Gestational diabetes how to lower blood sugar
Gestational Diabetes and Pregnancy | CDC
Gestational diabetes is a type of diabetes that is first seen in a pregnant woman who did not have diabetes before she was pregnant. Some women have more than one pregnancy affected by gestational diabetes. Gestational diabetes usually shows up in the middle of pregnancy. Doctors most often test for it between 24 and 28 weeks of pregnancy.
Often gestational diabetes can be managed through eating healthy foods and regular exercise. Sometimes a woman with gestational diabetes must also take insulin.
Learn more about Diabetes Self-Management Education and Support Services
Blood sugar that is not well controlled in a woman with gestational diabetes can lead to problems for the pregnant woman and the baby:
An Extra-Large Baby
Diabetes that is not well controlled causes the baby’s blood sugar to be high. The baby is “overfed” and grows extra-large. Besides causing discomfort to the woman during the last few months of pregnancy, an extra-large baby can lead to problems during delivery for both the mother and the baby. The mother might need a C-Section to deliver the baby. The baby can be born with nerve damage due to pressure on the shoulder during delivery.
C-Section (Cesarean Section)
A C-section is an operation to deliver the baby through the mother’s belly. A woman who has diabetes that is not well controlled has a higher chance of needing a C-section to deliver the baby. When the baby is delivered by a C-section, it takes longer for the woman to recover from childbirth.
High Blood Pressure (Preeclampsia)
When a pregnant woman has high blood pressure, protein in her urine, and often swelling in fingers and toes that doesn’t go away, she might have preeclampsia. It is a serious problem that needs to be watched closely and managed by her doctor. High blood pressure can cause harm to both the woman and her unborn baby. It might lead to the baby being born early and also could cause seizures or a stroke (a blood clot or a bleed in the brain that can lead to brain damage) in the woman during labor and delivery.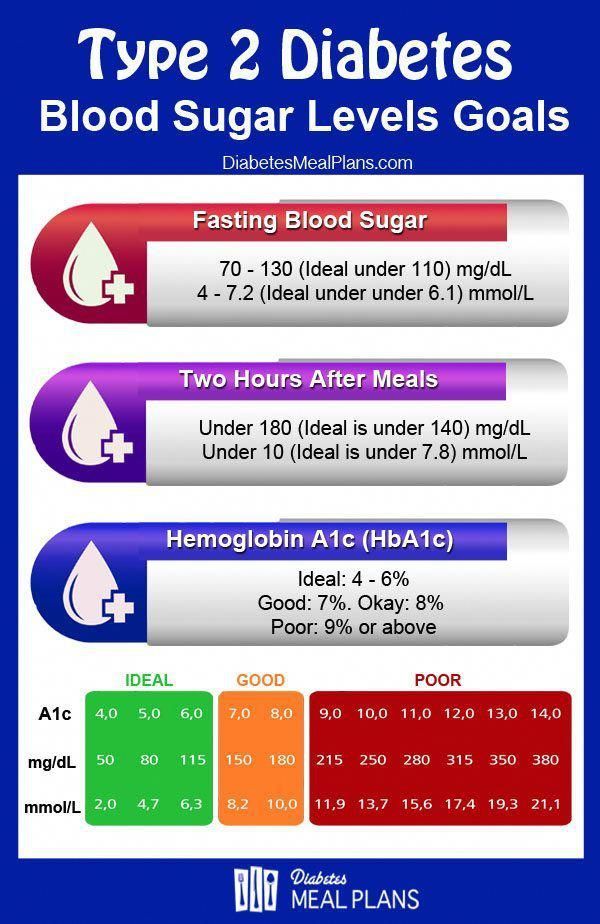 Women with diabetes have high blood pressure more often than women without diabetes.
Women with diabetes have high blood pressure more often than women without diabetes.
Low Blood Sugar (Hypoglycemia)
People with diabetes who take insulin or other diabetes medications can develop blood sugar that is too low. Low blood sugar can be very serious, and even fatal, if not treated quickly. Seriously low blood sugar can be avoided if women watch their blood sugar closely and treat low blood sugar early.
If a woman’s diabetes was not well controlled during pregnancy, her baby can very quickly develop low blood sugar after birth. The baby’s blood sugar must be watched for several hours after delivery.
