How early do headaches start in pregnancy
Headaches during pregnancy | Pregnancy Birth and Baby
Headaches during pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Headaches in women can often be triggered by a change in hormones during pregnancy. Expectant mothers may experience an increase or decrease in the number of headaches. Unexplained, frequent headaches later in your pregnancy could be a sign of a more serious condition called pre-eclampsia, so tell your doctor if this is the case.
Causes of headache during pregnancy
Many women experience headaches during pregnancy, especially in the first and third trimesters. If you're pregnant, you may notice an increase in the number of headaches you have at around week 9 of your pregnancy.
As well as hormonal changes, headaches in the early stages of pregnancy can be caused by an increase in the volume of blood your body is producing.
Other causes of headaches during pregnancy can include:
- not getting enough sleep
- withdrawal from caffeine (e.g. in coffee, tea or cola drinks)
- low blood sugar
- dehydration
- feeling stressed
- poor posture, particularly as your baby gets bigger
- having depression or anxiety
Migraine
Migraine is a particular type of headache that mostly occurs on one side of the head – it can be either moderate or very painful. People who experience migraine can also feel sick or vomit, and be sensitive to light or sound.
In pregnancy, migraine may get worse for the first few months, but for many women it can improve in the later stages of their pregnancy when the level of the hormone oestrogen stabilises. Other women may experience no change or a decrease in the number of migraine headaches while pregnant.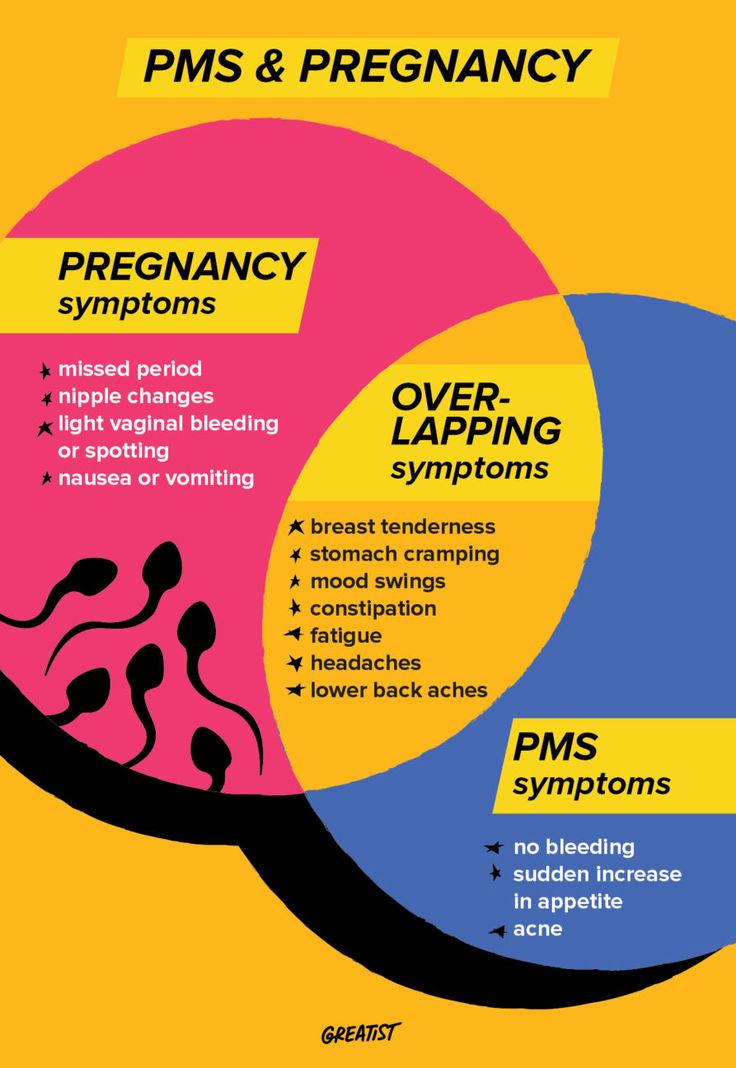 Some women may experience differences in migraine during different pregnancies.
Some women may experience differences in migraine during different pregnancies.
Treatment
It’s not advisable for pregnant women with migraine to use migraine medicine. For other headaches it's also recommended that you try to treat your headache without medicine.
You could try:
- getting more sleep or rest and relaxation
- pregnancy yoga classes or other exercise
- practising good posture, particularly later in your pregnancy
- eating regular, well-balanced meals
- putting a warm facecloth on your eye and nose area, if it is a sinus headache
- putting a cold pack on the back of your neck, taking a bath or using a heat pack, if it is a tension headache
- neck and shoulders massage
Pregnant women who experience migraine should avoid things that may trigger their migraine. This may include:
- chocolate
- yoghurt
- peanuts
- bread
- sour cream
- preserved meats
- aged cheese
- monosodium glutamate (MSG)
- caffeine (withdrawal from)
- bright or flickering lights
- strong smells
- loud sounds
- computer or movie screens
