Medical reasons for c section
Medical reasons for a c-section
A c-section is a surgery in which your baby is born through a cut that your doctor makes in your belly and uterus.
A c-section may be needed to protect the health of your or your baby. In these cases, a c-section may be safer than vaginal birth.
Your provider may want to schedule your c-section if there are problems during pregnancy that make vaginal birth risky.
If your pregnancy is healthy and you don’t have medical reasons for a c-section, it’s best to have your baby through vaginal birth.
What is a c-section?
A c-section (short for cesarean birth) is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. For some women and babies, a c-section is safer than vaginal birth. If you have medical conditions that affect your pregnancy, you may need a c-section to protect the health of your baby.
A c-section may be planned (also called scheduled). This means you and your health care provider decide when to schedule the c-section based on your health condition and the condition of your baby. Or a c-section may be an emergency. An emergency c-section has to be done immediately because your health or your baby’s health is in danger.
If there are medical reasons to schedule your c-section, talk to your provider about waiting until at least 39 weeks of pregnancy. This gives your baby the time she needs to grow and develop before birth. Scheduling a c-section should be for medical reasons only.
What are medical reasons for a c-section?
You may need a c-section because of complications that make vaginal birth unsafe for you or your baby. For example:
Complications during pregnancy
- You’ve had a c-section in the past or you’ve had other surgeries on your uterus (womb). The more c-sections you have, the greater your risk for pregnancy complications. Some women can safely have a vaginal birth after they’ve had a c-section.
 This is called a VBAC. If you’ve had a c-section in the past, talk to your provider to see if VBAC may be possible in your next pregnancy.
This is called a VBAC. If you’ve had a c-section in the past, talk to your provider to see if VBAC may be possible in your next pregnancy. - There are problems with the placenta, such as placenta previa, which can cause dangerous bleeding during vaginal birth. The placenta grows in your uterus and supplies the baby with food and oxygen through the umbilical cord.
- You have an infection, like HIV or genital herpes. You can pass these infections to your baby during vaginal birth. So a c-section is safer for your baby.
- You have a medical condition that may make vaginal birth risky, like diabetes or high blood pressure. Diabetes is when you have too much sugar in your blood. This can damage organs in your body, like blood vessels and nerves. High blood pressure is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy.
- You’re having multiples (twins, triplets or more).
Complications that affect your baby and labor and birth
- Your labor doesn’t progress.
 This means it’s too slow or stops.
This means it’s too slow or stops. - Your baby is very large.
- Your baby isn’t in a head-down position for birth. If your baby is in a breech position, it means his bottom or feet are facing down. A transverse position is when your baby’s shoulder is facing down. Some babies can be turned in the womb to move into a head-down position. But a c-section may be safer for your baby.
- The umbilical cord is pinched or you have umbilical cord prolapse. This is when the umbilical cord slips into the vagina before the baby.
- Your baby is in distress. This means he isn’t getting enough oxygen or his heartbeat may not be regular.
- Your baby has certain birth defects, like severe hydrocephalus. This is when fluid builds up on your baby’s brain. It can cause a baby’s head to be very large. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works.
What are the risks of scheduling a c-section for non-medical reasons?
Scheduling a c-section may cause problems for you and your baby because your due date may not be exactly right. Sometimes it’s hard to know exactly when you got pregnant. If you schedule a c-section and your due date is off by a week or 2, your baby may be born too early. Babies born early (called premature babies) may have more health problems at birth and later in life than babies born on time. This is why it’s important to wait until at least 39 weeks for a scheduled c-section.
If your pregnancy is healthy, it’s best to let labor begin on its own. If your provider talks to you about scheduling a c-section, ask if you can wait until at least 39 weeks to have your baby. This gives your baby’s lungs and brain all the time they need to fully grow and develop before he’s born.
If there are problems with your pregnancy or your baby’s health, you may need to have your baby earlier than 39 weeks. In these cases, your provider may recommend an early birth because the benefits outweigh the risks. Having a c-section before 39 weeks of pregnancy is recommended only if there are health problems that affect you and your baby.
In these cases, your provider may recommend an early birth because the benefits outweigh the risks. Having a c-section before 39 weeks of pregnancy is recommended only if there are health problems that affect you and your baby.
If your provider recommends scheduling a c-section, ask these questions:
- Why do I need to have a c-section?
- Is there a problem with my health or the health of my baby makes it necessary to have my baby before 39 weeks? Can I wait to have my baby closer to 39 weeks?
- What problems can a c-section cause for me and my baby?
- What will my recovery be like?
- Can I have a vaginal birth in future pregnancies?
