Getting treated for chlamydia
Chlamydia - Treatment - NHS
Chlamydia can usually be effectively treated with antibiotics. More than 95% of people will be cured if they take their antibiotics correctly.
You may be started on antibiotics once test results have confirmed you have chlamydia. But if it's very likely you have the infection, you might be started on treatment before you get your results.
The two most commonly prescribed antibiotics for chlamydia are:
- doxycycline – taken every day for a week
- azithromycin – one dose of 1g, followed by 500mg once a day for 2 days
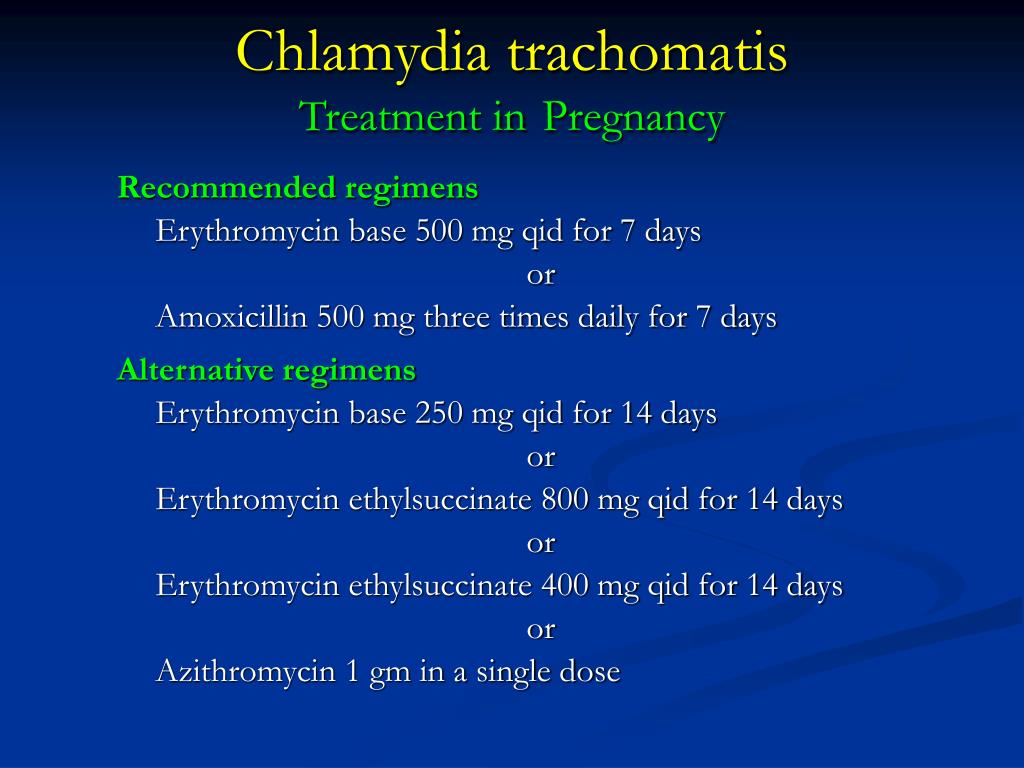
Your doctor may give you different antibiotics, such as amoxicillin or erythromycin, if you have an allergy or are pregnant or breastfeeding. A longer course of antibiotics may be used if your doctor is concerned about complications of chlamydia.
Some people experience side effects during treatment, but these are usually mild. The most common side effects include stomach ache, diarrhoea, feeling sick, and thrush in women.
When can I have sex again?
If you had doxycycline, you shouldn't have sex – including vaginal, oral or anal sex, even with a condom – until both you and your partner(s) have completed treatment.
If you had azithromycin, you should wait 7 days after treatment before having sex (including oral sex).
This will help ensure you don't pass on the infection or catch it again straight away.
Will I need to go back to the clinic?
If you take your antibiotics correctly, you may not need to return to the clinic.
However, you will be advised to go back for another chlamydia test if:
- you had sex before you and your partner finished treatment
- you forgot to take your medication or didn't take it properly
- your symptoms don't go away
- you're pregnant
If you're under 25 years of age, you should be offered a repeat test for chlamydia 3 to 6 months after finishing your treatment because you're at a higher risk of catching it again.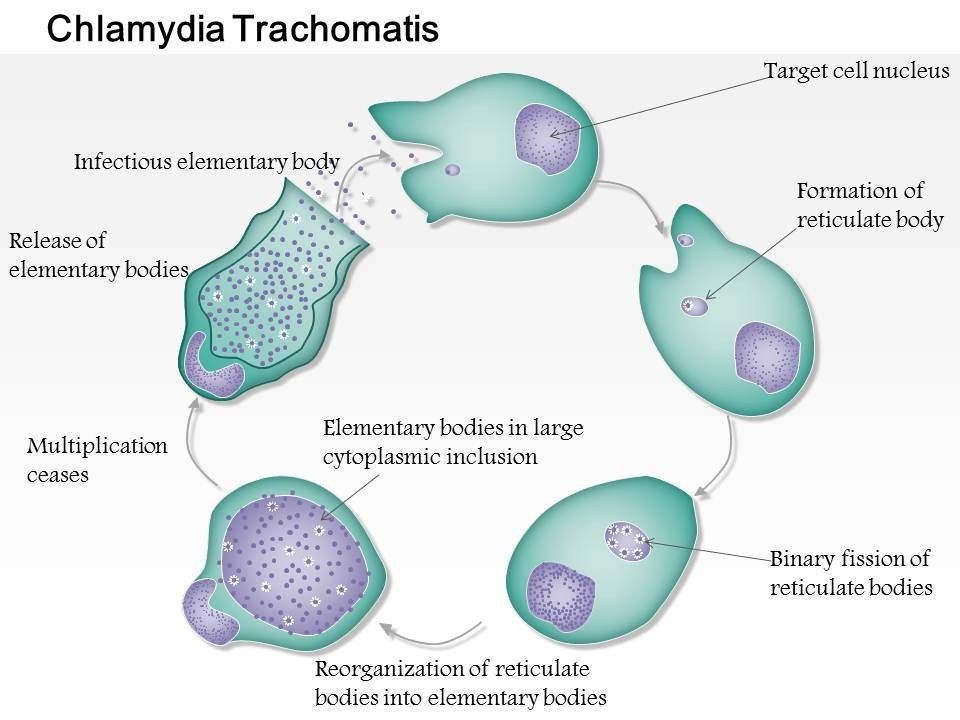
Testing and treating sexual partners
If you test positive for chlamydia, it's important that your current sexual partner and any other recent sexual partners you've had are also tested and treated.
