Formula allergies in newborns
Signs of a baby formula allergy
If your baby frequently vomits or has diarrhea after drinking formula, they may be allergic to the cow's milk protein found in most formulas.
Formula allergies are typically caused by a milk allergy. A milk allergy is an atypical immune response in which the body reacts to the protein in milk as though it's a foreign invader that needs to be fought off.
Milk allergy is the most common food allergy in children. In fact, 2 to 3 percent of kids under age 3 show symptoms of an allergy. Just because your baby has signs of a milk allergy, though, doesn't necessarily mean they're allergic to milk – it could be an intolerance or sensitivity, which often causes the same gastrointestinal issues.
If you think your baby might be allergic to the formula you're giving them, bring it up with your pediatrician. They can help pinpoint what's causing your baby's discomfort.
A milk allergy or intolerance can be hard to manage, but the good news is most babies outgrow it by about 18 months to 2 years old.
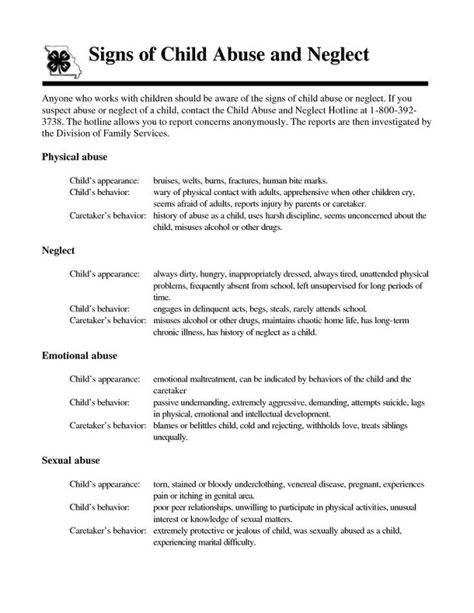
Signs of an allergic reaction to formula
It's not surprising that some of the most common signs of an allergic reaction to formula are gastrointestinal, including:
- Vomiting
- Diarrhea
- Blood or mucus in the stool
- Unusually hard or excessively loose, watery, and foul-smelling poop
- Abdominal pain
Frequent spit up and excessive gassiness may also be signs of a milk allergy.
Not all signs of a formula allergy are gastrointestinal, though. Other signs of an allergy include:
- Itchy, watery, or swollen eyes
- Chronic nasal stuffiness
- Runny nose
- Cough
Your child may also develop itchy raised bumps on the skin known as hives. This is a type of skin rash that often occurs as a result of an allergic reaction. Hives can appear anywhere on the body and may look like tiny spots, blotches or large bumps.
Another common rash that may appear with a formula allergy is known as eczema (atopic dermatitis) and can cause red, itchy or dry skin. Eczema tends to show up on the cheeks and scalp in babies but can appear anywhere on the body.
Eczema tends to show up on the cheeks and scalp in babies but can appear anywhere on the body.
If you notice that your baby is continually fussy or crying and has obvious signs of discomfort shortly after you've started feeding, talk to your baby's doctor. Babies with milk allergies can show symptoms anywhere from days to weeks after first drinking cow's milk-based formula.
In some cases, a severe food allergy may cause a life-threatening reaction called anaphylaxis. If your baby has any of the following symptoms, call 911 or go to an emergency room immediately:
- Turning blue
- Wheezing
- Trouble breathing
- Facial swelling (including the lips or tongue)
It can be difficult to tell the difference between a milk allergy and lactose intolerance, since both conditions can cause uncomfortable gastrointestinal symptoms. If you have any concerns at all, talk to your baby's pediatrician. They can help figure out whether your baby has a milk allergy, lactose intolerance, or some other issue.
Lactose intolerance is primarily a digestive issue in which the body doesn't produce enough of the enzyme lactase to properly digest the lactose in milk. Lactose intolerance can cause diarrhea, bloating, and gas in infants, but it's usually not dangerous. It's more common in adults than in children: If your child does have this condition, they likely won't start showing signs until they're at least 3 years old.
What to do if your baby has a formula allergy
First, check with your child's doctor to make sure that something else isn't causing the reaction. Once they rule out other possibilities, they may recommend a hypoallergenic (hydrolyzed) formula or an amino acid-based formula that's processed to avoid allergic reactions.
