a crucial time.
When to give epinephrine: For severe allergic reactions
Give your child an EpiPen any time they develop severe symptoms of an allergic reaction. Epinephrine is your child’s first line of defense when such a reaction occurs, because it is the only way to stop the reaction.
Severe symptoms of a food allergy reaction may appear seconds to minutes after your child eats a food they are allergic to, and almost always within two hours.
Severe allergic reaction symptoms may include:Skin symptoms:
- Hives that spread to many areas of the body
- Pale appearance
Throat and tongue symptoms:
- Swelling of the throat
- Tightness of the throat
- Swelling of the tongue
- Difficulty swallowing
- Change in voice or cry (e.g. a hoarse-sounding or squeaky voice)
- Slurred speech
- Difficulty vocalizing
Respiratory symptoms:
- Difficulty breathing
- Noisy breathing
- Shortness of breath
- Persistent, significant coughing
- Wheezing
Digestive symptoms:
- Chest pain
- Diarrhea
- Repeated vomiting
Cardiovascular symptoms:
- Drop in blood pressure
- Rapid heartbeat
- Dizziness
- Fainting/collapse
- Loss of consciousness
Other symptoms:
- Sense of impending doom (feeling like something very bad is about to happen)
- Feeling floppy (only in babies and younger children)
Give an EpiPen for anaphylaxis
When the symptoms of a food allergy reaction are severe, and involve more than one organ system, this is known as anaphylaxis.
Anaphylaxis is a life-threatening allergic reaction that requires prompt emergency attention.
Inject epinephrine immediately. Then, call 911.
Remember: severe symptoms that affect at least two organ systems = anaphylaxis. If you think your child has anaphylaxis (even if you have some doubts), inject epinephrine right away!
Let the emergency operator know that your child is experiencing anaphylaxis, and ask for an ambulance with epinephrine inside.
Stay with your child until the ambulance arrives, to make sure their symptoms don’t get worse. Keep them lying on their back if possible (or lying on their side if they’ve fainted or are vomiting.)
If your child’s anaphylaxis gets worse or doesn’t improve within 5 minutes of the first EpiPen, give your child a second EpiPen injection from a different EpiPen.
Have two or more EpiPens ready at all times, in case your child would ever need a second dose in an emergency. This applies at home, at school, and anywhere your child goes outside the home, in case of a food allergy emergency.
This applies at home, at school, and anywhere your child goes outside the home, in case of a food allergy emergency.
Anaphylaxis could also potentially return after 4-24 hours, even after you’ve given your child epinephrine. This returning severe reaction is called a biphasic reaction. If this happens, your child will need a second dose of epinephrine.
A biphasic reaction is another reason why it’s vital to have at least two Epi-pens ready for your child at all times.
Remember: Always carry two [or more] auto-injectors!
Give an EpiPen for other severe allergic reactions
But what if your child develops only one severe symptom of an allergic reaction, or severe symptoms in only one organ system?
In this case, you should still inject the EpiPen, because epinephrine is the only way to stop the severe symptoms of an allergic reaction. There’s a risk that other severe symptoms could develop (meaning your child will have anaphylaxis), and epinephrine will help reverse this process when your child needs it most.
Give an EpiPen for any severe food allergy reaction symptoms.
Keep monitoring your child’s symptoms. If they worsen or don’t improve 5 minutes after the first EpiPen, inject a second EpiPen.
If your child’s symptoms develop into anaphylaxis, call 911 right away!
EpiPens Are Safe
An epinephrine auto-injector is always safe to give your child if they’re having a severe allergic reaction, because it contains the exact dose of the medicine your child needs.
Even if you think your child "doesn't need" the EpiPen at this time, it still won't do any harm to inject. The benefits of injecting always outweigh potential risks. EpiPens save lives!
Follow this rule: If your child shows any severe allergic reaction symptoms, use the Epi-Pen immediately! Remember “Epi first, Epi fast!”