5 Tips for Women with Gestational Diabetes
- Eat Healthy Foods
Eat healthy foods from a meal plan made for a person with diabetes. A dietitian can help you create a healthy meal plan. Learn more about diabetes meal planning. - A dietitian can also help you learn how to control your blood sugar while you are pregnant.
 To find a registered dietician near you, please visit The Academy of Nutrition and Dietetics website.
To find a registered dietician near you, please visit The Academy of Nutrition and Dietetics website.
- Exercise Regularly
Exercise is another way to keep blood sugar under control. It helps to balance food intake. After checking with your doctor, you can exercise regularly during and after pregnancy. Get at least 30 minutes of moderate-intensity physical activity at least five days a week. This could be brisk walking, swimming, or actively playing with children.Learn more about physical activity during pregnancy » - Monitor Blood Sugar Often
Because pregnancy causes the body’s need for energy to change, blood sugar levels can change very quickly. Check your blood sugar often, as directed by your doctor. - Take Insulin, If Needed
Sometimes a woman with gestational diabetes must take insulin. If insulin is ordered by your doctor, take it as directed in order to help keep blood sugar under control.
- Get Tested for Diabetes after Pregnancy
Get tested for diabetes 6 to 12 weeks after your baby is born, and then every 1 to 3 years.For most women with gestational diabetes, the diabetes goes away soon after delivery. When it does not go away, the diabetes is called type 2 diabetes. Even if the diabetes does go away after the baby is born, half of all women who had gestational diabetes develop type 2 diabetes later. It’s important for a woman who has had gestational diabetes to continue to exercise and eat a healthy diet after pregnancy to prevent or delay getting type 2 diabetes. She should also remind her doctor to check her blood sugar every 1 to 3 years.
Women who had gestational diabetes or who develop prediabetes can also learn more about the National Diabetes Prevention Program (National DPP), CDC-recognized lifestyle change programs. To find a CDC-recognized lifestyle change class near you, or join one of the online programs.
More Information
Gestational Diabetes and Pregnancy [PDF – 1 MB]
View, download, and print this brochure about gestational diabetes and pregnancy.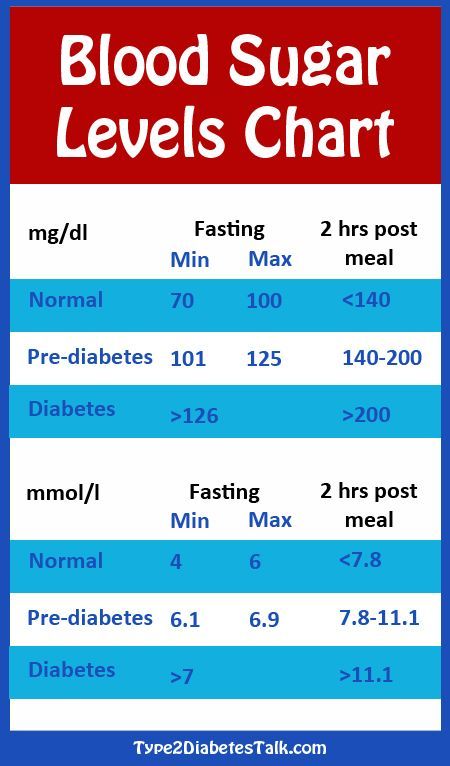
For more information on gestational diabetes, visit the American Diabetes Association’s website.
- Diabetes
- Before Pregnancy
- Healthy Pregnancy
- Birth Defects
- CDC’s National Center on Birth Defects and Developmental Disabilities
How to Treat Gestational Diabetes
Gestational Diabetes
Because gestational diabetes can hurt you and your baby, it is critical to start treatment quickly.
Treatment for gestational diabetes aims to keep blood glucose levels equal to those of pregnant women who don't have gestational diabetes. The treatment always includes special meal plans and scheduled physical activity, and it may also include daily blood glucose testing and insulin injections.