- sudden or excessive exercise
- emotional triggers such as arguments or stress
If you do take medicine for your headache or migraine you should check with your doctor, pharmacist or midwife first.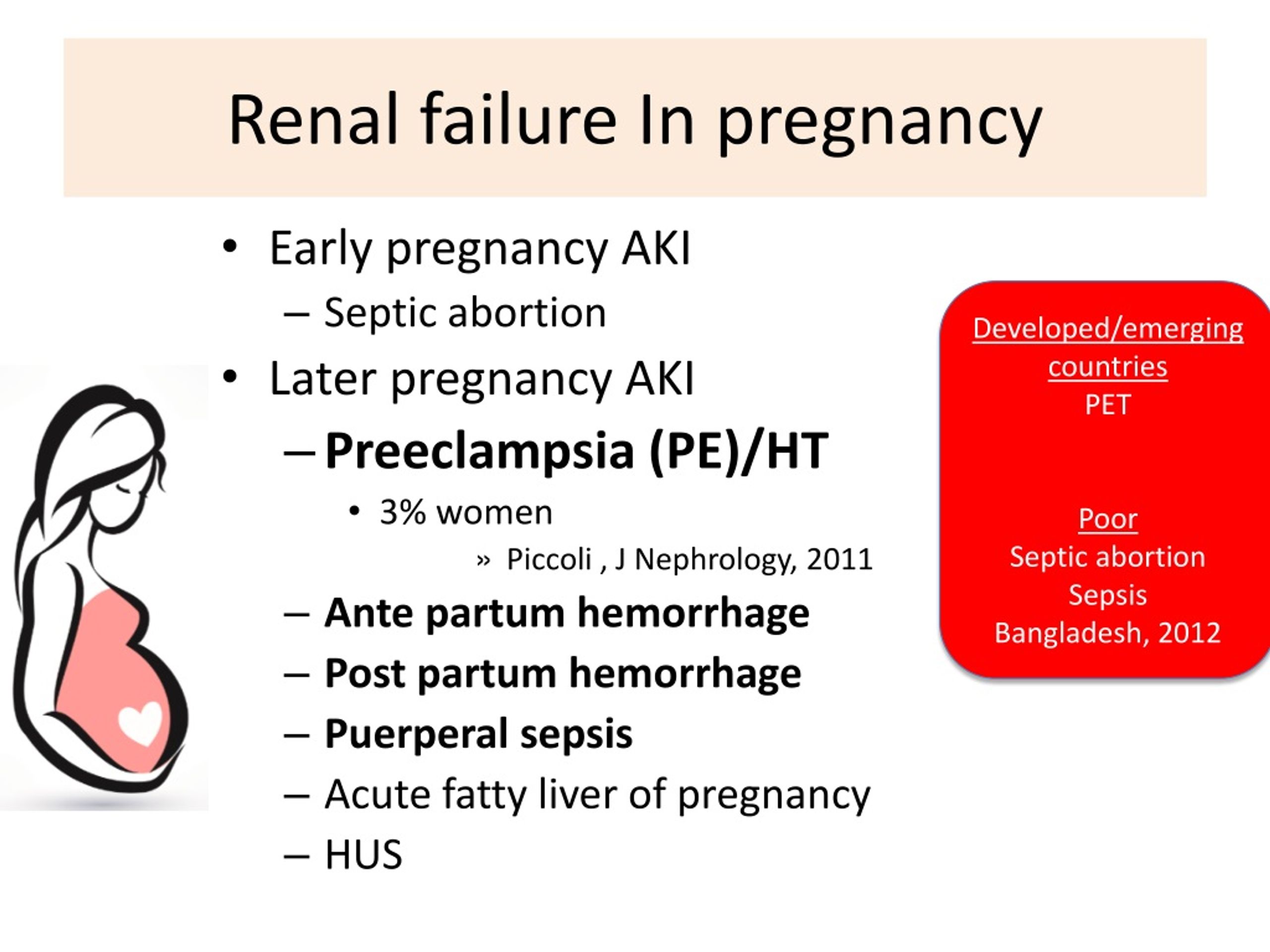 Paracetamol, with or without codeine, is generally considered safe for pregnant women to use but you should avoid using other pain medicine such as aspirin or ibuprofen.
Paracetamol, with or without codeine, is generally considered safe for pregnant women to use but you should avoid using other pain medicine such as aspirin or ibuprofen.
When to contact your doctor
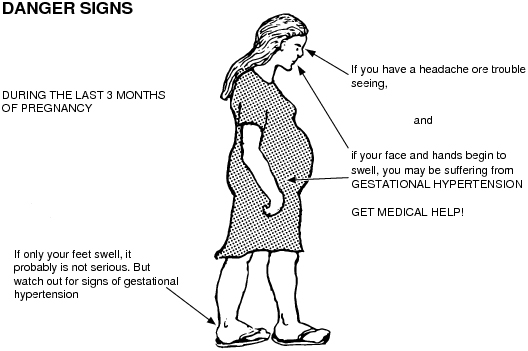
If you experience frequent headaches that don't go away with paracetamol, it could be a sign of a more serious medical condition called pre-eclampsia. This usually involves an increase in the pregnant woman's blood pressure and problems with her kidneys. There are also other serious risks for both you and your baby. Pre-eclampsia mostly occurs in the second half of pregnancy.
Contact your doctor, particularly if, along with your headaches, you have a pain below your ribs, feel like you have heartburn, you suddenly swell in your face, hands or feet, or you have problems with your eyesight.
Further information
- Speak with your doctor or midwife, particularly if you have any concerns about pre-eclampsia
- Phone Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse.
- For more information about headaches during pregnancy, visit Headache Australia.
- For more information about medication during pregnancy, see your doctor or pharmacist, or visit NPS MedicineWise.
Sources:
Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Pre-eclampsia and high blood pressure during pregnancy), Headache Australia (Migraine), Women's and Children's Health Network (Medicines during pregnancy), Headache Australia (Adults and headache), Headache Australia (Migraine – A common and distressing disorder), Raising Children Network (9 weeks pregnant), Raising Children Network (34 weeks pregnant), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Perinatal Anxiety and Depression), American Pregnancy Association (Pregnancy and Headaches), NPS Medicinewise (Taking medicines in pregnancy), Australian and New Zealand College of Obstetricians and Gynaecologists (Is paracetamol safe to use in pregnancy?)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2020
Back To Top
Related pages
- Common discomforts during pregnancy
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.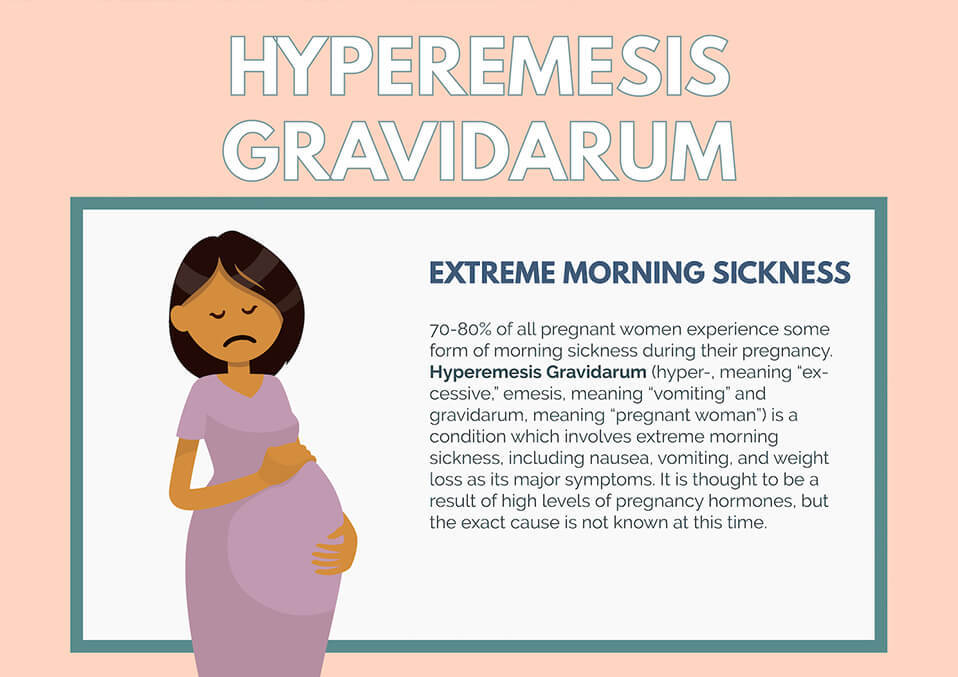 This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Headaches During Pregnancy | American Pregnancy Association
Headaches are one of the most common discomforts experienced during pregnancy and may occur at any time during your pregnancy, but they tend to be most common during the first and third trimesters.