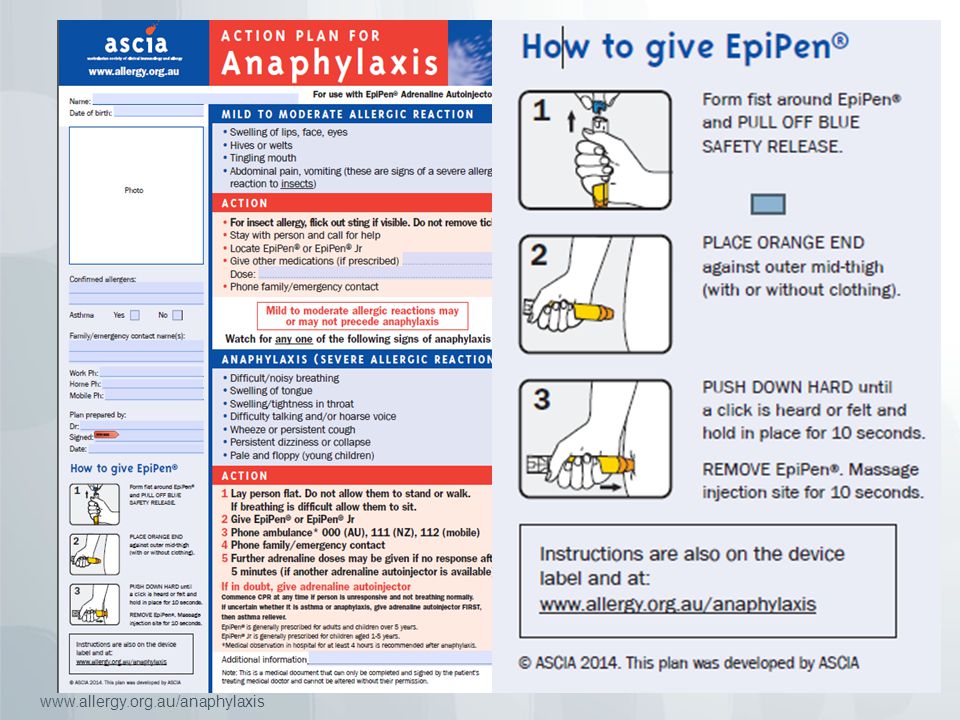
How to use an EpiPen
If you need a visual on how to use an EpiPen, watch this video from Nationwide Children’s Hospital.
If it is an emergency, and you need to give epinephrine immediately, skip to 2:52 for instructions.
Otherwise, here are written instructions for how to give epinephrine to babies and older children:
Giving epinephrine to a baby (under 2 years old):
1. Lay your child flat in your arms.
- Do not hold them upright. Do not let them stand or walk.
- If they are having difficulty breathing, sit them up.
- If they are vomiting, or have fainted, lay them on their side.
2. Pop the safety cap off of the EpiPen. Then, make a fist as you hold the EpiPen.
- Don’t place your thumb on either end!
- You can inject the Epi-pen through clothing --- no need to remove any of your child’s clothes before you continue.
3. Hold your child and their leg still.
4. Locate the biggest muscle in the outer thigh. This is the best place to inject an Epi-pen.
- This is about halfway between the hip and knee, on the side of the leg that faces out.
5. Push the needle end of the EpiPen down on the middle of baby’s outer thigh, so the needle goes into the thigh muscle. Listen for the click.
6. Hold the Epi-pen down on their thigh for 10 seconds, then release.
- Some other epinephrine brands require you to hold the auto-injector down on the thigh for different amounts of time. Follow the exact instructions that came with the auto-injector.
7. Massage your child’s thigh (where you injected the EpiPen) for 10 seconds.
8. Write down the exact time you used the Epi-pen.
Giving epinephrine to a child (2 years old or older):
1. Have your child sit or lie down on their back. Make sure they will stay still during the injection process.
Make sure they will stay still during the injection process.
- You can also have a toddler or younger child sit in your lap, if that’s easier for holding them still.
- If your child is vomiting, or has fainted, lay them on their side.
2. Pop the safety cap off of the EpiPen. Then, make a fist as you hold the EpiPen.
- Don’t place your thumb on either end!
- You can inject the Epi-pen through clothing --- no need to remove any of your child’s clothes before you continue.
3. Hold your child’s leg still.
4. Locate the biggest muscle in the outer thigh. This is the best place to inject an Epi-pen.
- This is about halfway between the hip and knee, on the side of the leg that faces out.
