Extreme exhaustion during pregnancy
Pregnancy: Can Fatigue Be a Sign of a Health Problem?
Are you dragging these days? Does a nap sound fantastic right now?
Life can be exhausting at times, but especially when you’re pregnant. It’s totally normal to have some degree of fatigue right now—you are growing a human inside of you!
“Fatigue may be one of the most common first symptoms of pregnancy a woman experiences,” said Kelley Saunders, MD, an OBGYN at Banner – University Medicine Women’s Institute in Phoenix, AZ. “It is very common and quite significant in the first trimester. For many women, this improves in the second trimester and returns in the late third trimester.”
Although it’s common among pregnant women, you may still wonder why.
Why does pregnancy make you so tired?
The biggest reason: It’s hard work making a baby and it can be taxing to your body. “Your body has to adjust to maintain your health and the health of the baby inside of you,” Dr. Saunders said. “The physiologic changes and increased metabolic demand start in early pregnancy and can continue even after childbirth while breastfeeding. ”
Beginning somewhere between conception and implantation, pregnancy hormones kick in – affecting your body, mood and sleep. During the first trimester, you may also experience morning sickness, frequent nighttime bathroom breaks and leg cramps, which can leave you feeling pretty tired.
Then starting around your second trimester, you may start to get a little pep in your step. You may start to feel more like yourself again. But don’t be alarmed if you are still pretty exhausted—especially if you have other children to care for. Fatigue is still possible during the second trimester.
In late pregnancy, you’ll most likely begin to feel tired again. At this point, your baby has grown quite a bit and is putting more physical demands on your body. You’re carrying around extra weight and it’s more difficult to get comfortable when you sleep. Add in leg cramps and heartburn, and sleep becomes even more elusive.
When is pregnancy exhaustion not normal?
While exhaustion is a common symptom of pregnancy, extreme fatigue is not normal and may be a sign of an underlying health condition. Dr. Saunders said you should see your health care provider if your fatigue is severe and persistent.
Dr. Saunders said you should see your health care provider if your fatigue is severe and persistent.
“A sudden onset of exhaustion and continual symptoms may be a sign of abnormal fatigue,” she said. “When fatigue is associated with fever, chest pain, difficulty breathing or an inability to perform routine daily activities, you should see your OBGYN for evaluation.”
Some of the potential underlying causes for your fatigue both during and outside of pregnancy may be due to the following:
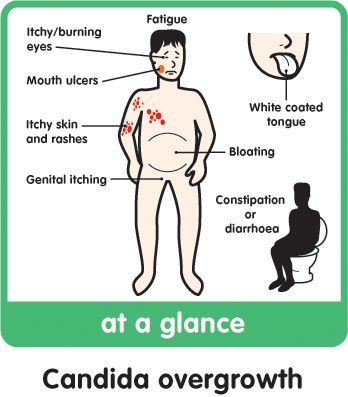
- Gestational diabetes: Your body may become resistant to insulin during pregnancy, which can cause you to feel very tired. Other symptoms include extreme thirst and frequent urination.
- Anemia: A lack of iron can cause you to have an insufficient number of red blood cells to transport oxygen to your tissues and can cause you to feel tired, lightheaded and weak.
- Infections (viral, bacterial or fungal): Being pregnant can make you more vulnerable to infections, such as urinary tract infections, which can make you fatigued.

- Thyroid problems: Having too much or too little thyroid hormones can cause you fatigue, along with fluctuations in your weight, irritability and depression.
- Prenatal depression: Feeling tired all the time can also be a side effect of depression. Other symptoms may include sadness, feelings of hopelessness and an inability to complete daily tasks or activities.
If you’re in need of a health care provider or have questions or concerns, you can find a Banner Health specialist at bannerhealth.com who can help.
Have a happy, healthy pregnancy
For helpful tips to boost your energy and stay healthy throughout your pregnancy, check out the following posts:
- 5 Tips for a Happy and Healthy Pregnancy
- Pregnant and Hungry? A Guide to Eating Right
- Prenatal Screening Tests to Expect Every Trimester
- Driving While Pregnant: Common Questions Answered
- Is a Headache During Pregnancy Something to Worry About?
Women's Health Pregnancy
Join the Conversation
The Most Tired You've Ever Felt
Growing a human is exhausting. It’s as if a magical spell was cast the day your pregnancy test came back positive — except Sleeping Beauty’s fairy didn’t gift you with 100 years of rest and true love’s kiss is what got you into this.