During the first trimester, your body experiences a surge of hormones and an increase in blood volume. These two changes can cause more frequent headaches. These headaches may be further aggravated by stress, poor posture or changes in your vision.
Other causes of headaches during pregnancy may involve one or more of the following:
- Lack of sleep
- Low blood sugar
- Dehydration
- Caffeine withdrawal
- Stress (due to many changes)
Women who have regular migraine headaches may discover that they experience fewer migraines during pregnancy; however, some women may encounter the same number or even more migraine headaches.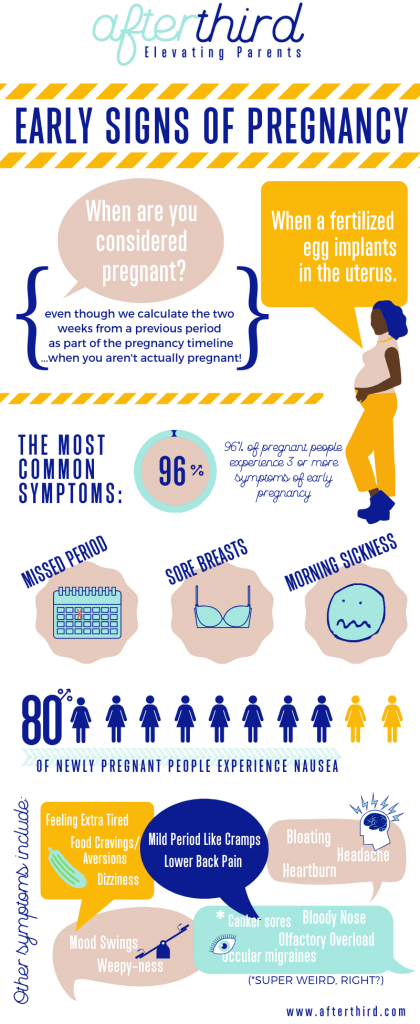 If you are pregnant, it is important to talk to your health care provider about any medications that you may be taking for headaches.
If you are pregnant, it is important to talk to your health care provider about any medications that you may be taking for headaches.
Headaches during the third trimester tend to be related more often to poor posture and tension from carrying extra weight. Headaches during the third trimester may also be caused by a condition called preeclampsia, which is high blood pressure during pregnancy.
How Do I Treat Headaches During Pregnancy?
During pregnancy, you want to try and relieve your headache by natural means if possible, however your health care provider may recommend acetaminophen.
You may want to try to relieve your headache with one or more of the following natural remedies:
- If you have a sinus headache, apply a warm compress around your eyes and nose
- If you have a tension headache, apply a cold compress or ice pack at the base of your neck
- Maintain your blood sugar by eating smaller, more frequent meals – this may also help prevent future headaches
- Get a massage – massaging your shoulders and neck is an effective way to relieve pain
- Rest in a dark room and practice deep breathing
- Take a warm shower or bath
- Practice good posture (especially during the third trimester)
- Get plenty of rest and relaxation
- Exercise
- Eat well-balanced meals
You may also reduce the likelihood of migraine headaches by avoiding common triggers of migraine headaches:
- Chocolate
- Alcohol
- Yogurt
- Aged cheese
- Peanuts
- Bread with fresh yeast
- Preserved meats
- Sour cream
When Should I Contact My Doctor?
- Before taking any medications
- If you do not experience any relief from the remedies above
- Your headaches get worse or more persistent
- You experience headaches that are different than normal
- Your headaches are accompanied by blurry vision, sudden weight gain, pain in the upper right abdomen, and swelling in the hands and face
Want to Know More?
- 7 Common Discomforts of Pregnancy
- Treating Muscle Cramps Naturally During Pregnancy
- Pregnancy and Leg Cramps
Compiled using information from the following sources:
1. Williams Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 55.
Williams Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 55.
2. National Headache Foundation.
https://www.headaches.org
3. Mayo Clinic Guide To A Healthy Pregnancy Harms, Roger W., M.D., et al, Part 3.
Headache during pregnancy: where does it come from and how to get rid of it
November 14, 2020 Likbez Health
Sometimes you just need to get some sleep, and sometimes you need to call an ambulance immediately.
When to call an ambulance
Call 103 or 112 urgently if you experience any of the following symptoms:
- sudden and severe headache;
- consciousness becomes confused or completely lost;
- pain worsens over 5 minutes;
- flies, spots flash in the eyes;
- throbbing and noisy in the ears;
- speech has become slurred, words are drawn out;
- arms and legs weaken, convulsions set in;
- the muscles of the neck are very stiff, it is impossible to reach the chest with the chin;
- fever of 39 °C or more;
- increased heart rate at rest;
- severe shortness of breath;
- the child pushes without stopping or stops abruptly;
- leaking water or blood;
- lower abdomen hurts, as if contractions had started.

Why pregnant women can get headaches
Pregnancy headaches are not always life threatening. But the doctor needs to be told about it in any case. If the symptom appeared for the first time and does not hurt much, postpone the conversation until a scheduled visit. If your headache is recurring or gets worse, it's best to make an appointment as soon as possible. The gynecologist will decide what needs to be done or refer you to another doctor.
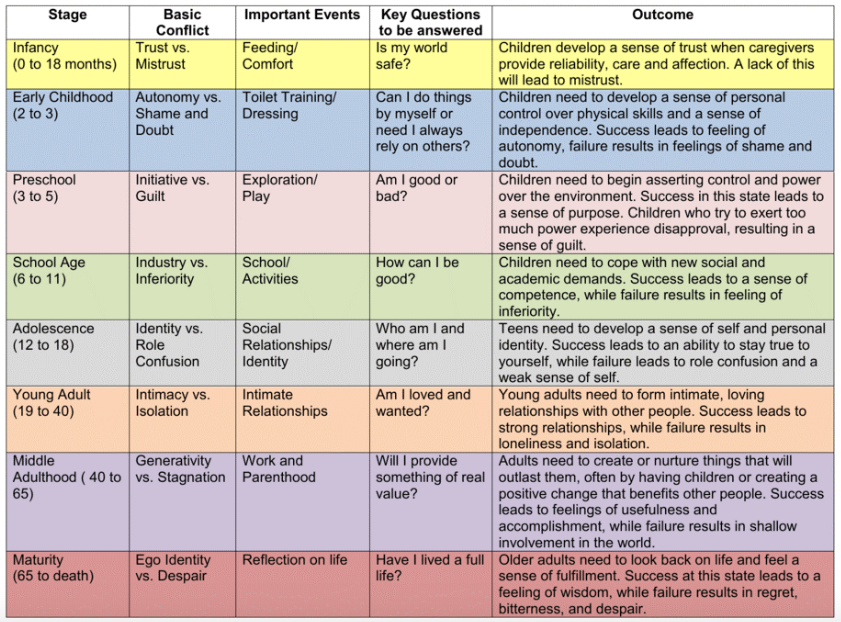
There are many causes of headaches. Scientists have found that in pregnant women in 57% of cases it is primary, that is, not associated with other diseases. The most common are migraines and tension headaches.