If you're testing your blood glucose, the American Diabetes Association suggests the following targets for women who develop gestational diabetes during pregnancy. More or less stringent glycemic goals may be appropriate for each individual.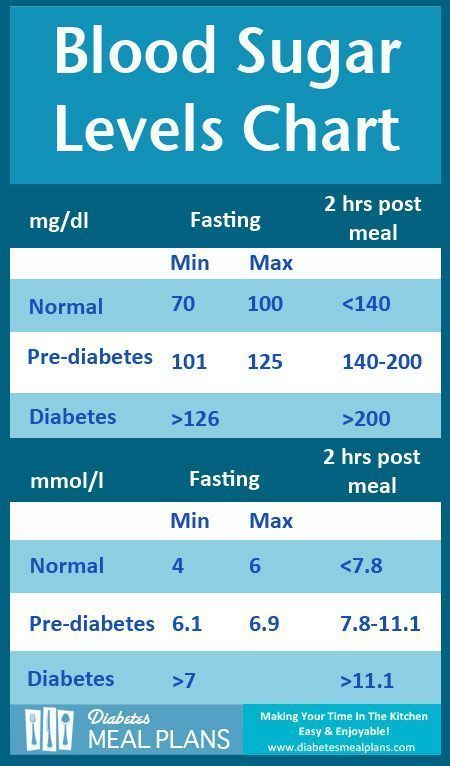
- Before a meal (preprandial): 95 mg/dl or less
- One hour after a meal (postprandial): 140 mg/dl or less
- Two hours after a meal (postprandial): 120 mg/dl or less
If you’re diagnosed with gestational diabetes, you will need help from your doctor, nurse educator and other members of your health care team so that your treatment can change as needed. For you as the mother-to-be, proper treatment helps lower the risk of a cesarean section birth that very large babies may require.
Sticking with your treatment plan will give you a healthy pregnancy and birth, and may help your baby avoid poor health in the future.
Keeping worry in perspective
While gestational diabetes is a cause for concern, the good news is that you and your health care team—your doctor, obstetrician, nurse educator and dietitian—work together to lower your high blood glucose levels. And with this help, you can turn your concern into a healthy pregnancy for you and a healthy start for your baby.
Looking ahead
Gestational diabetes usually goes away after pregnancy. But once you've had gestational diabetes, your chances are two in three that it will return in future pregnancies. In a few women, however, pregnancy uncovers type 1 or type 2 diabetes. It is hard to tell whether these women have gestational diabetes or have just started showing their diabetes during pregnancy, but they will need to continue diabetes treatment after pregnancy.
Many women who have gestational diabetes go on to develop type 2 diabetes years later. There seems to be a link between the tendency to have gestational diabetes and type 2 diabetes since both involve insulin resistance. However, certain basic lifestyle changes may help prevent diabetes after gestational diabetes. Learn about prevention.
Lower your risk by losing weight
Are you more than 20% over your ideal body weight? Losing even a few pounds can help you avoid developing type 2 diabetes.
Making healthy food choicesFollow simple daily guidelines like eating a variety of foods including fresh fruits and vegetables, limiting fat intake to 30% or less of daily calories and watching your portion sizes. Healthy eating habits can go a long way in preventing diabetes and other health problems.
Healthy eating habits can go a long way in preventing diabetes and other health problems.
Regular exercise allows your body to use glucose without extra insulin. This helps combat insulin resistance and is what makes exercise helpful to people with diabetes. However, it is important to check with your doctor before starting an exercise program.
More on losing weight
Gestational diabetes - causes, symptoms, diagnosis, treatment, diet, prevention of diabetes during pregnancy
