How do i know if my child has a seizure
Seizures | Boston Children's Hospital
What are the symptoms of a seizure?
A child may have a wide variety of symptoms depending on their type of seizures. Some seizures are easy to recognize through signs like shaking or temporarily losing consciousness. Other seizures are so mild that you might not even recognize them as seizures: They might involve only a visual hallucination, for example, or a moment of very strong emotions. In some cases, seizures have no outward signs at all.
Some signs that your child may be experiencing seizures include:
- staring
- tremors, convulsions, or jerking movements in the arms and legs
- stiffening of the body
- loss of consciousness
- breathing problems
- loss of bowel or bladder control
- falling suddenly for no apparent reason
- not responding to noise or words for short periods of time
- appearing confused or in a haze
- extreme sleepiness and irritability when waking up in the morning
- head nodding
- periods of rapid eye blinking and staring
- vomiting
- changes in vision, speech, or both
Sometimes these symptoms can have a cause other than seizures. Further testing will help doctors confirm suspected seizures or find another condition that is causing the symptoms.
Seizures don’t necessarily harm the brain, but some seizures do cause damage. The side effects of seizures, such as dramatic changes in behavior and personality, may remain even when your child isn’t actually having a seizure. In some cases, seizures are associated with long-term neurological conditions and problems with learning and behavior.
During the seizure itself, children may fall or get injured. It’s important to stay with your child during a seizure. Gently ease the child to the floor if sitting or standing, turn them on their side in case of vomiting and remove any surrounding hard objects. Seizures may leave your child exhausted. Unfortunately, just as troubling as the physical complications, seizures can also cause embarrassment and social isolation.
What are the different types of seizures?
Focal seizures
Focal seizures, formerly called partial seizures, happen when abnormal electrical activity has its onset in a particular area of the brain, known as the “seizure focus. ” They can occur in any lobe of the brain. Before a focal seizure, your child may experience an aura — a strange feeling that involves changes in hearing, vision, or sense of smell.
” They can occur in any lobe of the brain. Before a focal seizure, your child may experience an aura — a strange feeling that involves changes in hearing, vision, or sense of smell.
Focal seizures may last less than a minute and have different symptoms depending on which area of the brain is involved. They usually affect the muscles, causing a variety of abnormal movements that are limited to one muscle group, such as the fingers or the larger muscles in the arms and legs. If the abnormal activity is in the brain’s occipital lobe, your child may experience changes in vision. Your child may experience sweating or nausea or become pale but will not lose consciousness.
Focal seizures may be associated with altered consciousness. Your child can experience a variety of behaviors, such as gagging, lip smacking, running, screaming, crying, or laughing. After the seizure, during what’s called the postictal period, your child may feel tired.
Generalized seizures
Generalized seizures involve both sides of the brain. Children lose consciousness and have a postictal period (a recovery phase) after the seizure. The types of generalized seizures include:
Children lose consciousness and have a postictal period (a recovery phase) after the seizure. The types of generalized seizures include:
- Absence seizures (also called petit mal seizures) involve episodes of staring and an altered state of consciousness. They usually last no longer than 30 seconds but can happen several times a day. Your child’s mouth or face may move, or eyes may blink. Afterward, your child may not recall the seizure and may act as if nothing happened. Absence seizures almost always start between ages 4 and 12 and are sometimes mistaken for a learning or behavioral problem.
- Atonic seizures involve a sudden loss of muscle tone and may cause drop attacks: Your child may fall from a standing position or suddenly drop their head. During the seizure, your child is limp and unresponsive.
- Tonic seizures involve a sudden stiffening of parts of the body or the entire body. Brief tonic seizures may also cause drop attacks.
- Generalized tonic-clonic seizures (also called GTC or grand mal seizures) are characterized by five distinct phases:
- flexing of your child’s body, arms, and legs
- straightening out of their body
- tremors (shakes)
- contraction and relaxing of the muscles (the clonic period)
- a postictal period in which your child may be tired and sleepy, have problems with vision or speech, or have a bad headache or body aches
Myoclonic seizures
Myoclonic seizures involve sudden jerking in a group of muscles. These seizures tend to occur in clusters, happening several times a day or for several days in a row.
These seizures tend to occur in clusters, happening several times a day or for several days in a row.
Infantile spasms
Infantile spasms are a rare type of seizure disorder that occurs in the first year of life. They usually involve brief periods of movement in the neck, trunk, or legs, often when a child is waking up or trying to go to sleep. They usually last only a few seconds, but infants may have hundreds of these seizures a day. This can be a serious problem and can be associated with long-term complications. Spasms may also occur throughout life and can also cause drop attacks.
Status epilepticus
Status epilepticus is a situation in which seizures develop into a prolonged seizure of 30 minutes or longer duration. This condition is a medical emergency and may require hospitalization.
Febrile seizures
Febrile seizures are triggered by fever and usually happen in children between 6 months and 5 years of age. They involve muscle contractions — either mild (such as stiffening of the limbs) or severe (convulsions). Febrile seizures are fairly common, affect about 2 to 5 percent of children in the U.S., and often run in families. Febrile seizures that last less than 15 minutes are called “simple”; those lasting longer are called “complex.”
They involve muscle contractions — either mild (such as stiffening of the limbs) or severe (convulsions). Febrile seizures are fairly common, affect about 2 to 5 percent of children in the U.S., and often run in families. Febrile seizures that last less than 15 minutes are called “simple”; those lasting longer are called “complex.”
What causes seizures in children?