Everything else is a secondary headache caused by various pathologies. Usually it is high blood pressure and infections. But there are also more dangerous reasons.
1. Stress and fatigue
A pregnant woman's body experiences increased stress, because it has to work for two. If at the same time the expectant mother is exposed to stress, strong feelings or sleeps little, she develops a tension headache.
Discomfort lasts from 30 minutes to several days. The head hurts in the forehead, occiput, both temples. But there is no feeling that they put on a tight hoop or helmet. The pain does not get worse when bending over, walking, or climbing stairs, bright lights, or sounds.
What to do
Tension headache can go away on its own: just get some fresh air or sleep. Sometimes pleasant emotions help, which distract from experiences.
If the pain persists for 2-3 consecutive days, see a doctor. He will select painkillers that are safe for the child.
2. Medications
Any medicine that enters the stomach or bloodstream can cause headaches even if the dosage is correct. In pregnant women, this often occurs due to drugs for high blood pressure, heart disease, antibiotics, anticonvulsants.
Long-term use of non-steroidal anti-inflammatory drugs for headaches may cause the opposite effect: the pills do not remove, but provoke symptoms.
What to do
If your head hurts a few hours after taking the medicine, you need to see a doctor to change the medicine.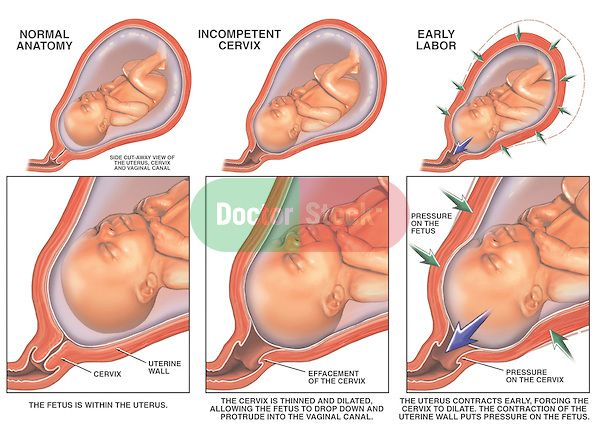 Do not drink non-steroidal anti-inflammatory drugs for more than 3-5 days. If they do not help, you need to tell the doctor about it.
Do not drink non-steroidal anti-inflammatory drugs for more than 3-5 days. If they do not help, you need to tell the doctor about it.
3. Love for coffee or rejection of it
Coffee can cause headaches during pregnancy. Unpleasant symptoms occur if you drink more than 3-4 cups a day.
Abrupt refusal of coffee is also harmful. It is worth finding out about pregnancy and stopping brewing a fragrant drink, and after 1-2 days, aching pain will appear in the temples and the back of the head.
What to do
Coffee is best avoided during pregnancy. If a headache occurs a day after this, you can drink a small cup of the drink and wait a day again. Gradually, the dependence on coffee will pass.
Coffee drinkers can reduce their drink intake to 1-2 cups per day.
4. Infection with fever
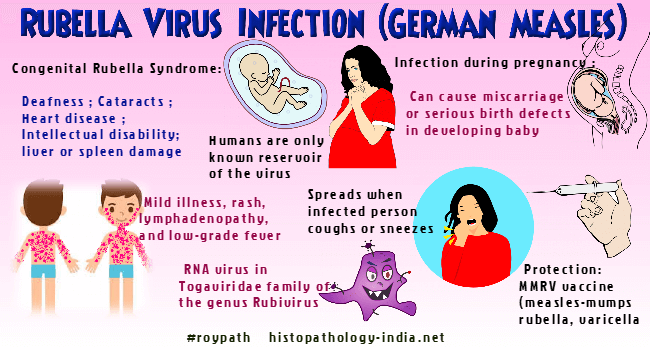
Acute viral (usually ARVI) or bacterial (eg, streptococcal tonsillitis) infections cause fever and headache. This is a normal reaction to foreign microorganisms.
But any infection is dangerous for pregnant women. It can cause fetal defects, growth retardation and even miscarriage. And with meningitis, especially listeriosis, there is a threat to the life of the mother.
What to do
If you have a headache with fever, call your doctor. He will prescribe safe medications or give you a referral to the hospital if a severe infection is suspected. In this case, you need strong antibiotics, droppers to maintain the body and sometimes hormones.
5. Preeclampsia and preeclampsia
After 20 weeks, preeclampsia may develop in pregnant women. This is a disease in which one of three symptoms or a combination of them may appear: high blood pressure, edema, and protein in the urine.
Without proper treatment, preeclampsia turns into preeclampsia. The pressure rises sharply, the head and lower abdomen hurt unbearably, the baby pushes unusually hard or, on the contrary, suddenly calms down. Preeclampsia can lead to placental abruption, damage to the liver and other organs, bleeding, and even seizures. Without urgent medical care, the fetus and mother die.
Without urgent medical care, the fetus and mother die.
What to do
When the first signs of preeclampsia appear, the pregnant woman is hospitalized to find treatment. After that, she is discharged home under the supervision of her gynecologist.
But if her health worsens, the doctor again sends the woman to the hospital, where she is prescribed medication to reduce pressure, special drips to keep her body functioning. If improvement does not occur within a day, a caesarean section is performed.
6. Migraine
One of the causes of migraine is a change in estrogen levels. But the disease very rarely appears due to pregnancy. On the contrary, in 70% of women, the symptoms subside dramatically after conception. Nevertheless, migraines torment many.
It may begin with an aura: flashes of light, spots before the eyes, tingling in the hands or numbness of half of the face, sometimes tinnitus. Each symptom can last from 20 minutes to an hour.
A migraine attack develops after the aura. In this case, one side of the head hurts and throbs, nausea or vomiting appears. A woman is irritated by bright lights, loud noises, smells. They make the pain worse.