5. Push the needle end of the EpiPen down on the middle of your child’s outer thigh, so the needle goes into the thigh muscle. Listen for the click.
6. Hold the Epi-pen down on their thigh for 10 seconds, then release.
Hold the Epi-pen down on their thigh for 10 seconds, then release.
- Some other epinephrine brands require you to hold the auto-injector down on the thigh for different amounts of time. Follow the exact instructions that came with the auto-injector.
7. Massage your child’s thigh (where you injected the EpiPen) for 10 seconds.
8. Write down the exact time you used the Epi-pen.
Keep in mind that each auto-injector brand may have slightly different instructions for injecting epinephrine. Make sure your family, your child’s teachers, and anyone who cares for your child outside the home knows how to use the auto-injector, following the exact instructions included with it.
You can also practice the injection process with a training Epi-pen. A training EpiPen doesn’t contain epinephrine and is only for practice, so you can get familiar with how to use the EpiPen before you might need it for an emergency. The more you practice, the more ready you’ll be to immediately inject epinephrine if a severe reaction occurs.
As with all aspects of food allergy management, ask your doctor if you have any questions about using epinephrine. They’re here to help protect your child!
--------------------------------
All health-related content on this website is for informational purposes only and does not create a doctor-patient relationship. Always seek the advice of your own pediatrician in connection with any questions regarding your baby’s health.
These statements have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease.
How much water should a child drink and what water should a child be given?
Child's health is one of the main concerns of parents. Did you know that water plays a key role in the formation of the child's body and strengthening immunity? In this article, we will tell you how much life-giving liquid per day is recommended for children of different ages to drink and why this is important.
Science has long proven the great importance of drinking the required amount of water per day. And this is not surprising. So, the body of an adult is 60-75% water, and a child is 80-9% water.0%. Water is easily absorbed by the body and has a strong influence on all processes occurring in it. Its lack leads to a deterioration in well-being, a decrease in immunity, and even weight gain. Often, the development of certain diseases is just a signal that our body does not have enough water! This liquid is especially important for children's health. And the sooner you help your child form the habit of drinking water regularly, the easier it will be for him to maintain a healthy lifestyle in adulthood.
As we have already said, water has a beneficial effect on health and is involved in vital processes. Regular consumption of a sufficient amount of water improves metabolism, maintains normal pressure and body temperature, reduces the risk of allergic reactions, and even has a positive effect on mood. Dehydration leads to rapid fatigue, fatigue, and the development of a number of diseases. Especially dangerous is the lack of water at elevated body temperature and on hot days.
Dehydration leads to rapid fatigue, fatigue, and the development of a number of diseases. Especially dangerous is the lack of water at elevated body temperature and on hot days.
Note!
The importance of keeping in drinking water the optimal ratio of biologically necessary macroelements (calcium, magnesium, phosphorus) and some microelements (selenium, potassium, zinc, iodine, fluorine) is recognized at the state level. Physiologically high-grade water plays a particularly important role in the diet of children, pregnant women, and the elderly [1] .
Here is just a small list of changes in the body, which leads to lack of water:
- infections and allergic reactions;
- dry skin;
- kidney stones;
- digestive and metabolic problems;
- pain in joints and back;
- problems with teeth and gums.
In short, water is a natural component of our body. For children, the correct regimen and certain volumes of consumption of this fluid are especially important, since it is in childhood that all body systems are formed. And the sooner the child gets used to the regular use of water, the less often you will visit the doctor with him.
And the sooner the child gets used to the regular use of water, the less often you will visit the doctor with him.
What kind of water to give your baby
What kind of water you give your baby will affect his health and well-being. Naturally, ordinary untreated tap water is out of the question, even if it is boiled. Water from wells or a pump room, as well as bottled water for adults, will not work either. The thing is that special regulatory requirements are imposed on children's drinking water and water for preparing baby food, which are contained in SanPiN 2.1.4.1116-02 (as amended on June 28, 2010).