A specialist sexual health adviser can help you contact your recent sexual partners, or the clinic can contact them for you if you prefer.
Either you or someone from the clinic can speak to them, or the clinic can send them a note to let them know they may have been exposed to a sexually transmitted infection (STI).
The note will suggest that they go for a check-up. It will not have your name on it, so your confidentiality will be protected.
Page last reviewed: 01 September 2021
Next review due: 01 September 2024
Where Can I Get Treated For Chlamydia?
In This Section
- Chlamydia
- What are chlamydia symptoms?
- Should I get tested for chlamydia?
- How do I get treated for chlamydia?
- How is chlamydia prevented?
Chlamydia can be easily cured with antibiotics.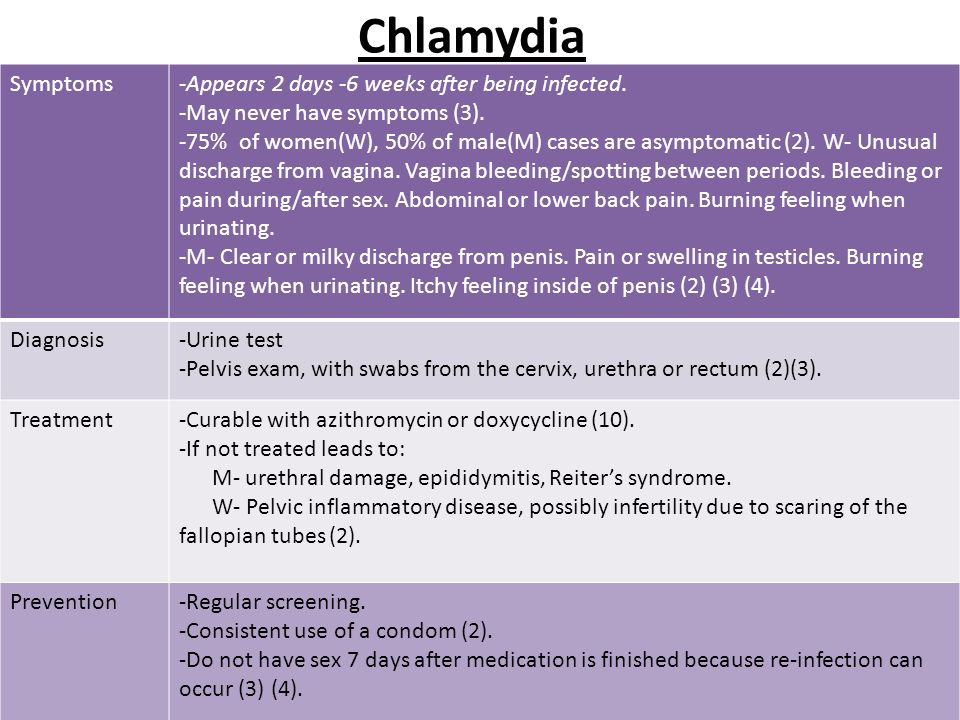 Your sexual partners need to be treated too. If you don’t treat chlamydia, it can lead to serious problems.
Your sexual partners need to be treated too. If you don’t treat chlamydia, it can lead to serious problems.
What’s the treatment for chlamydia?
Chlamydia is usually easy to get rid of. Your nurse or doctor will get you antibiotics to treat the infection. Sometimes you only have to take one dose of medication. Another chlamydia treatment lasts for 7 days. Your doctor will help you figure out which treatment is best for you.
If you’re treated for chlamydia, it’s really important for your sexual partners to get treated also. Otherwise, you can keep passing the infection back and forth, or to other people. Sometimes your doctor will give you medicine for both you and your partner.
What do I need to know if I get treated for chlamydia?
If you’re getting treated for chlamydia:
- Take all of your medicine the way your nurse or doctor tells you to, even if any symptoms you may be having go away sooner. The infection stays in your body until you finish the antibiotics.
- Your partner(s) should also get treated for chlamydia so you don’t re-infect each other or anyone else.
- Don’t have sex for 7 days. If you only have 1 dose of medication, wait for 7 days after you take it before having sex. If you’re taking medicine for 7 days, don’t have sex until you’ve finished all of your pills.
- Get tested again in 3-4 months to make sure your infection is gone.
- Don’t share your medicine with anyone. Your nurse or doctor may give you a separate dose of antibiotics for your partner. Make sure you both take all of the medicine you get.
- Even if you finish your treatment and the chlamydia is totally gone, it’s possible to get a new chlamydia infection again if you’re exposed in the future. Chlamydia isn’t a one-time-only deal. So use condoms and get tested regularly.
An antibiotic called Doxycycline is the most common medicine used to treat chlamydia.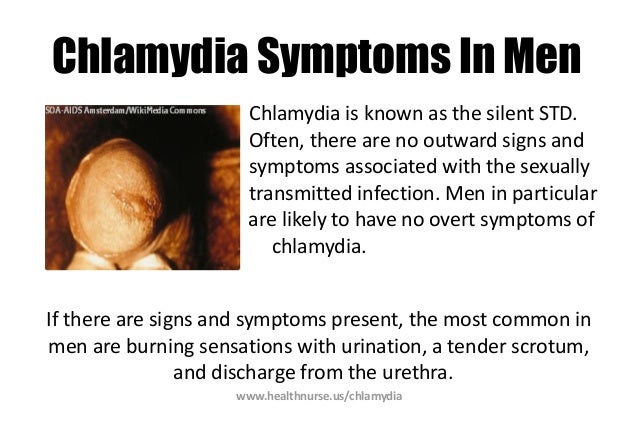 Like most medicines, it can cause mild side effects. The most common side effects of Doxycycline are nausea, vomiting, upset stomach, loss of appetite, mild diarrhea, skin rash or itching, change in skin color, vaginal itching, or discharge. These side effects should go away after you finish taking the medicine. Talk to your nurse or doctor about any medicines you’re already taking and any medical issues you already have before taking Doxycycline.