Last reviewed: October, 2018
See also: 39 weeks infographic
Reasons for a C-Section: Medical and Elective
One of the first major decisions you’ll make as a mom-to-be is how to deliver your baby.
While a vaginal delivery is considered safest, doctors today are performing cesarean deliveries more often.
A cesarean delivery — also called a C-section — is a common but complicated procedure that poses health risks for mom and baby.
Although cesarean deliveries are common and generally safe, they have more risks than delivering a baby vaginally. For this reason, vaginal births are recommended. But it’s possible to schedule a cesarean delivery in advance for medical reasons.
For example, if your baby is breech and doesn’t change position as your due date approaches, your doctor may schedule a cesarean delivery. Additionally, cesarean deliveries are usually scheduled for the medical reasons listed below.
It’s also possible to schedule a cesarean delivery for nonmedical reasons, but this isn’t recommended. A cesarean delivery is major surgery and there’s a greater risk for complications, including:
- blood loss
- organ damage
- allergic reaction to anesthesia
- infections
- blood clots
A scheduled surgery for nonmedical reasons is called an elective cesarean delivery, and your doctor may allow this option.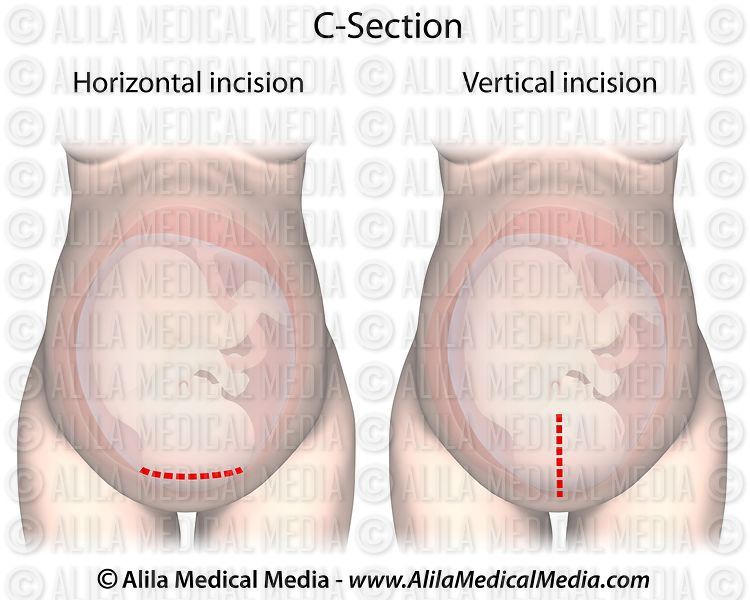 Some women prefer to deliver by surgery because it gives them more control in deciding when their baby is born. It can also reduce some anxiety of waiting for labor to start.
Some women prefer to deliver by surgery because it gives them more control in deciding when their baby is born. It can also reduce some anxiety of waiting for labor to start.
But just because you’re given the option of an elective cesarean delivery doesn’t mean it comes without risks. There are pros to a scheduled cesarean delivery, but there are also cons. Some health insurance plans also will not cover elective cesarean deliveries.
Pros of an elective C-section
- Lower risk of incontinence and sexual dysfunction after the birth of the baby.
- Lower risk of the baby being deprived of oxygen during delivery.
- Lower risk of the baby experiencing trauma while passing through the birth canal.
Cons of an elective C-section
- You’re more likely to need a repeat cesarean delivery with future pregnancies.
- There’s a higher risk of complications with cesarean deliveries.
- You’ll have a longer hospital stay (up to five days) and a longer recovery period.
A cesarean delivery might be scheduled by your doctor in advance of your due date. Or it may become necessary during labor because of an emergency.
Below are some of the most common medical reasons for a cesarean.
Prolonged labor
Prolonged labor — also called “failure to progress” or “stalled labor”— is the reason for nearly one-third of cesareans, according to the Centers for Disease Control and Prevention. It happens when a new mom is in labor for 20 hours or more. Or 14 hours or more for moms who’ve given birth before.
Babies that are too large for the birth canal, slow cervical thinning, and carrying multiples can all prolong labor. In these cases, doctors consider a cesarean to avoid complications.
Abnormal positioning
In order to have a successful vaginal birth, babies should be positioned headfirst near the birth canal.
But babies sometimes flip the script. They can position their feet or butt toward the canal, known as a breech birth, or position their shoulder or side first, known as a transverse birth.
A cesarean may be the safest way to deliver in these cases, especially for women carrying multiple babies.
Fetal distress
Your doctor may choose to deliver via emergency cesarean if your baby is not getting enough oxygen.
Birth defects
To reduce delivery complications,doctors will choose to deliver babies diagnosed with certain birth defects, like excess fluid in the brain or congenital heart diseases, through a cesarean to reduce delivery complications.
