How long can a woman produce milk
When does the breast milk of a mother dry-up completely
When does the breast milk of a mother dry-up completelyHome / Blog / WHEN DOES THE BREAST MILK OF A MOTHER DRY UP COMPLETELY?
Amri
28 Feb, 2022
WHEN DOES THE BREAST MILK OF A MOTHER DRY UP COMPLETELY?
There is no maximum age, up to which a mother can produce breast milk. Whenever the pregnancy happens, the lactogen process starts immediately. Usually after the age of 40, there are certain hormonal changes in the body, due to which the production of the breast milk is hampered. So, the ideal child bearing age is from 22-35 years, suggest doctors at AMRI Hospitals in Kolkata.
During this process, if a woman gets pregnant, then the lactogen process starts off from the latter part of pregnancy, and the mother starts to produce breast milk. In the initial 6 months, the breast milk production is the highest. After 1-2 years, the production gradually ceases. Production of milk in the breast is a process that hormone levels influence during and after pregnancy.
A woman’s ability to breastfeed can rely upon many factors. For the most part, breastmilk production depends on loss of milk to provide more (supply and demand). Additionally, it’ll rely upon the Mother’s health, like sufficient calorie intake and emotional well-being, as well as healthy endocrine levels. So long as a lady will tick these boxes and steers clear from lowering her medications, does not have excessive amount of stress and isn’t menopausal, she will definitely be able to continue producing milk. What is more important is that even years after a lady has stopped breastfeeding and lactation has ceased, she will be able to still hand express some milk!
Additionally, it depends on the mother that for how long she usually feeds her baby, as its all demand and produce. The very first thing everyone knows is that nothing will beat the healthy aspects from milk that a baby can get, explain medical practitioners at AMRI Hospitals, one of the best child hospital in Kolkata. The breastmilk therefore cannot be supplemented at least for the first 6 months after the birth.
The very first thing everyone knows is that nothing will beat the healthy aspects from milk that a baby can get, explain medical practitioners at AMRI Hospitals, one of the best child hospital in Kolkata. The breastmilk therefore cannot be supplemented at least for the first 6 months after the birth.
Some mothers feed their babies until 6 months; some do not feed because of various reasons like baby will not latch etc. Therefore low milk production leaves baby hungry, for which they switch to bottle feed etc. After a baby is born, the mothers’ breasts function to provide colostrums, which is the initial milk for the baby. Now whether or not the baby has it, the breasts will contain that milk since like seven months of physiological state.
If baby isn't fed, then the milk production can stop on its own. If the baby is fed regularly, then milk production continues.If the mother decides not to breastfeed her baby, her breasts won't be emptied once they begin producing milk. This may prevent breasts from producing milk, and the breasts can come back to near pre-pregnancy size. As long as the milk is not emptied from the breasts, they will become congested and swell, typically inflicting discomfort and pain on the mother. After some days, the breasts can "give up" making an attempt to supply milk and become smaller and less painful.
As long as the milk is not emptied from the breasts, they will become congested and swell, typically inflicting discomfort and pain on the mother. After some days, the breasts can "give up" making an attempt to supply milk and become smaller and less painful.
After delivery, as long as the milk comes out and the child continues to drink it, the woman will be able to produce milk. Once she stops expressing the milk, the breasts can stop lactating, till pregnancy happens once more.
According to the medical practitioners at AMRI Hospitals, one of the best hospitals in Kolkata, a woman can produce breast milk for twenty, thirty or more years, as long as there is a constant need for it,.
What are the two types of breast milk a woman produces?
There are two types of breast milk: for the initial few days, there is thick yellow coloured milk called the Colostrums, followed by the normal milk.
Colostrums:
The yellowish liquid that women start to secrete during the end of pregnancy after giving birth is nothing but the colostrum.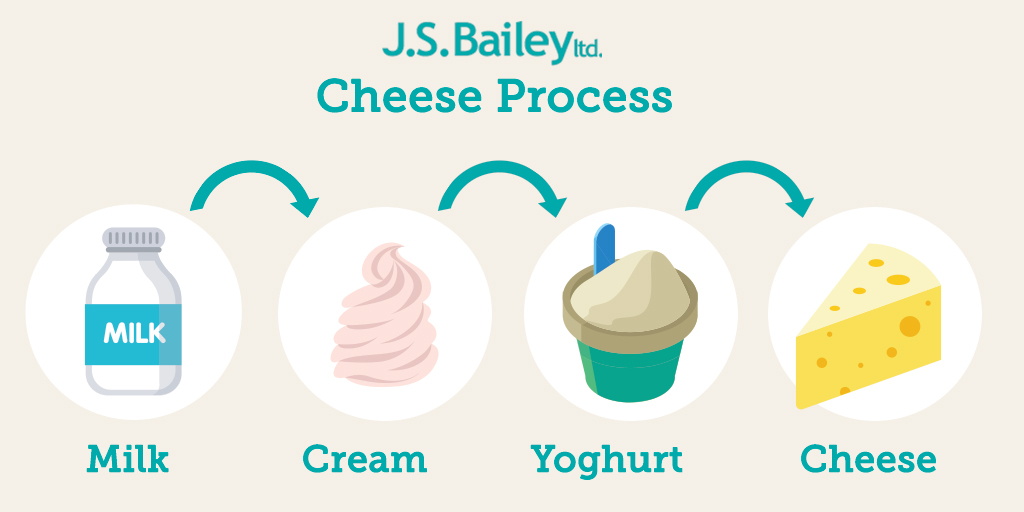 For many reasons, it is an important substance for the first few days of a baby’s life. Colostrum is a yellowish liquid that is secreted by the breast. It has a high content of proteins and minerals. The production of colostrum is carried out when the mammary glands are preparing to generate milk which will serve as the exclusive food for the baby during the first six months of life.
For many reasons, it is an important substance for the first few days of a baby’s life. Colostrum is a yellowish liquid that is secreted by the breast. It has a high content of proteins and minerals. The production of colostrum is carried out when the mammary glands are preparing to generate milk which will serve as the exclusive food for the baby during the first six months of life.
Benefits of colostrums/Foremilk
Colostrum is extremely vital for the baby throughout the primary days after birth. Besides breast milk, which will be incorporated a bit later, it constitutes the basis of the mandatory diet for this vital stage of a baby’s life.
Here are a couple of advantages that colostrum provides:
• They are a good supply of vitamins, minerals and calories. Most of the nutrients that a baby needs throughout the primary days may be found in high concentration in foremilk, as per the medical practitioners at AMRI Hospitals, one of the best child hospital in Kolkata.
• Provides protection against several diseases.