Seizures can take a wide variety of forms, depending in part on what part of the brain has the abnormal electrical activity. Many different diseases and injuries can cause children to have seizures. These include:
- head injuries
- birth trauma
- congenital conditions (conditions that your child is born with)
- poisoning
- fever or infection
- brain tumors
- maternal illness during pregnancy
- heredity
- degenerative brain disorders
- stroke
- metabolic problems and chemical imbalances in the body
- alcohol or drugs
- medications
Often, however, the exact cause of seizures cannot be determined.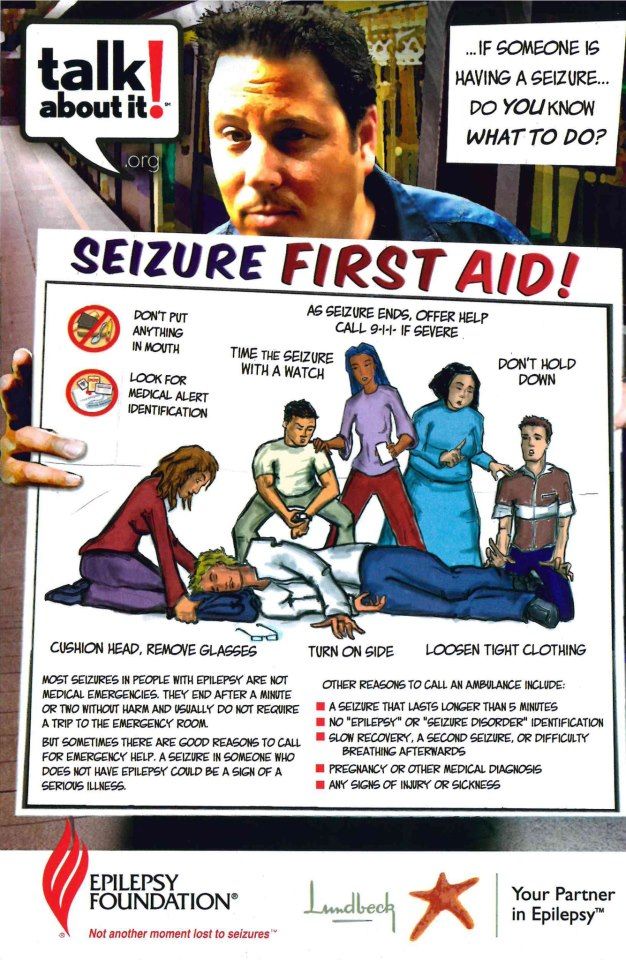
Seizures in children: Signs to look for and what to do
Share:
Approximately 4-5% of all children will experience a seizure at some point during their childhood. About 1% of children are diagnosed with epilepsy, and 1 in 26 people develop this neurological condition during their lifetime.
Given these statistics, it's vital for everyone to know what steps to take if they see a person having a seizure.
Seizures are common, and while a seizure may never happen to you or to a member of your family, it's good for everybody to know what to do in case of a seizure.
What causes seizures in children?
A seizure is an abnormal electrical discharge in the brain. There are many different types of seizures and many different reasons this can occur in a child. Not all seizures are caused by epilepsy. Other causes of seizures in children can include high fever (called febrile seizures), infection or traumatic head injury.
For other kids, when they get very upset and hold their breath, they have an event that looks like a seizure where they pass out or have some stiffening or shaking. This is not considered an epileptic seizure but rather a response to the child holding their breath.
Epileptic seizures occur when sudden electrical discharges in the brain happen without another cause provoking it. Anyone at any age can develop epilepsy, but young children and older adults are at greatest risk. People with epilepsy may identify triggers that increase chance of seizure. Common seizure triggers can include illness, not taking epilepsy medication, stress, flashing lights, certain times of day, dehydration or lack of sleep.
What does a seizure look like in a child?
A seizure can look like lots of different things in a child. The most commonly recognized signs of a seizure are when the body stiffens and shakes. These types of convulsive seizures (generalized tonic-clonic or "grand mal" seizures) can cause a person to fall and injure themselves, bite their tongue or lose control of the bladder or bowel.
Other seizures are not as obvious. Some children may have a seizure but only stare into space, blank out or not respond to a parent – these are sometimes called "absence" or petit mal (staring) seizures. Often when this happens, parents might think their child is not paying attention. This type of seizure can go undiagnosed for months or even years.
Depending on the type of seizure, a child can experience many different symptoms. Common signs of a seizure include:
- Blank staring
- Confused speech
- Loss of consciousness
- Uncontrollable shaking or jerking movements
- Wandering
What to do if a child has a seizure
Seizures can be frightening for a parent or loved one. But when a child has a seizure, it's important to remain calm and to focus on keeping the child safe.
The most important thing, and the hardest, is not to panic. Seizures can be scary to watch, but many times they will stop on their own, and seizures that stop in less than five minutes are not usually dangerous to the child.
Follow the recommendations below to help your child through the seizure safely.
First aid for convulsive seizures
If your child has a convulsion (a seizure where they lose consciousness with stiffening and shaking), follow these steps for seizure first aid:
- Stay calm and stay with your child
- Turn your child on their side
- Make your child as comfortable as possible, cushion the head and remove glasses
- Loosen any tight clothing
- Do not ever put anything in your child's mouth
- Do not try to "stop" the convulsions or restrain your child
- Pay attention to the length of the seizure – when the seizure started and stopped
- Call 911 for any seizure lasting more than 5 minutes, or if the child is injured during the seizure
First aid for absence seizures
When a child experiences an absence or staring seizure, the most important thing to do is to stay with the child to ensure they stay safe. Make sure they are fully conscious and aware before being left on their own.
Make sure they are fully conscious and aware before being left on their own.
If your child has an absence seizure, follow these steps for seizure first aid:
- Stay calm and stay with your child
- Time the seizure
- Don't grab or hold your child
- Explain to others what is happening
- Protect child from any hazards
When to seek emergency help for seizures in children
Many seizures in children will resolve on their own, and in those cases, children often do not require emergency care. However, if your child is experiencing their first seizure, you must take them to the emergency room or to your doctor to determine why it happened.
Call for emergency medical assistance if the seizure:
- Lasts more than 5 minutes
- Is the child's first seizure
- Causes an injury due to a fall
- Causes breathing difficulty
- Is convulsive and changes to a staring seizure and the parent isn't sure if the child is still having a seizure
If your child does not return to full awareness, seek medical assistance or call 911.
Safety precautions for children who have seizures
The biggest risk to children who have seizures is where they occur. If a child is walking down the stairs or is in the bathroom and has a seizure, the child risks falling and hurting themselves.
Most importantly, especially here in Texas in the summertime, if a child is in the water and has a seizure, they can fall under the water and drown. We tell parents to be very careful about watching kids anywhere around water, including lakes, pools, the bathtub or shower.
Take these seizure precautions to ensure your child remains safe.
- Avoid tub baths; showers are safer than baths
- Make sure the bathroom door is not locked
- No swimming without constant adult supervision
- Wear a life jacket at all times when boating or on a jet ski
- No climbing higher than 10 feet including ladders, trees and bunk beds
- Wear a helmet at all times when bike riding and horseback riding
- For children with frequent seizures, avoid bike riding on streets
- No cooking over an open stove (use microwave instead) or using an iron
- Teenagers with uncontrolled seizures shouldn't drive, including ATVs, mini-motor cycles, 4-wheelers
- Do not allow the handling of firearms
As a parent, it will be helpful to develop a plan and to share your plan with others to help keep your child safe during a seizure. Talk to your child's school or anyone who may be in contact with your child about seizure first aid and safety.
Talk to your child's school or anyone who may be in contact with your child about seizure first aid and safety.
About 4-5% of children will have a seizure at some point during childhood. @Childrens shares signs of a seizure and how to keep your child safe during a seizure.
Click to Tweet
Learn more
Designated as a Level 4 Epilepsy Center by the National Association of Epilepsy Centers, Children's Medical Center Dallas provides the highest level of treatment for the most complex cases of pediatric epilepsy, with additional advanced epilepsy treatment options available at our Level 3 Epilepsy Center in Plano. Learn more about our program and services.