Like most medicines, it can cause mild side effects. The most common side effects of Doxycycline are nausea, vomiting, upset stomach, loss of appetite, mild diarrhea, skin rash or itching, change in skin color, vaginal itching, or discharge. These side effects should go away after you finish taking the medicine. Talk to your nurse or doctor about any medicines you’re already taking and any medical issues you already have before taking Doxycycline.
What happens if you don’t get treated for chlamydia?
Even though chlamydia is common and doesn’t usually cause any symptoms, it can become a big deal if it’s not caught and treated early.
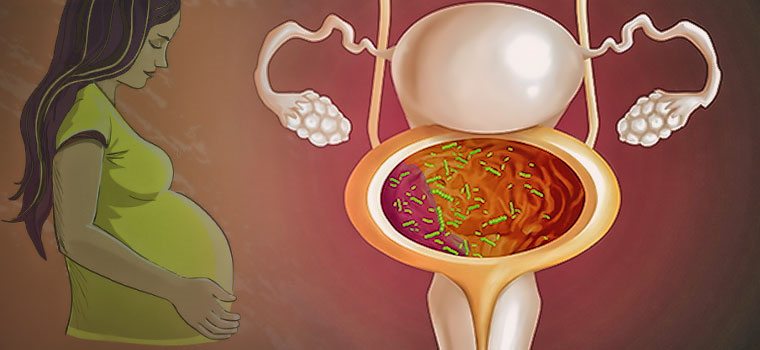
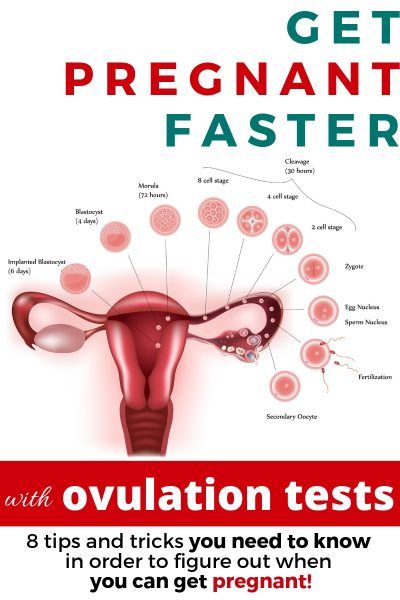
Chlamydia can spread to your uterus and fallopian tubes if it goes untreated for a long time. This can cause you to have pelvic inflammatory disease (PID). PID can cause permanent damage that leads to pain, infertility, or ectopic pregnancy. So getting tested regularly for chlamydia really lowers your chances of getting PID.
If you have a penis, a chlamydia infection can spread to your epididymis (a tube that carries sperm from your testicles) if it’s left untreated, and can cause chronic joint pain. Rarely, it can make you infertile.
Having chlamydia may increase your chances of getting or spreading HIV.
If you have chlamydia during your pregnancy and don’t treat it, you can pass it to your baby when you’re giving birth. Chlamydia can also cause eye infections and pneumonia in newborns, and it also increases the risk of delivering your baby too early.
Testing and treatment for chlamydia is quick, easy, and the best way to avoid all of these problems.
More questions from patients:
How long will I test positive for chlamydia after getting treatment?
If your nurse or doctor gives you a single dose of medicine, you have to wait 7 days before you’re no longer infected and can have sex again. If you’re taking medicine for 7 days, you won’t test negative until you’ve finished all of your pills.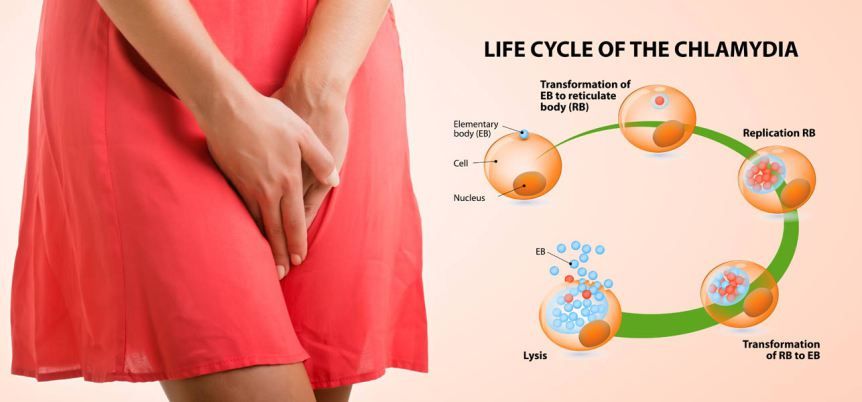 Either way, you need to wait 7 days until you should be cleared from the chlamydia infection.
Either way, you need to wait 7 days until you should be cleared from the chlamydia infection.
After that 7 day mark, you can have sex again without spreading the infection. If you were given pills to take, it’s important to take ALL of your medicine, even if the symptoms go away sooner. The infection stays in your body until you finish the antibiotic pills.
Getting chlamydia again is common. Even if you finish your treatment and the chlamydia is totally gone, it’s possible to get a new chlamydia infection again if you’re exposed in the future. Chlamydia isn’t a one-time-only deal. So use condoms and get tested again in 3-4 months to make sure your infection is gone.
Was this page helpful?- Yes
- No
Help us improve - how could this information be more helpful?
How did this information help you?