• Stimulates the primary stool referred to as faeces, which is a dark inexperienced stool, composed of the animal tissue cells of the intestines, water and gall.
What does colostrum contain?
As we have explained earlier, milk is an important supply of nutrients for babies throughout the primary days after childbirth. Here are many vital elements of this special milk:
• Amino acids that are elementary for cellular metabolism.
• Immunoglobulins enable the body to defend itself against infections and alternative threats.
• Vitamins allow the metabolism of proteins, fats and carbohydrates.
• Cytokines contain antivirals and play a crucial role within the development of joints.
Colostrum contains several alternative components that are necessary for numerous functions. It conjointly plays a crucial role, once it involves growth and immunity.
It conjointly plays a crucial role, once it involves growth and immunity.
Normal milk can be of two types:
Foremilk and hindmilk:
Normal milk can be of two types again: foremilk and hindmilk. Foremilk is the first milk that comes out from the breast. After few minutes, the latter part of the milk that comes is called the hind milk. Every infant needs these two types of milk at a time. So, it is advisable that mother empties one breast at a time, so that the baby can get both the foremilk and hind milk together. After that, they should move to other breast so that they can get both the foremilk and hind milk for the second time. The milk production can continue for up to a period of 2-3 years.
Breast milk, the healthiest food you can give to your baby, contains fat, which babies and even young kids need to grow and help their body absorb and process essential vitamins and minerals. If you're pregnant and researching about breast milk, fat content will come up in the context "foremilk" and "hindmilk."
If you're pregnant and researching about breast milk, fat content will come up in the context "foremilk" and "hindmilk."
Experts differentiate foremilk and hindmilk once a baby receives it during a feed. Colostrum is what your baby gets at the start of a feed, whereas hindmilk is the breast milk your baby consumes towards the tip of a feeding session. La Leche League International explains how milk turns into hindmilk: "As milk is created, fat sticks to the edges of the milk-making cells and therefore the watery part of the milk moves down the ducts toward your reproductive organ, where it mixes with any milk left there, from the last feed. The longer the time between feeds, the more diluted the leftover milk becomes."
There is no actual time lapse as to when milk become hindmilk. As your baby latches and feeds, the breast milk he consumes becomes fattier over time because the breast drains it fully.
Foremilk and hindmilk contain all the nutrients that build breast milk, and therefore is very precious for your baby.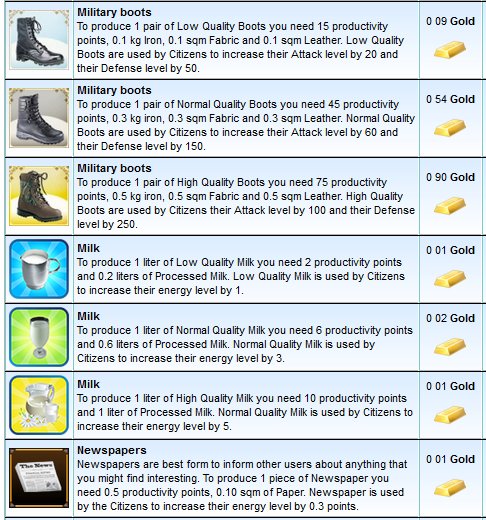 The minimal distinction is that hindmilk has higher amounts of fat and contains additional calories, explain doctors at AMRI Hospitals Kolkata. On the other hand, foremilk contains less fat; however is high in milk sugar, (i.e., sugar) which is additionally essential in your growing baby's diet. An excessive amount of milk may result in temporary genetic disease for a baby. It may additionally cause some babies to be additional fussy, gassy or show pain symptoms, or have loose inexperienced internal organ movements.
The minimal distinction is that hindmilk has higher amounts of fat and contains additional calories, explain doctors at AMRI Hospitals Kolkata. On the other hand, foremilk contains less fat; however is high in milk sugar, (i.e., sugar) which is additionally essential in your growing baby's diet. An excessive amount of milk may result in temporary genetic disease for a baby. It may additionally cause some babies to be additional fussy, gassy or show pain symptoms, or have loose inexperienced internal organ movements.
Although colostrum is only produced in limited quantities, it plays an important role in the lives of newborns. It’s important to emphasize once again, the importance of breastfeeding cannot be ignored at the start of a baby’s life.
Blog Archive
Month } Feb { } Mar { } Oct
Year2022
Locations
AMRI DHAKURIA
AMRI SALT LAKE
AMRI MUKUNDAPUR
AMRI BHUBANESWAR
AMRI SOUTHERN AVENUE
Recent Blog
What is kneecap (Patella). ..
..
The patella (knee cap) is a small bone in front...
read more
HEART STENT - AMRI’S TAKE
For long, majority of Indians have been under s...
read more
MINIMAL ACCESS CANCER SUR...
MINIMAL ACCESS CANCER SURGERY (MACS)
read more
THE EVOLUTION OF CANCER
Over the last century, cancer has evolved from...
read more
Causes & How It Works
Overview
Lactation is the process of making human milk. It's driven by hormones and results in milk coming from your nipple.What is lactation?
Lactation is the process of producing and releasing milk from the mammary glands in your breasts. Lactation begins in pregnancy when hormonal changes signal the mammary glands to make milk in preparation for the birth of your baby. It’s also possible to induce lactation without a pregnancy using the same hormones that your body makes during pregnancy.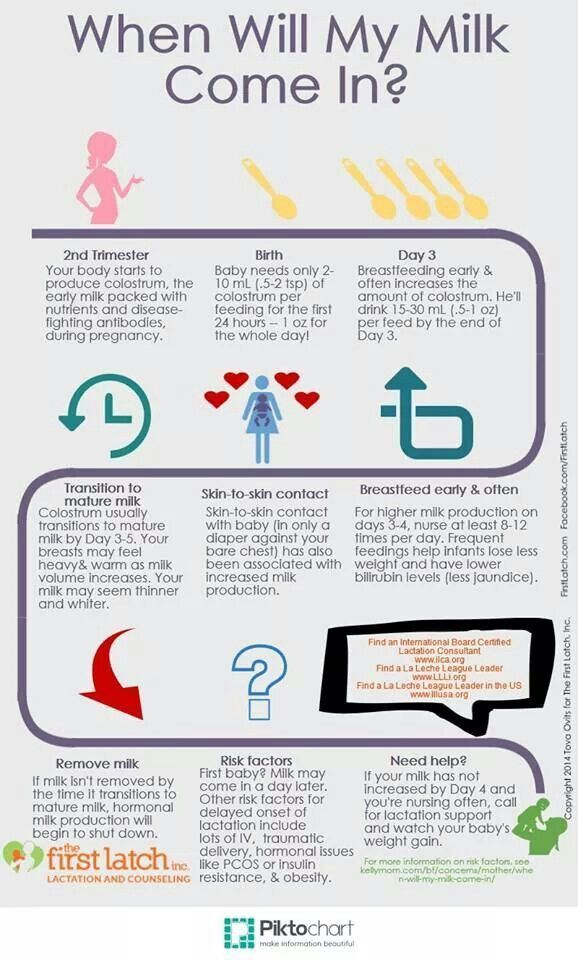 Lactation ends once your body stops producing milk.