Your doctor most likely won't recommend a soy formula – soy is also a highly allergenic food, so if your baby is allergic to milk, they may also be allergic to soy. In fact, about 8 to 14 percent of babies with a cow's milk allergy will also have a reaction to soy. Ask your baby's doctor before switching to a soy formula.
Ask your baby's doctor before switching to a soy formula.
Your baby's doctor may also recommend keeping epinephrine auto-injectors on hand for your baby in case they accidentally have a milk product and have a severe reaction to it.
advertisement | page continues below
Milk Allergy in Infants (for Parents)
What Is a Milk Allergy?
When a baby is allergic to milk, it means that his or her immune system, which normally fights infections, overreacts to proteins in cow's milk. Every time the child has milk, the body thinks these proteins are harmful invaders and works hard to fight them. This causes an allergic reaction in which the body releases chemicals like
histamine.
Cow's milk is in most baby formulas. Babies with a milk allergy often show their first symptoms days to weeks after they first get cow milk-based formula. Breastfed infants have a lower risk of having a milk allergy than formula-fed babies.
People of any age can have a milk allergy, but it's more common in young children. Many kids outgrow it, but some don't.
If your baby has a milk allergy, keep two epinephrine auto-injectors on hand in case of a severe reaction (called anaphylaxis). An epinephrine auto-injector is an easy-to-use prescription medicine that comes in a container about the size of a large pen. Your doctor will show you how to use it.
What Are the Signs & Symptoms of a Milk Allergy?
In children who show symptoms shortly after they have milk, an allergic reaction can cause:
- wheezing
- trouble breathing
- coughing
- hoarseness
- throat tightness
- stomach upset
- vomiting
- diarrhea
- itchy, watery, or swollen eyes
- hives
- swelling
- a drop in blood pressure causing lightheadedness or loss of consciousness
The severity of allergic reactions to milk can vary. The same child can react differently with each exposure. This means that even though one reaction was mild, the next could be more severe and even life-threatening.
The same child can react differently with each exposure. This means that even though one reaction was mild, the next could be more severe and even life-threatening.
Children also can have:
- an intolerance to milk in which symptoms — such as loose stools, blood in the stool, refusal to eat, or irritability or colic — appear hours to days later
- lactose intolerance, which is when the body has trouble digesting milk
If you're not sure if your child has an intolerance versus an allergy, talk to your doctor.
If Your Child Has an Allergic Reaction
If your child has symptoms of an allergic reaction, follow the food allergy action plan your doctor gave you.
If your child has symptoms of a serious reaction (like swelling of the mouth or throat or difficulty breathing, or symptoms involving two different parts of the body, like hives with vomiting):
- Give the epinephrine auto-injector right away. Every second counts in an allergic reaction.

- Then, call 911 or take your child to the emergency room. Your child needs to be under medical supervision because, even if the worst seems to have passed, a second wave of serious symptoms can happen.
How Is a Milk Allergy Diagnosed?
If you think your infant is allergic to milk, call your baby's doctor. He or she will ask you questions and talk to you about what's going on. After the doctor examines your baby, some stool tests and blood tests might be ordered. The doctor may refer you to an allergist (a doctor who specializes in treating allergies).
The allergist might do skin testing. In skin testing, the doctor or nurse will place a tiny bit of milk protein on the skin, then make a small scratch on the skin. If your child reacts to the allergen, the skin will swell a little in that area like an insect bite.
If the allergist finds that your baby is at risk for a serious allergic reaction, epinephrine auto-injectors will be prescribed.
Avoiding a Milk Allergy Reaction
If You're Breastfeeding
If your breastfed infant has a milk allergy, talk to the allergist before changing your diet.
If You're Formula Feeding
If you're formula feeding, your doctor may advise you to switch to an extensively hydrolyzed formula or an amino acid-based formula in which the proteins are broken down into particles so that the formula is less likely to trigger an allergic reaction.
You also might see "partially hydrolyzed" formulas, but these aren't truly hypoallergenic and can lead to a significant allergic reaction.
If you're concerned about a milk allergy, it's always best to talk with your child's doctor and work together to choose a formula that's safe for your baby.
Do not try to make your own formula. Commercial formulas are approved by the U.S. Food and Drug Administration (FDA) and created through a very specialized process that cannot be duplicated at home. Other types of milk that might be safe for an older child with a milk allergy are not safe for infants.