Please answer below.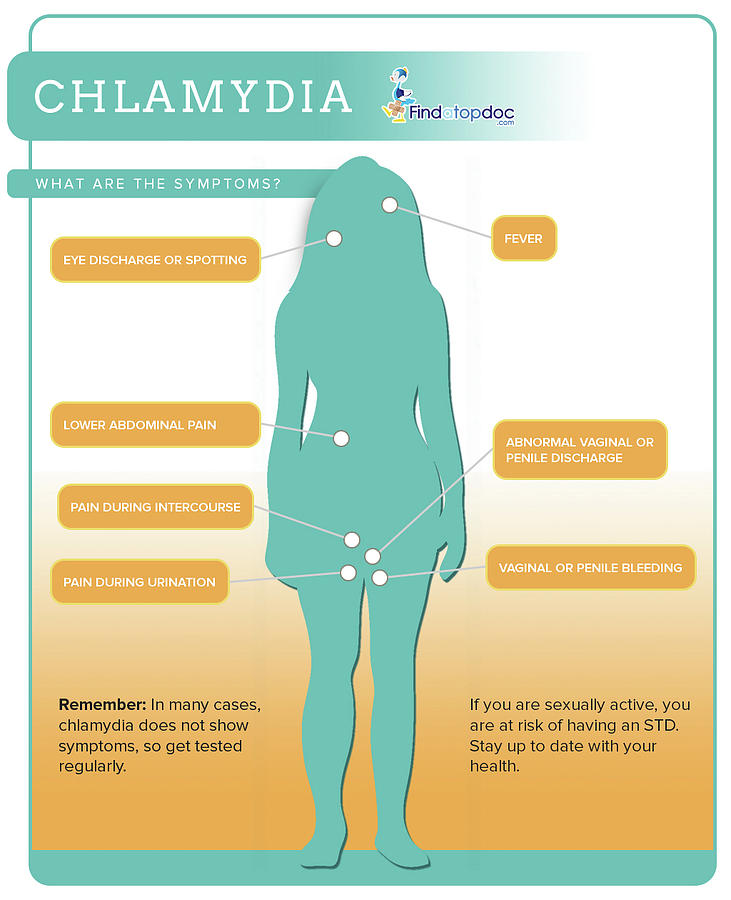
Are you human? (Sorry, we have to ask!)
Please don't check this box if you are a human.
You’re the best! Thanks for your feedback.
Thanks for your feedback.
Back to top
We couldn't access your location, please search for a location.
Zip, City, or State
Please enter a valid 5-digit zip code or city or state.
Please fill out this field.
Service All Services Abortion Abortion Referrals Birth Control COVID-19 Vaccine HIV Services Men's Health Care Mental Health Morning-After Pill (Emergency Contraception) Pregnancy Testing & Services Primary Care STD Testing, Treatment & Vaccines Transgender Hormone Therapy Women's Health Care
Filter By All Telehealth In-person
Please enter your age and the first day of your last period for more accurate abortion options. Your information is private and anonymous.
Your information is private and anonymous.
AGE This field is required.
Or call 1-800-230-7526
Treatment of chlamydia, chlamydia in the clinic "Your Doctor". Diagnostics. Sign up
Treatment of chlamydia, chlamydia in the clinic "Your Doctor"
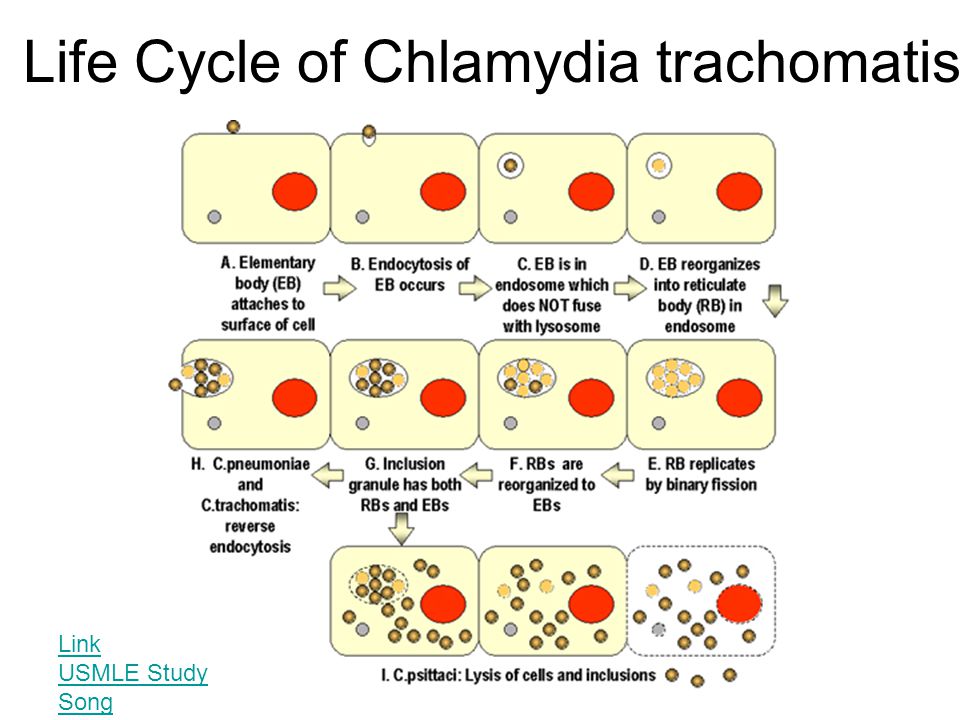
Chlamydia, Chlamydia is an infectious disease belonging to the class of sexually transmitted infections (STIs), which is caused by a specific pathogen - chlamydia. Currently, several types of chlamydia are known; the main and dangerous to humans is the species Chlamydia trachomatis. Chlamydia are obligate parasitic bacteria that, like viruses, can multiply inside the cells of the human body - they cause chlamydia. Chlamydia have a unique reproduction cycle that includes the existence of the bacterium in two forms - elementary bodies (ET) and reticular bodies (RT). The cycle of reproduction of bacteria is from 48 to 72 hours - from the moment the elementary body (EB) enters the cell, to the release of many newly formed EBs from the already destroyed cell, capable of infecting new, nearby cells. In the process of reproduction, ETs are transformed into transitional bodies, from which RTs are formed, and the latter, also through transitional forms, are again transformed into ETs. Outside the human body, chlamydia die when heated, as well as under the action of disinfectants. Chlamydia is transmitted from person to person mainly through sexual contact. Infection in the household way, through household items, linen, towels, washcloths, etc., also occurs, but it does not exceed 7-12% of the total number of infections. When introduced into the body, chlamydia can affect not only the genitourinary system, being the cause of more than half of infertile marriages and chronic inflammatory processes in the organs of the genitourinary system. Affecting the cardiovascular system, chlamydia often cause coronary heart disease and myocardial infarction, affecting the lungs, cause sluggish pneumonia that is not amenable to conventional treatment, as well as bronchial asthma. Described chlamydial lesions of the gastrointestinal tract, joints, eyes.