Children’s Health Family Newsletter
Get health tips and parenting advice from Children’s Health experts sent straight to your inbox twice a month. Sign up now.
when you don't know your child is sick
Do you think that epilepsy is convulsions, unconsciousness and foaming at the mouth?
In fact, this is not always the case. Specialists of the International Antiepileptic League distinguish more than 30 types of epileptic seizures , each of which manifests itself in different ways. Because of this, the disease can go unnoticed until it leads to disturbances in the functioning of the body and the development of the child.
Specialists of the International Antiepileptic League distinguish more than 30 types of epileptic seizures , each of which manifests itself in different ways. Because of this, the disease can go unnoticed until it leads to disturbances in the functioning of the body and the development of the child.
Unreasonable mood swings, restless sleep, headaches are all reasons to see a neurologist, according to the recommendations of the American Epilepsy Foundation. What else can hide epileptic seizures? When is it time to sound the alarm? What you need to know about the disease in order to help your child in time?
- What is an epileptic attack
- What does an attack of a child look like
- with what epilepsy
- attacks that occur at night
- How to treat epilepsy attacks
- Is it possible to prevent epilepsy attacks
and why it happens
Neurologists compare an epileptic seizure to an electrical storm in the brain.
The human nervous system consists of many cells (neurons) interconnected by nerve pathways. Through them, signals in the form of small electrical impulses come from the sense organs to the brain and to different parts of the body. Thanks to this, a person feels heat and cold, the taste of food, sees the world around him and can move around. But sometimes neurons in a certain part of the brain fail. A sharp and strong electrical discharge occurs in them, similar to a lightning strike. First, it spreads to neighboring nerve cells and gradually covers one or even two hemispheres of the brain, so it “shorts” the entire nervous system. This is what an epileptic seizure is.
According to the American Epilepsy Foundation, the main causes of such a seizure can be:
- head trauma;
- infections;
- congenital genetic disorders;
- birth injuries.
All this can lead to the development of epilepsy - a chronic disease in which attacks occur constantly, with a certain frequency. The main danger is that during each attack a certain number of neurons die. They are not restored, therefore, it is possible to preserve the health of the child only with timely diagnosis and proper treatment.
The main danger is that during each attack a certain number of neurons die. They are not restored, therefore, it is possible to preserve the health of the child only with timely diagnosis and proper treatment.
One seizure is not always epilepsy. In some cases, it may be the body's reaction to a high temperature or an allergy. The World Health Organization estimates that this happens in about 10% of people. In any case, to be sure of the health of your child, you should contact a neurologist and undergo an examination.
The World Anti-Epileptic League, as the main method for diagnosing epilepsy, highlights - electroencephalography. It records the electrical activity of the brain and allows you to detect even small seizures that do not have external manifestations. Epiactivity is not always easy to detect. It can manifest itself at a specific time of day or under certain circumstances, so there are various types of EEG with a transition to sleep and even multi-day monitoring. It is especially important that the study is conducted not for 15 minutes, but for at least several hours and fixes the state of the child in a dream. Against the background of a general relaxation of the nervous system during this period, any bursts of electrical activity become more noticeable.
It is especially important that the study is conducted not for 15 minutes, but for at least several hours and fixes the state of the child in a dream. Against the background of a general relaxation of the nervous system during this period, any bursts of electrical activity become more noticeable.
What does an epileptic seizure look like in a child? It all depends on the location of the accumulation of pathological neurons (epileptic focus) and the number of hemispheres subject to an attack.
Neurologists Say Parents Need to Know Epilepsy Foundation of America
It is especially important to pay attention to all of the symptoms of an epileptic seizure. Your description of what an epileptic seizure looks like in a child will help the neurologist accurately determine the form of the disease, and therefore choose the right treatment. If the first episode occurred, it is necessary to record the time and all its features:
- what your child was doing just before the accident;
- what happened to him during the attack;
- how the child felt immediately after the incident.
The doctor needs to be told if the child is taking any medications when he or she was vaccinated, and if there are any allergies. It is important to remember if similar cases occurred with one of the relatives. All this will allow you to make an accurate diagnosis.
Which epileptic seizures can occur in children (according to World Anti-Epileptic League )
Seizures that affect both hemispheres of the brain are called generalized. They can be:
- Tonic-clonic. There is a tension of all muscles (in Greek, tonos) and their rapid rhythmic contractions (clonos). As a result of this, convulsions are observed, arms and legs are involuntarily bent. A person loses consciousness for several minutes, and when he comes to, he does not remember what happened to him, feels tired and drowsy.
- Tonic. These are convulsive seizures of epilepsy without loss of consciousness, accompanied only by muscle tension.

- Atonic seizures. They pass without loss of consciousness and appear as a complete relaxation of all muscles, which lasts only 15-20 seconds.
- Myoclonic and clonic seizures of epilepsy. Appears as repetitive twitching of limbs or whole body.
- Absences. These are small seizures of epilepsy with loss of consciousness, which are more like daydreaming or thoughtfulness than illness. At the same time, the child does not have convulsions, he simply disconnects from the outside world for a few seconds, stares intently at one point, does not hear and does not react to anything. The greatest danger of such attacks is that they are difficult to notice. At the same time, children with absence epilepsy may experience several dozen such episodes daily.
There is a group of epileptic seizures that occur only in a certain part of the brain and do not spread to 2 hemispheres. They are called focal or partial. The symptoms of each of them depend on where exactly the epileptic focus is located. So, an attack of temporal lobe epilepsy begins with the fact that the child freezes and does not respond to external stimuli. Then he begins to automatically repeat a certain sequence of actions, for example, unbuttoning and fastening the buttons on clothes. After a few minutes, he stops, feels disoriented, and may not know where he is.
The symptoms of each of them depend on where exactly the epileptic focus is located. So, an attack of temporal lobe epilepsy begins with the fact that the child freezes and does not respond to external stimuli. Then he begins to automatically repeat a certain sequence of actions, for example, unbuttoning and fastening the buttons on clothes. After a few minutes, he stops, feels disoriented, and may not know where he is.
Quite often partial seizures of epilepsy are preceded by an aura - certain physical or psychological sensations. They also provide information about the location of the epileptic focus. With temporal lobe epilepsy, a child may experience auditory hallucinations, ringing in the ears, a certain smell or taste in the mouth. If the focus is located in the frontal lobe, the child complains of shortness of breath or intense thirst, if in the back of the head - the appearance of spots or lights before the eyes.
Seizures similar to epilepsy: what can be confused with the disease
In most cases, an epileptic attack can be confused with hysteria, which is a mental disorder and not a disease of the nervous system. So says Professor Antonio Russi, Europe's top epileptologist, who sees patients at the Teknon clinic in Barcelona (Spain). Hysteria also manifests itself in the form of mood swings, speech and vision disorders, loss of consciousness, paralysis of the limbs, convulsive seizures.