Children's water:
- must have a balanced mineral composition. However, the amount of salts and their concentration in children's water, according to the norms, is much lower than in water for adults;
- must be free of preservatives, including carbon dioxide and silver;
- if we are talking about bottled water, then the label must contain information that it is “water for baby food” and “water of the highest category”, as well as information that the product has been registered with Rospotrebnadzor.
In addition, indicators of children's water must comply with specific standard values (see Table 1).
Table 1. normative values of children's water indicators
| indicator | |
|---|---|
| 9000 mg/l | |
| iodide-ions | 0.04-0.06 mg/l |
| fluoride ions | 0.6–1 mg/l | potassium | 2–20 mg/l |
| calcium | |
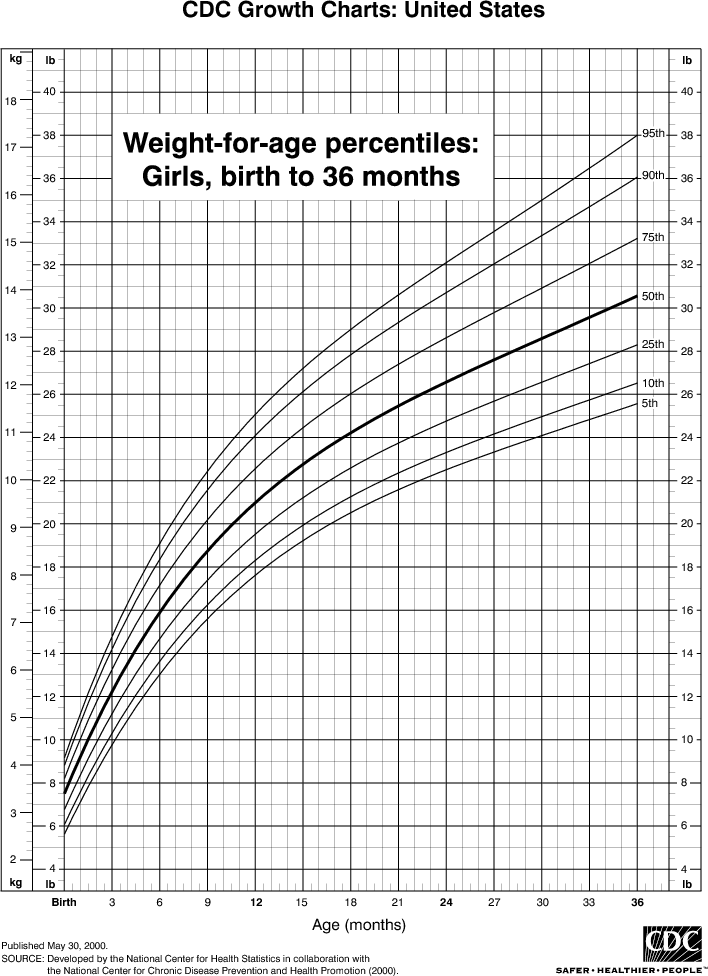
| 9000 900,000,000,000,000,10,30,30,30,30,30,30,30,007 /l Important! Not every bottled water has the right to be called children's water. Perhaps it is precisely because of the high regulatory requirements that manufacturers are afraid to put the cherished words “for baby food” on the labels, thereby relieving themselves of responsibility. According to research by the non-profit organization Roskontrol conducted in 2016, out of 11 samples of bottled water from popular brands, which is positioned by manufacturers as children's, only three were tested: this is only 27% of the total number of tested samples. Important! Heavy metals, which, unfortunately, can be found in many foods, tend to accumulate in the body. Accordingly, the norms are developed taking into account the total risk, which may have a delayed effect. Although a lot of time has passed since the testing by Roskontrol specialists, we were unable to find information on how exactly these shortcomings were corrected by manufacturers and whether they were corrected at all. In connection with such complaints about the quality of children's bottled water, many experts recommend giving children water purified in household filters intended for children, without the use of cartridges containing silver ions, which can disrupt the child's intestinal microflora and lead to the development of dysbiosis. Norm of water consumption for a childHow much water does a child need to drink? The consumption rate will depend on age, weight, mobility, physical condition and even weather conditions. From birth to one year old Babies up to four to six months old, as a rule, get all the nutrients, including water, from their mother's milk. During this period, doctors do not recommend drinking water for babies. First of all, because it is at this time that the intestinal microflora is formed and any intervention can affect the process. Moreover, water fills the stomach and creates a false feeling of fullness - because of this, the baby may not eat up. The composition of mother's milk is perfectly adjusted to the needs of the child. However, doctors allow giving babies from three months a little water on a spoon - but only in hot weather, when the child sweats or when his mouth dries up. In no case is it necessary to force, it is important to offer: if the baby wants, he will drink. This should be done between feedings. Water can also be given when the child has the following problems:
But this should also be done carefully, without persistence. But if the child is formula-fed or mixed-fed, then water has to be used for formula preparation and additionally given between feedings from the first day. But remember, the baby can drink no more than 100-200 ml per day. In general, babies under one year old need 50 ml of water per kilogram of body weight, but remember that approximately 75% of their water comes from milk and food. Therefore, in order to calculate how much of this life-giving fluid is needed to maintain water balance, it follows from the daily requirement indicator (50 ml, multiplied by the weight of the child) subtract the amount of water received with food (the volume of milk drunk in ml, multiplied by 0.75). One to three years old When solid foods are introduced into the baby's diet, the need for water increases. At the same time, children begin to actively move, so the intensity of fluid loss increases. You can calculate the daily water requirement in the same way: a child needs 50 ml of water per kilogram of weight. In this case, we are talking about pure non-carbonated water: juice, compote, tea and other similar drinks are not taken into account. Here are some signs that a child is not getting enough water:
Three to seven years The older the child, the more water he drinks. By school age, this volume will already reach 1.2–1.7 liters of water per day. At the same time, from the age of four, the nervous and skeletal system begins to actively form in the baby. Therefore, it is important that the water contains the required amount of fluorine and magnesium During this period it is important to teach the child to drink regularly. Care should be taken to ensure that water is always available. You can take handy bottles with you for walks. Important! For children with heart disease, kidney disease, diabetes mellitus, the drinking regimen must be prescribed by a doctor. Seven years and older At this age, the norm of water consumption is 1.7–2.5 liters of water per day. When calculating the individual value, it is worth considering the energy of your child. Prednisolone - how to inject
The child had Quincke's edema many years ago. Thank God the ambulance was on time. but they told me to carry a box with an ampoule of prednisolone everywhere with me on trips. In fact, for rapid angioedema, not only prednisone is needed, but also an injection of epinephrine, which will help the heart. Epinephrine is considered a first aid, and prednisolone is an auxiliary decongestant. We have epinephrine in injections Epi Pan or Ovi-Kyu The doctor told us to just inject in the ass, the whole ampoule, there seems to be one ml. And you need to buy European production (then there was still Indian, it seems) there was no such thing, an ambulance injects prednisolone and suprastin prednisolone is calculated strictly by weight. look at the instructions for the drug. In order to quickly relieve an allergic reaction such as anaphylactic shock and Quincke's edema, it is really necessary to use EpiPan. Look in your pharmacies - usually it has a shelf life of a year, you can prick with such a pen even through clothes and it is very easy to do. Yes, Epi Pen is not registered in Russia, and epinephrine in syringes must be stored in the refrigerator, unlike Epi Pen, i.e. you can't take it with you. During anaphylactic shock with edema, my daughter had a very strong heartbeat, after adrenaline, her pulse and respiration improved, and the trembling disappeared. Only then she was injected with prednisolone and an antihistamine. Our pediatrician told us after swelling that we need to have prednisolone in ampoules at home. We also bought syringes. And the antihistamine is not needed, she said that it helps very slowly. There is adrenaline that is stored without cold Why prednisolone and not dexamethasone? Vanya's edema was removed with dex, and then they "insured" with prednisal, it seemed to me that it works faster? +1 in intensive care, all the adrenaline is not in the refrigerator. This is one group of drugs for the same. Well, great. The fact that in Russia adrenaline, which must be stored in the refrigerator, I read on the Rus Med Server forum. Dexamethasone is 10 times stronger than prednisolone and 40-50 times stronger than hydrocortisone. But here it is believed that prednisolone is the drug of choice for children, dexamethasone is for adults who do not help prednisolone. But in general, in anaphylactic shock, the effectiveness of glucocorticosteroids is in doubt (I can give links in English) and the shock is relieved by adrenaline and h2 antihistamines, bronchodilators. And the hormone is injected just in case, to the heap. BUT since epinephrine is not even registered in Russia, then nothing can be done anyway. Unless there really are epinephrine syringes that can be stored at normal temperature. Epinephrine is adrenaline Of course it is adrenaline. Only in autoinjectors does it pass under the name epinephrine. Several doctors have already told me that anaphylactic shock = a person died if it did not happen within the walls of a hospital with intensive care, I don’t know, it happened to me just in the hospital, I don’t know that they injected and dripped, but I lay in intensive care probably for a week You puzzled me, I always inject dex for children - Vanka and Svyatoslav, and the ambulance also injects him, then they already drip prednisolone, Svyatoslav always for 10 days, Vanka was simply poured into/in without droppers. Before, I used to take Relanium with me, but as I understand it, this is not the same thing at all, Svyatoslav, I heard about adrenaline many times, but always with the caveat - do not inject yourself! but it would be nice to have with you, call an ambulance and what would they prick. In Russian, read Komarovsky what to do in case of shock: http://spravka.komarovskiy.net/lechenie-anafilakticheskix-reakcij.html He always writes that if every Russian first aid kit had adrenaline many lives would have been saved. After all, adrenaline is not only for anaphylactic shocks, but all kinds of accidents, many critical conditions. We were prescribed Epipen (adrenaline). Always with you. Prednisolone tablets (when