Dangers signs of pregnancy
DANGER SIGNS IN PREGNANCY - Counselling for Maternal and Newborn Health Care
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Counselling for Maternal and Newborn Health Care: A Handbook for Building Skills. Geneva: World Health Organization; 2013.
Counselling for Maternal and Newborn Health Care: A Handbook for Building Skills.
Show details
- Contents
Search term
What is in this session?
It is important to share information with women and their families about the early detection and recognition of danger signs and complications as part of birth and emergency planning. You need to discuss with them what the danger signs are and help them to think about and decide where they will go if they experience one or any of these.
What skills will I develop?
To provide information about danger signs and complications during pregnancy and childbirth
To support women in planning where to go and how to get there quickly if an emergency arises.
What am I going to learn?
By the end of this session you should be able to:
Know the danger signs and complications.
Be able to effectively communicate danger signs to women and their families.
Be able to effectively communicate how to access emergency care when a danger sign is recognized.
Danger signs and complications
All pregnant women, their partners and families should be aware of the signs of complications and emergencies and know when to seek care from the skilled attendant.
DANGER SIGNS DURING PREGNANCY
If any of the following signs occur, the woman should be taken immediately to the hospital or health centre.
vaginal bleeding
convulsions/fits
severe headaches with blurred vision
fever and too weak to get out of bed
severe abdominal pain
fast or difficult breathing.
If she has any of these signs she should go to the health centre as soon as possible:
Fever
Abdominal pain
Feels ill
Swelling of fingers, face and legs
Communicating danger signs
Most women have uneventful pregnancies and childbirth but sudden and unpredictable complications may happen at any time to any woman. Where problems do occur it is important to ensure that they are acted upon without delay. You need to find a way to explain in familiar terms (using local words) the danger signs, so that the woman, her family and others in the community can recognize them if they should occur, and to ensure they know where to go in case of an emergency. It would also be helpful here to refer to Session 7 on birth and emergency plans as many elements, including transport, where the nearest health facility is located, and logistical details regarding persons to support the family, should already have been discussed and planned in advance.
Where problems do occur it is important to ensure that they are acted upon without delay. You need to find a way to explain in familiar terms (using local words) the danger signs, so that the woman, her family and others in the community can recognize them if they should occur, and to ensure they know where to go in case of an emergency. It would also be helpful here to refer to Session 7 on birth and emergency plans as many elements, including transport, where the nearest health facility is located, and logistical details regarding persons to support the family, should already have been discussed and planned in advance.
Activity 1
2 hours 55 minutes
To begin reflecting on how to inform pregnant women and their families on the danger signs during pregnancy and build on women's past experience where possible.
Review the list of danger signs above.
What problems do women and families have in identifying each of these? Are there local terms that are used for any of them? Are there any local beliefs, explanations, or ways of handling danger signs that stop people from seeking care in a timely manner?
How do women prioritize the main danger signs? Are there certain signs that they feel need more urgent attention than others?
Are all women told about danger signs or just those women who are thought to be at high risk?
Organize a discussion with a group of women.
 Ask the group for their past experience with danger signs and complications.
Ask the group for their past experience with danger signs and complications.Have any of the women experienced danger signs before? If so, how did they recognize them?
What did they do? Who did they see?
Did they find transport urgently? If not, what could be done next time?
What information did they have or were there any gaps?
How could health workers have better prepared them?
Review the list of danger signs once again.
Is the community aware and able to recognize danger signs in pregnancy?
Think of ways to help the broader community in identifying danger signs and supporting women to reach appropriate care in a timely fashion.
Do you or other health agencies currently discuss danger signs in pregnancy with the broader community? What are the advantages of doing so?
What kind of support materials might improve the communication of danger signs?
Take into account the educational and cultural background of your audience (e.
 g. the counselling context) and the resources you have to develop, or to obtain materials.
g. the counselling context) and the resources you have to develop, or to obtain materials.
Finally, think about whether there are any other groups or providers in the community that you could work with to help alert the whole community to the danger signs in pregnancy and labour.
Write down some ideas in your notebook that could help you discuss danger signs with women and their families, both on a one-to-one basis and in a group setting.