So says Professor Antonio Russi, Europe's top epileptologist, who sees patients at the Teknon clinic in Barcelona (Spain). Hysteria also manifests itself in the form of mood swings, speech and vision disorders, loss of consciousness, paralysis of the limbs, convulsive seizures.
Spain, Barcelona
352 reviews
TrustScore
All reviews have been verified
- Bookimed patients in Teknon are received by Prof. Antonio Russi. This is an epileptologist with 35 years of experience. He specializes in the diagnosis of rare and most complex cases, therapy and surgery of epilepsy at any age. 95 of the doctor's patients out of 100 successfully control epileptic seizures after treatment. In 30 patients out of 100, it does not confirm the form of epilepsy that was determined at home. After additional tests, only 1 correctly prescribed medicine helps them to completely get rid of seizures.
- Only with Antonio Russi you will undergo an extended examination - electroencephalography of the brain during sleep and wakefulness for several days. During this period, the professor prescribes various antiepileptic drugs and evaluates how they affect the seizures. Such diagnostics allows you to accurately determine the location of the epileptic focus and select an effective treatment.
- In addition, Professor Russi prescribes pharmacogenetic testing. This is a study of the genetic characteristics of a person, which allows you to determine the reaction of his body to prescribed medications.
- The duration of a comprehensive examination for epilepsy is 7 days.
Read more
| Stereotactic operations | $26896 - $69929 |
| Vagus nerve stimulation | $48412 - $50564 |
According to the American Epilepsy Foundation, the main difference between seizures in hysteria is the preservation of consciousness. The child always remembers what happened to him during the attack. He also never gets hurt. If during an epileptic attack a person can fall right where he was standing, in hysteria he will do it carefully so as not to hit. Clonic seizures in hysteria are not just twitches of the body or limbs. Usually a person performs more meaningful actions, for example, tears his clothes.
The child always remembers what happened to him during the attack. He also never gets hurt. If during an epileptic attack a person can fall right where he was standing, in hysteria he will do it carefully so as not to hit. Clonic seizures in hysteria are not just twitches of the body or limbs. Usually a person performs more meaningful actions, for example, tears his clothes.
Hysteria, like epilepsy, requires appropriate treatment, therefore, at the first unusual manifestations, it is necessary to consult a neurologist.
When an epileptic seizure is only a symptom
Seizures similar to epilepsy can occur in a child with neoplasms in the brain (for example, a cyst or tumor) as a response to a head injury. Sometimes they are caused by a metabolic disorder, as a result of which the brain does not receive the trace elements necessary for its normal functioning.
This type of seizure is called symptomatic epilepsy or episyndrome. At the same time, in order to select the correct treatment, the doctor must not only determine where the epileptic focus is located, but also establish the primary disease that led to convulsions.
What Happens at Night: Epilepsy Seizures You May Not Know About
According to the World League Against Epilepsy, 12% of patients diagnosed with this condition have nighttime seizures. For some, the disease manifests itself exclusively in a dream. This greatly complicates the examination: doctors can unsuccessfully search for the cause of a child’s poor health for months.
How to detect a nocturnal epileptic seizure?
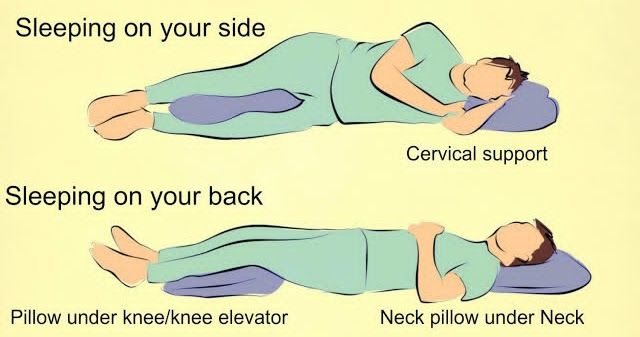
According to Medical News Today, indirect signs that a child had an epileptic seizure in a dream can be:
- night headache;
- bitten tongue or lips;
- saliva and blood stains on pillow;
- fatigue after sleep;
- muscle pain.
How to treat epilepsy attacks
Neurologists say that the main condition for effective treatment of epilepsy is accurate diagnosis. The doctor needs to very accurately determine the type of attack, the location of the epileptic focus in the brain and the cause of the disease. Only on the basis of these data will he be able to choose the method that will be the most effective.
Only on the basis of these data will he be able to choose the method that will be the most effective.
According to European protocols for the diagnosis of epilepsy, the examination of a child must necessarily include long-term electroencephalography. In addition to it, the doctor may prescribe magnetic resonance imaging (MRI) or computed tomography (CT), complete blood count, genetic testing.
For the treatment of epileptic seizures, neurologists use 2 main methods - medication and surgery, according to medical protocols. Most patients (more than 70%) can get rid of seizures with 1 or 2 properly selected drugs (according to the World Health Organization). In this case, it is especially important to adhere to all the recommendations of the doctor and the established schedule for taking medications. In case of violation of the prescribed regimen, seizures may return.
Doctors rarely use surgical treatment of epilepsy (in 25% of cases, according to WHO). The neurologist prescribes it only after making sure that no drugs and their combinations can control epilepsy.
Epilepsy: can it be prevented
It is impossible to completely eliminate the risk of developing the disease, since it is often genetic. However, compliance with all precautions and attention to the health of your child will minimize the possibility of an epileptic seizure.
In order to prevent the development of epilepsy in a child, The World Health Organization (WHO) advises to adhere to these basic rules:
Neurologist for parents about children
What is common between a child who is afraid to go to the blackboard and an excellent student who suffers from skin allergies and tics?
Between an impulsive child who is rude to teachers and hits classmates, and a fearful and insecure C student with headaches and impaired attention?
Between a restless, irritable, nervous child for any reason and his desk neighbor suffering from sleep disorders and enuresis, who is not interested in anything, who is not affected by either shouts or deuces?
Many of these manifestations of behavior in children are based on violations of the mechanisms of development of the nervous system . ..
..
What explains the disturbances in the baby's nervous activity if there are no visible changes in the brain?
The fact is that outwardly correctly formed brain is not yet a guarantee of its normal operation. Having experienced unfavorable influences in a critical period (intrauterine, during childbirth or in a newborn), the brain "goes out of the schedule" of its development into the most critical phase. The formation of the most important functions does not have time to "fit" into the optimal age period allotted for this, into a kind of peak in the plasticity of the nervous system, and then, in addition to what has already been said, the baby may develop irreversible conditions ....
But if everything that happens in childhood were irreversible, then childhood diseases of the nervous system would be incurable...
And this is not so!
How to treat brain diseases? Our pediatric neurologists and psychoneurologists will answer this.
