Genetic screening before pregnancy
What You Need To Know – Forbes Health
Table of Contents
- What Is Genetic Testing Before Pregnancy?
- Should I Have Genetic Carrier Testing Done Before Getting Pregnant?
- What Genetic Conditions Can I Be Tested for?
- When Should I Have Genetic Carrier Testing Done?
- How Much Does Genetic Testing Cost?
- What If Some of My Test Results Come Back Positive?
{{ tocState.toggleTocShowMore ? 'Show more' : 'Show less' }}
Preconception testing, or genetic testing before pregnancy, involves screening parents for genetic disorders or abnormalities before trying to conceive. This can help people feel more informed about their own health history before making the choice to have a child.
After reviewing the results, doctors can help people identify fertility issues or potential health concerns before trying to conceive.
Here’s what you need to know about genetic testing before pregnancy, from the types of testing available to the costs involved.
featured partner offer
Partner Offers feature brands who paid Forbes Health to appear at the top of our list. While this may influence where their products or services appear on our site, it in no way affects our ratings, which are based on thorough research, solid methodologies and expert advice. Our partners cannot pay us to guarantee favorable reviews of their products or services
CoQ10 Liquid Capsules
- 120 mg of CoQ10 per liquid capsules
- Contains no starch, artificial coloring, preservatives, or flavoring
- Supports healthy egg quality for women
- Supports male fertility with improved sperm concentrations and count
Learn More
On Natalist's Website
What Is Genetic Testing Before Pregnancy?
Genetic testing is “very helpful for family planning, particularly in cases where you pick up genetic mutations you didn’t know existed,” says Debbra Keegan, M. D., an OB-GYN and the clinical director of third party reproduction for the Institute for Reproductive Medicine and Science in New Jersey.
D., an OB-GYN and the clinical director of third party reproduction for the Institute for Reproductive Medicine and Science in New Jersey.
Genetic testing, also known as carrier screening, is a test that can identify whether a person carries a gene for specific genetic disorders. There are two types of carrier screening—targeted and expanded. Targeted carrier screening involves testing for genetic disorders based on a person’s family history or ethnicity. In this case, blood, saliva or tissue samples are taken to look for certain conditions that may run in a person’s family. Expanded carrier screening involves testing for multiple genetic disorders regardless of ethnicity or family history.
Doctors may utilize their own screening panel, which often includes the most severe disorders that people would want to be aware of. Expanded screening is also done using a simple blood or saliva test, but has the capability of identifying hundreds of various disorders.
Upon receiving results, individuals will learn whether they carry an abnormal gene for a certain disorder or condition. Babies receive two copies of each gene—one from each parent—and if both copies for the specific condition do not work properly, the baby will inherit the condition. This is why parents can be carriers of a disorder without actually having the disorder themselves. If one parent is tested and identified as a carrier for a condition, the other parent is then tested to see if they are also a carrier. Reviewing the results with your doctor can help you to determine the best steps moving forward in trying to conceive.
Babies receive two copies of each gene—one from each parent—and if both copies for the specific condition do not work properly, the baby will inherit the condition. This is why parents can be carriers of a disorder without actually having the disorder themselves. If one parent is tested and identified as a carrier for a condition, the other parent is then tested to see if they are also a carrier. Reviewing the results with your doctor can help you to determine the best steps moving forward in trying to conceive.
Should I Have Genetic Carrier Testing Done Before Getting Pregnant?
The American College of Obstetricians and Gynecologists (ACOG) recommends carrier screenings for anyone who is planning to become pregnant or is currently pregnant. Ideally, testing should be done before conception so parents are aware of the risk of passing genetic conditions to their children. Although genetic testing cannot identify every possible issue, the goal is to provide people with enough information to make a decision about conception or pregnancy management.
Individuals have the right to meet with their doctor and explore their options before deciding to pursue genetic testing, says Alan Martinez, M.D., an OB-GYN and reproductive endocrinology and infertility specialist at the Reproductive Science Center of New Jersey. “Some patients may not believe it is right for them and may not want the information,” he explains. “Although [genetic testing] might be offered or recommended, the patients have the right to leave whatever happens up to chance.”