Gestational diabetes is diabetes that occurs during pregnancy. From 1 to 20% (on average - 7%) of expectant mothers face such a problem. For the majority, this pathology after childbirth disappears without a trace, but in 10-15% it turns into type II diabetes mellitus. Half of women who have gestational diabetes during pregnancy acquire type II diabetes within the next 10-15 years after giving birth. nine0005
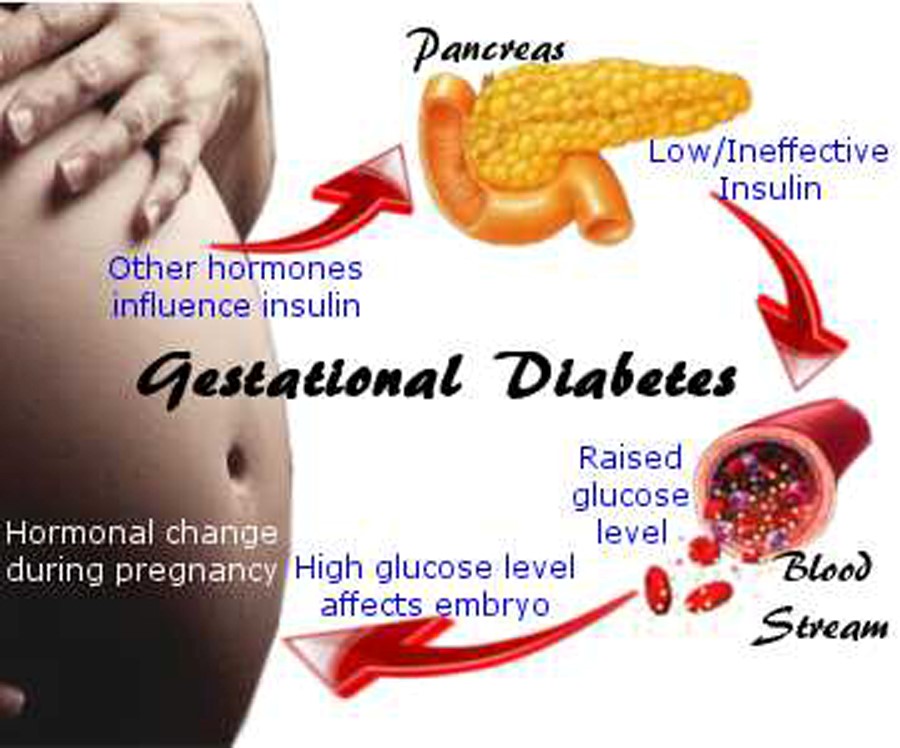
Causes of gestational diabetes
The exact mechanism of the onset of the disease is still not completely clear. Doctors are inclined to believe that the hormones responsible for the proper development of the fetus block the production of insulin, which leads to a violation of carbohydrate metabolism. During pregnancy, more glucose is required for both the woman and the baby. The body compensates for this need by suppressing the production of insulin.
Doctors are inclined to believe that the hormones responsible for the proper development of the fetus block the production of insulin, which leads to a violation of carbohydrate metabolism. During pregnancy, more glucose is required for both the woman and the baby. The body compensates for this need by suppressing the production of insulin.
There are other possible causes of gestational diabetes, such as autoimmune diseases that destroy the pancreas. In principle, any pathology of the pancreas can increase the risk of diabetes during pregnancy. nine0005
Risk of diabetes during pregnancy
This pathological condition threatens the health of both mother and child. Even before birth, the fetus begins to actively produce insulin to compensate for the increased glucose in the mother's blood. Such children are prone to low blood sugar from birth, they have a higher risk of obesity and type II diabetes in adulthood.
Gestational diabetes increases the risk of high blood pressure as well as preeclampsia, a severe form of preeclampsia. It is manifested by headaches, nausea, vomiting, visual disturbances, lethargy, drowsiness or insomnia. This is one of the most severe disorders during pregnancy, affecting the central nervous system. nine0003
It is manifested by headaches, nausea, vomiting, visual disturbances, lethargy, drowsiness or insomnia. This is one of the most severe disorders during pregnancy, affecting the central nervous system. nine0003
Another worrying factor is that diabetes during pregnancy contributes to rapid weight gain in the baby during the prenatal period (macrosomia). This causes difficulties in childbirth and poses a threat to the mother. A large child is considered to be over 4 kg. These children are at higher risk of birth injury and are more likely to need a caesarean section. Due to the large size of the fetus, an early delivery may be required. At the same time, the risk of preterm birth is high.
Also, high sugar in pregnant women increases the risk of cardiovascular and nervous pathologies of the fetus, increases the risk of respiratory distress syndrome in the baby (a condition that makes breathing difficult), and generally increases the incidence of complications during pregnancy and childbirth.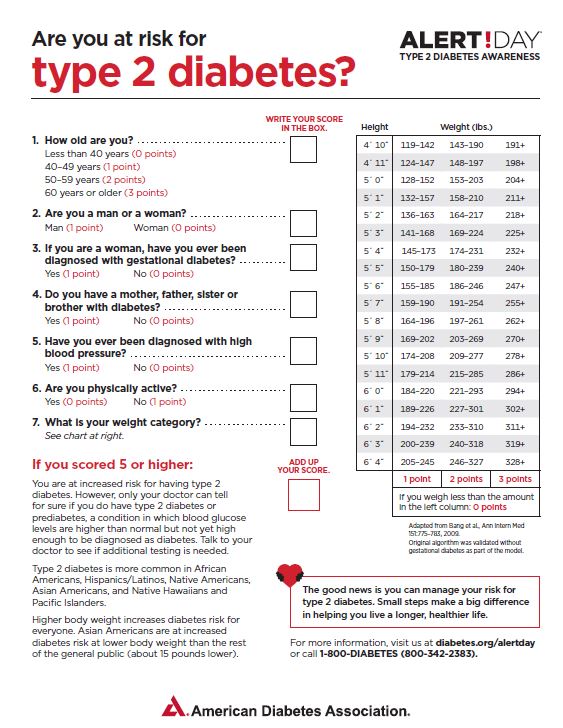 nine0005
nine0005
Risk factors for gestational diabetes
- Age under 18 and over 30 years of age.