Repeat cesarean
About 90 percent of women who’ve had a cesarean can deliver vaginally for their next birth, according to the American Pregnancy Association. This is known as vaginal birth after cesarean (VBAC).
Moms-to-be should talk with their physician to decide whether a VBAC or repeat cesarean is the best and safest option.
Chronic health condition
Women may deliver via cesarean if they live with certain chronic health conditions like heart disease, high blood pressure, or gestational diabetes. Vaginal delivery with one of these conditions may be dangerous for mom.
Vaginal delivery with one of these conditions may be dangerous for mom.
Doctors will also suggest a cesarean if the mom-to-be has HIV, genital herpes, or any other infection that could be transferred to the baby through vaginal delivery.
Cord prolapse
When the umbilical cord slips through the cervix before the baby is born, it’s called a cord prolapse. This can lessen blood flow to the baby, putting the baby’s health at risk.
While rare, a cord prolapse is a serious condition that requires an emergency cesarean delivery.
Cephalopelvic disproportion (CPD)
A CPD is when a mom-to-be’s pelvis is too small to deliver the baby vaginally, or if the baby’s head is too large for the birth canal. In either case, the baby can’t pass through the vagina safely.
Placenta issues
Doctors will perform a cesarean when the low-lying placenta partially or completely covers the cervix (placenta previa). A cesarean is also necessary when the placenta separates from the uterine lining, causing the baby to lose oxygen (placenta abruption).
According to the American Pregnancy Association, placenta previa happens to 1 in every 200 pregnant women. About 1 percent of pregnant women experience placental abruption.
Carrying multiples
Carrying multiples can pose different risks during pregnancy. It can cause prolonged labor, which can put mom in distress. One or more babies may also be in an abnormal position. Either way, a cesarean is often the safest route for delivery.
Since pregnancy and birth can be unpredictable at times, moms-to-be should be prepared in case a cesarean delivery is necessary. Giving birth is a beautiful and miraculous thing, and it’s best to be as prepared for the unexpected as possible.
Q:
Why are so many more women today scheduling elective C-sections? Is this a dangerous trend?
Anonymous patient
A:
The trend in elective cesarean deliveries is growing. One study showed that 8 percent of mothers requested an elective cesarean delivery. While popular, this trend can have serious complications, including the risk of blood loss, infection, blood clots, and adverse reactions to anesthesia. It’s important to remember that a cesarean delivery is a major abdominal surgery, and typically has a longer recovery than a vaginal delivery. If you’re thinking about scheduling an elective cesarean delivery, you should talk to your doctor more about the risks and benefits.
While popular, this trend can have serious complications, including the risk of blood loss, infection, blood clots, and adverse reactions to anesthesia. It’s important to remember that a cesarean delivery is a major abdominal surgery, and typically has a longer recovery than a vaginal delivery. If you’re thinking about scheduling an elective cesarean delivery, you should talk to your doctor more about the risks and benefits.
Katie Mena, MDAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
One thousand and one indications for caesarean section. Part 2
Many women whose babies are about to be born will be offered a caesarean section. If we undertake to analyze all possible situations, the information will take up volumes. There are several ways to classify the causes for being born "upper way". We will try to separate absolute and relative indications for surgery.
Cases in which there are absolute indications for caesarean section are extremely rare. More frequent relative indications depend to a large extent on factors as diverse as the personality, age and professional experience of the midwife and doctor; the country where the child is born, the protocols and accepted norms existing in this clinic; character, lifestyle, family environment and circle of friends of the expectant mother; the latest research published in reputable medical journals and media coverage, data obtained from popular websites, etc. This is why caesarean section rates vary so much from obstetrician to obstetrician, clinic to clinic, and country to country.
The presence of a scar on the uterus (usually after a previous caesarean section) is an example of a relative and debatable indication: the frequency of operative delivery for this reason has increased and decreased at various periods in the history of childbearing. Today, general attention is drawn to the risk of stillbirth for an unexplained reason, although its absolute risk is very small. The presence of a history of caesarean section is such a common situation and such an urgent problem that we will consider it separately.
The presence of a history of caesarean section is such a common situation and such an urgent problem that we will consider it separately.
- "Lack of progress during labor." often cited as the reason for the first caesarean section. In most cases, the lack of progress in childbirth is due to the widespread misunderstanding of the physiology of childbirth in our time. It will take decades to re-understand that humans are mammals and their key need for childbirth is peace and privacy. It will take decades to understand that the midwife is, first of all, a figure like a mother, that is, a person next to whom you feel safe, who does not scrutinize or criticize us. Under the current circumstances, it would be dangerous to make it a priority to reduce the frequency of caesarean sections. The immediate consequences of this will be an increase in the number of dangerous interventions in vaginal delivery and an increase in the number of newborns in need of pediatric care. In the meantime, we must recognize that in the age of industrialized childbirth, most caesarean sections are completely justified, and the lack of progress in childbirth is the most common indication for surgery.