It’s as if a magical spell was cast the day your pregnancy test came back positive — except Sleeping Beauty’s fairy didn’t gift you with 100 years of rest and true love’s kiss is what got you into this.
If only you could sleep more…
It’s completely normal for a pregnant woman to feel fatigued, especially during the first and third trimesters.
Somewhere between morning sickness and elastic waistbands, Little Bo-Peep has lost your sheep (she probably sold them to Sleeping Beauty) and there are none left for you to count to sleep.
One of the first signs of pregnancy is fatigue. It smacks you by surprise, like the sliding glass door you assumed to be open.
Beginning as early as conception and implantation, pregnancy hormones instantly affect your body, mood, metabolism, brain, physical appearance, and sleep pattern.
In the second trimester, which begins at week 13, many women get a fresh surge of energy. This is a great time to tackle those important before-baby-arrives chores, because as you enter the third trimester, which begins at week 28, that extreme exhaustion returns.
Simply put, you feel tired because you’re growing a baby.
In addition to hormonal changes, physical and emotional changes also lower your energy levels and make you feel fatigued.
Some of these changes include:
- increased levels of estrogen and progesterone (which, by the way, acts as a natural sedative)
- lower blood pressure and blood sugar
- increased blood flow
- disrupted sleep
- digestion issues
- morning sickness
- stress and anxiety
- frequent urination
- heartburn
- back, hip, and pelvic pain
When to contact your doctor or midwife
If insomnia, restless legs syndrome (the uncontrollable urge to move your legs while resting), sleep apnea (a potentially serious disorder in which breathing repeatedly stops and starts), preeclampsia, or any other condition is hindering your sleep, talk to your doctor or midwife during your next appointment.
Other reasons to contact your doctor or midwife include, if you:
- feel concerned that the pregnancy fatigue is a sign of something more, like anemia, gestational diabetes, or depression
- develop any changes in your vision
- experience dizziness
- urinate less frequently
- have shortness of breath, pain in your upper abdomen, or heart palpitations
- experience severe headaches
- notice a swelling of your hands, ankles, and feet
Your healthcare practitioner can help you uncover any problems and offer additional solutions.
Growing a baby obviously takes a toll on your body. Don’t ignore the signals your body is sending you. Reach out to others if you’re struggling to sleep throughout your pregnancy. Ask for help from your partner.
No matter how tired you get, you should avoid taking any over-the-counter medicines as a sleeping aid.
Most pregnant women should spend at least 8 hours in bed, aiming for at least 7 hours of sleep every night. If possible, try going to sleep a little earlier than usual.
As your body changes, make sleep a priority and follow these tips to combat pregnancy fatigue:
Keep your bedroom dark, clean, and cold
Create the right atmosphere for optimal rest.
In order for your body to reach deep sleep, cover any windows with blackout curtains. Turn off any digital clocks and unplug nightlights illuminating a glow (cover the display with electrical tape if you don’t want to completely turn the device off).
Set the bedroom temperature a little cooler than the rest of your home, for optimal quality of sleep. Eliminate any needless clutter and wash your bedsheets often. Save your bed for sleep, cuddling, and sex.
Eliminate any needless clutter and wash your bedsheets often. Save your bed for sleep, cuddling, and sex.
Take a nap
Napping can make up for any sleep lost at night, due to frequent trips to the bathroom, body aches, and every other pregnancy irritation. Avoid napping in the late afternoon and early evenings.
If your employer frowns upon nap time, find a good spot in the breakroom and put your feet up while you eat lunch.