In this case, one side of the head hurts and throbs, nausea or vomiting appears. A woman is irritated by bright lights, loud noises, smells. They make the pain worse.
Seizures last from a few hours to a week or more. After a migraine, there is a feeling of severe fatigue, exhaustion, and an awkward turn of the head can return the pain.
What to do
Any medication for migraine during pregnancy must be prescribed by a doctor. In some cases, drugs from the group of beta-blockers are used.
Studies have shown that frequent migraine in pregnancy is associated with a lack of magnesium. The doctor will help you choose the appropriate type of vitamin and mineral complex and its dosage.
7. Cerebral vascular disease
Hormone problems in some pregnant women increase blood clotting, which increases the risk of thrombosis, stroke or bleeding in the meninges. These conditions are very dangerous: a woman can die within a few minutes or remain disabled.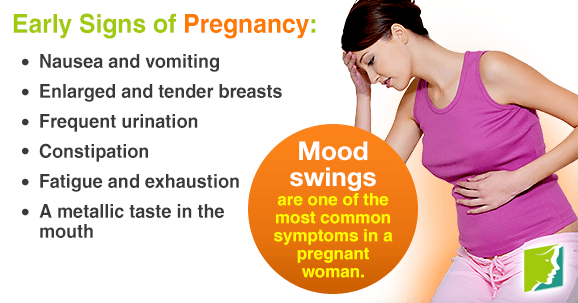
Vascular involvement is always accompanied by several symptoms:
- severe headache on one side;
- nausea and vomiting;
- blurred vision;
- loss of consciousness;
- convulsions.
What to do
Urgently call an ambulance. The pregnant woman must be laid or seated so that she does not hit when she falls. You can't give medicine! You can only open the window so that there is more air in the room.
Which treatment the doctor prescribes depends on the specific disease. These can be drugs that reduce blood clotting and dissolve blood clots. In some cases, urgent surgery is needed.
8. Brain tumors
Studies show that progesterone and estrogens during pregnancy can trigger or accelerate the growth of tumors in the brain. Symptoms of the disease appear slowly, over several months, and depend on the size and location of the tumor.
The headache may gradually increase, then vision, speech, hearing deteriorate, limbs go numb and convulsions appear.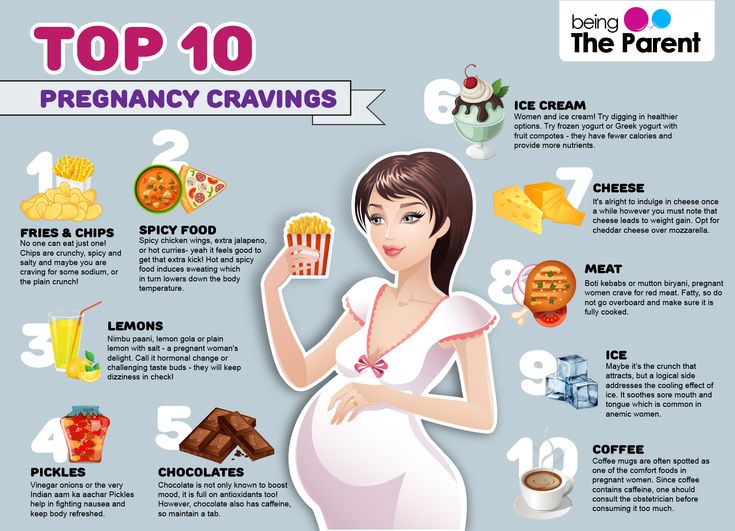 Sometimes it is difficult for a woman to keep her balance.
Sometimes it is difficult for a woman to keep her balance.
What to do
If a pregnant woman often has a headache or she forgets what she wanted to buy in the store and how to cook her favorite borscht, confuses her way home, you need to go to a neurologist. First, he will prescribe standard treatment, simple and safe medicines, rest, good sleep.
If this does not help, the symptoms persist or worsen, a deep examination is needed. The pregnant woman will be sent for an MRI of the brain. This procedure is safe for the fetus. If the diagnosis is confirmed, surgery may be required.
What to do if the doctor cannot find the cause of the pain
If you have been examined and the doctor cannot tell you why your head hurts and diagnoses you with vascular dystonia, this is cause for concern. There is no such disease.
Seek another doctor. Perhaps he uses new diagnostic methods that will help to deal with the problem and choose a treatment.
How to avoid pregnancy headaches
Experts recommend:
- Avoid triggers.
 For example, if you notice that certain foods, smells, or situations cause headaches, try not to encounter them.
For example, if you notice that certain foods, smells, or situations cause headaches, try not to encounter them. - Protect yourself from stress, do not worry about trifles.
- Move more. During pregnancy, walk every day in the fresh air and do special exercises for expectant mothers.
- Eat right. Try to eat a lot of vegetables and fruits, dairy products, drink at least 2.4 liters of liquid. Every day, the menu should include fish, poultry or lean meat. And it is better not to buy sweet, fast food and other junk food.
- Follow the daily routine. You need to sleep at least 8 hours a day and go to bed no later than 22-23 hours in order for melatonin to be produced normally.
- Learn to relax. Learn simple meditation techniques or breathing exercises.
Read also 🧐
- How pregnancy develops by week
- How to calculate the duration of pregnancy
- What rights does a pregnant woman have at work
- 7 best sex positions for pregnant women
- How to recognize a miscarriage and what to do next
Pregnancy headache
Authors: A.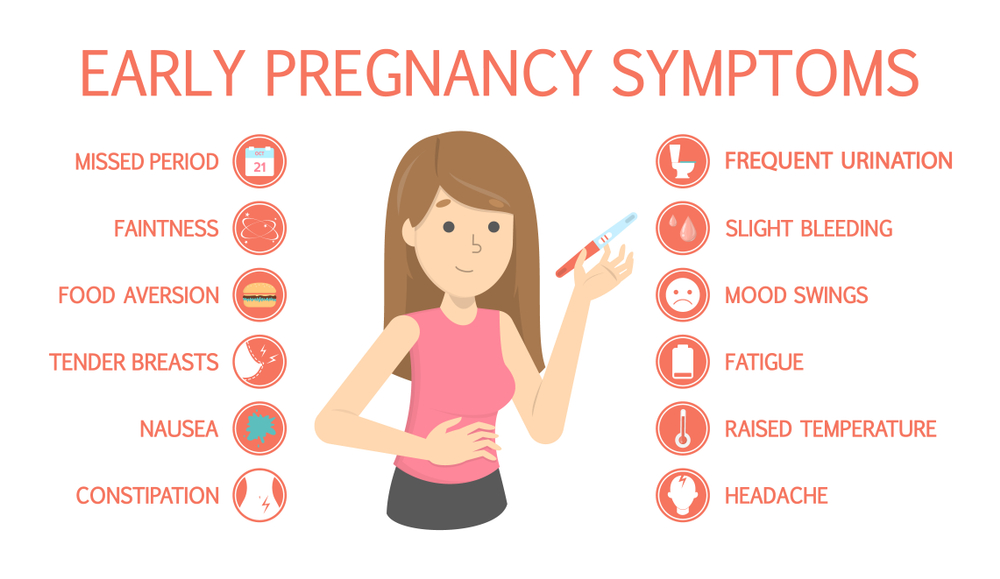 Yu. Limanskaya, Yu.V. Davydova
Yu. Limanskaya, Yu.V. Davydova
19.01.2017
A.Yu. Limanskaya
Tension headache and migraine are the most common types of headaches (30-78% and 15% respectively). According to the WHO, primary headache is in general in 10th place among all conditions leading to disability, and in women, in 5th place. In 16% of patients, episodic tension-type headache becomes chronic. The economic loss in Western Europe and North America due to headache-related disability is estimated at $17-20 billion a year. To date, there is a trend towards an increase in the incidence of headache in young people.