- Mismatch between the size of the pelvis and the head of the fetus. simply means that the baby's head is too big to fit through the pelvic bones. This is a vague concept, because the correspondence between the size of the baby's head and the mother's pelvis depends to a large extent on the exact position of the head and how it "configures" during childbirth. In the case when a decision is made to perform a caesarean section in childbirth, it can be difficult to distinguish between a mismatch in the size of the pelvis and the head of the fetus and a “lack of progress in childbirth”: in the same circumstances, a woman can be arbitrarily named as the reason for either the first or the second.
- Suffering (distress) of the fetus. It is also a vague concept, since different specialists use different criteria to diagnose this condition. Suffering of the fetus often occurs in the absence of progress in childbirth. As a result, it can be difficult to separate these two indications for caesarean section.
 Currently, labor induction is one of the main risk factors for the complex of complications that will later be recorded in the history of childbirth as weakness of labor activity, mismatch in the size of the fetal head and mother's pelvis, or fetal distress.
Currently, labor induction is one of the main risk factors for the complex of complications that will later be recorded in the history of childbirth as weakness of labor activity, mismatch in the size of the fetal head and mother's pelvis, or fetal distress.
Uterine fibroids and ovarian cysts are not absolute indications, unless they are very large or low-lying, which prevents the child from passing through the birth canal.
A history of anal sphincter tear is also a relative indication for caesarean section. According to an American study, caesarean section prevents fecal incontinence in only one out of two women who had a sphincter tear during childbirth. Breech (breech) presentation is a typical example of how a single article published in the medical literature can turn the whole world upside down overnight. It can be said without exaggeration that the turning point in the history of childbirth in the breech presentation was the day of October 21, 2000. On this day, the Lancet, one of the world's most respected medical journals, published the results of a major study conducted in 121 clinics in 26 countries. It has great scientific value, as it was randomized: scientists randomly divided pregnant women into two groups and were able to compare the outcome of a planned caesarean section and vaginal delivery.
It has great scientific value, as it was randomized: scientists randomly divided pregnant women into two groups and were able to compare the outcome of a planned caesarean section and vaginal delivery.
Only pure breech and mixed breech presentation have been studied. Pure breech presentation is the position of the fetus in the uterus, in which the child's legs are bent at the hip and unbent at the knee joints, that is, the legs are extended along the body. With a mixed breech presentation, the child's legs are bent both at the knees and at the hip joints, but are located above the buttocks, that is, the baby seems to be sitting in Turkish. Cases of foot presentation, when one or two legs are located below the buttocks, were excluded from the study. Here is the conclusion of the authors: “For a full-term baby in the breech presentation, a planned caesarean section had a more favorable outcome than a planned vaginal delivery; severe complications in mothers occurred with the same frequency in both groups.
From that day on, it became difficult to find an obstetrician who would take on the responsibility of delivering a breech birth through the birth canal. A common tactic is to try to rotate the baby 3-4 weeks before the expected birth. If this fails, a planned caesarean section is recommended.
In view of the widespread misunderstanding of the physiology of childbirth, it must be admitted that in most cases today it is better to have a caesarean section than to try to give birth on your own surrounded by frightened doctors. This will continue until we recognize the core needs of the woman giving birth, in particular the need for peace and privacy. There are women who are not fundamentally against a caesarean section, but, intuitively or rationally, feel that it would be better for the child to wait for the onset of labor. This view is shared by many pediatricians, who emphasize that the risk of respiratory problems in a child is lower after a "caesarean section in childbirth. " We must keep in mind that one of the declared advantages of giving birth in a hospital is the ability to perform the operation at any time, day or night. It is often claimed that emergency caesarean section is associated with a higher risk of maternal complications compared to elective surgery. But do not confuse "caesarean section in childbirth" with an emergency caesarean section.
" We must keep in mind that one of the declared advantages of giving birth in a hospital is the ability to perform the operation at any time, day or night. It is often claimed that emergency caesarean section is associated with a higher risk of maternal complications compared to elective surgery. But do not confuse "caesarean section in childbirth" with an emergency caesarean section.
Today we should also think about those women who, despite all the difficulties, strive to avoid a caesarean section and give birth naturally. Here are a few simple rules of thumb that I've gradually learned from my own experience of about 300 breech births (including two home births): and silent, who tries not to attract attention and is not afraid to take birth in a breech presentation.