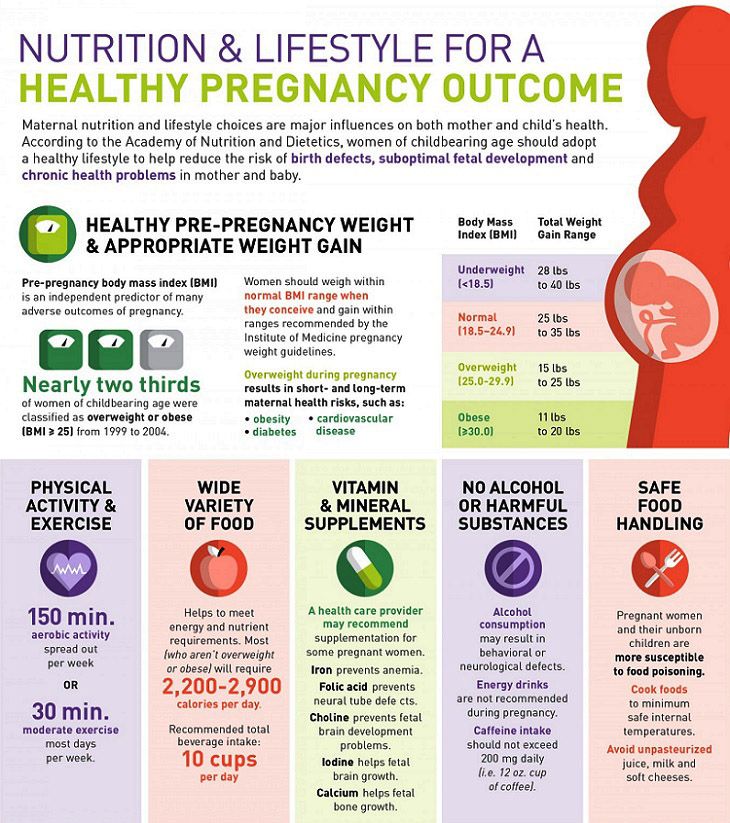
Eat healthy meals and stay hydrated
In the beginning, pregnancy can also lower your blood pressure and blood sugar, which can make you feel tired. But a lack of sleep can cause your blood sugar levels to rise, increasing the risk for gestational diabetes.
Keep your blood sugar and energy levels balanced by eating often, such as six small meals a day. Frequent meals that are high in nutrients and protein help to combat fatigue.
To avoid nighttime leg cramps, stay hydrated by drinking enough water and fluids throughout the day.
Keep a pregnancy journal or dream diary
Keep a journal throughout your pregnancy. If you’re feeling anxious or stressed, try writing in it.
Pregnant women experience more vivid dreams and better dream recall, due to hormonal shifts affecting sleep patterns, increased fatigue, and repeatedly waking in the middle of a sleep cycle.
Sleep diaries can also be enlightening, providing concrete data about your bedtime, how long it takes for you to fall asleep, nighttime awakenings, awake time, and sleep quality.
Avoid caffeine after lunchtime
As far as stimulants go, caffeine may keep you awake long into the night or cause you to wake more frequently. It can also keep your baby active, kicking and rolling around inside your belly as you try to sleep.
Experts recommend pregnant women limit their caffeine intake to two home-brewed cups of coffee, or less than 200 milligrams, per day.
Pamper yourself
Ask for help from family and friends. Take a warm bath. Ask your partner for a massage. Take a break.
Take a warm bath. Ask your partner for a massage. Take a break.
Wear soft, non-restrictive clothing and sit in a cozy chair with a good book and read for a little bit. Light a lavender candle. Play soothing instrumental music. Have a cup of warm chamomile tea.
You get it.
Exercise
The demands of pregnancy together with the weight gained puts an enormous amount of pressure on your body.
In addition to more restful sleep, The American College of Obstetricians and Gynecologists states the following benefits of exercise during pregnancy:
- reduced back pain
- eased constipation
- decreased risk of gestational diabetes, preeclampsia, and cesarean delivery
- healthier weight gain during pregnancy
- improved overall general fitness
- strengthened heart and blood vessels
- improved ability to lose the baby weight after your baby is born
It can take a few hours for your body to fully wind down after energetic workouts, so plan for any physical activity to take place earlier in the day. If the exercise is light, like yoga, it’s unlikely to interfere with your sleep.
If the exercise is light, like yoga, it’s unlikely to interfere with your sleep.
Always check with your medical practitioner or midwife before beginning a new exercise program during pregnancy.
Pregnancy can be a tiring experience — both emotionally and physically. It’s important to remember: You are not alone.
Nearly all women experience more fatigue than usual at some point during their pregnancy. Take it as a message from your body. It’s telling you to rest, and you should definitely listen.
Pregnancy stress threatens the health of the unborn child - DW - 11/07/2013
Vladimir FradkinNovember 7, 2013
It is well known that severe stress is harmful. Now scientists have taken up the question of how the stress experienced by the mother during pregnancy affects the health of the child.
https://p.dw.com/p/1ADc4
Advertising
Pregnancy, even if it is not the first, in itself, of course, is a fair amount of stress. But even if this were not so, hardly any woman manages to avoid the stress caused by various events of everyday life for all nine months. And therefore, almost any expectant mother asks the question: how will the stress she experiences affect the child? Can the fear, pain, grief, irritation, or arousal of the mother be transmitted to the fetus in the womb?