Lactation ends once your body stops producing milk.
Feeding your baby directly from your breasts is called breastfeeding (or sometimes chestfeeding) or nursing. You can also feed your baby milk that you have expressed or pumped from your breast and saved in a bottle.
Where does human milk come from?
Human milk comes from your mammary glands inside your breasts. These glands have several parts that work together to produce and secrete milk:
- Alveoli: These tiny, grape-like sacs produce and store milk. A cluster of alveoli is called lobules, and each lobule connects to a lobe.
- Milk ducts: Each lobe connects to a milk duct. You can have up to 20 lobes, with one milk duct for every lobe. Milk ducts carry milk from the lobules of alveoli to your nipples.
- Areola: The dark area surrounding your nipple, which has sensitive nerve endings that lets your body know when to release milk. To release milk, the entire areola needs stimulation.
- Nipple: Your nipple contains several tiny pores (up to about 20) that secrete milk.
 Nerves on your nipple respond to suckling (either by a baby, your hands or a breast pump). This stimulation tells your brain to release milk from the alveoli through the milk ducts and out of your nipple.
Nerves on your nipple respond to suckling (either by a baby, your hands or a breast pump). This stimulation tells your brain to release milk from the alveoli through the milk ducts and out of your nipple.
It helps to think of the lactation system as a large tree. Your nipple is the trunk of the tree. The milk ducts are the branches. The leaves are the alveoli.
Why do people lactate?
The primary reason people lactate is to feed a baby. Lactation is a biological, hormonal response that occurs during and after pregnancy to feed a newborn baby. Your body triggers specific hormones to initiate milk production and ejection (releasing of milk). All mammals lactate for this purpose and it’s possible to induce lactation in men and in non-pregnant women using the right hormone medications.
Function
What triggers lactation?
A series of hormonal events, which begin when you’re pregnant, trigger the lactation process. That process is called lactogenesis.
Stage one lactogenesis: This begins around the 16th week of pregnancy and lasts until a few days after you give birth.
- Estrogen and progesterone rise and cause your milk ducts to grow in number and size. This causes your breasts to become fuller. Your mammary glands begin to prepare for milk production.
- Your nipples darken and your areolas become larger.
- Your Montgomery glands (small bumps on the areola) secrete oil to lubricate your nipple.
- Your body begins making colostrum. It’s highly nutritious and filling and serves as your baby’s first milk.
Stage two lactogenesis: This stage starts about two or three days postpartum (after giving birth). It’s when milk production intensifies.
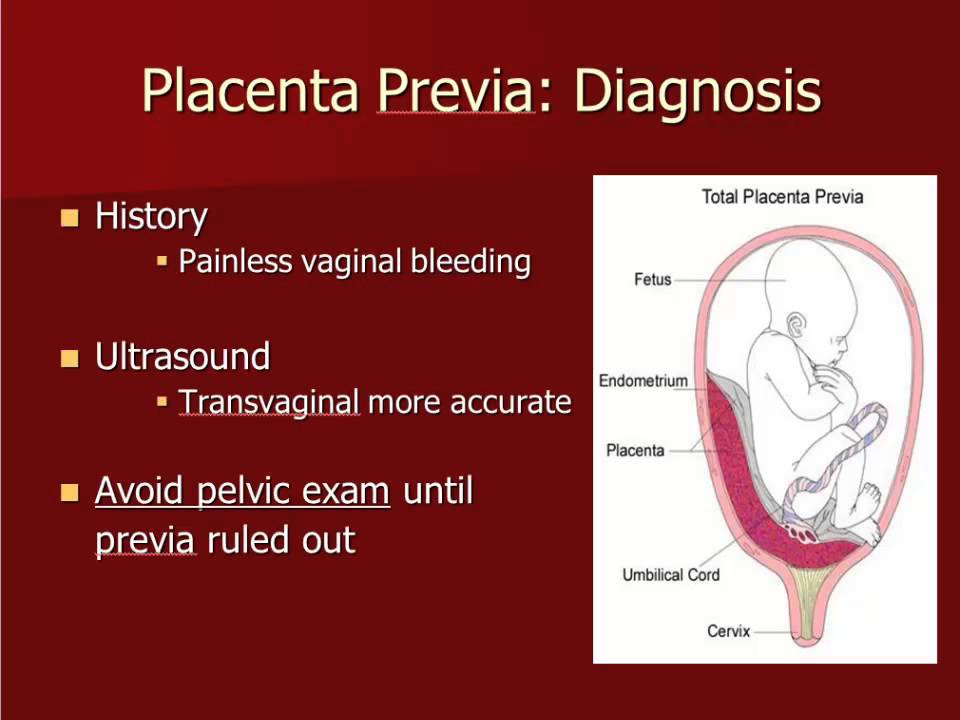
- Once your baby and placenta are delivered, a sudden drop in your estrogen and progesterone causes the hormone prolactin to take over.
- Prolactin is the hormone that produces milk.
- You’ll notice your milk production increases dramatically at this stage.
 It’s often referred to as milk “coming in.”
It’s often referred to as milk “coming in.” - Your breasts are often engorged (or overly full of milk) to the point where they feel sore, painful or tender.
Stage three lactogenesis: This describes the rest of the time you lactate.
- Lactation generally continues as long as milk is removed from your breast.
- The more milk that’s removed, the more milk your body makes to replace it. Frequent feeding or pumping will cause your body to make more milk.
Hormones for lactation
The hormone prolactin controls the amount of milk you produce, and your body begins producing prolactin early in pregnancy. At first, the high levels of estrogen, progesterone and other pregnancy hormones suppress prolactin. Once you deliver the placenta, those pregnancy hormones drop and prolactin takes charge.
When your baby suckles, it stimulates nerves that tell your body to release prolactin and oxytocin. Prolactin causes the alveoli to make milk and oxytocin causes muscle contractions that push out of the alveoli and through the milk ducts.
When milk is released, it’s called a “letdown,” and it takes about 30 seconds of suckling before the letdown occurs. Because you can’t control which breast receives the hormones, the letdown can cause milk to drip from both nipples.