This breech delivery approach can significantly reduce the overall caesarean section rate, as breech presentation occurs in 3% of full-term pregnancies. Now more and more caesarean sections are done in the case of twins. One of the reasons is that in 40% of cases, one of the twins is in a breech presentation, and in 8% of cases, both. Even more often, caesarean section is indicated in cases where one of the children is much larger than the other: this situation is potentially dangerous for a child with a smaller weight, especially if the children are of the same sex. The idea of a planned caesarean section in the case of twins may discourage those who are most concerned about the danger of having a premature baby. Also occasionally there are situations when the second child has to be helped to be born by caesarean section after the first was born naturally. The birth of a second child from twins often seems to be more risky than the first. One of the reasons is the unhealthy turmoil that occurs every time in the delivery room immediately after the birth of the first child, at the very time when it is so important to maintain an atmosphere of reverence, at least until the second child and the placenta are born. This is another modern trend related to the widespread misunderstanding of the role of peace and solitude (privacy).
The idea of a planned caesarean section in the case of twins may discourage those who are most concerned about the danger of having a premature baby. Also occasionally there are situations when the second child has to be helped to be born by caesarean section after the first was born naturally. The birth of a second child from twins often seems to be more risky than the first. One of the reasons is the unhealthy turmoil that occurs every time in the delivery room immediately after the birth of the first child, at the very time when it is so important to maintain an atmosphere of reverence, at least until the second child and the placenta are born. This is another modern trend related to the widespread misunderstanding of the role of peace and solitude (privacy).
Today, triplets are almost always delivered by caesarean section, although this practice has been questioned from time to time. Cases of independent triplets are described... including at home after a previous caesarean section!
There is also an upward trend in caesarean sections among HIV-infected women.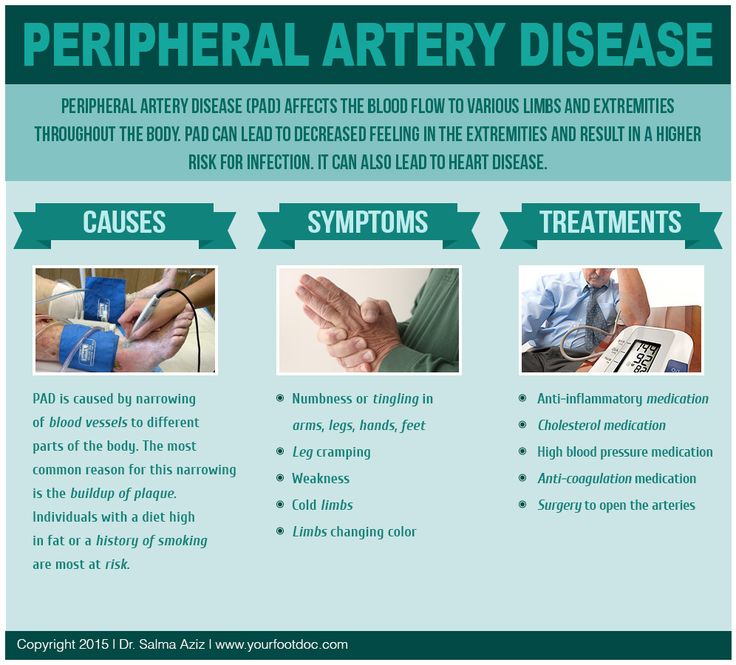 The goal is to reduce the risk of transmission of the virus from mother to child. This indication is yet another example of how routine practice can change overnight in this age of evidence-based medicine. From 19Between 1994 and 1998, about 20% of HIV-infected women in the United States had caesarean sections. In 1998, a study was published that showed that the risk of infection in a child is significantly reduced if vaginal delivery is avoided. After that, between 1998 and 2000, the caesarean section rate in this situation rose to 50%. It is likely to increase further with the advent of new technology that protects the child from any contact with maternal blood.
The goal is to reduce the risk of transmission of the virus from mother to child. This indication is yet another example of how routine practice can change overnight in this age of evidence-based medicine. From 19Between 1994 and 1998, about 20% of HIV-infected women in the United States had caesarean sections. In 1998, a study was published that showed that the risk of infection in a child is significantly reduced if vaginal delivery is avoided. After that, between 1998 and 2000, the caesarean section rate in this situation rose to 50%. It is likely to increase further with the advent of new technology that protects the child from any contact with maternal blood.
The herpes virus can also be transmitted to the baby during childbirth through natural routes. Most often, herpes infection is recurrent. This means that the woman already had exacerbations before pregnancy. In this case, there is almost no risk of infection, since the mother has managed to form antibodies that cross the placenta (IgG), which can protect the baby. The risk is more significant in those rare cases when the primary infection of the mother occurred during pregnancy, when she has time to form only IgM class antibodies that do not pass through the placenta. In this case, caesarean section can reduce the risk of transmission of the virus.