But even if this were not so, hardly any woman manages to avoid the stress caused by various events of everyday life for all nine months. And therefore, almost any expectant mother asks the question: how will the stress she experiences affect the child? Can the fear, pain, grief, irritation, or arousal of the mother be transmitted to the fetus in the womb?
Maternal stress hormone in fetal blood
Not only can they be transmitted, but they must be transmitted, although, of course, still not fully, doctors say. The placenta contains a number of hormones designed to protect the fetus from the harmful effects of cortisol, the mother's stress hormone. But it still penetrates into the blood of the embryo. True, there its concentration is about 10 times lower than the maternal one, however, it is also enough to have a significant effect on the fetal body.
And not just significant, but long-term, often even permanent. This conclusion was reached by a group of doctors led by Professor Matthias Schwab (Matthias Schwab) from the Hans Berger Neurological Clinic at the University Hospital of Jena. The scientists reported the results of their research at the 21st annual session of the German Somnological Society, which took place in Wiesbaden.
The scientists reported the results of their research at the 21st annual session of the German Somnological Society, which took place in Wiesbaden.
“Antenatal stress leads to a long-term increase in fetal cortisol levels and accelerates brain maturation,” says Prof. Schwab, who heads the Intrauterine Brain Development and Later Life Programming of Disease Working Group. “For this reason, the stress experienced by the mother during pregnancy , is a serious risk factor that increases the likelihood of a child developing later depression and other pathologies.
Dreaming of a lamb in the womb of a sheep
Professor Schwab and his colleagues conducted their experiments on sheep, since in these animals the course of pregnancy and the formation of the embryo have a significant similarity with the same processes in humans. Pregnant - that is, pregnant - sheep, the researchers injected betamethasone, a synthetic glucocorticoid drug related to cortisol, which is often prescribed to women with the threat of premature birth. This drug speeds up the development of the lungs in the fetus, which increases the chances of a premature baby to survive. Betamethasone was administered to pregnant sheep at a stage corresponding in pregnant women to the period between the 25th and 32nd weeks.
This drug speeds up the development of the lungs in the fetus, which increases the chances of a premature baby to survive. Betamethasone was administered to pregnant sheep at a stage corresponding in pregnant women to the period between the 25th and 32nd weeks.
At the same time, scientists monitored the intrauterine brain activity of embryos using electroencephalography. It turned out that betamethazole accelerates the maturation of not only the lungs, but also the brain, says Professor Schwab: “This is evidenced, first of all, by the early appearance of dreams. Usually, the formation of dreams occurs in the last third of pregnancy, and this development occurs very gradually. And betamethasone literally includes there is some kind of toggle switch in the brain, and dreams are formed in 2-4 days."
Brain development inhibits cell growth and division
Another consequence of the introduction of the hormone was an abnormally frequent alternation of the phases of REM and non-REM sleep. This fragmentation of sleep, if it becomes permanent, indicates a high risk of developing depression later in life and, according to Professor Schwab, is often diagnosed in newborns whose mothers experienced severe stress during pregnancy.
This fragmentation of sleep, if it becomes permanent, indicates a high risk of developing depression later in life and, according to Professor Schwab, is often diagnosed in newborns whose mothers experienced severe stress during pregnancy.
The problem is that the premature maturation of brain structures occurs due to a slowdown in cell division and body growth, the scientist says. This is confirmed by other doctors. "Children given injections to accelerate lung maturation showed a very significant increase in stress axis activity and had a markedly lower birth weight," says Thorsten Braun, a gynecologist at the Charité University Hospital in Berlin.
Therapy with betamethasone is fraught with behavioral disorders
In Germany, 8 to 10 percent of pregnant women receive betamethasone. The fact that this drug reduces mortality among premature babies by 31 percent has long been scientifically proven. However, animal experiments have shown that taking the drug also causes long-term side effects - in particular, hypertension - and also contributes to the development of cardiovascular diseases and diabetes in later life.
As for a person, here scientists have identified, first of all, an increased risk of developing depression and behavioral abnormalities. Recently, Professor Schwab and his colleagues examined 40 eight-year-old children who had previously undergone intrauterine therapy with betamethasone. Comparing the test results of these children with the test results of children in the control group revealed significant differences, the scientist emphasizes: ". Electroencephalography also showed that these children could not relax before testing, and could not concentrate during testing.