A child psychoneurologist, unlike an adult neuropathologist, has to deal with almost all the pathologies inherent in the body:
- damage to the nervous system in utero and during childbirth as a result of various adverse factors
- disorders of motor development (from tempo delays in the formation of initial motor skills to paresis and paralysis)
- birth and domestic traumatic brain injury and their consequences
- epilepsy, other convulsive conditions
- sleep disorders, including paroxysmal
- cerebrovascular accidents (strokes) in both acute and chronic stages
- congenital and acquired hydrocephalus
- "rejuvenated" multiple sclerosis, brain tumors and other progressive diseases of the nervous system
- pains of various origins
- hereditary neuromuscular diseases and other genetic diseases affecting the nervous system
- behavioral disorders, adaptation problems, neurotic reactions and habits (tics, stuttering, urinary incontinence, obsessions, fears, etc.
 )
) - diseases of the mental sphere (early childhood schizophrenia, autism, mental retardation - intellectual deficiency of varying severity)
- disorders "accompanying" chronic somatic diseases
and many other disorders, except perhaps a very small range of genetic conditions, age-dependent, but they also tend to rejuvenate ...
Perinatal damage to the nervous system is a collective diagnosis that implies a violation of the function or structure of the brain (encephalopathy) and spinal cord of various origins that occurs in the perinatal period (from the 28th week of intrauterine development, including birth, to the period corresponding to the first week of a child's life with processes characteristic of him adaptation of the newborn to environmental conditions). Causes that affect the occurrence of symptoms of PPNS can be:
- intrauterine infections (rubella, herpes, cytomegalovirus, syphilis, etc.)
- exacerbations of chronic diseases of the future mother with adverse changes in metabolism
- intoxication
- exposure to various types of radiation
- genetic conditioning
- long dry period
- absence or weak intensity of contractions and inevitable in these cases stimulation of labor activity
- insufficient opening of the birth canal
- rapid labor
- use of manual birthing techniques
- cesarean section
- fetal entanglement with umbilical cord
- large body weight and size of the fetus
- neuroinfections
- injuries
The consequence of these causes is a violation of breathing and circulation (asphyxia, hypoxia), energy deficiency of the heart and brain, insufficiency of individual organs or functional systems (multiple organ failure), leading in some cases to irreversible phenomena.
Birth trauma of newborns is damage to the organs and tissues of the fetus that occurs during childbirth as a result of a discrepancy between the birth expelling forces (contractions, attempts) and the elasticity of the tissues of the fetus. Predisposing causes include: toxicosis of pregnant women, cardiovascular diseases of the mother, infections during pregnancy, metabolic disorders, prematurity and overmaturity, etc. Prenatal asphyxia (hypoxia) of the fetus plays a special role in the occurrence of birth trauma.
Sometimes injuries are accompanied by intracranial hemorrhages, cerebral edema with increased intracranial pressure, with the development of hydrocephalus (dropsy of the brain), fractures of the clavicles and humerus, spine, injuries of the facial nerve and paralysis of the brachial plexus, etc.
Traumatic brain injury (including domestic). Head injuries can vary greatly in severity, from minor bruising of the soft tissues of the head to severe damage to the skull and brain. In young children, even sometimes outwardly “harmless” falls from a small height can hide fractures of the skull, its internal platinum with damage to brain tissue. Mechanical trauma to the skull leads to compression of the brain tissue, tension and displacement of its layers, and a temporary sharp increase in intracranial pressure. The displacement of the medulla may be accompanied by rupture of the brain tissue and blood vessels (hemorrhage), brain contusion. Usually, these mechanical disturbances are accompanied by complex changes in the brain and their consequences.
In young children, even sometimes outwardly “harmless” falls from a small height can hide fractures of the skull, its internal platinum with damage to brain tissue. Mechanical trauma to the skull leads to compression of the brain tissue, tension and displacement of its layers, and a temporary sharp increase in intracranial pressure. The displacement of the medulla may be accompanied by rupture of the brain tissue and blood vessels (hemorrhage), brain contusion. Usually, these mechanical disturbances are accompanied by complex changes in the brain and their consequences.
Epilepsy is a chronic neuropsychiatric disease characterized by a tendency to recurrent sudden seizures. Seizures are of various types (convulsive and non-convulsive), but any of them is based on a very high electrical activity of nerve cells in the brain.
Epilepsy has been known since ancient times. Epileptic seizures were noted in many prominent people, such as the apostle Paul and Buddha, Julius Caesar and Napoleon, Handel and Dante, Van Gogh and Nobel.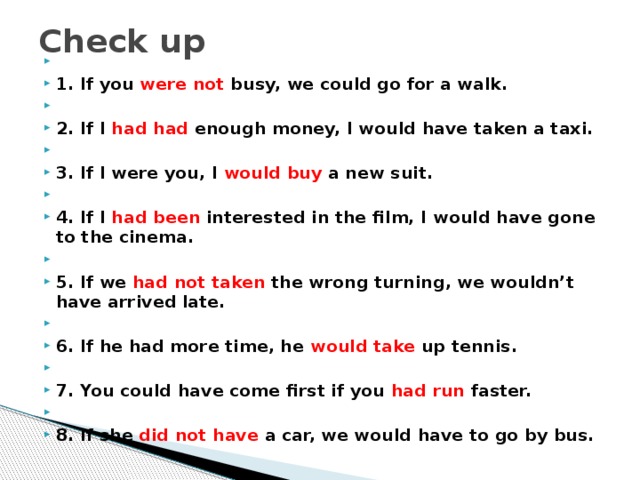 Its prevalence reaches 15-20 cases per 1000 people. In addition, approximately one in 20 children had seizures at least once with a rise in temperature. There are epilepsy as an independent disease, epileptic syndromes (with various diseases of the brain) and epileptic reactions to sudden external stimuli (poisoning, intoxication, environmental influences, trauma, stress, etc.)
Its prevalence reaches 15-20 cases per 1000 people. In addition, approximately one in 20 children had seizures at least once with a rise in temperature. There are epilepsy as an independent disease, epileptic syndromes (with various diseases of the brain) and epileptic reactions to sudden external stimuli (poisoning, intoxication, environmental influences, trauma, stress, etc.)
Paroxysmal sleep disorders (parasomnias). Paroxysmal sleep disorders have been known since antiquity and are described in the writings of Hippocrates and Aristotle. Some of them are similar to epilepsy, both in terms of manifestations and diagnostic characteristics. To date, a large number of independent syndromes that occur during sleep are known, which are associated with the peculiarities of the development of the child's nervous system (including general medical, neurological, emotional, social problems, environmental factors). These are such as enuresis, night terrors and nightmares, vegetative disorders (excessive sweating, respiratory rate disorders, asthma attacks and palpitations), bruxism (teeth grinding), excessive motor activity during sleep, startling, sleepwalking, sleepwalking, paroxysmal night pains, convulsions in limbs, disturbed awakening after sleep.