hives are severe or slight swelling) and Zyrtec (for mild cases). Sadly, EpiPens have saved more than one life. Nightmare Our kids with severe allergies always have these EpiPens with them and know how to inject themselves with it. Adrenaline injects during cardiac arrest (not shock is given, as shown in all series, namely adrenaline), but for this you need to know what kind of heart rate a person has. Because if it is ventricular tachycardia or atrial febrile (looks exactly like cardiac arrest), then you need an electric shock, and with adrenaline you will immediately send a person to the next world. We were also scolded for not getting injected right away, even though we had epipen with us. I was expecting some swelling or difficulty breathing, but there were hives on my stomach and vomiting. We went to the hospital and literally in the hospital, literally in minutes, a very strong edema, tachycardia and the inability to breathe and swallow began. those. another 5 minutes of delay and it would have happened on the road, I could not have brought the child. It's good that we did it, a lesson for us. It seems that in America they are now going to allow children to inject adrenaline without a prescription if they suspect shock. This happened after the boy was bitten by a wasp at the game, the nurse was there and she had a lot of epipen from other people's children, but there was no epipen on the boy and there was no permission from the doctor to inject him with epipen. They couldn't save, but they could. Here, it seems, they will be allowed to inject adrenaline even if there is no prescription for it, school nurses will have extra injections. I think that in a situation with the risks of anaphylactic shock, it is not just that all children are given epipenes and from the age of 7 they are taught to inject themselves with it. Those. The benefits probably outweigh the risks in this case. But I don't know about other situations, although in case of accidents I know people sometimes use epipenes while waiting for an ambulance. BUT, naevrnoe, situations for the use of adrenaline should be described. There should not be any descriptions of other situations where adrenaline is used, because professionals connect a monitor to the victim and watch the heart rate - it depends on what to do in a particular situation. It is IMPOSSIBLE to determine by eye adrenaline, electric shock, cardioversion (I don’t know how in Russian), atropine or an artificial rhythm, for this you need to check your heart rate. I don't know what you're arguing about. we are talking about anaphylactic shock in the absence of professionals with monitors. In the West, an injection of adrenaline is given to everyone who has the risk of anaphylactic shock, and even 2 syringes at once, because. one dose may not be enough before the professionals arrive with monitors. In other situations, these are not my complaints about the fact that there should be adrenaline in every first-aid kit, but Dr. Komarovsky. Many cases have been described of people dying of shock in the dentist's office. those did not have adrenaline, for example, and just in life there are hikes, long trips, summer cottages, villages, quick allergic reactions to bites or food. And there is a description of the symptoms that require the use of adrenaline BEFORE the professionals arrive. Apparently, this is done not to harm people, but to benefit. Thank God, they don't scare me with details about different rhythms, because, apparently, the benefits exceed the risks. I'm arguing about this: "Adrenaline is not only for anaphylactic shocks, but all kinds of accidents, many critical conditions." I wrote where else adrenaline is used and why it cannot be used just by eye. Thank you I repeat, as I said above, this is Komarovsky's action "adrenaline is in every car first-aid kit" If you really really need it, you can order from Ukraine or Europe. http://one-apteka.com.ua/allmeds/heart/kupit-epipen-0.3mg.html http://s-pharma.net/epipen.html We always have someone driving, I just need to understand if I need it and if so, how to use it :?) We give out to everyone who has a tendency to edema in the face and throat. |
 To do this, the label must necessarily indicate - "for baby food." According to the experts of the quality monitoring system "Roskontrol" [2] , the phrases "for children" or "from the first days of life" often found on bottles of water are just a marketing ploy that does not impose on the manufacturer the obligation to follow the requirements of the legislation for the mineral composition and security. And, of course, the presence of children's drawings is also not a confirmation that the contents of the bottle meet the quality standards for children's drinking water.