Inducing lactation in people who aren’t pregnant requires medication that mimics hormones your body makes during pregnancy. Suckling from the nipple can initiate lactation, either with a breast pump or by a baby. This is a complex process that involves working closely with a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
When do you lactate during pregnancy?
Lactation begins as early as a few weeks into the second trimester of your pregnancy. As estrogen and progesterone levels rise, your body prepares for lactation by increasing the number of milk ducts in your breasts, and those milk ducts will transport milk from the alveoli to your nipples. About midway through pregnancy, your body creates colostrum, which is your baby’s first milk.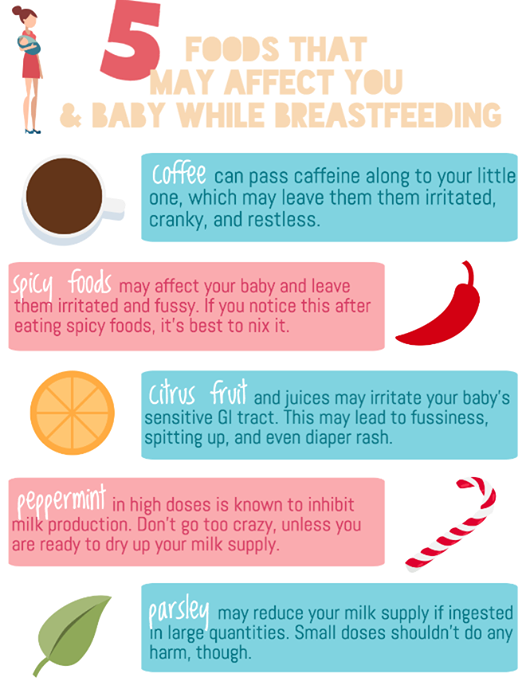
Can you lactate when you’re not pregnant?
Yes, it’s possible to lactate if you’re not pregnant. Inducing lactation is a complex process that usually involves using hormone-mimicking drugs for several months to produce milk. The second part of lactation is expressing the milk through your nipple. Stimulation from infant suckling, pumping with a breast pump or hand-expressing signals the brain to release the milk. It’s common for people in this situation to receive assistance from a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
How do you stop lactation?
There are many reasons why you might need to stop producing milk, and you can stop lactating either naturally or with the help of hormonal drugs.
Natural milk suppression
Lactation is a supply-and-demand process. Your milk supply gradually goes down as your baby relies less on breast milk, or as you reduce the number of times you nurse or pump.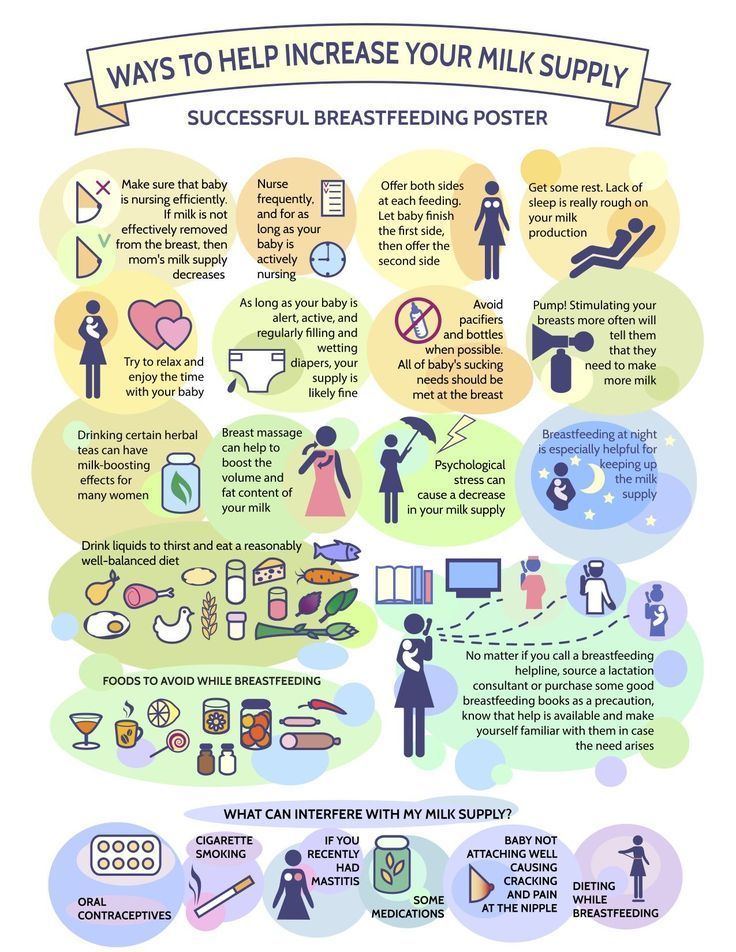 Generally, if you decrease the volume of milk removed from your breasts, your body will slow milk production.
Generally, if you decrease the volume of milk removed from your breasts, your body will slow milk production.
Suppressing your milk can feel uncomfortable and most people will become engorged (the term for overfilled breasts). You may also leak milk or develop a clogged milk duct. However, you can treat that pain by taking an over-the-counter pain reliever, wearing a firm bra or using an ice pack on your breasts.
Medication suppression
Medications can also be an option if you need to stop producing milk. Your healthcare provider can explain more about lactation-suppressing drugs, as well as the benefits and possible side effects.
Anatomy
Where are the mammary glands located?
Mammary glands are commonly called breasts and both genders have them. They are located on your chest and are composed of connective tissue, fat and special glandular tissue that makes milk. A woman’s glandular tissue is slightly different because it contains the alveoli and lobules necessary for producing milk. Women also have much more glandular tissue.
Women also have much more glandular tissue.
Conditions and Disorders
What are common conditions that affect your ability to lactate?
The ability to lactate and the length of time you’re able to produce milk varies. Some can produce milk for years, while others have trouble producing enough milk for their baby.
Some common factors that can impact lactation or breastfeeding are:
- Hormonal levels and conditions.
- Medications.
- Undergoing radiation therapy in the past.
- Trauma to your breast or nipples.
- Breast augmentation, reconstruction or other breast surgeries.
- Other medical conditions like HIV infection.
- Use of drugs and alcohol.
If you’re nursing or pumping your milk to bottle-feed your baby, you should always consult with your healthcare provider before starting any new medications or treatments. Many medications can pass to your baby through breast milk, which may have dangerous effects on your baby.
What is lactational amenorrhea?
Lactation amenorrhea (ah-men-oh-re-uh) means you aren’t menstruating (getting a period) due to lactation. When you’re lactating, your body produces prolactin, the hormone that produces milk. Prolactin reduces the amount of luteinizing hormone (LH) in your body, which helps trigger the release of an egg during ovulation. If you aren’t producing enough LH, you can’t ovulate or get your period. The length of time you can be amenorrheic due to lactation varies from a few months or until you’re completely done lactating.