No reason to panic
Apparently, the increased content of the stress hormone in the blood at the stage of intrauterine development leads to the fact that the body of the embryo gets used to this situation and begins to perceive it as the norm. "These babies are already programmed in the womb to produce too much of the stress hormone later in life," says Professor Schwab.
The Dutch colleagues of the German scientist - doctors at the University of Tilburg - found that maternal stress affects the fetus most negatively between the 12th and 22nd weeks of pregnancy: its consequences make themselves felt even 20 years later.
But still, one should not panic, says Professor Schwab: “Stress during pregnancy is a completely normal thing. And injections of betamethasone, this hormonal accelerator of lung development, are an important and necessary therapy if there are indications for it. You just need to keep in mind that An elevated level of stress hormone in the blood of the embryo seems to play a more important role in the development of later diseases than has been previously believed.
Write to the editor
Advertising
Skip section Related topicsRelated topics
Show more
Skip section Top topic1 page of 3
Toxicosis is a painful condition that develops during pregnancy. Toxicosis is early (usually occurs in the first trimester) and late (appears in the second or third trimester). In severe cases, toxicosis can pose a danger to the mother and child.
Toxicosis during early pregnancy: symptoms
- Heightened sense of smell. Tobacco smoke, cosmetics, the scent of flowers, or any other odor is irritating.
- Changing gastronomic tastes. "Classics of the genre" - pickles, herring, oranges. By the way, contrary to the existing misconception, the gender of the unborn child does not affect the food preferences of a woman. Toxicosis during pregnancy as a girl is no different from toxicosis during pregnancy as a boy. A woman's eating habits depend on the needs of the body.
- Nausea, vomiting, salivation. Usually these symptoms make themselves felt in the morning hours, but sometimes they haunt a woman around the clock.
- A mild form of toxicosis is accompanied by vomiting no more than 5 times a day and does not require the intervention of specialists.
- The average form of toxicosis is characterized by vomiting up to 10 times a day, and it is a reason for mandatory consultation with a doctor.

- Severe toxicosis during pregnancy occurs in 1 out of 500 cases. If a woman vomits more than 10 times a day, suffers from salivation, she needs urgent hospitalization.
- Deficiency of fluid and nutrients can lead to dehydration and metabolic disorders, as a result of which toxins will only accumulate. The expectant mother is waiting for great weight loss and exhaustion. During severe toxicosis, there is a risk of tachycardia, toxic liver dystrophy, arterial hypotension.
- One of the symptoms of early toxicosis can be dermatoses: for example, eczema or itching (sometimes only in the vulva).
- In rare cases, seizures, bone pain and brittleness may occur. The reason for this is disturbances in the metabolism of phosphorus and calcium, as well as changes in the functioning of the parathyroid glands.
- In exceptional cases, the development of bronchial asthma is possible.
Toxicosis during early pregnancy: causes
There are many hypotheses explaining the causes of early toxicosis. The most famous among them:
The most famous among them:
- Immunological theory. A cell, consisting of foreign genes and proteins, is perceived by the body as a foreign body that needs to be disposed of.
- Hormonal theory. Already on the 6th - 8th day after fertilization, the embryo actively produces the pregnancy hormone - human chorionic gonadotropin (hCG). Its concentration is growing rapidly, but by the 12th week it begins to fall, then toxicosis usually disappears. One of the arguments in favor of this theory is the coincidence of peak hCG values with the onset of vomiting.
- Toxic theory. The development of the fetal egg is accompanied by the formation of toxins that poison the mother's body.
- Neuro-reflex theory. The fetal egg irritates the nerve receptors of the uterus and provokes disturbances in the interaction of the central nervous system, the autonomic nervous system and internal organs. A failure occurs in the work of the subcortical nuclei of the central nervous system, which leads to the appearance of zones of pathological excitation at the most vulnerable points - in the vomiting center and the center of salivation.

- Psychogenic theory. Toxicosis develops against the background of experiences associated with pregnancy.
All these hypotheses complement each other, but the most convincing, according to experts, is the neuro-reflex theory.