To do this, the label must necessarily indicate - "for baby food." According to the experts of the quality monitoring system "Roskontrol" [2] , the phrases "for children" or "from the first days of life" often found on bottles of water are just a marketing ploy that does not impose on the manufacturer the obligation to follow the requirements of the legislation for the mineral composition and security. And, of course, the presence of children's drawings is also not a confirmation that the contents of the bottle meet the quality standards for children's drinking water.  In the rest, an unbalanced salt composition was revealed, as well as a significant excess in the number of microorganisms that actively multiply at a temperature of 37°C, the content of chloroform, and even traces of mercury were found, although in small quantities [3] .
In the rest, an unbalanced salt composition was revealed, as well as a significant excess in the number of microorganisms that actively multiply at a temperature of 37°C, the content of chloroform, and even traces of mercury were found, although in small quantities [3] . 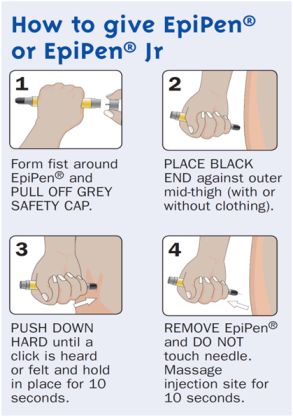 Moreover, the use of household filters allows not only to purify water from microorganisms, excess salts, but also to enrich it with microelements necessary for the child, such as fluorine and magnesium.
Moreover, the use of household filters allows not only to purify water from microorganisms, excess salts, but also to enrich it with microelements necessary for the child, such as fluorine and magnesium.  And if the baby is hot, he is more often applied to the breast and as a result receives a lot of foremilk, which is 88-90% water. It is important that the mother herself consumes the required amount of water and does not feel thirsty!
And if the baby is hot, he is more often applied to the breast and as a result receives a lot of foremilk, which is 88-90% water. It is important that the mother herself consumes the required amount of water and does not feel thirsty! 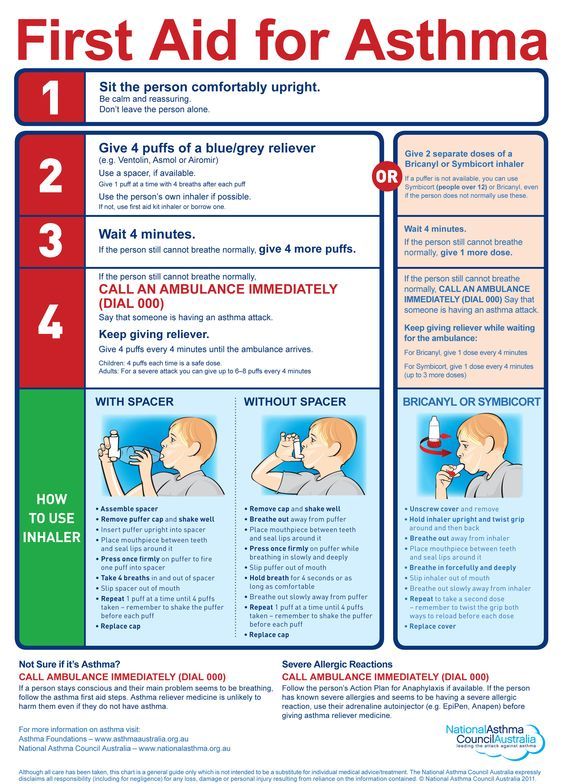

 If he plays sports and is generally physically active, then the amount of fluid you drink should be increased. Also keep in mind that the composition of water for children aged 12 and over should be as close as possible to the composition of water for adults. And remember that during periods of illness or in hot weather, the need for fluid increases.