Along with these sleep disorders, there are also sleep-wake rhythm disturbances associated with sleep disorders (dyssomnias), as well as sleep disorders with concomitant diseases (ARVI, rhinitis, various pain syndromes, teething period in children, etc.), sleep disorders can also be observed in psychiatric diseases, etc.
Cerebral circulation disorders in children. Children may develop all types of cerebral circulation disorders, starting with their initial manifestations (in the form of headaches, dizziness, mental disorders, intellectual retardation, etc.) and ending with strokes. Blood diseases, brain tumors, improper development of the walls of the cerebral vessels themselves (aneurysms), diabetes mellitus, alcohol and drug use can lead to vascular diseases of the brain, both in adults and in children. The probability of their development is quite high in case of heart disease, cardiac arrhythmias, heart defects and inflammatory diseases of the heart muscle. Inflammatory diseases of the vessels of the brain - vasculitis - can also be the cause of impaired cerebral circulation. In children, vasculitis is more common with rheumatism. Cerebral circulation disorders of the brain and spinal cord in children can also be long-term consequences of a birth injury of the spine.
In children, vasculitis is more common with rheumatism. Cerebral circulation disorders of the brain and spinal cord in children can also be long-term consequences of a birth injury of the spine.
A nervous child is an irritable, naughty child who does not know how and does not want to control himself. Moreover, almost 90% of completely different children fall under this parental “diagnosis”. The birth of a nervous child may depend on the fact that the expectant mother was nervous, suffered from toxicosis, and had a difficult birth. But even in the case when there is none of the above reasons, and your child was born and grows in favorable conditions, congenital insufficiency of certain brain structures can become the cause of nervousness. Under the concept of "nervous child" from the point of view of medicine can hide both a child with increased emotional sensitivity, and with anomalies in the development of character, neurosis, with organic disorders of the brain.
A child also becomes nervous when he does not get enough sleep, watches TV all day, listens to horror films when the house is very noisy and crowded, the family quarrels when he is the only child in the family, and adults who love him fulfill his every whim or desire, thinking that in this is true love.
If something worries you in the behavior of a nervous child, be sure to consult a doctor: a neurologist, psychoneurologist, clinical psychologist. In most cases, we are not talking about serious mental disorders, but about ordinary ailments, which, if they are “captured” in time, are quite easy to correct. Specialists will be able to find out the cause using various types of examinations - ultrasound (ultrasound), electroencephalography (EEG), laboratory tests, neuropsychological and pathopsychological examinations. The treatment of a nervous child is complex - medication (psychopharmacotherapy), psychosocial treatment (aimed at correcting the microsocial environment surrounding the child, at forming support and helping relationships), psychotherapy (aimed at correcting behavior),
Neurotic reactions are psychogenic disorders that appear due to quarrels, conflicts, "biting" feelings of loneliness, any fears. A neurotic reaction easily arises from an experienced sad or terrible event for a person.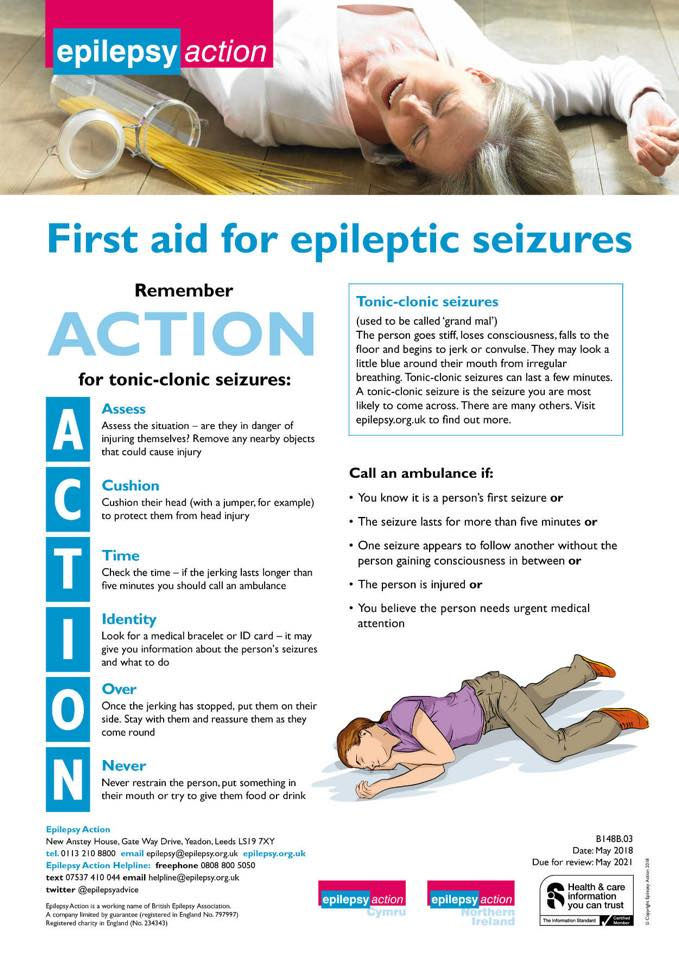 The intense rhythm of modern life and school loads are also pushing towards them, and more and more often they are found in the most vulnerable - in our children. Of course, the life of a little man is not without problems. But the problems of children are different. It's one thing when they fit into the framework of age-related developmental norms. But some baby problems can only be solved by specialists, such as tics, stuttering, enuresis, attention deficit hyperactivity disorder, finger and tongue sucking, body and head rocking (yactation), masturbation (masturbation) that occurred in prepubertal age, nail biting (onychophagia) hair pulling (trichotillomania), etc.
The intense rhythm of modern life and school loads are also pushing towards them, and more and more often they are found in the most vulnerable - in our children. Of course, the life of a little man is not without problems. But the problems of children are different. It's one thing when they fit into the framework of age-related developmental norms. But some baby problems can only be solved by specialists, such as tics, stuttering, enuresis, attention deficit hyperactivity disorder, finger and tongue sucking, body and head rocking (yactation), masturbation (masturbation) that occurred in prepubertal age, nail biting (onychophagia) hair pulling (trichotillomania), etc.
With mental retardation, assistance is provided by a child neurologist, psychoneurologist, psychiatrist. Parents do not always realize the desirability of early contacting these specialists, although they can help with the child's problems, including behavioral and emotional ones. Mandatory consultation of an endocrinologist, cardiologist, because. the reasons for the delay may lie in neurological, hormonal disorders, diseases of the cardiovascular system. The child may need to conduct additional studies - MRI (magnetic resonance imaging), computed tomography (CT), ultrasound (ultrasound), EEG (electroencephalography). For a more accurate understanding of the causes of the origin of the child's problems.
the reasons for the delay may lie in neurological, hormonal disorders, diseases of the cardiovascular system. The child may need to conduct additional studies - MRI (magnetic resonance imaging), computed tomography (CT), ultrasound (ultrasound), EEG (electroencephalography). For a more accurate understanding of the causes of the origin of the child's problems.
