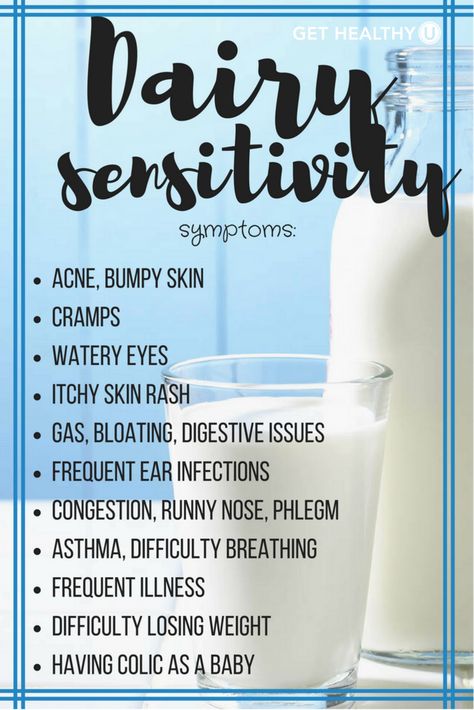
Dairy skin rash
Cow’s milk allergy - Better Health Channel
About cow's milk allergy
An allergy to cow’s milk and related dairy products affects one in 50 in babies and is different to lactose intolerance. Very few adults are allergic to cow’s milk. People who are allergic to cow’s milk can also be allergic to milk from other animals such as goats, sheep and buffalo.
Symptoms of milk allergy vary and range from mild reactions to a severe allergic reaction (anaphylaxis). Some people experience symptoms immediately, but in others, the symptoms can take time to develop.
If you think you, or someone in your care, have a cow’s milk allergy, visit your doctor for a diagnosis. To manage a cow’s milk allergy, all food containing milk must be avoided (under strict medical supervision).
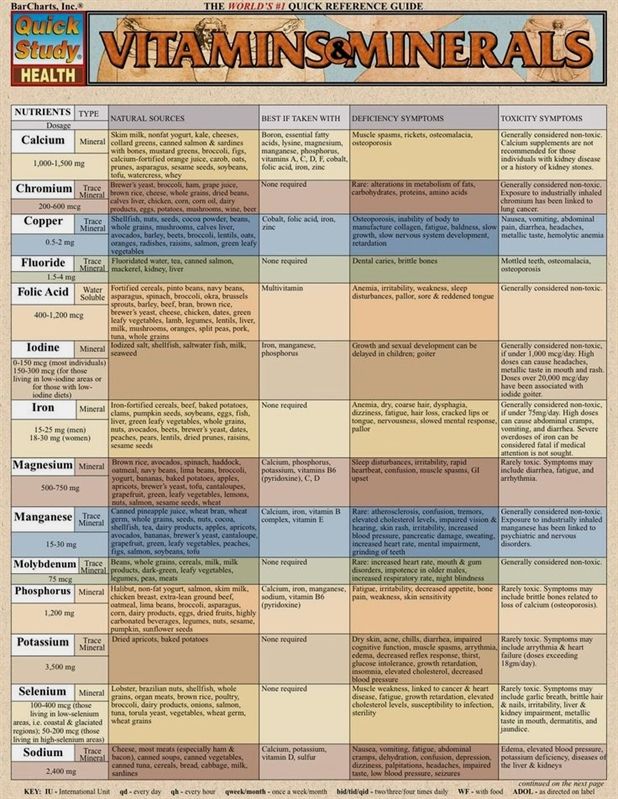
Exclusion and reintroduction of cow's milk and other dairy foods should only be undertaken with advice from a medical specialist (and in many cases, a dietitian), particularly in cases of anaphylaxis. If long-term exclusion is required, an alternative source of calcium and protein is needed, to ensure adequate nutrition and growth.
Do not change your child’s diet without consulting a doctor or your child could suffer from nutritional deficiencies.
Food allergies can be life threatening. If you, or someone in your care, have a severe allergic reaction (anaphylaxis), call triple zero (000) for an ambulance. Do not stand or walk. Administer adrenaline (epinephrine) via injector (EpiPen® or Anapen®), if available.
Causes of cow’s milk allergy
Milk allergy is most commonly caused by an allergy to cow’s milk, although some people are allergic to milk from other animals such as goats, sheep and buffalo.
In all allergies, the immune system reacts to triggers, also known as allergens. Your immune system produces antibodies that detect the allergen, causing inflammatory reactions and the release of chemicals, including histamine, which cause allergic symptoms.
In the case of milk, the triggers are milk proteins including whey and casein. You or your child may be allergic to either one of these proteins, or both.
You or your child may be allergic to either one of these proteins, or both.
More research is needed into the causes, diagnosis and treatment of food allergy.