Does lactation reduce my risk of any diseases?
Studies have shown that breastfeeding reduces a woman’s risk of ovarian and breast cancers. It can also lower your risk for Type 2 diabetes and high blood pressure.
Care
How do you maintain milk production?
Maintaining lactation is mostly based on supply and demand. The more your baby breastfeeds or the more milk you express with a breast pump, the more your body will make. There are ways to suppress lactation with hormones or oral contraceptives. If you wish to maintain lactation, some things you should do are:
There are ways to suppress lactation with hormones or oral contraceptives. If you wish to maintain lactation, some things you should do are:
- Continue nursing on-demand or pump milk frequently (approximately every four hours).
- Eat a healthy diet with enough calories. Low-calorie diets can decrease milk supply.
- Drink plenty of water to stay hydrated. Human milk is primarily water.
- Avoid smoking, drugs or alcohol. These can reduce your supply and transfer to your milk.
Frequently Asked Questions
What is the difference between lactation and colostrum?
Lactation describes the process of making and secreting milk from your breast. Colostrum is the first milk your breasts create during lactation and the first milk your baby drinks. It’s thick, yellow and commonly called “liquid gold.” Colostrum is high in protein, minerals, vitamins and antibodies.
What is hormone therapy for inducing lactation?
Couples or families who wish to induce lactation, maybe because of adoption, surrogacy or other reasons, can try hormone therapy. Induced lactation means you’re creating a milk supply without being pregnant. It’s a process that involves taking estrogen and progesterone for several months to make your body believe it’s pregnant. This helps prepare your breasts for lactation. Some medications and herbs are believed to help establish a milk supply, too.
Induced lactation means you’re creating a milk supply without being pregnant. It’s a process that involves taking estrogen and progesterone for several months to make your body believe it’s pregnant. This helps prepare your breasts for lactation. Some medications and herbs are believed to help establish a milk supply, too.
Several weeks before your baby arrives, begin pumping your breasts with a breast pump. This encourages your body to release prolactin, which produces milk. Ideally, you express your milk several times a day, just like you would if you had a baby. This helps establish a supply. You can also freeze any milk you produce for use once your baby arrives.
If you’re considering this as an option, you should talk to your healthcare provider about your desire to feed your baby with human milk. Induced lactation works for many people, but not all.
A note from Cleveland Clinic
If you want to feed your baby human milk, it’s helpful to understand the process of lactation so you know what to expect.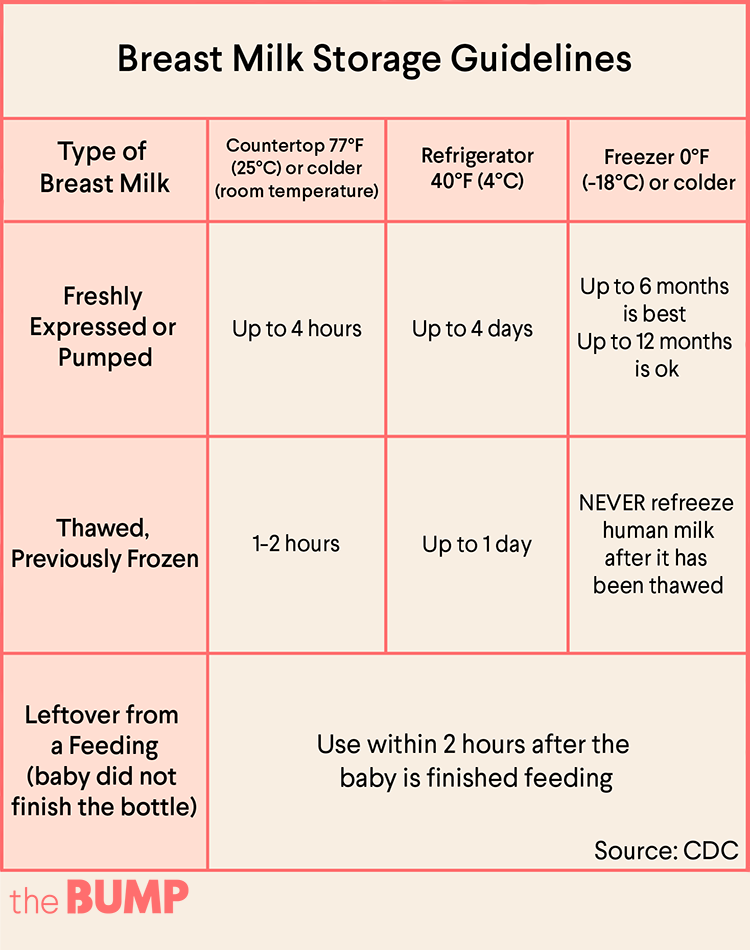 Talk to your healthcare provider about how to best prepare for nursing or expressing milk. Remember, lactation can look different for everyone depending on your circumstances and health history. If you struggle with lactation at any point, you may feel embarrassed or even ashamed. But struggling with lactation is very common, and lactation specialists and other healthcare providers can help you as you try to overcome these difficulties.
Talk to your healthcare provider about how to best prepare for nursing or expressing milk. Remember, lactation can look different for everyone depending on your circumstances and health history. If you struggle with lactation at any point, you may feel embarrassed or even ashamed. But struggling with lactation is very common, and lactation specialists and other healthcare providers can help you as you try to overcome these difficulties.
Breast milk production | Baby's needs
Did you know that the amount of breast milk adapts to your baby's needs? In this article, you will learn amazing facts about breast milk production in the first days, weeks and months.
Share this information
Your body is capable of producing breast milk for your baby at every stage of development. Understanding how milk production “turns on”, what happens to milk when you feed your baby, and why production adjusts to his needs as he grows, will help you start this amazing process in the right way.
Day one: milk production at birth
The baby is usually ready to breastfeed from birth. When he grabs the breast and begins to suck rhythmically, the milk-producing cells “turn on” and the formation of the first breast milk, colostrum, starts. 1 Try to feed your baby as much as possible in the first hour of his life, and then as soon as he shows interest in feeding. This will help lay the foundation for good milk production later on. 2
The first days: the arrival of milk
At this stage, your body's level of progesterone, the
pregnancy hormone, which begins to fall after the placenta comes out, is reduced, and the hormones responsible for milk production - prolactin, insulin and hydrocortisone - are included in the work. These hormones will help start milk production. 3 Around the third day of your baby's life, milk will begin to come in and you will feel that your breasts have filled up and become noticeably firmer. 1
1
First month: shaping milk production
During the first weeks, your body will be especially sensitive to the amount of milk produced as it learns to produce the right amount. Prolactin levels increase dramatically each time you empty your breasts, thereby helping shape the lactation process. It also contributes to the maturation of your milk in terms of composition. At this stage, transitional milk is produced and the amount continues to grow. 3.4
For good long-term milk production, it is very important that you are close to your baby during the first few weeks. The more often you breastfeed, the more milk will be produced. This process resembles the law of supply and demand. Each time after emptying the breast, whether it is feeding the baby or pumping, even more milk will be produced.