According to indications, medications can be prescribed that improve memory and attention, reduce excitability and develop perseverance. Children, unlike adults, have more reserves and capabilities of the body. With timely assistance, the phenomena of mental retardation are noticeably smoothed out in the future, there is a good adaptation in everyday life.
What is Attention Deficit Hyperactivity Disorder (ADHD)?
"Hyperactivity" is restlessness, inattention and impulsivity, frequent nocturnal awakenings, occurs most often in childhood and affects the general atmosphere in your family and the social future of your child. This syndrome is a "hodgepodge" of various diseases, their cause must be found out.
This syndrome is a "hodgepodge" of various diseases, their cause must be found out.
Early organic brain damage in the perinatal period (for example, complications during pregnancy, birth trauma, hypoxia in childbirth), as well as genetic and socio-psychological factors (family conflicts, defects in education, acute and chronic stresses that reduce the resistance of the nervous system to external and internal influences).
"Disaster children", "difficult children" - this is how children with ADHD are called. Indeed, they cause so much trouble to their parents, they constantly get into some kind of unpleasant situations, since they often do not have a developed sense of self-preservation and control over behavior. At school, they cannot learn the educational material, be at the desk during the entire lesson. At the same time, such children most often do not show mental retardation or pronounced neurological disorders, although increased excitability can also manifest itself in various early lesions of the nervous system (head trauma, neuroinfections, etc. ). Such children require an individual approach in the educational process, so the recommendations of the teacher are important. Do not consider such children aggressive and dangerous to other children. With age, in the process of social interaction, the phenomena of hyperactivity become less pronounced. Sometimes such people become leaders, have increased efficiency.
). Such children require an individual approach in the educational process, so the recommendations of the teacher are important. Do not consider such children aggressive and dangerous to other children. With age, in the process of social interaction, the phenomena of hyperactivity become less pronounced. Sometimes such people become leaders, have increased efficiency.
With ADHD, a neurologist, a neuropsychiatrist, a psychiatrist, a medical psychologist (clinical psychologist), and even better - all together can help, because then doctors will have the opportunity to discuss a comprehensive treatment regimen that will be most effective.
So, it is necessary to find out what the state of physical health is, whether the characteristics of the child’s behavior are the result of organic disorders in the brain, ultrasound (ultrasound), EEG (electroencephalography), MRI (magnetic resonance imaging), consultation with a neurologist.
It is important to assess the state of the cardiovascular system (consult a therapist, a cardiologist), determine the level of hormones and get advice from an endocrinologist.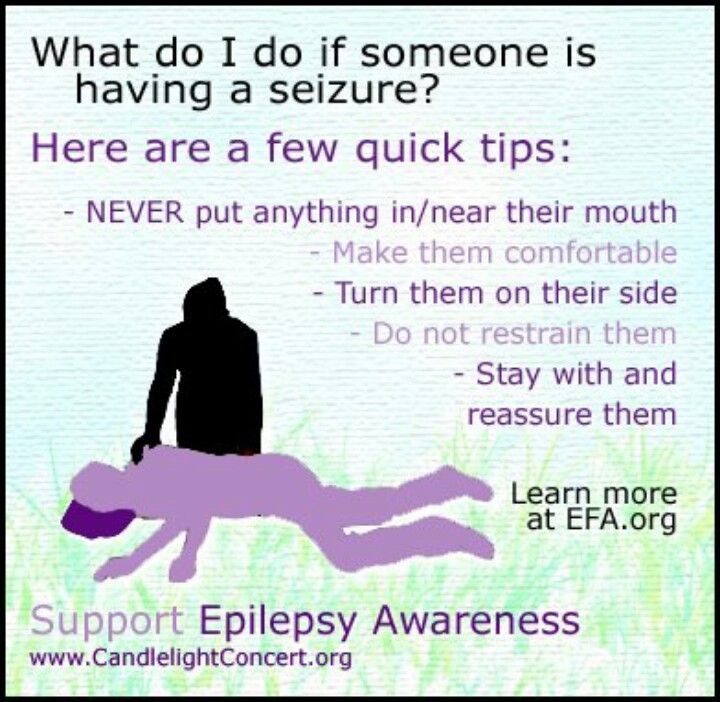
Treatment is complex - biological, psychological and social. Drug treatment (psychopharmacotherapy) is aimed at reducing motor anxiety, improving the functions of cognition of the surrounding world, and normalizing sleep.
Enuresis
Enuresis (second name - urinary incontinence) - the inability of a person to "endure" to the toilet, a constant struggle with wet sheets.
Potty training is one of the stages in the overall mental and physical development of the child. The age at which it is already possible to talk about enuresis in a child should be at least 4-5 years.
The causes of enuresis are very different - mental trauma, anomalies in the development of the urinary tract, underdevelopment of the lumbosacral spine, improper daily routine, poor nutrition, endocrine disorders, delayed maturation of the nervous system.
Enuresis can be both an independent disease and a manifestation of any other disease. There are enuresis day and night, primary and secondary. In primary enuresis, there is a lack of previous control over the emptying of the bladder. Secondary enuresis is said to be in the event that a person controlled the process of urination for at least 6 months, and then again began to urinate in his pants or bed, due to the influence of urological, neurological, mental or endocrine diseases.
In primary enuresis, there is a lack of previous control over the emptying of the bladder. Secondary enuresis is said to be in the event that a person controlled the process of urination for at least 6 months, and then again began to urinate in his pants or bed, due to the influence of urological, neurological, mental or endocrine diseases.
With enuresis, there are persistent sleep disturbances, problems with falling asleep and waking up, excessively deep sleep, night terrors, sleep-talking and sleepwalking. If such a child is forcibly awakened, then orientation disorder with motor excitation and fears can be observed.
Who can help with enuresis?
With enuresis, a psychoneurologist will help. Additionally, you need to be examined to exclude a malformation of the urinary tract and spine, diabetes mellitus, diseases of the central nervous system. Consultations of a pediatrician, endocrinologist, laboratory tests, ultrasound examination of the kidneys and bladder (ultrasound), EEG (electroencephalography) will be needed.
Treatment of enuresis is complex. Drug treatment (psychopharmacotherapy) is aimed at eliminating anxiety and fears, stabilizing mood. Psychotherapy - to eliminate emotional disorders and change behavior, in particular, compliance with the daily routine, food and drink regimen - fluid restriction, eating foods with only a low fluid content. Other non-drug methods of influence are acupuncture, manual therapy.