Our View
WHO recommends that health services work with women, their families and the broader community so that they have appropriate and comprehensible information on the danger signs during pregnancy, as any woman can develop complications, and to ensure that all are aware of where to seek care in the case of an emergency.
Explore with women what they know about danger signs and make sure they know them all. Some danger signs are more difficult than others to recognize such as oedema. When counselling women about danger signs you need to explore with them what is normal, what is unusual and what is a danger sign.
The next important step is to help the woman and her family plan where they will go and how they will reach the skilled attendant if they have any of these signs. Refer to Session 7 as much of this information should already have been discussed and drafted into a birth and emergency plan.
HOW CAN YOU HELP WOMEN AND FAMILIES BETTER UNDERSTAND THE DANGER SIGNS?
Women and their families need to be able to recognize danger signs accurately and act appropriately. For example, bleeding requires immediate transport to a health facility because a woman, particularly with anaemia, can die in a matter of hours.
Knowing about the danger signs in advance will help communities and families implement their birth and emergency plans.
If you have a highly literate population you might consider communicating all the danger signs in a leaflet or fact sheet or some other method that can be given out at routine antenatal care. If your population is less literate, you will have to rely on verbal or pictorial methods.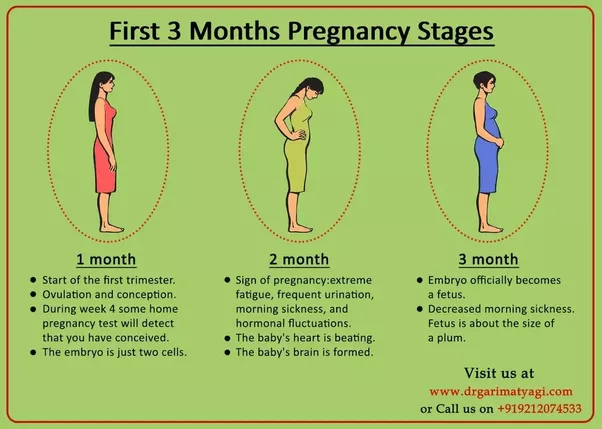 It is difficult to remember all the danger signs, particularly if a person has little formal education. You need to work with the community and with other health providers to increase awareness of women and other community members of the danger signs, and of the importance of reaching an appropriate care provider urgently if any should appear. Once again it is important to ensure emergency transport schemes are in place (Session 7).
It is difficult to remember all the danger signs, particularly if a person has little formal education. You need to work with the community and with other health providers to increase awareness of women and other community members of the danger signs, and of the importance of reaching an appropriate care provider urgently if any should appear. Once again it is important to ensure emergency transport schemes are in place (Session 7).
All women and their families need to be given information on danger signs
Communicating danger signs without fear
Research has shown that using fear-based messages about danger signs is not effective unless used correctly.
It will be hard to communicate danger signs without creating fear. When discussing danger signs with women and their families, provide a realistic description that would help them to identify the signs in an emergency. Avoid frightening the woman with the worst-case scenario of what might happen. While complications such as bleeding, obstructed labour or infection are relatively rare, the focus should be on recognition of the signs and awareness of what to do if they occur. While as a health worker you are used to seeing complications, remember for the woman it can be very frightening. Reassure her that you will do everything you can to help her, try to alleviate her fears, and support her, but remember to answer her questions and concerns truthfully. It will not be helpful to make false promises or reassurances about pregnancy outcomes.
While as a health worker you are used to seeing complications, remember for the woman it can be very frightening. Reassure her that you will do everything you can to help her, try to alleviate her fears, and support her, but remember to answer her questions and concerns truthfully. It will not be helpful to make false promises or reassurances about pregnancy outcomes.
REMINDER
Pregnancy is a normal and natural process. Most women do not experience emergencies during pregnancies, but any woman could. Women need to know when to seek care from an appropriate provider. A good counsellor will get the balance right between informing women and their families of the possible danger signs and what to do, and supporting women and their families to enjoy their pregnancy as a happy experience.
What did I learn?