The risk is more significant in those rare cases when the primary infection of the mother occurred during pregnancy, when she has time to form only IgM class antibodies that do not pass through the placenta. In this case, caesarean section can reduce the risk of transmission of the virus.
What about frail babies, especially premature ones, and those who are called "underweight", "out of gestational age"? So much conflicting data has been published that any doctor can always find an article in support of his point of view. What about the "special children" who were born as a result of long-term fertility treatment using the latest methods of artificial insemination? What about other "special" babies born shortly after an unexplained fetal death in a previous pregnancy?
In the future, if we don't get back to understanding the key needs of a woman in childbirth, it will probably be easier and faster to consider the remaining reasons for deciding to have a vaginal birth than to try to analyze a thousand and one possible indications for a caesarean section.
Michel Auden
caesarean section chapter 13
caesarean section should only be performed if medically indicated
Caesarean section should only be performed if medically indicated.- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find Country »
- A
- B
- C
- D
- D
- E
- Y С
- and
- th
- to
- l
- m
- N
- O
- P
- 9000
- T
- F 9000 9000 9000 9
- Sh
- Sh
- b
- S
- b
- E
- Yu
- I
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Press releases/
- item/
- Caesarean section should only be performed if medically indicated
\n
\nA caesarean section may be necessary in cases where vaginal delivery could pose a risk to the mother or baby, such as prolonged labor, distress, or fetal presentation. At the same time, caesarean section can lead to serious complications, disability or death, especially in the absence of opportunities to safely perform surgical interventions or treat possible complications.
At the same time, caesarean section can lead to serious complications, disability or death, especially in the absence of opportunities to safely perform surgical interventions or treat possible complications.
\n
Impact on reducing maternal and child mortality
\n
\nSince 1985, it has been accepted in the international health community that the ideal caesarean section rate is 10-15%. Findings from new studies show that if caesarean section rates increase to 10% at the population level, maternal and neonatal mortality rates decrease. However, if the frequency of its implementation exceeds 10%, the available data do not indicate an improvement in mortality rates.
\n
\n“These findings highlight the importance of caesarean section in saving maternal and newborn lives,” says Dr Marleen Temmerman, Director of the WHO Department of Reproductive Health and Research.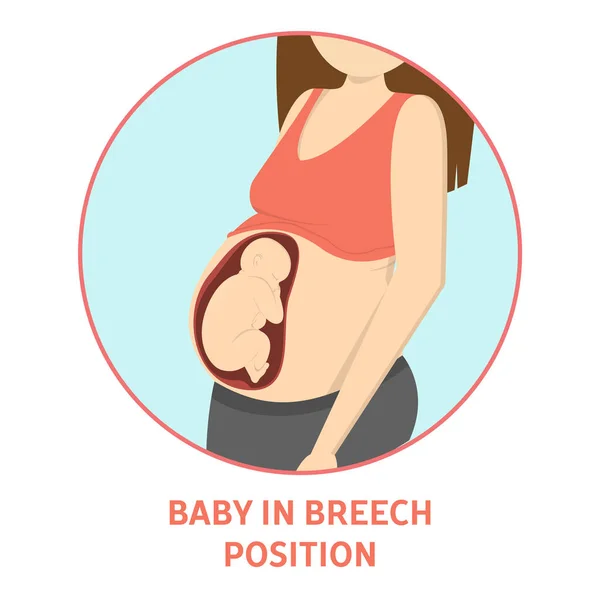 “They also show how important it is to ensure that caesarean sections are available to women who need it, and not just strive to achieve any specific targets.”
“They also show how important it is to ensure that caesarean sections are available to women who need it, and not just strive to achieve any specific targets.”
\n
\nAt the population level, the effect of caesarean section on maternal and neonatal outcomes, such as stillbirth or complications such as birth asphyxia, remains unknown. Further research is needed regarding the effects of caesarean section on women's psychological and social well-being.
\n
\nDue to additional costs, high rates of unnecessary caesarean sections can result in a drain on resources to the detriment of other services in overburdened and weak health systems.
\n
Robeson system
\n
\nThe absence of a standardized internationally recognized classification system for sequential monitoring and comparative analysis of data on the frequency of caesarean section, which is of practical importance, is one of the factors hindering a better understanding of trends in this area . The WHO proposes to adopt the Robeson classification as the internationally recognized caesarean section classification system.
The WHO proposes to adopt the Robeson classification as the internationally recognized caesarean section classification system.