If he plays sports and is generally physically active, then the amount of fluid you drink should be increased. Also keep in mind that the composition of water for children aged 12 and over should be as close as possible to the composition of water for adults. And remember that during periods of illness or in hot weather, the need for fluid increases.  I really want to play it safe and play it safe, because both on the train and on the plane, maybe even someone can be helped in an acute situation, if that!
I really want to play it safe and play it safe, because both on the train and on the plane, maybe even someone can be helped in an acute situation, if that! 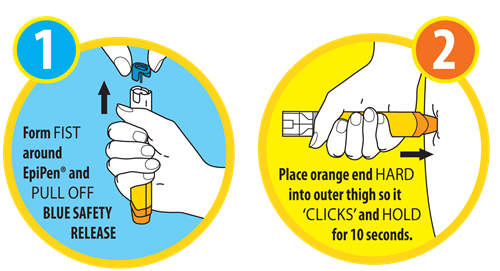

 In Russia, not a single auto-injector with adrenaline is registered, respectively, nothing with the name epinephrine is registered. In order not to list all brands of autoinjectors, for simplicity, I use the name epinephrine. In Russia, there are kind of disposable syringes that are already filled with adrenaline, but they write that they need to be stored in the refrigerator, they have no adult-child dosage difference, and they are not auto-injectors.
In Russia, not a single auto-injector with adrenaline is registered, respectively, nothing with the name epinephrine is registered. In order not to list all brands of autoinjectors, for simplicity, I use the name epinephrine. In Russia, there are kind of disposable syringes that are already filled with adrenaline, but they write that they need to be stored in the refrigerator, they have no adult-child dosage difference, and they are not auto-injectors. 
 With difficulty breathing, it is generally better to inject immediately.
With difficulty breathing, it is generally better to inject immediately. 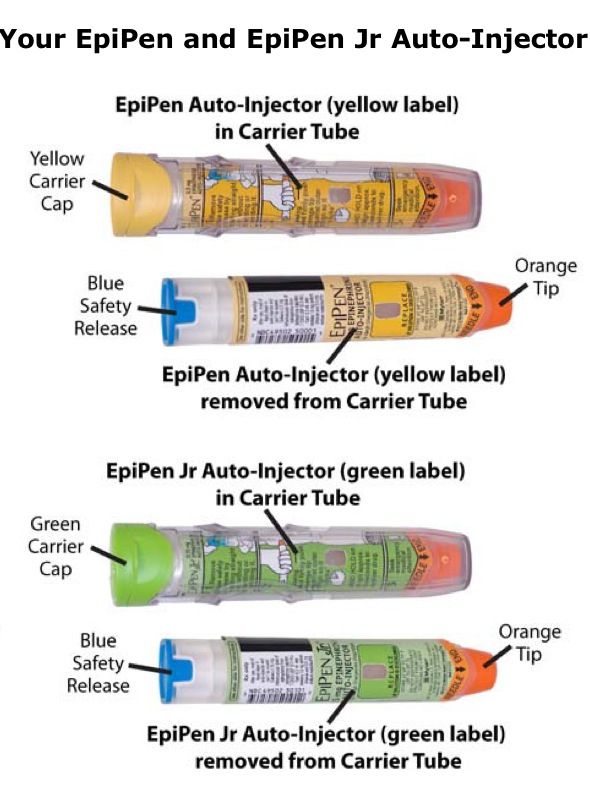
 They say that the consequences of the injection are not so many, but it can save a life.
They say that the consequences of the injection are not so many, but it can save a life.