Yu.V. Davydova
The International Headache Society defines migraine as a throbbing, unilateral headache associated with nausea, sensitivity to light, sound, and turning of the head.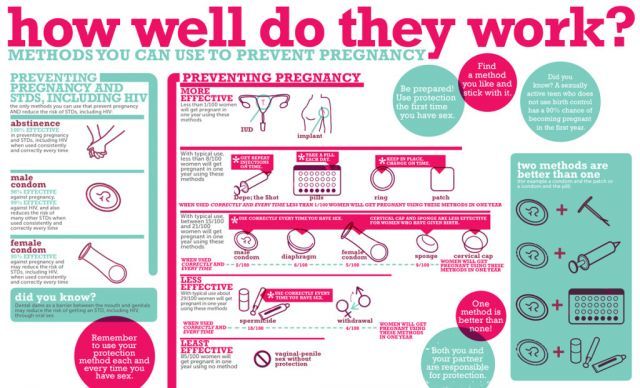
In a broader sense, this pathology can be considered as a hereditary disease in which physiological changes (whether external, such as changes in weather conditions, or internal, such as changes in sleep patterns) often cause stereotypical attacks with migraine symptoms, as defined above. Migraine occurs three times more often in women than in men, with the highest rates in women during active childbearing age, peaking at 27% at age 41 years. To date, there is no evidence that migraine itself affects fertility or the course of pregnancy, but the quality of life in pregnant women with migraine is significantly reduced.
According to some researchers, migraine and tension-type headache in pregnant women are risk factors for the development of arterial hypertension and preterm birth (F. Facchinetti et al., 2009). Pregnancy can provoke the occurrence of diseases accompanied by headache (preeclampsia, thrombosis of the cerebral arteries, compression of the brain as a result of the presence of tumors). Relevant today is the rapid diagnosis of pathology and an adequate choice of therapeutic and obstetric tactics for the treatment of headaches in pregnant women due to the great medical and social significance of the problem.
Relevant today is the rapid diagnosis of pathology and an adequate choice of therapeutic and obstetric tactics for the treatment of headaches in pregnant women due to the great medical and social significance of the problem.
Antiphospholipid syndrome (APS) is defined by the presence of antiphospholipid antibodies (APLA) associated with an increased risk of thrombosis or recurrent spontaneous abortions. The most serious complications can occur in secondary APS against the background of inflammatory systemic autoimmune diseases. Studies conducted in neurological clinics have found that it is migraine, and not headache of all types, that is significantly associated with APLA in patients with systemic autoimmune pathology. However, in patients with systemic lupus erythematosus (SLE), headache is significantly associated with positive APLA titers. Also in this group, cerebral ischemic lesions were significantly more common.
During pregnancy, a woman may experience many health problems. For example, a headache during pregnancy occurs quite often, at different times of the day and for various reasons. Oddly enough, but a woman's frequent headache may be a sign of pregnancy, which she does not yet know about.
For example, a headache during pregnancy occurs quite often, at different times of the day and for various reasons. Oddly enough, but a woman's frequent headache may be a sign of pregnancy, which she does not yet know about.
More than 80% of women sooner or later complain of a headache during pregnancy. Even if a woman was absolutely healthy before pregnancy, then during the bearing of a child she gets a headache. Sometimes it becomes so strong that it is difficult to endure. Headache can occur at any time during pregnancy, but it tends to be most common during the first and third trimesters.
There are factors that can cause headaches during pregnancy.
1. Hormonal changes: The state of the nervous system depends on the woman's hormonal status, that is, on the quantity and quality of hormones produced.
2. Hypotension during pregnancy is associated with the predominance of progesterone over other hormones; the vasodilating effect of progesterone leads to a decrease in blood pressure, cerebral hypoxia and, as a result, to headache.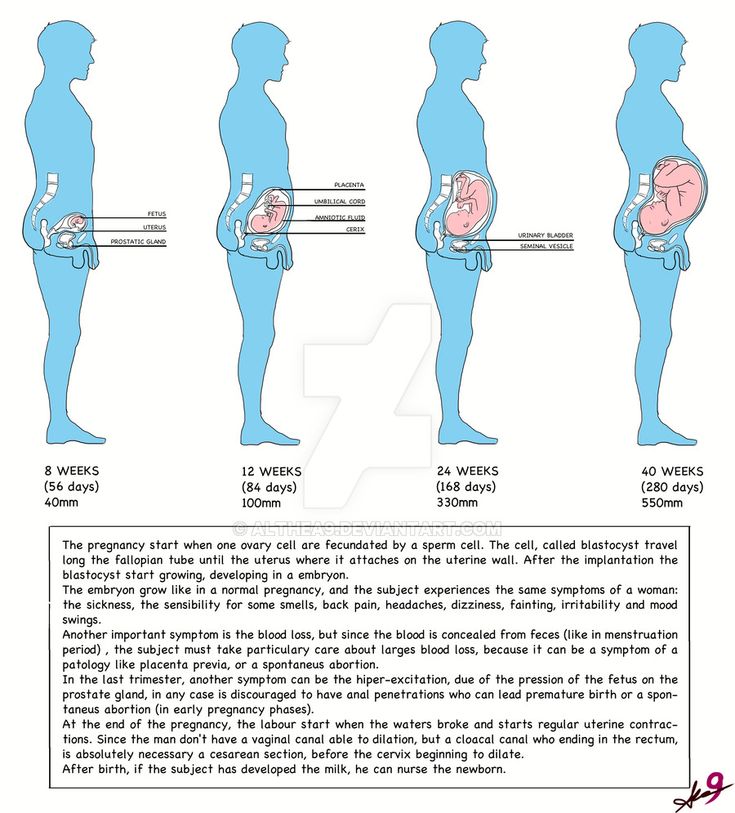
3. Arterial hypertension and preeclampsia cause headache as a result of generalized vasospasm and circulatory disorders in the central nervous system.