Factors contributing to the development of toxicosis
In most women, toxicosis lasts from 6 to 12-13 weeks. But this is not an axiom. Someone has a pregnancy without toxicosis, and someone is sick all 9 months. It is very difficult to predict the reaction of the body. However, factors are known that increase the risk of development and severity of toxicosis during pregnancy. Among them:
- multiple pregnancy,
- heredity,
- too young or, on the contrary, mature age,
- underweight,
- chronic diseases of the gastrointestinal tract and liver,
- abortion,
- malnutrition,
- bad habits,
- stress.
Early toxicosis: what to do?
There is no universal remedy for toxicosis: everything is very individual. However, in any case, in order to alleviate the symptoms of malaise, it is necessary to reconsider the usual lifestyle and diet.
However, in any case, in order to alleviate the symptoms of malaise, it is necessary to reconsider the usual lifestyle and diet.
- Get more rest. Sleep at least 8 hours a day and walk outdoors for at least 1.5 hours.
- Eat small meals 6 to 7 times a day.
- Eliminate hot, spicy and fatty foods from your diet.
- Introduce foods rich in pyridoxine (vitamin B6) into your diet. Its lack can exacerbate toxicosis during pregnancy. There is not so much vitamin B6 in animal food, so focus on plant products: rice, barley and buckwheat, millet, beans, soy.
- Include foods rich in complex carbohydrates in your evening menu. Cereals, potatoes, pasta made from durum wheat will help maintain a stable level of glucose in the blood and avoid its sharp drop in the morning.
- Before going to bed, leave a glass of water, a lemon, some biscuits or crackers on your bedside table. After waking up, without getting up, add lemon to the water, drink it and eat cookies or crackers.

- Stay in bed after breakfast. Lie down for a bit and only then slowly get up.
- If gagging occurs while brushing teeth, change toothpaste or limit mouthwash.
- Consult your doctor about herbal teas. Chamomile, calendula, lemon balm and valerian can alleviate your condition.
- Talk to your doctor about taking ginger. In American literature, it is known as one of the most effective remedies for toxicosis.
Toxicosis in late pregnancy: causes
Late toxicosis during pregnancy is better known as "preeclampsia". This is a serious complication, which is accompanied by disruption of the functioning of vital organs. Most often, toxicosis in late pregnancy occurs in women younger than 19 and older than 30. Risk factors:
- multiple pregnancy,
- early toxicosis,
- fetal malnutrition,
- Rh conflict,
- heredity,
- anemia,
- obesity,
- hypertension,
- kidney diseases,
- endocrine diseases,
- malnutrition,
- preeclampsia during previous pregnancies.

The cause of late toxicosis is a violation of blood microcirculation and water-salt metabolism. Spasm of small vessels provokes a decrease in blood flow velocity and the formation of blood clots. The volume of circulating blood decreases, and the permeability of the walls of blood vessels increases. As a result, blood circulation is disturbed, and tissue nutrition deteriorates. Changes occur in organs that can lead to necrosis (death of cells and tissues).
Toxicosis in late pregnancy: stages and symptoms
There are 4 stages of late toxicosis: dropsy, nephropathy, preeclampsia and eclampsia.
- dropsy. This is the mildest form of gestosis. It is characterized by a sharp increase in weight and swelling.
- Nephropathy. In addition to edema, other symptoms of late toxicosis appear: protein in the urine and high blood pressure. Its sudden changes are especially dangerous for the fetus. Possible premature detachment of the placenta, bleeding, premature birth.

- Preeclampsia. The woman's condition is deteriorating. Against the background of high pressure, headaches occur, rippling in the eyes, nausea, vomiting, sometimes drowsiness, lethargy, forgetfulness. The woman is worried about chest pain, shortness of breath, shortness of breath. All these signs may indicate the development of an even more severe form of late toxicosis.
- Eclampsia. This is the most dangerous stage of gestosis. Blood circulation is disturbed in the brain. This is fraught with convulsions and loss of consciousness. As a result of eclampsia, severe complications develop: edema of the lungs, brain, kidney and heart failure. Possible death of the mother and fetus.
Toxicosis in late pregnancy: prevention
- Minimize stress.
- Reduce salt (to 3-5 grams per day) and fluid (to 1 liter per day). Consult your doctor about this.
- Regularly visit the antenatal clinic and take the necessary tests. A decrease in platelets in the blood, asymmetry of pressure on the hands, a decrease in pulse pressure for a doctor are indicators of pregestosis - the preclinical stage of late toxicosis during pregnancy.