Remember that it is normal for newborns to eat frequently, perhaps even every 45 minutes, and this does not mean that they are not getting enough milk. Frequent feedings help shape milk production, so feed your baby on demand, not on a schedule.
Frequent feedings help shape milk production, so feed your baby on demand, not on a schedule.
“In the first few weeks you may feel like you don’t have enough milk because your baby will be feeding all the time, but that’s okay,” says UK mom-of-two Jo, “We tend to think that the baby wants to eat every few hours, but that is not necessarily the case."
Don't forget that babies also breastfeed for comfort. Breastfeeding helps them calm down and adjust to their new life outside the womb. In addition, feeding helps to establish a connection between you.
Stable milk production in the first month
If you follow your baby's needs and feed him as often and for as long as he wants, milk production should adjust. 5
Some mothers try to increase the period between feedings so that the breasts can produce more milk during this time, but this should not be done, as this may have the opposite effect. 2
If you are unable to breastfeed directly for the first two weeks, express your milk to build and maintain your milk supply during this critical period and beyond.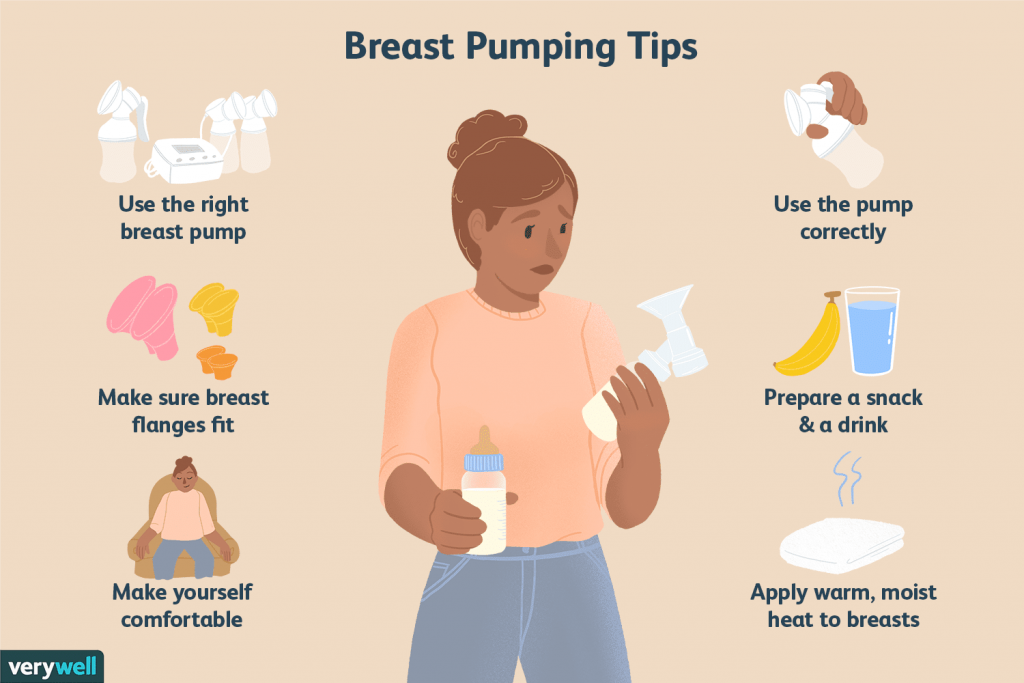
Did you know that feeding your baby extra formula unnecessarily can reduce your milk production? The chest will not receive a signal to increase production, because it will not be emptied. In addition, if the baby sleeps longer after formula, he may miss his usual next feeding time.
This is a kind of “supplementing trap”. After three to four days of formula supplementation, during which the breasts have emptied less, the body will receive a signal that breastfeeding has stopped, and the amount of milk produced will begin to decrease. As a result, the baby will remain hungry and will need additional formula supplementation. And so on in a circle ... As a result, this will lead to really low milk production, and the baby will eat mainly the mixture.
Breast milk production after six weeks
After a month of breastfeeding, post-feeding bursts of prolactin secretion begin to decrease, milk matures, and the body gets used to producing as much milk as your baby needs.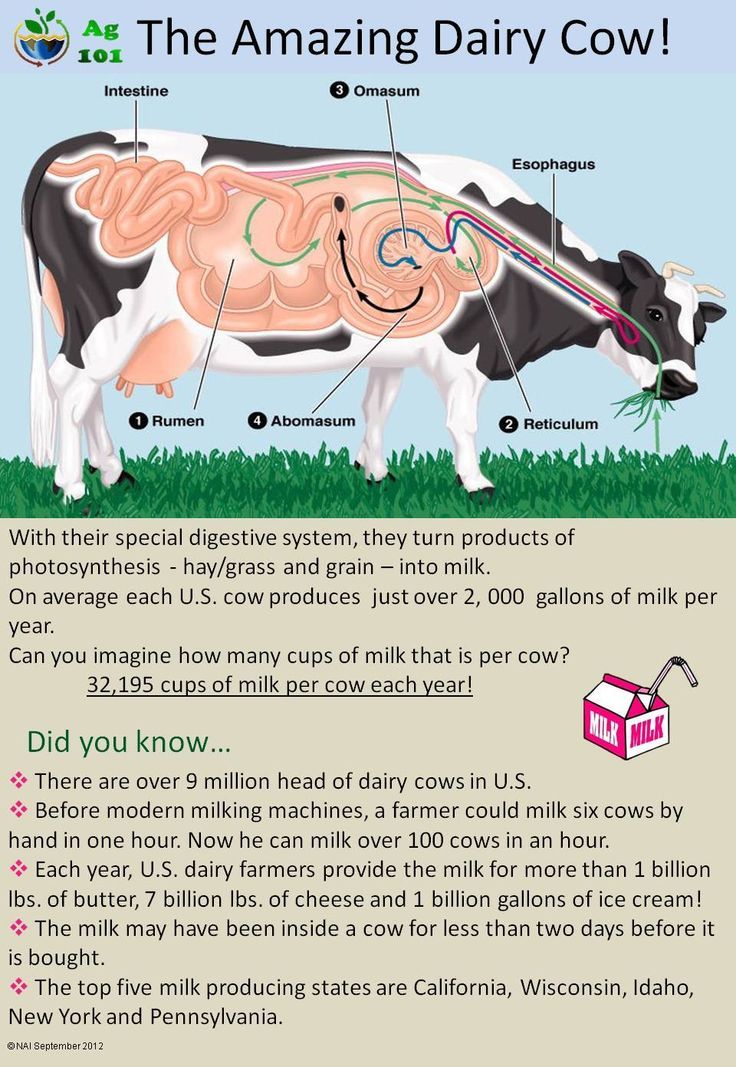 In fact, the chest begins to work "on autopilot." 4 You may also notice at this time that your breasts are softer and your milk flow has stopped.