4. Nutritional factors - cold food or eating foods containing tyramine and phenylamine (nitrogen compounds that can affect blood vessels) can cause headache attacks; pregnant women who are prone to migraine headache should be careful in consuming the following foods: chocolate, nuts, yogurt, chicken liver, avocados, citrus fruits, bananas, canned and pickled foods, Japanese cuisine, tea, coffee, cola, sausages, red wine, cheese.
5. Hunger headache occurs as a result of a decrease in blood glucose levels and impaired supply of nutrients to the brain.
6. Overweight.
7. Eye strain or prolonged forced stay in the same uncomfortable position.
8. Allergic reactions.
9. Dehydration of the body.
Dehydration of the body.
10. Exacerbation of chronic diseases - spine, especially osteochondrosis, due to increased load during pregnancy, static and dynamic loads often cause headaches; neurocirculatory asthenia as a cause of vasospasm and as a consequence of the appearance of a feeling of heaviness in the head, mood lability and headache.
11. Occurrence of infectious and other diseases such as: meningitis, encephalitis, sinusitis, pyelonephritis, glomerulonephritis and certain ophthalmic pathologies; the characteristic manifestations of this headache are its intensity and the lack of effect of pain medications.
12. Stress factor. Lability of the nervous system, ups and downs in mood, excitement, psycho-emotional stress, depression - all this can cause a headache.
13. Changing weather conditions. During pregnancy, fluctuations in atmospheric pressure can lead to headaches.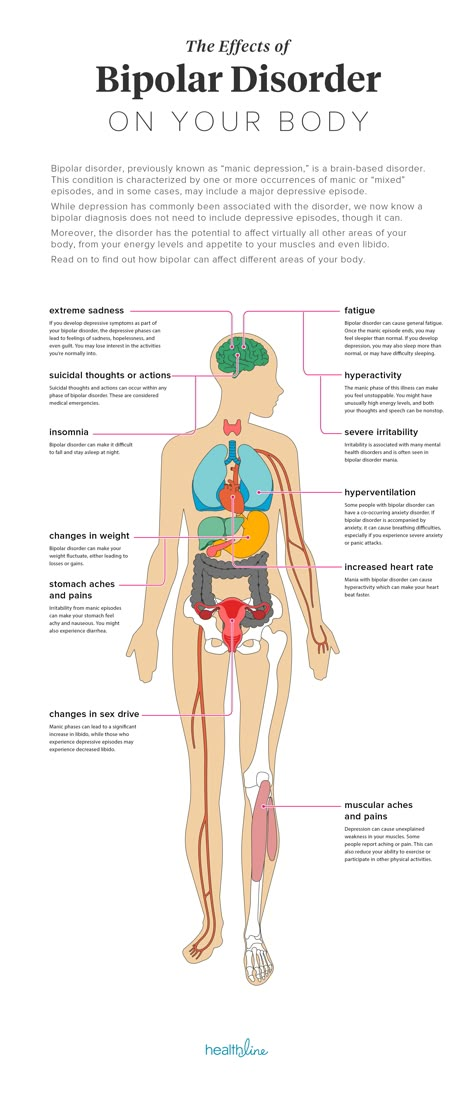
14. Physical stimuli - flickering light, noise, strong odors.
15. Weekend headache. If you sleep longer than usual during the day, the cause of headache can be, for example, venous congestion.
16. Indoor climate: too dry or warm air, a lot of tobacco smoke.
The most common form of headache during pregnancy is migraine, which is accompanied by visual impairment, gastrointestinal disorders, nausea, vomiting, photoreaction, and various vestibular disorders.
In the United States, 28 million people aged 12 and older suffer from migraine, of which 21 million are women aged 25-55. In about 25% of families, one of its members suffers from migraine.
A feature of migraine pain is known to be severe, throbbing pain, predominantly hemicrania, often preceded by aura and marked photoreaction.
It is noteworthy that about 15% of women who have never experienced migraine before, first encounter it with the onset of pregnancy. On the other hand, there are cases when during pregnancy a woman completely stops migraine attacks. In this case, this is due to changes in hormonal status and the absence of ovulation and menstruation.
On the other hand, there are cases when during pregnancy a woman completely stops migraine attacks. In this case, this is due to changes in hormonal status and the absence of ovulation and menstruation.
The occurrence of migraine in women under the influence of hormonal changes is possible throughout the entire menstrual cycle. The positive effect of pregnancy on migraine is observed in 55-90% of women during the gestation period, regardless of the type of migraine. The relief of headache symptoms during pregnancy and their possible worsening after childbirth is likely due to uniformly high and stable estrogen levels during pregnancy and their rapid decline after childbirth.
Another type of headache in pregnancy is tension headache. As a rule, it is characterized by medium intensity, unlike migraine, it often covers the entire head. The pain of tension squeezes the head like a hoop, or causes a pulling sensation; occurs mainly as a result of stress or overexertion.
- If a woman has frequent headaches before pregnancy, the risk of developing preeclampsia increases by 2.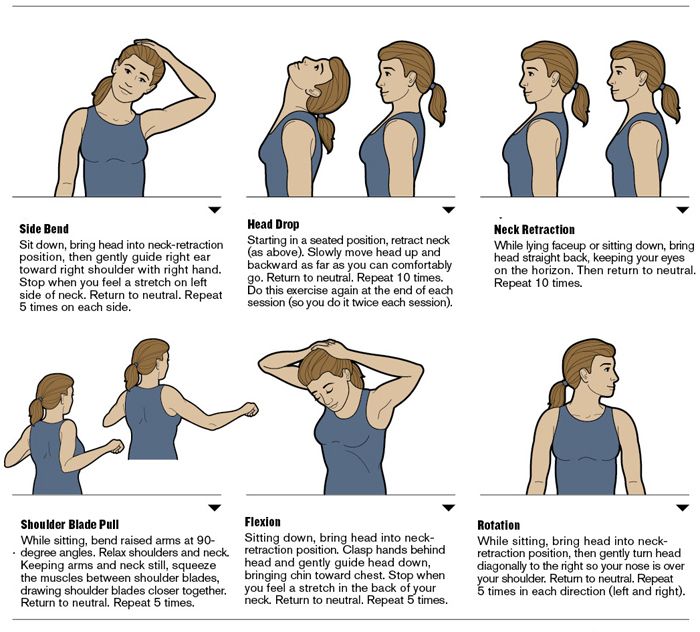 4 times
4 times
- If a woman is diagnosed with migraine before pregnancy, the risk of developing preeclampsia increases by 3.5 times migraine attacks are observed in the early stages - the risk of developing preeclampsia increases by 4 times
Pregnancy headache treatment
A pregnant woman needs medical advice when:
- headache has become almost constant, and has recently changed its character;
- headache in the morning and all day;
- pain is constantly localized in a certain area of the head;
- headache is accompanied by other symptoms - impaired vision, hearing, speech, motor functions, sensitivity, etc.;
- Pain accompanies high or low blood pressure.