Other types of milk that might be safe for an older child with a milk allergy are not safe for infants.
If you have any questions or concerns, talk with your child's doctor.
Allergy in infants treatment, allergy in newborns, allergy in infants, food allergy in infants, allergic rash in infants › Outpost Clinic
(044) 502-22-62
(multi-channel)
093 / 068 / 066 / 502-22-62
License of the Ministry of Health of Ukraine
(093) 502-22-62
(068) 502-22-62
- en
- en
- UK
What is the danger of developing allergies in an infant
One of the most common causes of allergy in infants is formula milk. Despite the fact that manufacturers try to adapt milk formulas as much as possible, they still cannot be fully adapted to the child.
Despite the fact that manufacturers try to adapt milk formulas as much as possible, they still cannot be fully adapted to the child.
If the parents or relatives of the baby have allergies, asthma, allergic rhinitis, urticaria or atopic dermatitis, then through the genes they can "reward" him with a predisposition to allergies. The risk of developing an allergy in a baby to milk formula depends on the degree of predisposition of the child, the more allergies in the family, the higher the likelihood of developing an allergy:
- 10-20% - family without allergies;
- 20-40% - 1 parent is allergic;
- 50-80% - both parents suffer from allergic diseases.
For children with a predisposition to allergies, it is very important not to get cow's milk, which is very high in casein (mother's milk is much less). Therefore, attention should be paid to the fact that children prone to allergies are not supplemented in maternity hospitals with conventional mixtures, as this leads to allergization of the child from the first days, while there is a breakdown in adaptation, and further such children are more likely to develop allergies.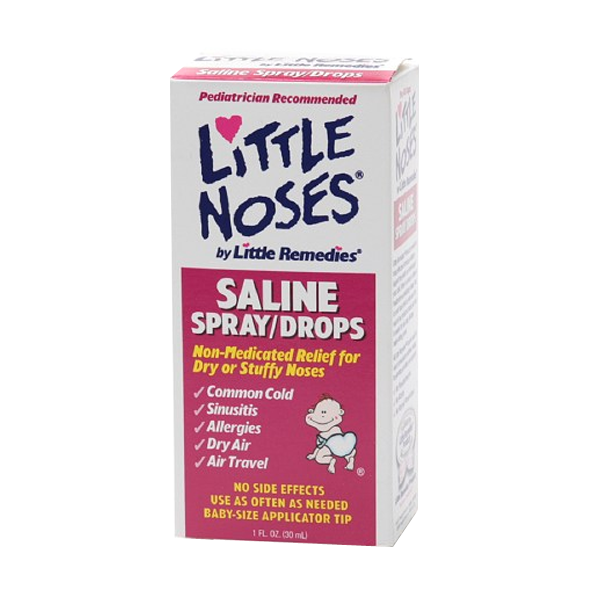
Manifestations of allergy in infants to milk formulas
Signs of allergy to milk protein can manifest themselves both in the immediate type (IgE-dependent, the reaction manifests itself after the use of the milk formula during the first 30 min-2 hours), and the delayed type (IgG4 dependent) - does not appear immediately, but within one or two days. Allergy in infants to formula milk is manifested by:
- rash on the skin in the form of various dermatitis, urticaria, rash around the mouth;
- inflammation on the cheeks, buttocks, legs, back, vulva in the form of redness, papules, accompanied by itching;
- gastrointestinal manifestations in the form of vomiting, hiccups, regurgitation, stool disorders (constipation, diarrhea, bloating, intestinal colic).
What components of milk formula cause allergies in a child? 80% of milk formulas are made on the basis of cow's milk, because cow's milk in its composition is the most identical to human milk and contains the necessary proteins and trace elements for the growth and development of the child. 20% of mixtures are made on the basis of soy or goat milk.
20% of mixtures are made on the basis of soy or goat milk.
Food allergies in infants. Allergy of children under one year to milk
Cow's milk contains proteins such as casein, lactalbumin and lactoglobulin. All three proteins can cause allergies in a child, either individually or all at the same time. Lactalbumin and lactoglobulin are thermolabile, which means that they are destroyed by boiling and can no longer cause allergies in a child. Casein, on the other hand, is thermostable (that is, it does not break down when boiled and can cause an allergic reaction). Unfortunately, most children are allergic to casein.