In the process of reproduction, ETs are transformed into transitional bodies, from which RTs are formed, and the latter, also through transitional forms, are again transformed into ETs. Outside the human body, chlamydia die when heated, as well as under the action of disinfectants. Chlamydia is transmitted from person to person mainly through sexual contact. Infection in the household way, through household items, linen, towels, washcloths, etc., also occurs, but it does not exceed 7-12% of the total number of infections. When introduced into the body, chlamydia can affect not only the genitourinary system, being the cause of more than half of infertile marriages and chronic inflammatory processes in the organs of the genitourinary system. Affecting the cardiovascular system, chlamydia often cause coronary heart disease and myocardial infarction, affecting the lungs, cause sluggish pneumonia that is not amenable to conventional treatment, as well as bronchial asthma. Described chlamydial lesions of the gastrointestinal tract, joints, eyes. According to our research, chlamydia leads to a violation of the connective tissue of the fatty capsule of the kidneys, causing the occurrence of nephroptosis; and also, according to our research, chlamydia is detected in 88% of patients suffering from Peyronie's disease - fibroplastic induration of the penis. At the same time, chlamydia is a very common disease - it is detected more white than in 30% of both women and men suffering from chronic inflammatory processes in the organs of the genitourinary system. Often, chlamydia is combined with other sexually transmitted infections - mycoplasmosis, trichomoniasis, gardnerellosis, candidiasis. Only humans suffer from chlamydia of the genitourinary system, the most common animals surrounding humans are immune to this infection. nine0003 Symptoms of chlamydia, chlamydia Chlamydia, as a rule, has a chronic course, with mild symptoms of a varied order, or asymptomatic. In some cases, the disease can have an acute and subacute clinical course.
According to our research, chlamydia leads to a violation of the connective tissue of the fatty capsule of the kidneys, causing the occurrence of nephroptosis; and also, according to our research, chlamydia is detected in 88% of patients suffering from Peyronie's disease - fibroplastic induration of the penis. At the same time, chlamydia is a very common disease - it is detected more white than in 30% of both women and men suffering from chronic inflammatory processes in the organs of the genitourinary system. Often, chlamydia is combined with other sexually transmitted infections - mycoplasmosis, trichomoniasis, gardnerellosis, candidiasis. Only humans suffer from chlamydia of the genitourinary system, the most common animals surrounding humans are immune to this infection. nine0003 Symptoms of chlamydia, chlamydia Chlamydia, as a rule, has a chronic course, with mild symptoms of a varied order, or asymptomatic. In some cases, the disease can have an acute and subacute clinical course. In the acute form, patients show redness of the mucous membranes of the urethra, cervix, sometimes some increase in the urge to urinate, scanty mucopurulent discharge from the urethra and vagina. In the chronic course of the disease, these symptoms are erased, mild. In this case, slight discharge can occur only in the morning or after hypothermia. With an asymptomatic course of the disease, patients do not present any health complaints. In men, chronic chlamydial urethritis can sometimes be accompanied by a feeling of heaviness, discomfort in the urethra, and a slight burning sensation. According to our research, long-term urogenital chlamydia in almost 100% of cases leads to the development of prostatitis with subsequent spread to the seminal vesicles and scrotal organs. In women, chlamydia lesions of the urethra, Bartholin glands, vagina, uterus are often asymptomatic, only in a small part of patients accompanied by a feeling of heaviness in the lower abdomen and pain in the lumbar region, especially during menstruation.
In the acute form, patients show redness of the mucous membranes of the urethra, cervix, sometimes some increase in the urge to urinate, scanty mucopurulent discharge from the urethra and vagina. In the chronic course of the disease, these symptoms are erased, mild. In this case, slight discharge can occur only in the morning or after hypothermia. With an asymptomatic course of the disease, patients do not present any health complaints. In men, chronic chlamydial urethritis can sometimes be accompanied by a feeling of heaviness, discomfort in the urethra, and a slight burning sensation. According to our research, long-term urogenital chlamydia in almost 100% of cases leads to the development of prostatitis with subsequent spread to the seminal vesicles and scrotal organs. In women, chlamydia lesions of the urethra, Bartholin glands, vagina, uterus are often asymptomatic, only in a small part of patients accompanied by a feeling of heaviness in the lower abdomen and pain in the lumbar region, especially during menstruation. In some patients, chlamydia occurs in severe form, while, along with damage to the genitourinary system, there are lesions of the joints, conjunctiva of the eyes, skin and mucous membranes of the oral cavity and nasopharynx, as well as the rectum. In women, chlamydia adversely affects the course of pregnancy and is often transmitted to newborns. With asymptomatic chlamydia, the first signs of this disease are, as a rule, the symptoms of already developed complications, with their specific manifestations. nine0003 Diagnosis of chlamydia, chlamydia An important principle in the diagnosis of chlamydia is regularity. For men and women who are sexually active outside of marriage, it is necessary to undergo tests for the presence of chlamydia every six months. For people living in marriage, such a period can be from one year to one and a half years. Patients with diseases of the joints, eye lesions, sluggish diseases of the internal organs and the gastrointestinal tract, patients suffering from pathology of the cardiovascular system, lung diseases, bronchial asthma, frequent pharyngitis and tonsillitis should be subjected to a mandatory study for the presence of chlamydia - the causative agents of chlamydia.