HEADACHE IN CHILDREN
Children often complain of headaches. For the most part, it is, as doctors say, benign in nature and only in rare cases become a manifestation of a serious general or neurological disease. Therefore, it is important not to brush aside the timid complaint of a child, who sometimes still cannot clearly articulate what hurts him. Parental anxiety, prompting them to go to the doctor to identify the causes of the child's ill health, is understandable and justified.
Why do children have headaches?
Acute headache in children is primarily one of the main symptoms of acute neuroinfectious diseases, as well as paroxysmal conditions, while chronic headache is a frequent manifestation of vegetative dystonia and neurosis.
The most common tension headache. It is based on a painful contraction of the muscles of the soft tissues of the head (scalp) or the cervico-occipital region. Tension headache is usually associated with emotional stress. What is the child's stress? Do not count them. This, for example, preparing for a test or exams, the loss of a beloved pet, a quarrel with a friend ... An overweight child who does not want to undress in the presence of classmates often complains of a headache before physical education classes. The duration of such pain usually does not exceed 1 - 2 hours. Of course, the doctor cannot cancel the control exams at school, but parents, teachers, and the doctor must work hard to eliminate and mitigate stressful effects. The doctor usually prescribes prophylactic drugs.
The most characteristic type of vascular headache is MIGRAINE. This disease is associated with genetically determined changes in the cerebral vessels. Migraine attacks in children, as in adults, provoke physical and mental overload, emotional stress, changes in atmospheric pressure, weather conditions, allergic reactions: for example, cheese and chocolate loved by a child can cause a headache.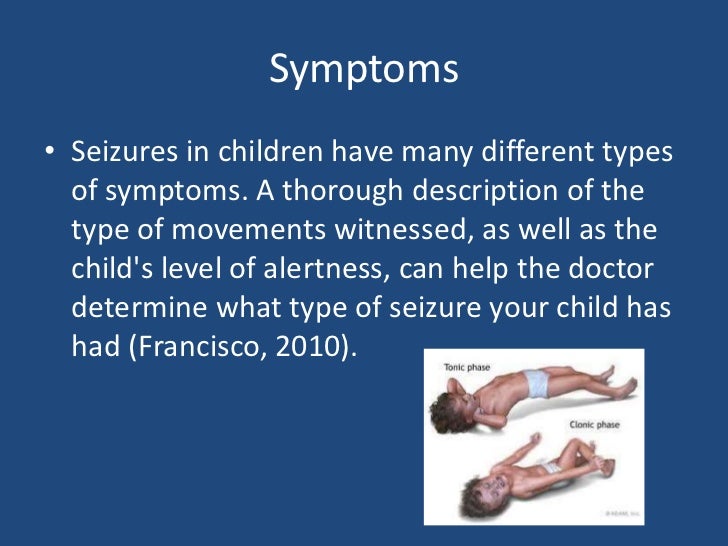
More often, children have a simple form of migraine. The phase preceding the onset of an attack of pain includes irritability, malaise, dizziness, nausea, blurred vision or the appearance of spots before the eyes, a sharp change in mood.
Parents should be aware that a child suffering from migraine has a particularly sensitive type of nervous system that reacts to various stimuli with pain sensations along the vessels of the brain and scalp. Therefore, it is very important with the help of a doctor to identify as much as possible all the factors that provoke seizures, and, if possible, exclude them from the lives of children.
Often children are diagnosed with PSYCHOGENIC HEADACHE. It can be associated with depression, fear of entering school, intensify with difficulties in mastering the school curriculum and lack of contact with peers or parents. Such children require consultation of a psychoneurologist and a psychologist.
It happens that parents fear that their child's headache is caused by a BRAIN TUMOR. Although this is the rarest cause, it should be ruled out by careful examination. In children, tumors are localized mainly in the posterior cranial fossa, cause difficulty in the outflow of cerebrospinal fluid, and increase its pressure. The pain is felt in the back of the head or neck, accompanied by nausea and vomiting. The child often looks lethargic, indifferent. There is unsteadiness of gait. The development of hemiparesis (weakness in the muscles of the left or right limbs) may indicate the development of a tumor in one of the hemispheres of the brain. The most informative diagnostic procedure for confirming or excluding a brain tumor is computed tomography, which is usually referred to the patient.
Although this is the rarest cause, it should be ruled out by careful examination. In children, tumors are localized mainly in the posterior cranial fossa, cause difficulty in the outflow of cerebrospinal fluid, and increase its pressure. The pain is felt in the back of the head or neck, accompanied by nausea and vomiting. The child often looks lethargic, indifferent. There is unsteadiness of gait. The development of hemiparesis (weakness in the muscles of the left or right limbs) may indicate the development of a tumor in one of the hemispheres of the brain. The most informative diagnostic procedure for confirming or excluding a brain tumor is computed tomography, which is usually referred to the patient.
It is extremely rare for children to experience neuralgic pain that has a paroxysmal character. These are short, successive attacks of penetrating, cutting, burning pain localized in the face (cranial neuralgia or prosopalgia) with the presence of zones, the irritation of which provokes an attack (touch, washing, eating, etc. ), here in particular refers to trigeminal neuralgia.
), here in particular refers to trigeminal neuralgia.
In addition, there is a drug headache caused by taking certain medications, such as antihistamines, antibiotics, etc.
Headache associated with the abuse of various analgesics, more often non-steroidal anti-inflammatory drugs, as well as anti-migraine drugs, is called overuse, or ricochet. The caffeine withdrawal headache is also known among lovers of strong tea and coffee when it is impossible to drink your favorite drink again and again.
If a child has a headache combined with a high fever and tension in the muscles of the neck, making it difficult to bend the head forward, there is reason to suspect MENINGITIS. In such cases, consult a doctor without delay.
Mixed headache. Headache is only a subjective symptom that accompanies various diseases. To successfully treat a headache, it is necessary, first of all, to find out the mechanism of its occurrence, since different types of headache require a completely different approach.
Examination of children suffering from headache begins with a thorough study of complaints, the history of the development of the disease and a careful medical examination. If during the examination symptoms of an organic lesion of the central nervous system are revealed, then special instrumental and laboratory studies are carried out to clarify the diagnosis. Help for headaches is provided by neurologists and psychoneurologists. For correct diagnosis, studies are important - ultrasound of the vessels (Dopplerography), EEG, MRI, CT, examination by an ophthalmologist, and other specialists according to indications.
They don't have to be afraid. On the contrary, without tightening, do everything prescribed by the doctor. For only then the result of the treatment of your child will be ensured as much as possible.
Headache treatment. Our center uses a pathogenetic approach to the treatment of headaches. It includes not only drug therapy, but also non-traditional methods in treatment (acupuncture, manual therapy), psychological correction, rational psychotherapy and recommendations for lifestyle changes (behavioral medicine).