- Unbalanced diet with a lot of fast carbohydrates.
- Bad habits (smoking, alcohol abuse).
- Overweight and obesity. Excess weight obviously implies a violation of metabolic processes.
- Lack of physical activity.
- Previous gestational diabetes or pre-diabetes. The tendency to diseases of this series does not disappear with time. nine0032
- Polycystic ovary syndrome.
- Diabetes in a close relative. The risk of gestational diabetes is doubled or more if close relatives have any form of diabetes.
- Previous birth of a child over 4 kg or a large fetus during the current pregnancy.
- Race. The Caucasian race has the lowest risk of developing gestational diabetes, most often black women suffer from this problem.
Unfortunately, GDM can also develop in a perfectly healthy woman without risk factors, so you need to visit a doctor and not skip the recommended screenings.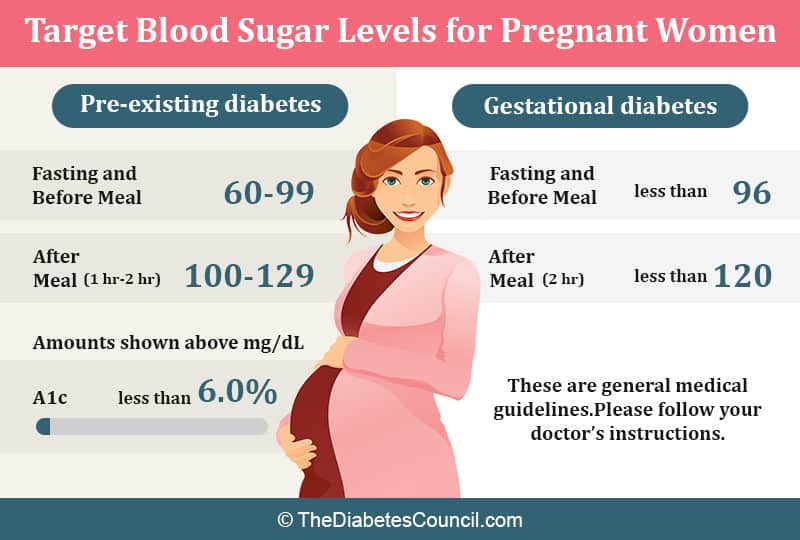 nine0003
nine0003
Symptoms of gestational diabetes
In most cases, the disease is asymptomatic for a long time, and this is its danger. Usually, the problem is detected after the 20th week of pregnancy through a blood sugar test.
Severe symptoms are rare and all non-specific: intense thirst, weight gain, increased daily urination. Sometimes patients complain of fatigue and lack of energy.
Diagnosis of gestational diabetes
There is also good news. All pregnant women, when registering, must take a blood test for glucose levels, therefore, if you regularly undergo all the prescribed examinations, you will find a problem at the very initial stage.