You have considered how to communicate danger signs to a woman and her family, as well as the larger community. This has helped you to decide what format can be used to convey issues relating to danger signs. Furthermore, it is important to link discussions of danger signs with a concrete plan (such as the birth and emergency plan in Session 7) in order to ensure that women and their families know where to go during an obstetric emergency, and how to get there urgently.
Furthermore, it is important to link discussions of danger signs with a concrete plan (such as the birth and emergency plan in Session 7) in order to ensure that women and their families know where to go during an obstetric emergency, and how to get there urgently.
Do you feel confident about communicating danger signs to women and their families? What else could you do to improve the way you communicate danger signs? What kinds of support materials can you develop? Who else can you work with in the community to raise awareness of emergency signs and the importance of seeking appropriate care when they occur?
The next time you counsel a woman about danger signs, write up what happened and what you did in your notebook. You could then share this with a colleague and ask for feedback on what could have been improved or done differently, as well as what you did well.
Copyright © World Health Organization 2013.
All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel. : +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: tni.ohw@snoissimrep).
: +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: tni.ohw@snoissimrep).
Bookshelf ID: NBK304178
Contents
- PubReader
- Print View
- Cite this Page
- PDF version of this title (5.7M)
In this Page
- What is in this session?
- What skills will I develop?
- What am I going to learn?
- Danger signs and complications
Other titles in this collection
- WHO Guidelines Approved by the Guidelines Review Committee
Recent Activity
ClearTurn OffTurn On
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
See more...
7 Pregnancy Complications: Bleeding, Preeclampsia, and More
Some symptoms during pregnancy are par for the course, but others are cause for alarm. How do you know the difference?
Written by Denise Mann
You may wonder what symptoms during pregnancy warrant immediate medical attention and what symptoms can wait until your next prenatal visit.
Always ask your doctor at your visits about your concerns. But keep in mind some symptoms do need swift attention.
1. Bleeding
Bleeding means different things throughout your pregnancy. “If you are bleeding heavily and have severe abdominal pain and menstrual-like cramps or feel like you are going to faint during first trimester, it could be a sign of an ectopic pregnancy,” Peter Bernstein, MD, ob-gyn professor at New York's Albert Einstein College of Medicine and Montefiore Medical Center, says.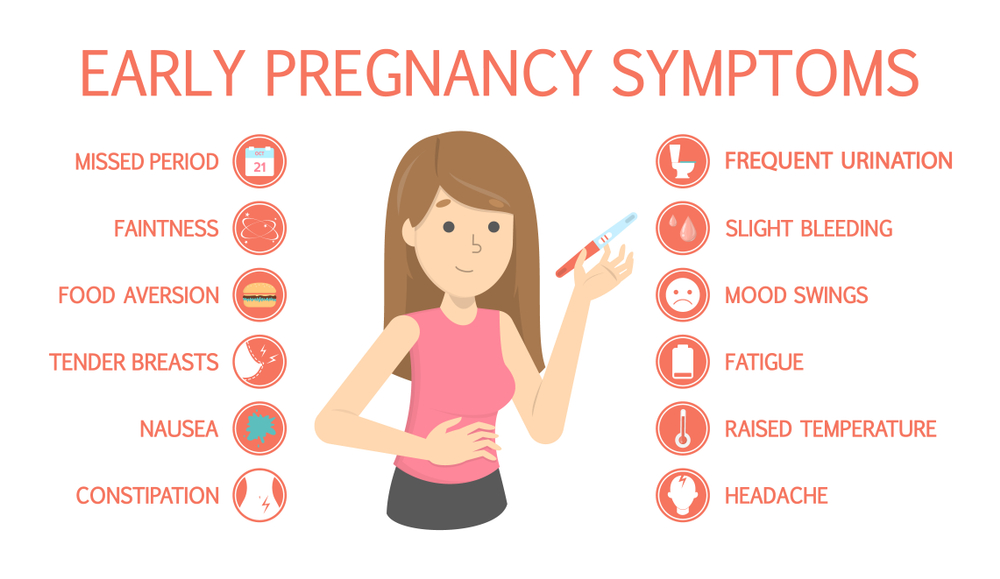 Ectopic pregnancy, which occurs when the fertilized egg implants somewhere other than the uterus, can be life-threatening.