In some patients, chlamydia occurs in severe form, while, along with damage to the genitourinary system, there are lesions of the joints, conjunctiva of the eyes, skin and mucous membranes of the oral cavity and nasopharynx, as well as the rectum. In women, chlamydia adversely affects the course of pregnancy and is often transmitted to newborns. With asymptomatic chlamydia, the first signs of this disease are, as a rule, the symptoms of already developed complications, with their specific manifestations. nine0003 Diagnosis of chlamydia, chlamydia An important principle in the diagnosis of chlamydia is regularity. For men and women who are sexually active outside of marriage, it is necessary to undergo tests for the presence of chlamydia every six months. For people living in marriage, such a period can be from one year to one and a half years. Patients with diseases of the joints, eye lesions, sluggish diseases of the internal organs and the gastrointestinal tract, patients suffering from pathology of the cardiovascular system, lung diseases, bronchial asthma, frequent pharyngitis and tonsillitis should be subjected to a mandatory study for the presence of chlamydia - the causative agents of chlamydia.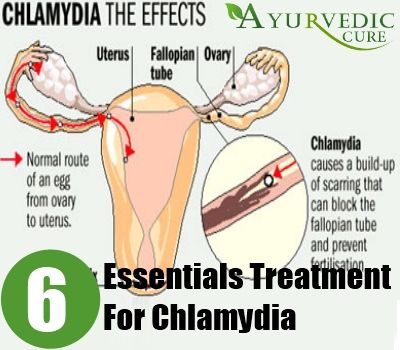 All patients suffering from infertility and inflammatory processes in the genitourinary system are subject to mandatory testing for chlamydia. In the diagnosis of chlamydia, methods of special laboratory and bacteriological diagnostics are of primary importance. The simplest are immunoluminescent methods that allow the detection of chlamydia antigens directly in a microscopic preparation. For this purpose, the method of direct immunofluorescence (DIF) is usually used, using monoclonal antibodies to various antigens of the pathogen. At the same time, the PIF method, according to the estimates of various authors, is effective within 45 - 67% and can give false positive results. In recent years, molecular biological methods have become the gold standard in the diagnosis of chlamydial infection - chlamydia, primarily PCR (DNA diagnostics), which, under all conditions from material sampling to its delivery, amplification and evaluation, is effective, according to some authors, in nine0% or more.
All patients suffering from infertility and inflammatory processes in the genitourinary system are subject to mandatory testing for chlamydia. In the diagnosis of chlamydia, methods of special laboratory and bacteriological diagnostics are of primary importance. The simplest are immunoluminescent methods that allow the detection of chlamydia antigens directly in a microscopic preparation. For this purpose, the method of direct immunofluorescence (DIF) is usually used, using monoclonal antibodies to various antigens of the pathogen. At the same time, the PIF method, according to the estimates of various authors, is effective within 45 - 67% and can give false positive results. In recent years, molecular biological methods have become the gold standard in the diagnosis of chlamydial infection - chlamydia, primarily PCR (DNA diagnostics), which, under all conditions from material sampling to its delivery, amplification and evaluation, is effective, according to some authors, in nine0% or more. However, in reality, according to our estimates, the effectiveness of this method is not higher than 75-80%. The currently existing methods of serological diagnostics (microimmunofluorescence, enzyme immunoassay) have limited diagnostic value and cannot be used as the only ones in the diagnosis of chlamydia. The most effective diagnostic methods include the method of cultural inoculation of the material. This method is highly specific and indispensable for determining the cure of the disease. Recently, another high-precision method has been used to diagnose chlamydia - NASBA, which is a molecular biological study of chlamydial ribonucleic acid (RNA diagnostics). To obtain highly accurate patient examination results, it is recommended to examine the material with at least three different methods simultaneously. nine0003 Treatment of chlamydia, chlamydia The introduction of modern treatment technologies makes it possible to completely cure chlamydia, subject to appropriate conditions.
However, in reality, according to our estimates, the effectiveness of this method is not higher than 75-80%. The currently existing methods of serological diagnostics (microimmunofluorescence, enzyme immunoassay) have limited diagnostic value and cannot be used as the only ones in the diagnosis of chlamydia. The most effective diagnostic methods include the method of cultural inoculation of the material. This method is highly specific and indispensable for determining the cure of the disease. Recently, another high-precision method has been used to diagnose chlamydia - NASBA, which is a molecular biological study of chlamydial ribonucleic acid (RNA diagnostics). To obtain highly accurate patient examination results, it is recommended to examine the material with at least three different methods simultaneously. nine0003 Treatment of chlamydia, chlamydia The introduction of modern treatment technologies makes it possible to completely cure chlamydia, subject to appropriate conditions. Treatment should be carried out under the direct supervision and prescription of a physician. The duration of treatment, as a rule, is at least 20 days, however, in the presence of developed complications, this period can be extended. A general prerequisite for successful treatment is the simultaneous treatment of sexual partners - even in cases where chlamydia is reliably detected only in one of them. During the course of the treatment process and subsequent control, sexual activity is prohibited for both partners. The treatment process is complex and includes both specific antibacterial drugs and non-specific drugs and physiotherapy. As in the treatment of viral infections, the treatment of chlamydia includes the mandatory use of immune preparations, most often endogenous interferon inducers, in combination with antichlamydial antibiotics (ciprofloxacins, ofloxacins, levofloxacins, etc.). Treatment should be optimized taking into account the individual characteristics of the course of the disease, taking into account the stage of the inflammatory process, its localization, the presence or absence of complications.
Treatment should be carried out under the direct supervision and prescription of a physician. The duration of treatment, as a rule, is at least 20 days, however, in the presence of developed complications, this period can be extended. A general prerequisite for successful treatment is the simultaneous treatment of sexual partners - even in cases where chlamydia is reliably detected only in one of them. During the course of the treatment process and subsequent control, sexual activity is prohibited for both partners. The treatment process is complex and includes both specific antibacterial drugs and non-specific drugs and physiotherapy. As in the treatment of viral infections, the treatment of chlamydia includes the mandatory use of immune preparations, most often endogenous interferon inducers, in combination with antichlamydial antibiotics (ciprofloxacins, ofloxacins, levofloxacins, etc.). Treatment should be optimized taking into account the individual characteristics of the course of the disease, taking into account the stage of the inflammatory process, its localization, the presence or absence of complications. A patient with chlamydia is considered cured if, within 3 months after the end of treatment, chlamydia is not detected in him during control laboratory tests. nine0011
A patient with chlamydia is considered cured if, within 3 months after the end of treatment, chlamydia is not detected in him during control laboratory tests. nine0011 Chlamydia - KVD №2
What is chlamydia?