Doctor's prescriptions depend on the underlying cause of the headache. Sometimes several factors influence at once, so it is difficult to make an accurate diagnosis. If the headache bothers you regularly, you should contact a neurologist for a specific examination.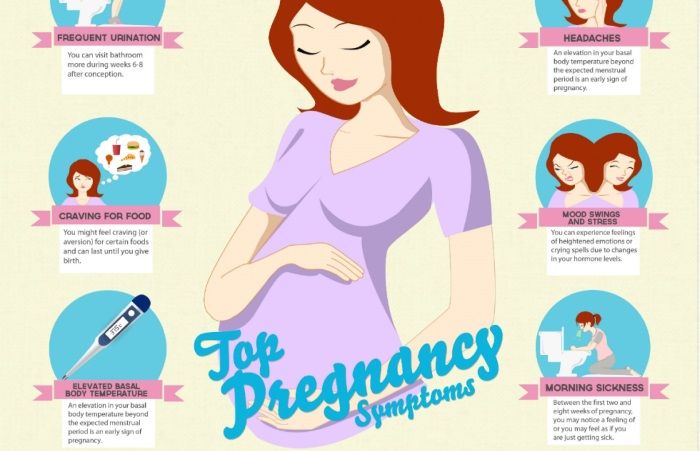
Primary therapy during pregnancy - non-drug (relaxation, sleep, massage). For the treatment of acute migraine attacks, paracetamol (1000 mg) is considered the drug of choice, preferably in the form of suppositories. The table shows data on the possibility of using a number of drugs for the treatment of headache during pregnancy.
The risks associated with the use of aspirin (acetylsalicylic acid) and ibuprofen are considered relatively low if the drugs are taken episodically and removed in the last trimester.
Information on the safety of triptan treatment during pregnancy is available for only a few drugs in this group (sumatriptan, naratriptan and rizatriptan). According to information databases containing information on pregnancy outcomes in women who received these drugs, there were no facts indicating serious risks to the mother and fetus.
With some triptans (sumatriptan, zolmitriptan, naratriptan), there is currently a possibility of a small increase in preterm birth, so triptans are acceptable in severe migraine in exceptional cases. However, data on the use of triptans continues to accumulate and there is not yet sufficient evidence for the safety of the use of triptans during pregnancy.
However, data on the use of triptans continues to accumulate and there is not yet sufficient evidence for the safety of the use of triptans during pregnancy.
Dihydroergotamine and ergotamine tartrate are contraindicated in pregnant women.
Headache definitely cannot be tolerated, it must be correctly diagnosed, differentiated and treated.
The American Academy of Neurology recommends a brain scan for the following cases (MRI only is recommended during pregnancy)
- if, in the presence of a headache, a neurological deficit occurs or any, even short-term, changes in the neurological status;
- if the headache has atypical manifestations and does not fit into the strict framework of establishing a diagnosis of migraine;
- if there is a proven immunodeficiency;
- a sudden severe headache in women for the first time.
- Number:
- Thematic issue "Gynecology, Obstetrics, Reproductology" No.
 4 (24), chest 2016
4 (24), chest 2016
11/20/2022 Obstetrics / gynecology The use of antiseptics in the treatment of vaginal infections in various etiology
Such antiseptics are an alternative to antibiotic therapy in the treatment of bacterial vaginosis due to a wide spectrum of antimicrobial activity, low toxicity and high biomass content of tissues. The Recommendations present the advantages and disadvantages of the main antiseptic products available today, which can be stasted for the treatment of vaginitis in various etiologies. ...
11/20/2022 Obstetrics/gynecology Aspects of treatment of pain syndrome in endometriosis
Pain syndrome in endometriosis is headache, for which patients go to the doctor.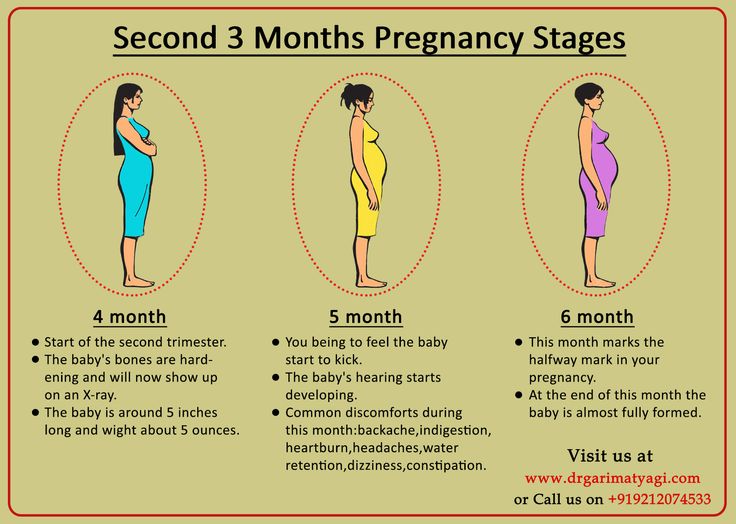 To fight with pain in case of any illness, there may be a combination of chiropractic drugs, however, non-steroidal antispasmodic preparations are most commonly used to relieve pain. ...
To fight with pain in case of any illness, there may be a combination of chiropractic drugs, however, non-steroidal antispasmodic preparations are most commonly used to relieve pain. ...
11/20/2022 Obstetrics/gynecologyAbdominal hysterectomy and post-surgical follow-up: emphasis on diseases Vidkrita abdominal hysterectomy is accompanied by a significant algogenic afferent impulse from the surgical intervention. Also, the search for effective methods to prevent post-operative pain should be relevant. In the article, the analysis of the current approached pre-juvenile (pre-operative) stoppage of non-drug effects for superior pain control. Given the literature, we can show that the total choice of paracetamol, dexketoprofen, nalbuphine, as well as ropivacaine or bupivacaine allows to implement the concept of multimodal analgesia and optimize the process of renewal after surgery.