Ectopic pregnancy, which occurs when the fertilized egg implants somewhere other than the uterus, can be life-threatening.
Heavy bleeding with cramping could also be a sign of miscarriagein first or early second trimester. By contrast, bleeding with abdominal pain in the third trimester may indicate placental abruption, which occurs when the placenta separates from the uterine lining.
“Bleeding is always serious,” women’s health expert Donnica Moore, MD, says. Any bleeding during pregnancy needs immediate attention. Call your doctor or go to the emergency room.
2. Severe Nausea and Vomiting
It's very common to have some nausea when you're pregnant. If it gets to be severe, that may be more serious.
“If you can’t eat or drink anything, you run the risk of becoming dehydrated,” Bernstein says. Being malnourished and dehydrated can harm your baby.
If you experience severe nausea, tell your health care provider. Your doctor may prescribe medication or advise changing your diet.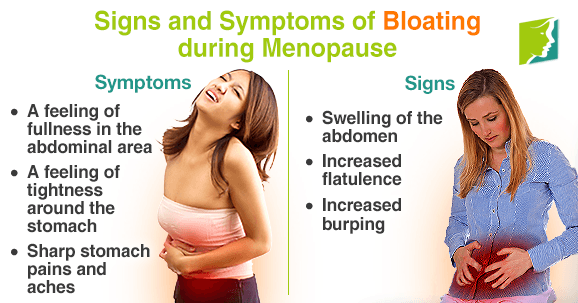
3. Baby’s Activity Level Significantly Declines
What does it mean if your previously active baby seems to have less energy? It may be normal. But how can you tell?
Some troubleshooting can help determine if there is a problem. Bernstein suggests that you first drink something cold or eat something. Then lie on your side to see if this gets the baby moving.
Counting kicks can also help, Nicole Ruddock, MD, assistant professor of maternal and fetal medicine at University of Texas Medical School at Houston, says. “There is no optimal or critical number of movements,” she says, “but generally you should establish a baseline and have a subjective perception of whether your baby is moving more or less. As a general rule, you should have 10 or more kicks in two hours. Anything less should prompt a phone call to your doctor.”
Bernstein says to call your doctor as soon as possible. Your doctor has monitoring equipment that can be used to determine if the baby is moving and growing appropriately.
4. Contractions Early in the Third Trimester
Contractions could be a sign of preterm labor. “But a lot of first-time moms may confuse true labor and false labor,” Ruddock says. False labor contractions are called Braxton-Hicks contractions. They’re unpredictable, non-rhythmic, and do not increase in intensity. “They will subside in an hour or with hydration,” Ruddock says. “But regular contractions are about 10 minutes apart or less and increase in intensity.”
If you're in your third trimester and think you're having contractions, call your doctor right away. If it is too early for the baby to be born, your doctor may be able to stop labor.
5. Your Water Breaks
You walk into the kitchen for a drink and feel a flood of water rush down your legs. “Your water could have broken,” Ruddock says, “but during pregnancy the enlarged uterus can cause pressure on your bladder too. So it could be urine leakage.” Ruddock says that sometimes water breaking is a dramatic gush of fluid, but other times it is more subtle.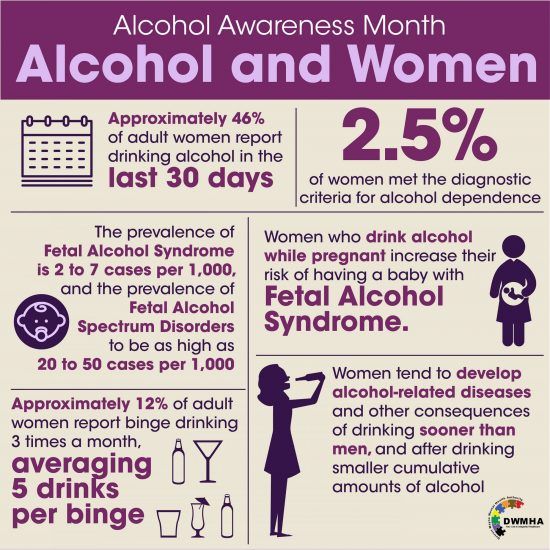
“If you are not sure if it is urine versus a true rupture of the membrane, go to the bathroom and empty your bladder," she says. "If the fluid continues, then you have broken your water.” Call your doctor or go to the hospital.