Chlamydia is a common sexually transmitted infection (STI). The disease is caused by the bacterium Chlamydia trachomatis (Chlamydia trachomatis), which affects the female genital area and is the cause of non-gonococcal urethritis in men. Manifestations of chlamydia are usually minor or absent, but serious complications develop. Complications can cause irreparable damage to the body, including infertility - all this proceeds very secretly. nine0011
Chlamydia also causes penile discharge in infected men.
Ways of transmission of chlamydia
Chlamydia can be transmitted through:
- vaginal or anal contact with an infected partner;
- less common with oral sex;
- use of sex toys with an infected partner;
- infection of a newborn during childbirth from a sick mother.
Absolutely all sexually active people can get chlamydia. The greater the number of sexual partners, the greater the risk of infection. The risk of infection is especially high in girls, because their cervix is not fully formed. About 75% of new cases occur in women under 25 years of age. By the age of 30, approximately 50% of sexually active women have had chlamydia. In sexually active men, the risk of infection is highest between the ages of 20 and 24. nine0011
You cannot get chlamydia through kissing, hugging, dishes, baths, towels.
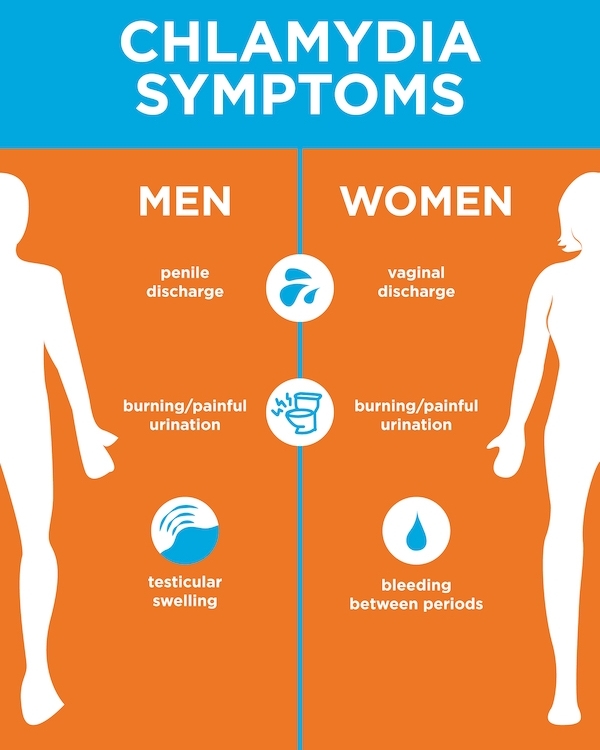
Manifestations of chlamydia
Chlamydia is very secretive. About 75% of infected women and 50% of infected men are asymptomatic. If manifestations of the disease develop, then this occurs approximately 1 to 3 weeks after infection.
In women, chlamydia first affects the cervix and urethra (urinary canal).
Manifestations:
- unusual vaginal discharge; nine0026
- pain or discomfort when urinating;
If the infection penetrates to the appendages, manifestations are possible:
- pain in the lower abdomen;
- pain in the lumbar region;
- nausea;
- slight increase in temperature;
- pain during intercourse or bleeding after it;
- bleeding between periods.
Symptoms in men:
- clear or cloudy discharge from the penis; nine0026
- pain or discomfort when urinating;
- there may be burning and itching in the area of the outlet of the urethra;
- rarely pain and/or swelling of the testicles.
Men or women who have anal sex with an infected partner can infect the rectum, resulting in inflammation, pain, discharge, or bleeding from the rectum.
Chlamydia can cause sore throat (pharyngitis) in men and women who have oral contact with an infected partner. nine0011
What complications can develop if chlamydia is not treated?
If the disease is left untreated, serious short-term and persistent complications develop. Like the disease itself, complications often occur insidiously.
In women with untreated chlamydia, the infection can spread from the urethra to the fallopian tubes (tubes that carry eggs from the ovaries to the uterus) - this causes (in 40% of cases) the development of pelvic inflammatory disease (PID).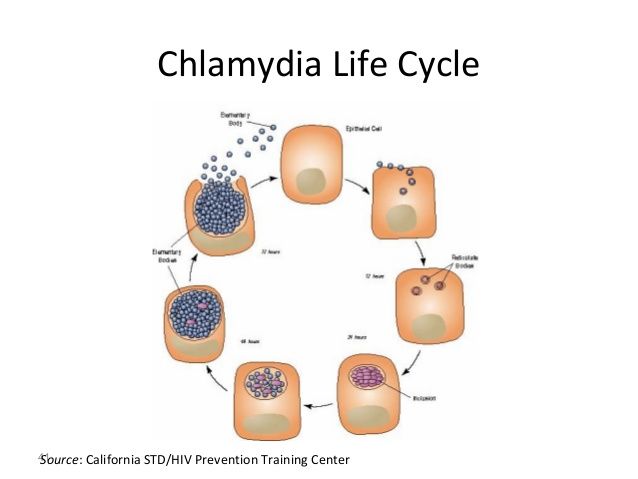 PID causes permanent damage to the fallopian tubes, uterus, and surrounding tissues. Chronic pelvic pain, infertility and ectopic pregnancy are the result of PID. nine0011
PID causes permanent damage to the fallopian tubes, uterus, and surrounding tissues. Chronic pelvic pain, infertility and ectopic pregnancy are the result of PID. nine0011
Women with chlamydia are more susceptible to contracting HIV infection, the risk increases by almost 5 times.
To prevent serious consequences of chlamydia, annual chlamydia screening is required for all sexually active women 25 years of age and younger. An annual examination is necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia. nine0011
Complications of chlamydia are rare in men. The infection sometimes extends to the epididymis and causes pain, fever, and, rarely, male infertility (sterility).