In fact, the chest begins to work "on autopilot." 4 You may also notice at this time that your breasts are softer and your milk flow has stopped.
At this stage, women often have fears of "losing milk".
However, this only means that milk production has been established and now fully meets the needs of the child. It is noteworthy that although the baby continues to grow, he will consume approximately the same amount of milk both at six weeks and at six months. You may notice that the baby began to suckle the breast longer, but less often. On some days he may eat a little less than usual - his appetite changes in the same way as an adult.
Now your body will produce exactly the amount of milk,
as much as your baby needs. Therefore, the more milk the baby
drinks (or you express), the more it will produce.
How does this happen? The reason for this is thought to be the so-called "feedback lactation inhibitor" that controls milk production. The more milk in the breast, 2 the higher the inhibitor level, so a full breast produces less milk than one that has been emptied.
The more milk in the breast, 2 the higher the inhibitor level, so a full breast produces less milk than one that has been emptied.
What is the rate of milk production?
Mothers often worry about their milk supply and think about how to increase it. However, if the baby is healthy and growing well, problems usually do not arise.
“I was worried that my newborn daughter was not getting enough milk as she was feeding very quickly and always from one breast even though I offered both,” says Marjorie, mother of two in the UK, “But when I pumped from using a breast pump, I was surprised at how much milk I produced, and calmed down. I just had to keep feeding her little and often.”
Keep in mind, however, that not all mothers are able to express a lot of milk right away. You can also try hand expressing milk and see if there is a change in breast fullness.
If you're worried about your milk supply, read our tips for symptoms of too little or too much milk.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet Gynecol Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". F Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
3 Ostrom KM. A review of the hormone prolactin during lactation. Prog Food Nutr Sci . 1990;14(1):1-43. - Ostrom KM, "Review of the role of the hormone prolactin during lactation." Prog Food Nutr Sai. 1990;14(1):1-43.
1990;14(1):1-43. - Ostrom KM, "Review of the role of the hormone prolactin during lactation." Prog Food Nutr Sai. 1990;14(1):1-43.
4 Cox DB et al. Blood and milk prolactin and the rate of milk synthesis in women. Exp Physiol. 1996;81(6):1007-1020. - Cox D.B. et al., Effects of blood and milk prolactin on milk production in women. Exp Physiol. 1996;81(6):1007-1020.
5 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-95. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3): e 387-95.
When it's time to stop breastfeeding :: City Polyclinic No. 12
There is a great variety of opinions on this matter: the time when it is time to wean a child from the breast varies from several months to infinity from the point of view of self-weaning advocates. But this issue has always been considered from the point of view of benefit to the baby. And what does medicine say about what terms of involution will be useful not for a child, but for a woman?
But this issue has always been considered from the point of view of benefit to the baby. And what does medicine say about what terms of involution will be useful not for a child, but for a woman?
What is lactation involution?
Involution of lactation (from lat. involutio - coagulation) is a physiological process that completes the period of breastfeeding. This biological mechanism starts on the 40th day from the moment the baby was last attached to the breast. Since the onset of involution, the mammary glands decrease in size and stop producing breast milk. Usually, the process of involution is recommended to be carried out gradually so that the child can adapt to a new way of getting food, and also learn to calm down without being attached to the mother's breast.
Under normal conditions, each mammary gland will continue to lactate as long as milk is removed from it - and this phenomenon, the same for animals and humans, is used in agriculture.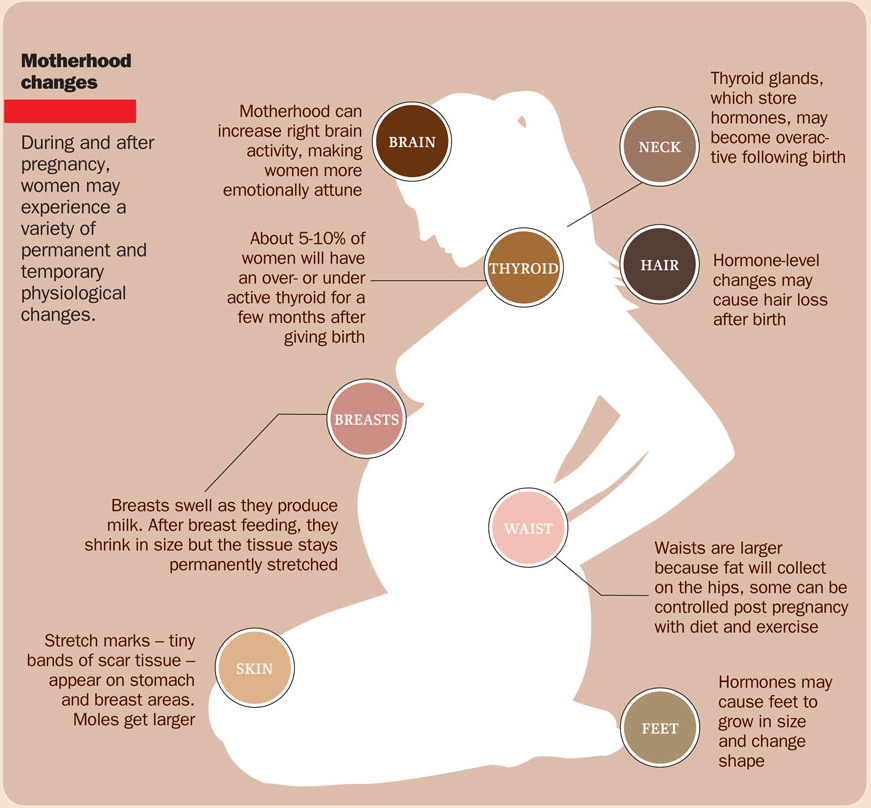 As the volume of milk production decreases, its composition changes: the content of fat, immunoglobulins increases, and the level of lactose decreases. If lactation is not stopped forcibly, it can continue until the baby is weaned from the breast; under natural conditions, this usually occurs in 2 - 2.5 years.