\n
\nAccording to the Robeson system, each woman entering the maternity ward can be assigned to one of 10 groups based on easily identifiable characteristics such as the number of previous pregnancies, whether the baby is head-first, gestational age, caesarean section history, number of children and signs of onset of labor. The use of this system will allow for a comparative analysis of the frequency of caesarean sections both within individual institutions and between different health care institutions, as well as between countries and regions.
\n
\n“Obtaining information in a standardized, unified and reproducible manner is essential for healthcare providers who want to optimize caesarean delivery and evaluate and improve the quality of care,” explains Dr. Temmerman.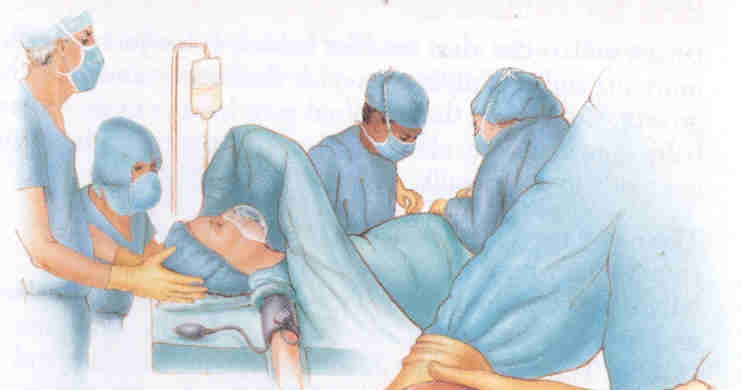 “We call on the entire medical community and decision-makers to take these findings into account and put them into practice as soon as possible.”
“We call on the entire medical community and decision-makers to take these findings into account and put them into practice as soon as possible.”
\n
Notes to editors
\n
\nThe WHO caesarean section statement is based on the results of two studies performed under the UNDP/UNFPA/WHO/World Bank Special Program for Research, Development and Research Training in Human Reproduction. This program, carried out with the participation of the WHO Department of Reproductive Health and Research, is the main instrument for conducting research in the field of human reproduction in the United Nations system.
\n
","datePublished":"2015-04-09T23:59:00.0000000+00:00","image":"https://cdn.who.int/media/images/default -source/imported/car-chris-black-jpg.jpg?sfvrsn=5d088ac9_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo": {"@type":"ImageObject","url":"https://www.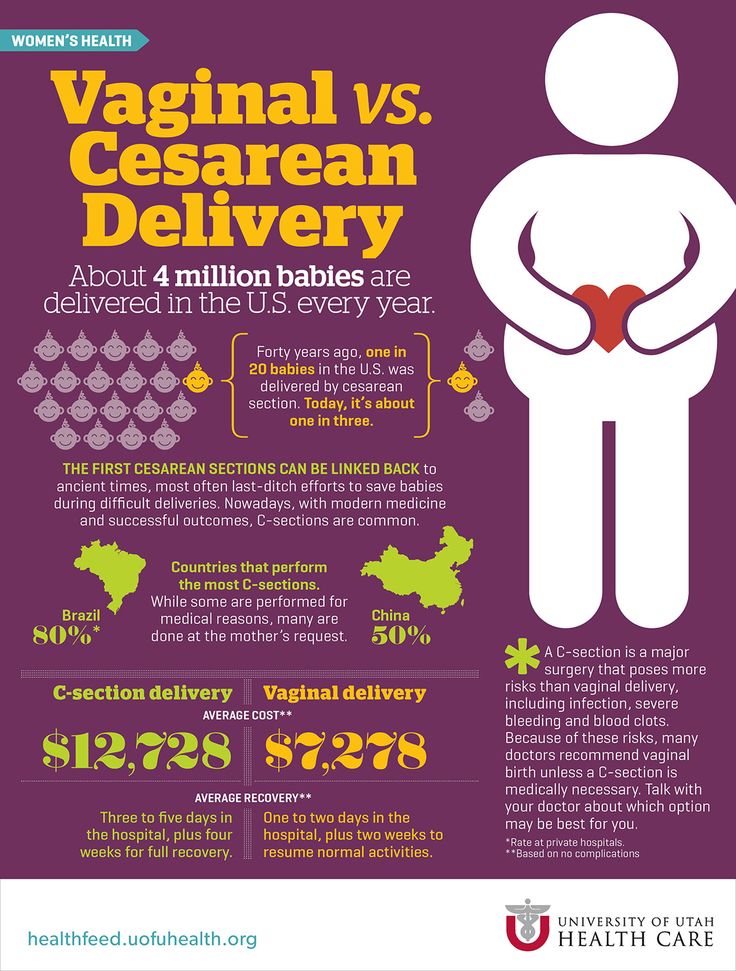 who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified ":"2015-04-09T23:59:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news/item/09-04-2015-caesarean-sections-should-only-be-performed-when-medically-necessary","@context":"http://schema.org","@type":"NewsArticle"};
who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified ":"2015-04-09T23:59:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news/item/09-04-2015-caesarean-sections-should-only-be-performed-when-medically-necessary","@context":"http://schema.org","@type":"NewsArticle"};
Caesarean section is one of the most common surgical procedures in the world, and its frequency continues to increase, especially in high- and middle-income countries. While caesarean sections can save lives, they are often performed when there is no medical indication, putting women and their children at risk of developing health problems in the short or long term. The new WHO statement highlights the importance of taking into account the needs of the patient in each case and abandoning the practice of achieving targets.