Diagnosis of allergy in infants you can check for allergies in infants to all the main protein components of milk. This is possible only with the help of molecular allergy diagnostics, which determines the allergy not to the entire product, but to its individual components.
Allergic rash in infants. Allergy to cereals
Sometimes milk formulas may contain various cereals (buckwheat, oats, rice), then the child may be allergic to these cereals. Such mixtures are usually intended for older children - after 6 months. Accordingly, tests are made for the respective components of the cereals. You can just separately make IgE for wheat, rye and others. But it is best to do molecular component diagnostics → on the main (major) proteins of cereals (rPhl p1, rPhl p5b), which are included in buckwheat, wheat, rye, fescue and many other cereals, as well as minor (rPhl p7, rPhl p12) proteins, due to which cross-reactions with other foods and plants often occur.
Such mixtures are usually intended for older children - after 6 months. Accordingly, tests are made for the respective components of the cereals. You can just separately make IgE for wheat, rye and others. But it is best to do molecular component diagnostics → on the main (major) proteins of cereals (rPhl p1, rPhl p5b), which are included in buckwheat, wheat, rye, fescue and many other cereals, as well as minor (rPhl p7, rPhl p12) proteins, due to which cross-reactions with other foods and plants often occur.
What are hypoallergenic formulas and are they prescribed for allergies in infants? If initially we know that the parents are allergic and the likelihood of developing allergies in the child is high, then it is recommended to immediately start feeding with hypoallergenic mixtures, preventing the development of allergies in the child.
Hypoallergenic mixtures are hydrolysates of cow's milk proteins (i.e. the protein is broken down into amino acids). As a rule, there is no allergic reaction to these mixtures. But hydrolysates, due to the split protein, become bitter in taste. Therefore, at the beginning it happens that the child does not want to eat, and although his taste buds are not as developed as in an adult, he still feels a bitter taste, especially since mother's milk is sweet. Therefore, it is necessary to gradually accustom the child to the hydrolyzate, at first, in the first 3-5 days, he may refuse, and then he gets used to it. It is important that parents do not rush to cancel the mixture, as a mixture that cannot be fed to the child.
But hydrolysates, due to the split protein, become bitter in taste. Therefore, at the beginning it happens that the child does not want to eat, and although his taste buds are not as developed as in an adult, he still feels a bitter taste, especially since mother's milk is sweet. Therefore, it is necessary to gradually accustom the child to the hydrolyzate, at first, in the first 3-5 days, he may refuse, and then he gets used to it. It is important that parents do not rush to cancel the mixture, as a mixture that cannot be fed to the child.
Types of hypoallergenic mixtures for allergy in an infant
There are hydrolysates depending on the degree of milk protein hydrolysis: moderate and high hydrolysates. If the baby’s allergy is not severe, then moderate hydrolysates are recommended, since they have small amounts of allergens and thus “train” and “accustom” the baby’s immune system.
Does your child have skin rashes, gastro-intestinal problems?! This is a minimally traumatic tactic for examining infants and older children. Search for the cause of problems, taking into account possible allergies.
Stages:
- Fecal analysis for a coprogram, which looks at the degree of digestion of food, signs of inflammation in the intestine, the presence of pathogenic (iodophilic) flora, etc.
- Ultrasound of the abdominal organs, which allows to detect possible developmental anomalies (atresia, underdevelopment of the bile ducts, deformation of the gallbladder, etc.)
- Blood test to determine the level of total immunoglobulin E and / or Phadiatop Infant. Fadiatop Infant is an allergy screening test that contains all the main foods - milk, eggs, wheat, etc., as well as inhaled allergens. If this test is positive, then component allergy diagnostics is necessary. If negative, then go to step
- Component diagnosis of allergy to casein, lactalbumin, lactoglobulin (if the child consumes only milk formula). If the child is more than 6 months old and he uses various cereals, then component diagnostics for cereals is necessary.
- If allergy tests are negative, tests for lactase deficiency and celiac disease are performed.