What Genetic Conditions Can I Be Tested for?
“We can now screen for over 500 different types of [disorders] depending on the company or test you are using,” says Dr. Keegan. “This gives us the opportunity to prevent the transmission of inherited genetic disorders through the technology available and a simple blood test.”
The ACOG recommends considering family history and ethnicity, in addition to the most common genetic conditions, when deciding which mutations to include. Parents may also benefit from genetic counseling, which is a service that helps people understand the results of their tests and make informed decisions throughout the process.
Parents may also benefit from genetic counseling, which is a service that helps people understand the results of their tests and make informed decisions throughout the process.
Here are some of the most common conditions identified through genetic carrier screening:
Cystic Fibrosis
There are currently almost 40,000 children and adults living with cystic fibrosis in the U.S[1]About Cystic Fibrosis. Cystic Fibrosis Foundation. Accessed 8/25/2022. . Cystic fibrosis is a disease that affects the lungs, pancreas and other organs. People who have cystic fibrosis have difficulties breathing. The mutation involved with cystic fibrosis causes a protein to not function correctly, which then causes mucus buildup in multiple organs throughout the body.
Fragile X Syndrome
About 1 in 7,000 males and about 1 in 11,000 females have fragile X syndrome, the most common cause of inherited intellectual disability[2]Data and Statistics on Fragile X Syndrome. Centers for Disease Control and Prevention. Accessed 8/25/2022. . Fragile X is associated with lower than average IQ, developmental delays and other co-occurring health conditions including seizures, autism, hyperactivity, attention difficulties and more.
Spinal Muscular Atrophy (SMA)
One in every 6,000 babies is born with spinal muscular atrophy, or SMA, which is a group of genetic disorders that cause a weakening of the muscles[3]Spinal Muscular Atrophy. Johns Hopkins Medicine. Accessed 8/25/2022. . Symptoms may vary, but people with SMA may require physical and occupational therapy, support devices such as wheelchairs or assistance with breathing. Symptoms generally worsen over time and there is no cure.
Tay-Sachs Disease
Although anyone can be a carrier, Tay-Sachs disease is more common for people of Ashkenazi Jewish ancestry, as one in every 27 members of the population is a carrier for the disease[4]Tay-Sachs Disease. Mount Sinai. Accessed 8/25/2022. . Symptoms may include deafness, blindness, seizures, decreased muscle tone, dementia and others.
Sickle Cell Disease
It is estimated that approximately 100,000 people in the U.S. have sickle cell disease[5]Sickle Cell Disease. Centers for Disease Control and Prevention. Accessed 8/25/2022. . This inherited condition is most common in Black or African American people but can affect any race. Sickle cell disease includes a group of red blood cell disorders that can cause acute chest syndrome, anemia, blood clots or infections.
Sickle cell disease includes a group of red blood cell disorders that can cause acute chest syndrome, anemia, blood clots or infections.
When Should I Have Genetic Carrier Testing Done?
Those who are thinking about trying to conceive, are currently pregnant or have experienced difficulties trying to conceive should ask their doctor about genetic carrier testing. Doctors may also recommend testing if the individual has had more than one miscarriage, a previous pregnancy or child with an inherited condition or the loss of a baby before one year of age.
If you have a family history of certain health issues, genetic carrier testing may also help you to identify the potential risks associated with passing a certain condition to a child.
“Just because a couple has healthy children doesn’t mean they shouldn’t elect to do [genetic testing] in the future,” says Dr. Martinez.
How Much Does Genetic Testing Cost?
The cost of DNA analysis has decreased in recent years, as technology utilized for genetic testing has become more advanced. Instead of conducting multiple separate tests, genetic testing can now be performed with a single blood or saliva test.
Instead of conducting multiple separate tests, genetic testing can now be performed with a single blood or saliva test.
Genetic carrier screening can cost between $100 and $2,000 depending on the type of testing being performed. Testing may be covered by your insurance if the tests are recommended by your physician, but if you have questions, it’s best to contact your insurance company to see what your plan might cover.