The normal value is 3.3-5.1 mmol / l in the analysis of blood from a vein on an empty stomach. Patients whose glucose level exceeds 5.1 mmol / l are at risk. In this case, the doctor will order a glucose loading test or a glucose tolerance test to confirm or refute the diagnosis.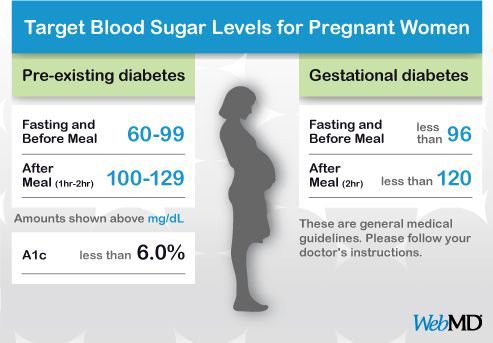 It is carried out at the 24-28th week of pregnancy. Such a study includes two stages: first, a woman takes a regular blood test for fasting glucose, after which she drinks a special solution containing 75 grams of glucose, and takes the test again two hours later. If a disease is suspected, the same analysis is repeated again after a few hours. nine0003
It is carried out at the 24-28th week of pregnancy. Such a study includes two stages: first, a woman takes a regular blood test for fasting glucose, after which she drinks a special solution containing 75 grams of glucose, and takes the test again two hours later. If a disease is suspected, the same analysis is repeated again after a few hours. nine0003
The diagnosis of gestational diabetes is made if the fasting blood glucose level is less than 7 mmol / l, but above 5.1 mmol / l, and the level of venous blood glucose two hours after ingestion of 75 g of glucose is above 8.5 mmol / l .
Prenatal diabetes treatment
The first step in treating GDM is a balanced diet and moderate exercise. The main goal of the diet is to reduce sugar to normal values, so the expectant mother will have to give up sweets and fast carbohydrates. nine0003
Recommended for pregnant women:
- Eat a little, but often.
- Avoid high glycemic foods (sugar, honey, potatoes, white bread, muffins, bananas, grapes).
- Refuse fast food and fatty sweet pastries.
- Drink plenty of fluids if there are no contraindications from the kidneys.
- Diversify the diet with fresh vegetables, lean meat, cereals.
Like all pregnant women, it is important for patients with GDM to receive the full range of vitamins and minerals that are necessary to maintain their own health and the proper development of the fetus. nine0003
Walking, swimming, water gymnastics, physiotherapy exercises for pregnant women - any light activity will benefit.
If diet and exercise fail to lower blood sugar levels, insulin therapy is indicated.
Important: Women with high blood sugar should check their glucose levels daily. Measurements are taken on an empty stomach and an hour after each meal using a home glucometer.
Prevention of gestational diabetes
Unfortunately, there are no 100% effective measures that would protect against this disease.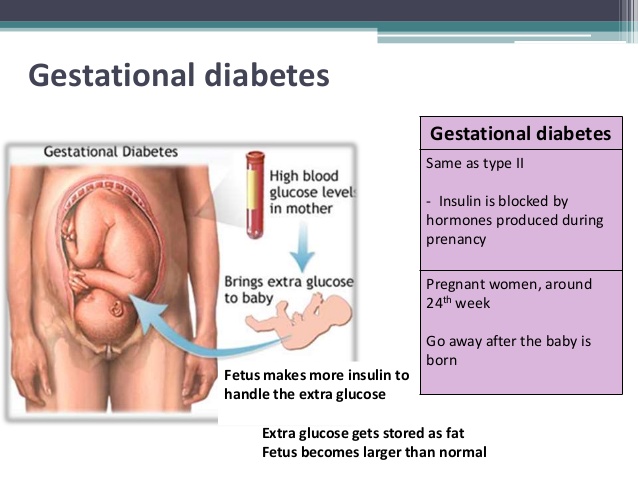
But the more good habits a woman develops before pregnancy, the easier pregnancy and childbirth will be:
- From the first days of pregnancy, eat healthy food: choose foods high in fiber and low in fat. Focus on vegetables and whole grains. Strive for variety and watch portion sizes. nine0031 Stay active. Try to do 30 minutes of exercise every day. Take daily walks, ride a bike, go swimming.
- Plan pregnancy at a healthy weight and do not gain more than recommended. Gaining weight too quickly can increase your risk of gestational diabetes.
Although there is no universal protection against GDM, a healthy lifestyle can reduce the risk of its occurrence. The most important thing is to detect the problem in time and prevent it from developing. nine0003
Dietary advice during pregnancy to prevent gestational diabetes
What is the problem?
Can dietary advice to pregnant women prevent the development of diabetes during pregnancy, known as gestational diabetes mellitus (GDM), which can cause health complications for women and their babies?
Why is this important?