6. A Persistent Severe Headache, Abdominal Pain, Visual Disturbances, and Swelling During Your Third Trimester
These symptoms could be a sign of preeclampsia. That’s a serious condition that develops during pregnancy and is potentially fatal. The disorder is marked by high blood pressure and excess protein in your urine that typically occurs after the 20th week of pregnancy.
“Call your doctor right away and get your blood pressure tested,” Bernstein says. “Good prenatal care can help catch preeclampsia early.”
7. Flu Symptoms
Our experts say it’s important for pregnant women to get the flu vaccine since pregnant women are more likely to get sick and have serious complications from the flu than other women during flu season.
But if you do get the flu, "don’t rush into a hospital or doctor’s office where you can spread it to other pregnant women," Bernstein says. "Call your doctor first."
Warning signs during pregnancy - CGP on REM city polyclinic No. 11
We discuss the most pressing issues of pregnancy management in the classroom at the Young Mother's School and invite our women to an active constructive dialogue.
Schools are held in the format of an interactive conversation, we invite you to ask questions to the doctor, get comprehensive advice on planning and managing pregnancy, contraception and women's health. Our obstetrician-gynecologists are ready to do everything possible for a comfortable pregnancy, however, we hardly get feedback from our women. nine0003
Ladies, Women's Health Schools are held every Thursday from 13.00 to 14.00.
First trimester warning signs that require medical attention:
- vomiting more than 8-10 times a day
- bleeding from the genital tract
- severe pain in the abdomen or side.

- The pain may be dull at first and then begins to increase.
Physiological changes during pregnancy that do not require special treatment:
- nausea
- change of taste
- appearance or darkening of pigment spots on the skin
- soreness of the mammary glands.
There are three trimesters during pregnancy. The first trimester corresponds to the first three months of pregnancy, the second - the period from 4 to 6 months of pregnancy,
Signs that require immediate medical attention in the second trimester of pregnancy:
- persistent or severe headache
- blurred vision or flickering of dark dots ("flies") before the eyes
- noticeable or sudden onset and rapidly increasing edema
- bleeding from the genital tract
- severe persistent abdominal pain
- persistent vomiting
- no fetal movement within 24 hours
- profuse watery vaginal discharge (amniotic fluid rupture)
You should know and seek immediate medical attention if you develop any of the following symptoms in the third trimester of pregnancy:
- bleeding from the genital tract
- profuse watery vaginal discharge (amniotic fluid discharge)
- persistent or severe headache
- blurred vision or flickering of dark dots ("flies") before the eyes
- fever up to 38C or more nine0013 severe abdominal pain
- weakening or absence of fetal movements
- contractions at intervals of 5-10 minutes.

Signs that urgently need to seek medical attention in the postpartum period:
- profuse bleeding (you have to change several pads per hour), bright red or with clots
- purulent, foul-smelling discharge from the genital tract, severe pain in the lower abdomen nine0013 increase in body temperature up to 38 C or more
- soreness, discharge in the area of the postoperative suture on the anterior abdominal wall or in the perineum
- engorgement, soreness, redness of the mammary glands.