“It does depend on the insurance, but typically the routine, recommended screening is covered in women who are either pregnant or trying to get pregnant,” says Dr. Keegan.
What If Some of My Test Results Come Back Positive?
If test results come back positive for certain genetic conditions, prospective parents can analyze the results with their doctor and identify the risks of passing them on. Genetic counselors can also review results with people and assist them in exploring their options, if necessary. Individuals can then decide whether they would like to undergo the in vitro fertilization (IVF) process to ensure certain inherited conditions are not passed onto their children.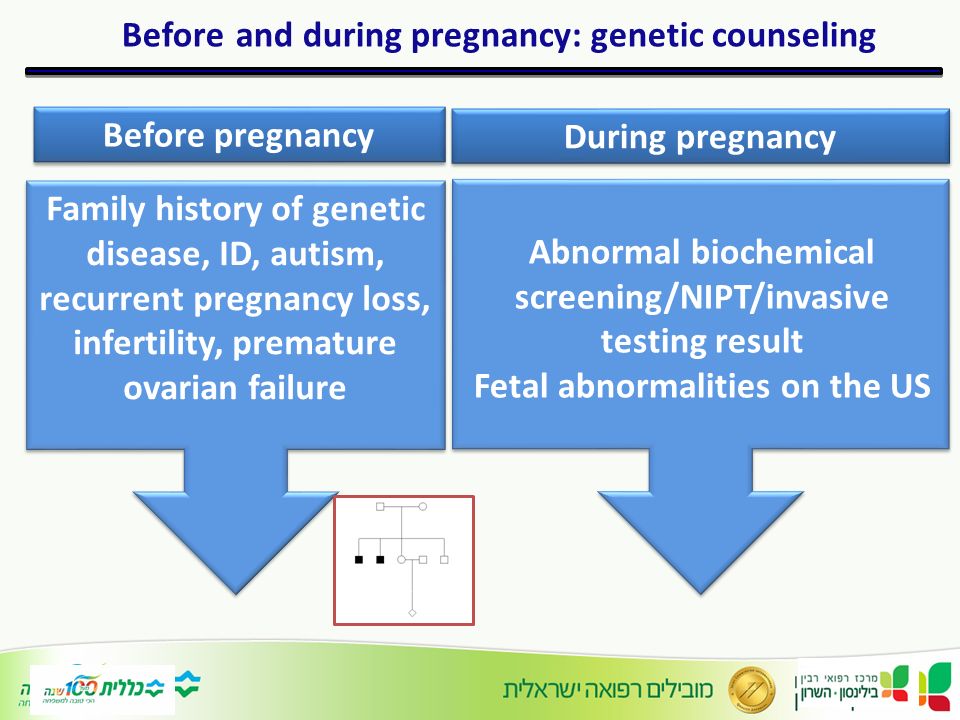
If parents decide to pursue IVF, they have the option of undergoing pre-implantation genetic testing (PGT). “Testing is applied to cells that are removed from the embryos,” explains Dr. Keegan. “With various genetic platforms, they can tell us what the status of the embryo is. The patient can then undergo an embryo transfer of the unaffected or potential donor embryo.” This ensures the fetus does not carry the unwanted genetic condition.
For some parents, a donor gamete—an egg or sperm cell—can be utilized if test results and personal choice deem it a viable option. “Patients will already have genetic information of the gamete when they go to make the purchase so they can make sure they are also negative for any mutations,” says Dr. Martinez. Same-sex couples, people who have had cancer or radiation or lower quality eggs may choose this option.
If you are interested in learning more about your personal genetic information, it is important to speak with your general practitioner, reproductive endocrinologist or OB-GYN. Your doctor can review your specific situation and recommend the next steps.
Your doctor can review your specific situation and recommend the next steps.
Family Health History and Planning for Pregnancy
Thinking about having a baby? If you have a family health history that includes a birth defect, developmental disability, newborn screening disorder, or genetic condition, you might be more likely to have a baby with this condition. Learning more about your family health history before you get pregnant can give you time to address any concerns. Remember to consider the family health history of both potential parents, not just mom. Be sure to discuss any concerns with your doctor.