Prevention of allergies in newborns and older children
Breastfeeding helps to strengthen the child's immune system. Even though the parents are allergic, it is desirable that the mother breastfeed the child. Through breast milk, the child gets acquainted with all the proteins of the surrounding world and, along with an allergic reaction, an anti-allergic reaction, an adaptive one, is produced in it. Thus, the child quickly adapts and outgrows this increased sensitivity to various substances and proteins of the surrounding world.
how it manifests itself, what it looks like, what to do, how long it takes for a newborn to be allergic to formula
We deal with the signs of intolerance to baby food and answer the question of what to do if the baby has an allergy to infant formula.
Nutrition for babies in the first year of life if breastfeeding is not possible should be prescribed by a pediatrician. He will definitely ask about the presence of allergies in parents and close relatives, ask about how the pregnancy went, did the mother take antibiotics, does the mother have bad habits. These are all risk factors for food allergies in babies.
He will definitely ask about the presence of allergies in parents and close relatives, ask about how the pregnancy went, did the mother take antibiotics, does the mother have bad habits. These are all risk factors for food allergies in babies.
How infants are allergic to formula
The reaction to an allergen manifests itself through different body systems. Here are the symptoms of a food allergy:
- On the skin : redness that starts on the face and spreads throughout the body, small blisters, peeling
- From the digestive system : regurgitation, loose stools, especially green, constipation, bloating, colic
- Respiratory : shortness of breath, cough, wheezing
How long does it take to become allergic to the mixture
How quickly the disease will make itself felt depends on the characteristics of the child's health. In some babies, the first signs of allergies occur immediately after feeding. In others, the allergen will manifest itself only after a few days, when it accumulates in the body. In any case, you should immediately contact a specialist who will diagnose and prescribe adequate treatment.
In others, the allergen will manifest itself only after a few days, when it accumulates in the body. In any case, you should immediately contact a specialist who will diagnose and prescribe adequate treatment.
Allergy to hypoallergenic mixture
Hydrolyzed mixtures are called hypoallergenic - those where the milk protein is split into amino acids and peptides, which are easily absorbed by the body and in most cases do not cause an undesirable reaction. They are prescribed in cases of severe allergies. They are bitter, and babies are reluctant to eat them.
However, an undesirable reaction can also occur on a hypoallergenic mixture. That is why only a pediatrician should recommend the mixture and select treatment in case of an allergy.
Why are babies allergic to formula?
The reasons are different. A doctor and tests will help to deal with them.
The most common of the reasons:
- temporary or congenital lactase deficiency.
 The tests prescribed by the pediatrician will help to establish this reason. And treatment can be a temporary or permanent transition to a lactose-free mixture, such as soy. How to recognize lactase deficiency, read the article of our pediatrician.
The tests prescribed by the pediatrician will help to establish this reason. And treatment can be a temporary or permanent transition to a lactose-free mixture, such as soy. How to recognize lactase deficiency, read the article of our pediatrician. - allergy to animal protein - casein. After passing the analysis, the doctor will recommend replacing the mixture with soy or hydrolyzed. Read more about lactase deficiency and cow protein allergy in our article.
- incorrect transition to artificial feeding or a new mixture. Learn how to change the mixture so as not to harm the baby's body.
- rotavirus infection. This is a temporary, but rather acute condition, during which the child needs special nutrition. Learn more about nutrition during rotavirus.
- excess food. This is the most common cause of allergic dermatitis in artificial babies who cannot regulate the amount of formula they eat. Why this happens, find out from our material.
- formula is not suitable for your baby.
 Children prone to allergies may react to the composition of improved mixtures enriched with vitamins and trace elements. How to understand what exactly caused the allergy? It is necessary to pass tests and follow the advice of a pediatrician to switch to a suitable mixture.
Children prone to allergies may react to the composition of improved mixtures enriched with vitamins and trace elements. How to understand what exactly caused the allergy? It is necessary to pass tests and follow the advice of a pediatrician to switch to a suitable mixture.
What to do
Regardless of whether treatment is required, a reduction in the volume of the mixture eaten or a transition to a new diet, the appointment should be made by a doctor.
Therefore, the first thing to do is to contact a pediatrician who will establish the cause, possibly offer to take tests and prescribe treatment.
Soy mixtures for allergies
Soy infant formula is prescribed for allergies to animal protein - casein. And in the absence of allergies to soy. Therefore, if the doctor has prescribed an analysis for an allergy to animal protein, ask if it is worth immediately taking an analysis for a reaction to soy protein.
Soy nutrition is an absolutely complete replacement for dairy nutrition until the transition to adult food.