As the volume of milk production decreases, its composition changes: the content of fat, immunoglobulins increases, and the level of lactose decreases. If lactation is not stopped forcibly, it can continue until the baby is weaned from the breast; under natural conditions, this usually occurs in 2 - 2.5 years.
The process starts when the pituitary gland stops producing enough of the hormone prolactin. Milk production continues for some time after the cessation of its suction. As they write in the materials of the WHO, “if in most mammals “drying” occurs on the 5th day after the last feeding, then the period of involution in women lasts an average of 40 days. During this period, it is relatively easy to restore full lactation if the child resumes frequent suckling.
Thus, as soon as attachments to the breast become rare and short, the process of involution begins. This can happen at any time - it is known that sometimes children themselves refuse breastfeeding for a variety of reasons that need to be discussed separately. There is an inhibition of protein synthesis and structural changes in the mammary gland - the reverse replacement of the glandular tissue with adipose tissue begins, which allows the breasts to return to their previous size and shape.
There is an inhibition of protein synthesis and structural changes in the mammary gland - the reverse replacement of the glandular tissue with adipose tissue begins, which allows the breasts to return to their previous size and shape.
Signs of lactation involution
If involution occurs naturally, it usually starts when the child is two years old. At this time, the frequency of attachment naturally decreases: the child has other interests, including interest in "adult" food. How can a nursing mother understand that involution has begun?
The breasts shrink slightly and do not fill with milk even if you do not feed for more than 12-24 hours. That is why if at this time the child stops breastfeeding, this does not cause any frustration and suffering from excess milk in the mother. Milk, in terms of composition, properties and appearance, is increasingly reminiscent of colostrum.
The baby's sucking activity is markedly increased. This is due to the fact that milk production is reduced, and the child is still trying to suck out the same amount of portion.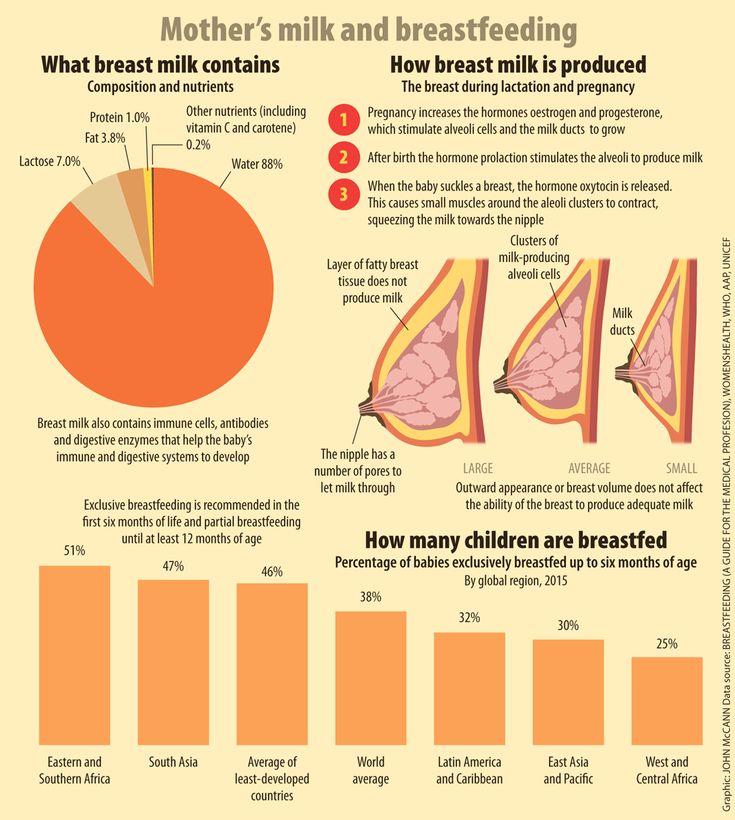 A child for one feeding can be applied to one breast, then to the other - and so on several times. The period of such sucking activity can last up to several months.
A child for one feeding can be applied to one breast, then to the other - and so on several times. The period of such sucking activity can last up to several months.
Mother's psychological readiness for weaning. This is a very important sign that should not be ignored. As soon as a nursing mother is tired of breastfeeding, this is a sign that the process is either incorrectly regulated, or, if there have been no problems with lactation so far, it is coming to an end.
Psychological readiness of the child for weaning. Usually, by the age of two, the child is socialized, ceases to experience an urgent need for tactile contact with the mother, and begins to receive the necessary nutrients from other sources. The psychological need for the child gradually disappears
Forced involution
If there is a need to wean the child prematurely, then you need to be prepared for the following consequences:0003
- pain and discomfort in the mammary glands of varying intensity;
- formation of seals in the area of the mammary glands;
- fever;
- deterioration in general condition;
- purulent-inflammatory complications (breast abscess and mastitis).

If the need to interrupt lactation is associated with medical indications, then it is necessary to carry out involution under the supervision of a physician. What needs to be done first? Reduce the number of feedings by offering the baby a different food source. In addition, strict control of fluid intake with its restriction is necessary, and additional pumping may be required in order to avoid stagnation of milk.
If you are tired of breastfeeding
The psychological state of a breastfeeding mother is a very important criterion that must be paid close attention to. Lactation is a very energy- and resource-intensive project for the female body, and it is not surprising that exhaustion sets in sooner or later. Some nursing mothers can wait for natural involution without any problems, but for many there comes a point when, due to fatigue, continuing to feed is impossible. Unfortunately, this objective situation (the amount of forces and resources is strictly individual) often causes a feeling of guilt in a nursing mother, since the advertising of the need for breastfeeding before self-weaning has reached its maximum in recent years. What needs to be assessed at this moment? On one side of the scale, there is a benefit for the child, and on the other, the psychological and physical comfort of the mother.
What needs to be assessed at this moment? On one side of the scale, there is a benefit for the child, and on the other, the psychological and physical comfort of the mother.
Many will choose the comfort of their mother in such a situation, and they will be right. How long breastfeeding will continue is up to her to decide, since only she can assess the degree of her exhaustion. After all, there are now excellent breast milk substitutes, and a calm and rested mother is an irreplaceable resource that cannot be replaced by anything.
Many experts say that breastfeeding up to a year and a half may be optimal. Thus, the well-known pediatrician Dr. Komarovsky recommends starting breastfeeding correction starting at the age of one: at this age it is already time to introduce calming rituals that replace breastfeeding, and also gradually reduce the number of daily feedings. WHO recommendations to breastfeed children for more than two years, according to Komarovsky, are due to high infant mortality rates in Asia and Africa, where a child's life often directly depends on how long his mother breastfeeds.