Rarely, chlamydial infection can cause inflammation of the joints in combination with skin lesions, inflammation of the eyes and urinary tract - this is the so-called Reiter's syndrome.
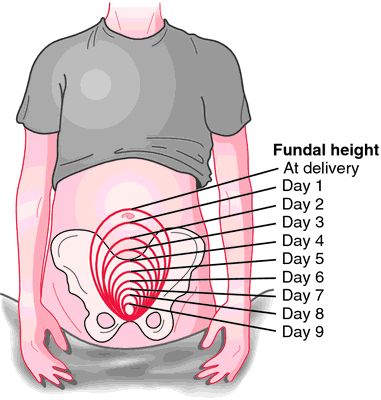
The effect of chlamydia on a pregnant woman and her child
Chlamydia in pregnant women increases the risk of miscarriage, premature detachment of the placenta.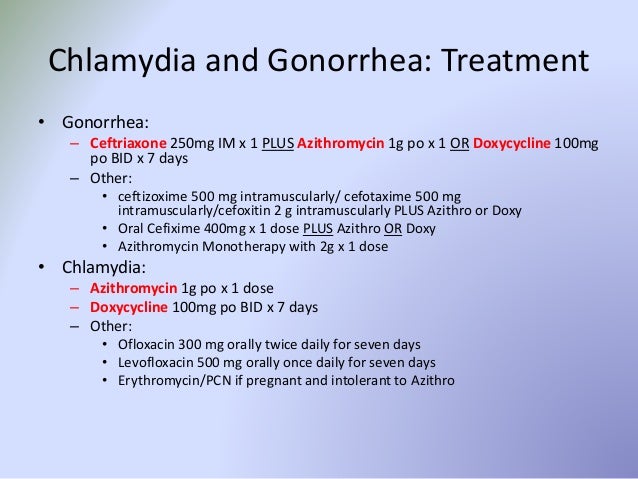 Newborns from infected mothers can get eye and lung infections. A lung infection (pneumonia) can be fatal to a newborn. nine0011
Newborns from infected mothers can get eye and lung infections. A lung infection (pneumonia) can be fatal to a newborn. nine0011
Diagnosis of chlamydia
Diagnosis includes observation of the patient's clinical symptoms, testing for chlamydia smears from the cervix, scraping from the urinary canal, the first morning urine. Most often, the study is carried out by PCR (polymerase chain reaction). Swabs and scrapings may cause minor discomfort.
Additionally, a blood test is performed by ELISA (enzyme-linked immunosorbent assay) for the presence of immunity to chlamydia, this auxiliary test often helps to establish an accurate diagnosis. nine0011
Chlamydia treatment
Chlamydia treatment is with oral antibiotics. To prevent re-infection, all sexual partners must be found, examined and treated. Patients with chlamydia should refrain from unprotected sex during treatment, otherwise it is possible to re-infect the sexual partner. Unfortunately, after successful treatment, re-infection with chlamydia is possible, since a strong immunity to this microorganism does not develop.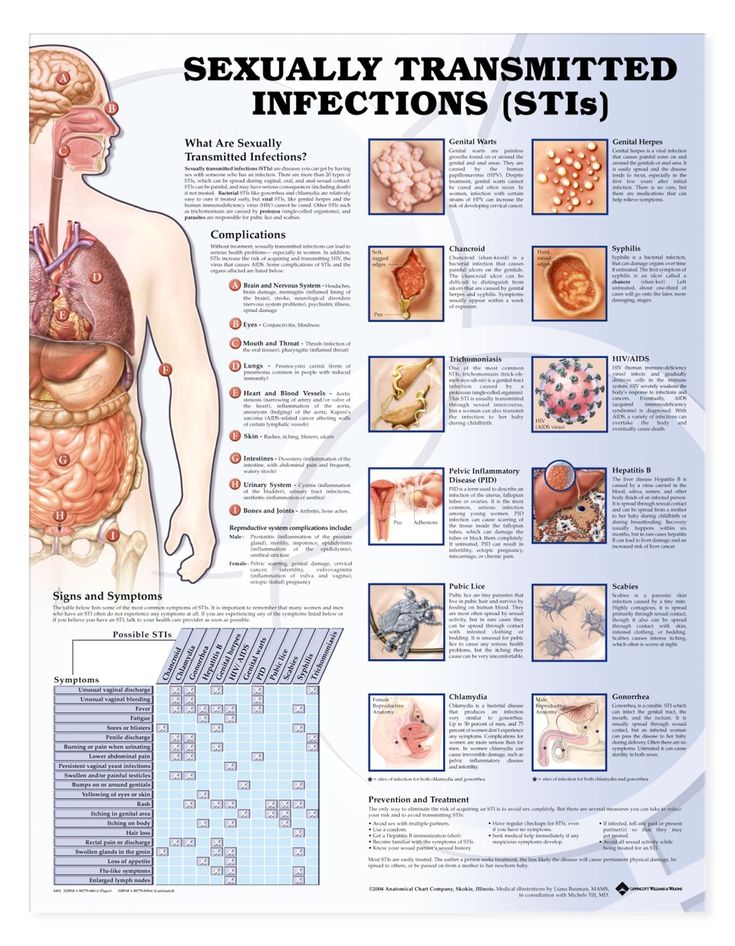 Repeated infection of women with chlamydia leads to a significant increase in the risk of serious complications, including infertility. A re-examination is carried out 4 weeks after treatment. nine0011
Repeated infection of women with chlamydia leads to a significant increase in the risk of serious complications, including infertility. A re-examination is carried out 4 weeks after treatment. nine0011
Chlamydia prevention
The best way to prevent sexually transmitted infections is through long-term sexual contact with one healthy sexual partner. Latex male condoms, when used correctly, drastically reduce the risk of transmission.
Annual chlamydia screening required for all sexually active women aged 25 and under. An annual examination is also necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia. nine0011
Any manifestations, such as pain or discomfort when urinating, unusual rash, discharge are a signal to stop sexual intercourse and immediately examine in a specialized clinic - KVD. If the patient is found to have chlamydia (or any other STI), he must inform his sexual partners so that they also undergo a full examination and appropriate treatment.