Women with GDM have a higher risk of high blood pressure, protein in the urine (preeclampsia), and caesarean section. Their babies may grow large and, as a result, may be injured at birth or cause injury to their mothers during childbirth. In addition, there may be long-term health problems for women and their babies, including an increased risk of cardiovascular disease and type 2 diabetes. The number of women with this diagnosis is growing worldwide, so it is important to find simple and cost-effective ways to prevent the development of gestational diabetes. nine0003
Their babies may grow large and, as a result, may be injured at birth or cause injury to their mothers during childbirth. In addition, there may be long-term health problems for women and their babies, including an increased risk of cardiovascular disease and type 2 diabetes. The number of women with this diagnosis is growing worldwide, so it is important to find simple and cost-effective ways to prevent the development of gestational diabetes. nine0003
Carbohydrates are the main nutrient influencing post-meal blood glucose levels. The glycemic index (GI) can be used to characterize the ability of carbohydrate-based foods to raise blood glucose levels after consumption. Certain diets, such as those low in fiber and high in the GI of food, may increase the risk of developing GDM. It has been suggested that dietary advice during pregnancy may help in preventing the development of GDM in women. nine0003
What evidence did we find?
We searched for studies published up to 3 January 2016 and included 11 randomized controlled trials involving 2786 pregnant women and their infants.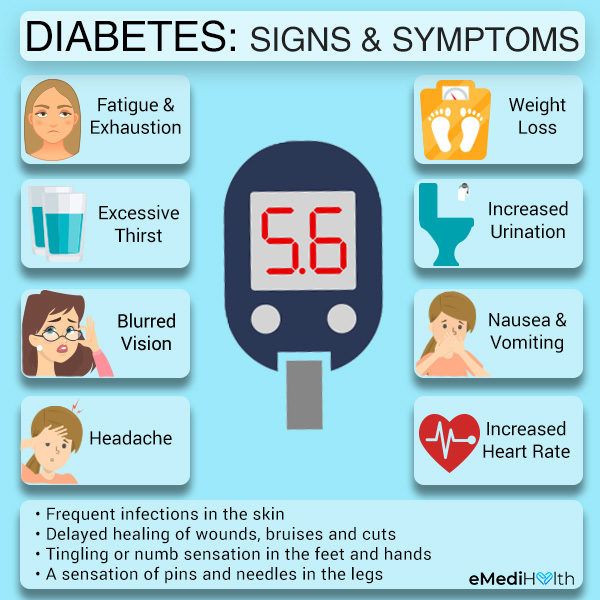 The quality of the evidence was rated as low to very low and the overall risk of trial bias was unclear to moderate. Six trials compared dietary recommendations with standard management, four compared low GI versus moderate-high GI dietary recommendations, and one trial compared high-fiber dietary recommendations with standard recommendations. nine0003
The quality of the evidence was rated as low to very low and the overall risk of trial bias was unclear to moderate. Six trials compared dietary recommendations with standard management, four compared low GI versus moderate-high GI dietary recommendations, and one trial compared high-fiber dietary recommendations with standard recommendations. nine0003
Possible reduction in GDM in women who received dietary advice compared to standard management in five clinical trials (1279 women, very low quality of evidence ), although between women who received dietary advice with low GI compared with average - high GI in four studies (912 women, low-quality evidence ) showed no clear difference in GDM. Two studies (282 women) showed no clear difference between women who received nutritional advice compared with standard care for preeclampsia ( low-quality evidence ), although fewer women with high blood pressure during pregnancy received dietary advice ( low-quality evidence ). There is no clear difference between the groups of women who received low-GI, moderate-high GI dietary advice in terms of the number of babies born above normal for their gestational age in the three studies (777 babies, low-quality evidence ). Only one study comparing dietary advice and standard management reported the number of infants who died (either before or shortly after birth) with no deaths in this trial. nine0003
There is no clear difference between the groups of women who received low-GI, moderate-high GI dietary advice in terms of the number of babies born above normal for their gestational age in the three studies (777 babies, low-quality evidence ). Only one study comparing dietary advice and standard management reported the number of infants who died (either before or shortly after birth) with no deaths in this trial. nine0003
There were no clear differences in most other outcomes assessed in clinical trials comparing dietary advice with standard medical management, including caesarean section, perineal injury, and infant skinfold thickness at six months. However, women who received dietary advice gained less weight during pregnancy in five trials (1336 women) ( low-quality evidence ).
Similarly, there are no clear differences in other outcomes found in clinical trials comparing low and moderate-high GI dietary recommendations, including caesarean section and weight gain during pregnancy.