A caesarean section may be necessary when vaginal delivery could pose a risk to the mother or baby, such as prolonged labor, distress, or fetal presentation. At the same time, caesarean section can lead to serious complications, disability or death, especially in the absence of opportunities to safely perform surgical interventions or treat possible complications.
At the same time, caesarean section can lead to serious complications, disability or death, especially in the absence of opportunities to safely perform surgical interventions or treat possible complications.
Impact on reduction of maternal and child mortality
Since 1985, it has been accepted in the international health community that the ideal caesarean section rate is 10-15%. Findings from new studies show that if caesarean section rates increase to 10% at the population level, maternal and neonatal mortality rates decrease. However, if the frequency of its implementation exceeds 10%, the available data do not indicate an improvement in mortality rates.
“These findings highlight the importance of caesarean section in saving maternal and newborn lives,” says Dr Marleen Temmerman, Director of the WHO Department of Reproductive Health and Research. “They also show how important it is to ensure that caesarean sections are available to women who need it, and not just strive to achieve any specific targets. ”
”
At the population level, the impact of caesarean section rate on maternal and neonatal outcomes, such as stillbirth or complications such as birth asphyxia, remains unknown. Further research is needed regarding the effects of caesarean section on women's psychological and social well-being.
Because of the added cost, high rates of unnecessary caesarean sections can result in a drain on resources to the detriment of other services in overburdened and weak health systems.
Robeson system
The lack of a standardized, internationally recognized classification system for consistent monitoring and comparative analysis of data on caesarean section rates of practical relevance is one of the factors hindering a better understanding of trends in this area. The WHO proposes to adopt the Robeson classification as the internationally recognized caesarean section classification system.
According to the Robeson system, each woman entering the maternity ward can be assigned to one of 10 groups based on easily identifiable characteristics such as number of previous pregnancies, whether the baby is head-first, gestational age, history of caesarean section, number of children, and signs start of childbirth.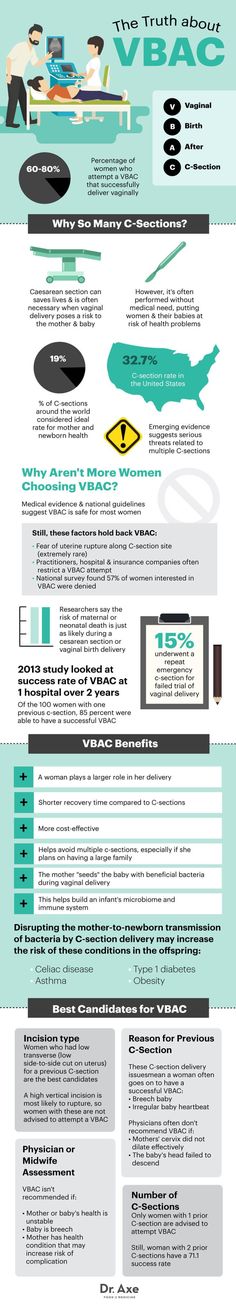 The use of this system will allow for a comparative analysis of the frequency of caesarean sections both within individual institutions and between different health care institutions, as well as between countries and regions.
The use of this system will allow for a comparative analysis of the frequency of caesarean sections both within individual institutions and between different health care institutions, as well as between countries and regions.
“Getting information in a standardized, unified, and reproducible manner is essential for healthcare providers who want to optimize caesarean delivery and evaluate and improve the quality of care,” explains Dr. Temmerman. “We call on the entire medical community and decision-makers to take these findings into account and put them into practice as soon as possible.”
Notes to editors
The WHO caesarean section statement is based on the results of two studies carried out under the UNDP/UNFPA/WHO/World Bank Special Program for Research, Development and Research in Human Reproduction. This program, carried out with the participation of the WHO Department of Reproductive Health and Research, is the main instrument for conducting research in the field of human reproduction in the United Nations system.