Based on your family health history, your doctor might refer you for genetic counseling. Other reasons for genetic counseling include having had
- Infertility (trouble getting pregnant),
- 2 or more miscarriages,
- A previous pregnancy or child with a genetic condition or birth defect, or
- A baby who died at less than 1 year of age.

After genetic counseling, you might decide to have genetic testing for conditions that could affect your baby. Results from these tests could impact your pregnancy planning. Testing before you get pregnant can give you time to think about what the results mean for you and consider all your options.
Parents can have a baby with a genetic condition even though neither parent has it. Babies inherit two copies of each gene, one from each parent. For some genetic conditions, the baby will only have the condition if both copies of the gene related to the condition do not work properly. In cases like these, each parent has one copy of the gene that works properly and one that does not. If the baby inherits both non-working copies of the gene, the baby has the condition. Thus, the parents are “carriers” for the condition, meaning that they don’t have the condition themselves but can have children with it.
If a genetic condition runs in your family, you might be a carrier for that condition. Likewise, you might be a carrier for genetic conditions that are more common in your racial or ethnic group. Examples include sickle cell disease in Black people and Tay-Sachs disease in people of Ashkenazi and Eastern European Jewish descent. Your doctor might ask if you want to have screening, called carrier screening, to check if you are a carrier for conditions that are more common in your racial or ethnic group. Talk to your doctor if you want to know about carrier screening for genetic conditions that run in your family, such as fragile X syndrome. Current recommendations 1external icon state that all women should be offered carrier screening for cystic fibrosisexternal icon and spinal muscular atrophyexternal icon and should be checked for hemoglobinopathies such as sickle cell disease and thalassemia.
Likewise, you might be a carrier for genetic conditions that are more common in your racial or ethnic group. Examples include sickle cell disease in Black people and Tay-Sachs disease in people of Ashkenazi and Eastern European Jewish descent. Your doctor might ask if you want to have screening, called carrier screening, to check if you are a carrier for conditions that are more common in your racial or ethnic group. Talk to your doctor if you want to know about carrier screening for genetic conditions that run in your family, such as fragile X syndrome. Current recommendations 1external icon state that all women should be offered carrier screening for cystic fibrosisexternal icon and spinal muscular atrophyexternal icon and should be checked for hemoglobinopathies such as sickle cell disease and thalassemia.
If the results show that you are a carrier for a genetic condition, the other parent would also need to have carrier screening to know if you could have a baby with the condition.
1 Recommendations are from the American College of Obstetricians and Gynecologists and the American College of Medical Genetics
Family Health History Checklist: Planning a Pregnancy
□ Gather family history information before seeing the doctor.
□ Use the US Surgeon General’s online tool for collecting family histories, called “My Family Health Portrait.”
□ Tell your doctor if you have any family members with a genetic condition, chromosomal abnormality, developmental disability, birth defect, newborn screening disorder, or other problem at birth or during infancy or childhood, especially if you have had a previous pregnancy or child affected by one of these conditions.
o Talk to those family members, if possible, to find out their specific diagnoses.
o Ask for a copy of their genetic or diagnostic test results, if any, to share with your doctor.
□ Alert your doctor if you have had a previous premature birth, miscarriage, stillbirth, or a child who died from sudden infant death syndrome (SIDS).
□ Follow your doctor’s recommendations. For example, if you have had a previous pregnancy or child affected by spina bifida or anencephaly, your doctor might recommend that you take a higher than normal dose of the B vitamin, folic acid, before and during pregnancy.
Genetic tests when planning a pregnancy
You are planning a pregnancy . This already indicates that you, as future parents, are consciously and responsibly approaching the birth of a healthy child and are an adherent of a new developing trend in young families - a preventive course in family health.
Your next step is to get a professional answer to the question of how to properly prepare for conception and the development of a trouble-free, safe pregnancy, and, finally, for childbirth without complications.
Your reliable mentor in preparing for pregnancy is, of course, your doctor, the OB/GYN. Here begins the first stage of preparation - pregravid counseling ( Latin "gravida" - pregnancy ). Next, the doctor will draw up an individual preconception program for your couple.