#gynecologist #GP11 #obstetrician_gynecologist #health_school #pregnancy #alarm_signs_of_pregnancy #symptoms0003 Perinatal Center MMCC Kommunarka - childbirth under the policy of compulsory medical insurance Everything about the new Perinatal Center in Kommunarka: conditions of stay, features, photo, address, phone. Catalog of maternity hospitals Perinatal center GKB №67 named after. Perinatal Center City Clinical Hospital No. 67 named after. L.A. Vorokhobova - reviews, doctors, registration for childbirth free of charge under compulsory medical insurance. Catalog of maternity hospitals Family Planning and Reproduction Center – childbirth free of charge under compulsory health insurance TsPSiR on Sevastopolskaya - about the center, reviews, doctors, an appointment for childbirth under the MHI policy. Catalog of maternity hospitals Bauman - childbirth under the MHI policy Perinatal Center of the City Clinical Hospital No. 29 named after N.E. Bauman on Hospital Square, 2. Registration for childbirth is free of charge under the compulsory medical insurance policy. Catalog of maternity hospitals O.M. Filatov - childbirth under the MHI policy Maternity hospital GKB No. 15 named after. O.M. Filatov on Vykhino, st. Veshnyakovskaya, d. nine0003 Catalog of maternity hospitals Perinatal center S. Maternity hospital No. 7 GKB im. S.S. Yudina on Kolomensky passage, 4, building 2. Registration for childbirth is free of charge under the MHI policy. Catalog of maternity hospitals Maternity hospital №2 GKB im. F. I. Inozemtseva (formerly maternity hospital No. 20 of the D.D. Pletnev City Clinical Hospital) - childbirth under the compulsory medical insurance policy F.I. Inozemtseva (formerly the Maternity Hospital No. 20 of the Pletnev City Clinical Hospital) on Verkhnaya Pervomaiskaya, 57. Registration for childbirth is free of charge under the CHI policy. nine0003 Catalog of maternity hospitals A.K. Yeramishantseva - childbirth under the policy of OMS Maternity Ward No. 1 of the City Clinical Hospital named after. A.K. Yeramishantsev. Registration for childbirth is free of charge under the compulsory medical insurance policy. Catalog of maternity hospitals Maternity hospital GKB im. Maternity hospital No. 17 GKB im. V.V. Veresaeva on the 800th anniversary of Moscow, house 22. Registration for childbirth is free of charge under the compulsory medical insurance policy. Catalog of maternity hospitals Maternity hospital No. 3 TsPSiR Branch No. 4 - births under the MHI policy Maternity hospital No. 3 TsPSiR on Nezhinskaya, 3. Registration for childbirth is free of charge under the CHI policy. Catalog of maternity hospitals Maternity hospital GKB No. 52 - childbirth under the compulsory medical insurance policy Maternity hospital No. 26 at City Clinical Hospital No. 52 on Sosnovaya, 11. Registration for childbirth is free of charge under the compulsory medical insurance policy. Catalog of maternity hospitals Perinatal center GKB im. M.P. Konchalovsky - childbirth under the policy of compulsory medical insurance Perinatal Center of the City Clinical Hospital named after. Catalog of maternity hospitals F.I. Inozemtseva — childbirth under the compulsory medical insurance policy Maternity hospital No. 36 GKB im. F.I. Inozemtseva on Fortunatovskaya, 1, bldg. 2. Registration for childbirth is free of charge under the CHI policy. Catalog of maternity hospitals Maternity hospital №4 GKB im. V.V. Vinogradova - childbirth under the MHI policy Maternity hospital No. 4 GKB im. V.V. Vinogradova on the street. Novatorov, d. 3. Registration for childbirth is free of charge under the compulsory medical insurance policy. Catalog of maternity hospitals Maternity hospital №27 V.V. Veresaeva - childbirth under the compulsory medical insurance policy Maternity hospital No. 27 (formerly GKB named after S.I. Spasokukotsky) - about the maternity hospital, reviews, doctors, registration for childbirth free of charge under the CHI policy. L.A. Vorokhobov — childbirth under the MHI policy
L.A. Vorokhobov — childbirth under the MHI policy  S. Yudina - childbirth under the MHI policy
S. Yudina - childbirth under the MHI policy  V.V. Veresaeva - childbirth under the policy of compulsory medical insurance
V.V. Veresaeva - childbirth under the policy of compulsory medical insurance  M.P. Konchalovsky in Zelenograd. Registration for childbirth is free of charge under the compulsory medical insurance policy. nine0003
M.P. Konchalovsky in Zelenograd. Registration for childbirth is free of charge under the compulsory medical insurance policy. nine0003