Next, the doctor will draw up an individual preconception program for your couple.
The main task of such a program is to assess the health of future parents, correct existing disorders if necessary, and recommend a healthy lifestyle. And all this in order for the couple to enter the gestational period in the best state of health and complete psychological readiness.
Do not forget that the share of genetic causes in reproductive failures is quite high. Their consequence may be an interrupted pregnancy, intrauterine fetal death, the birth of a child with a severe genetic disease, malformations of intrauterine development.
Therefore, we recommend that all couples preparing to conceive undergo medical genetic counseling and, if necessary, additional genetic tests.
A geneticist will assess the personal genetic risks for your couple and answer the main questions:
- Is it possible for your couple to conceive naturally in order to have a healthy child?
- Will there be problems with bearing a child?
- Is there and what is the risk of having a child with hereditary diseases?
When preparing for pregnancy, do not ignore the geneticist's office, especially if you have:

Things to know when planning a pregnancy:
- It is wrong to think that preconception preparation concerns only the expectant mother. It is necessary for both future parents to go through it, since both a man and a woman are equally responsible for the health of the child, both in terms of their own general somatic health, and in terms of the transmitted genetic load.
- Unawareness of future parents of their own genetic status can lead to severe reproductive failure. Examples: lack of conception, early miscarriages, fetal malformations, hereditary diseases in a child, intrauterine fetal death, pregnancy complications such as fetoplacental insufficiency, preeclampsia, premature detachment of a normally located placenta, and others.
- Pregnancy and childbirth in women younger than 19 and older than 35 years are associated with an increased likelihood of various complications for the mother and fetus. In preparation for pregnancy, such patients are differentiated into a risk group.
- Women with a burdened gynecological and somatic history not only have a worse prognosis for the onset and gestation of pregnancy, but also an increased risk to their own health associated with pregnancy.
- Also, to reduce the risk of reproductive failure, the optimal intergenetic (interpartum) interval should be adhered to. Too short an interval between successive births, or vice versa, excessive elongation, significantly increases the risk of developing various congenital malformations, preterm birth.
In our center, preparing for pregnancy, you can undergo the following genetic examination:
- examine your own karyotype (karyotyping - evaluation of the chromosome set for the presence of chromosomal defects). A number of chromosomal defects in parents, without affecting their state of health in any way, can be the cause of a chromosomal disease in an unborn child;
- evaluate the histocompatibility of a couple to predict and prevent miscarriage;
- identify or eliminate the predisposition of your hemostasis system to thrombophilic complications during pregnancy. As you know, among them are premature detachment of a normally located placenta, fetoplacental insufficiency, gestosis, chronic miscarriage, and even stillbirth;
As you know, among them are premature detachment of a normally located placenta, fetoplacental insufficiency, gestosis, chronic miscarriage, and even stillbirth;
- to determine the degree of genetic contribution to your folate metabolism. It is known that folic acid deficiency during pregnancy can provoke miscarriage, fetal death, the birth of a child with isolated neural tube defects, anomalies of the limbs, ears, urinary system, cleft palate, omphalocele, defects of the cardiovascular system. In men, folic acid affects the quantity and genetic quality of spermatozoa;
- determine your predisposition to preeclampsia, one of the most dangerous complications of pregnancy;
- in order to prevent the birth of a child with a hereditary monogenic disease (examples of the most common: cystic fibrosis, phenylketonuria, spinal amyotrophy, sensorineural hearing loss), we recommend that future parents be tested for monogenic diseases. You can find it in the section "Prevention of diseases".
Genetic testing for pregnancy planning
Karyotyping of one or both spouses
Karyotyping is a study of a quantitative set of chromosomes, as well as their structural rearrangements (chromosomal aberrations). Rearrangements can be intra- and interchromosomal, may be accompanied by a violation of the order of chromosome fragments (deletions, duplications, inversions, translocations). Chromosomal rearrangements are divided into:
- Balanced. And inversions, reciprocal translocations do not lead to the loss or addition of genetic material, so their carriers are usually phenotypically normal.
- Unbalanced. Deletions and duplications change the dose ratio of genes, and, as a rule, their carriage is associated with significant deviations from the norm.
A healthy person should have 22 pairs of autosomes and 1 pair of sex chromosomes (XX or XY). For couples suffering from infertility, karyotyping is prescribed rather because of reinsurance, its appointment is more justified in recurrent miscarriage, especially if it was associated with proven aneuploidy of the embryo / s.
In infertile patients, chromosomal rearrangements are rare. With recurrent miscarriage, balanced rearrangements are more common, but occupy only 4-5% in the structure of the causes of recurrent miscarriage. At the same time, such patients always have a chance to have a healthy baby without expensive examination and treatment. Without appropriate research and treatment, the risks of recurrent miscarriage and the birth of a child with severe manifestations of an unbalanced translocation exist, but they are quite low.
Since the analysis is carried out on a commercial basis, the couple should understand that the detection of karyotype disorders will entail a recommendation to do pre-implantation genetic diagnosis of embryos (PGD) for a specific chromosome breakage, as well as PGT-A to rule out numerical chromosomal abnormalities in embryos.
Screening of one or both spouses for the most common monogenic diseases
This screening can be safely offered to all couples. Why? We are all carriers of at least a few autosomal recessive monogenic diseases. As a rule, we do not know about this, since the second gene from the paired chromosome from the other parent is not broken, and the disease does not manifest itself in any way. If spouses are carriers of the same disease, then the risk of having a sick child is 25%.
Why? We are all carriers of at least a few autosomal recessive monogenic diseases. As a rule, we do not know about this, since the second gene from the paired chromosome from the other parent is not broken, and the disease does not manifest itself in any way. If spouses are carriers of the same disease, then the risk of having a sick child is 25%.
In this regard, some donor cell banks test all their donors for the most common monogenic diseases in the population. Obviously, screening is also a safe bet, and that the risk of having a sick child is low (no higher than 1 in 1,000). But if suddenly, as a result of IVF using donor cells or a perfectly healthy couple, a child is born with an incurable genetic disease with severe manifestations, then the consequences will be dire.
If you still doubt whether you should take this test, at least rule out the carriage of SMA, spinal muscular atrophy! The main panel also includes sensorineural hearing loss, cystic fibrosis, phenylketonuria, adrenogenital syndrome.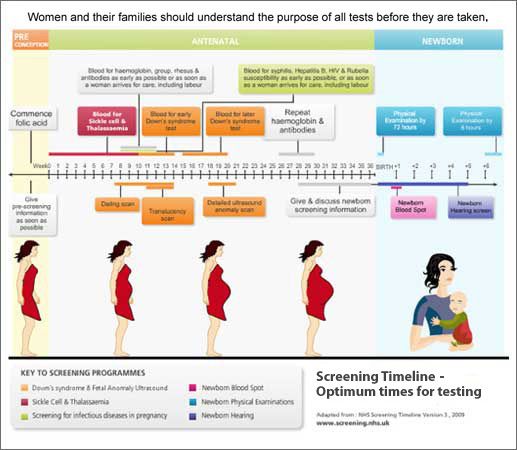
Cystic Fibrosis Mutation (CFTR) Genetic Tests and AZF Mutations
In severe forms of male infertility (azoospermia or significant oligozoospermia, less than 5 million spermatozoa in 1 ml of semen repeatedly), andrologists usually prescribe additional genetic tests for cystic fibrosis mutations (CFTR) and AZF mutations.
If a carrier of cystic fibrosis is detected, it is recommended to examine the partner for the same disease (remember that if partners have the same mutation, the probability of having a sick child in a couple is 25%).
If an AZF mutation is detected, IVF with PGT-A and female embryo transfer are recommended, since the boy will inherit the same mutation (the Y chromosome will inevitably be inherited from his sick father), and the child will also be infertile.
Examination for repetitions in the FMR1 gene (Fragile X Syndrome)
With a low ovarian reserve (AMH less than 1 ng / ml) in women under 35 years of age and premature ovarian failure (cessation of menstruation before 40 years of age), a woman is usually examined for repetitions in the FMR1 gene (this is a fragile (fragile) X chromosome syndrome).