Some reactions to milk are not caused by allergies
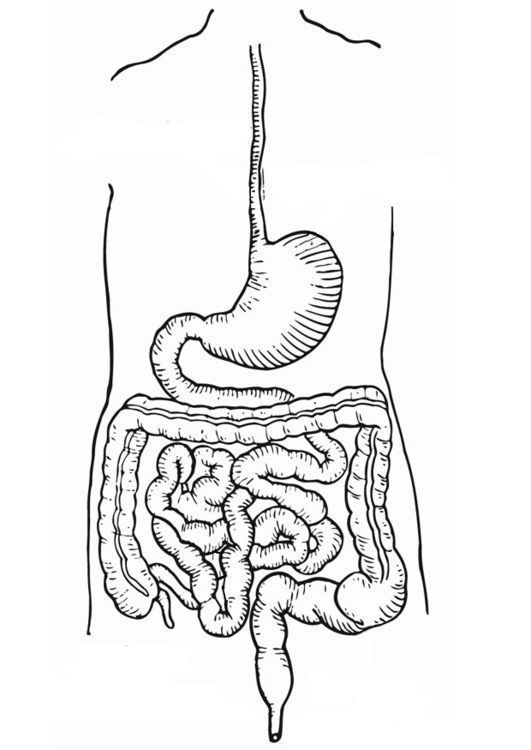
Some people can have a physical reaction to milk that is not due to an allergy. If you lack an enzyme called lactase, which breaks down the milk sugar lactose, you can experience symptoms that seem similar to an allergy (diarrhoea, vomiting, stomach pain and gas). This is called lactose intolerance and is different from milk allergy, because it does not involve your immune system reacting to a trigger.
Some people also experience excess thick mucus in their throat after eating or drinking dairy products, but this is not caused by an allergy. The Australasian Society of Clinical Immunology and Allergy (ASCIA) advises that this mucus production is not a health risk.
Symptoms of cow’s milk allergy
Symptoms of a cow’s milk allergy can appear within minutes or several days of consuming cow’s milk or dairy products. The severity of the symptoms will depend on the person and the amount of cow’s milk they consume.
The severity of the symptoms will depend on the person and the amount of cow’s milk they consume.
Symptoms that can appear within minutes of having a small amount of milk include:
- raised red bumps of skin – hives (urticaria)
- itchy, red, weeping or crusty rash of the skin – dermatitis or eczema
- swelling of the face
- wheeze or persistent cough
- vomiting
- diarrhoea.
If your child is prone to a severe allergic reaction to milk, these symptoms can also appear very rapidly.
Symptoms that can appear within hours include:
- vomiting
- diarrhoea
- rashes or eczema.
Symptoms that can appear within days include:
- eczema
- diarrhoea
- asthma.
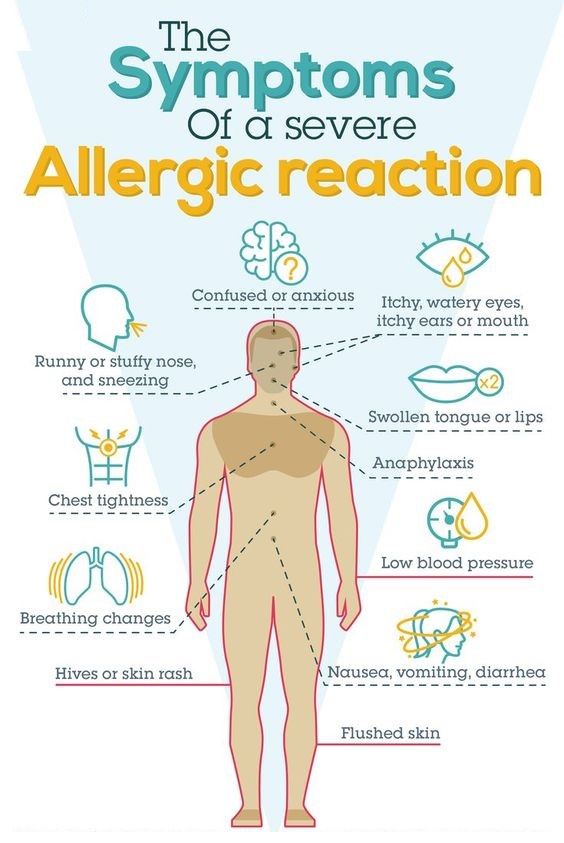
Severe allergic reaction – anaphylaxis
Cow’s milk is one of the most common foods to cause severe allergic reactions. Severe allergic reaction (anaphylaxis) is life threatening.
Symptoms of a severe allergic reaction include:
- difficult or noisy breathing
- swelling of the tongue
- swelling or tightness of the throat
- difficulty talking or hoarse voice
- wheeze or persistent cough
- persistent dizziness or collapse
- paleness and floppiness in young children
If you, or someone your care, have a severe allergic reaction (anaphylaxis), call triple zero (000) for an ambulance.
- Do not stand or walk.
- Administer adrenaline (epinephrine) via injector (EpiPen® or Anapen®), if available.
- Further adrenaline may be given if there is no response after 5 minutes.
- Give adrenaline first, then asthma reliever puffer, if required.
Keep a record of your symptoms
Keep a diary that describes your symptoms or your child’s symptoms and when and where they occur. Your diary could include information about whether the symptoms occur:
- inside your home, outside or both
- for a short time or longer
- at night, during the day or when you wake up
- after you have had a particular food or drink
- after you have taken a particular medication, either prescription or over the counter from a pharmacy or supermarket
- after you have taken a herbal medicine.
Diagnosis of cow’s milk allergy
If you or your child have allergic symptoms, visit your family doctor who will ask some questions about your reactions.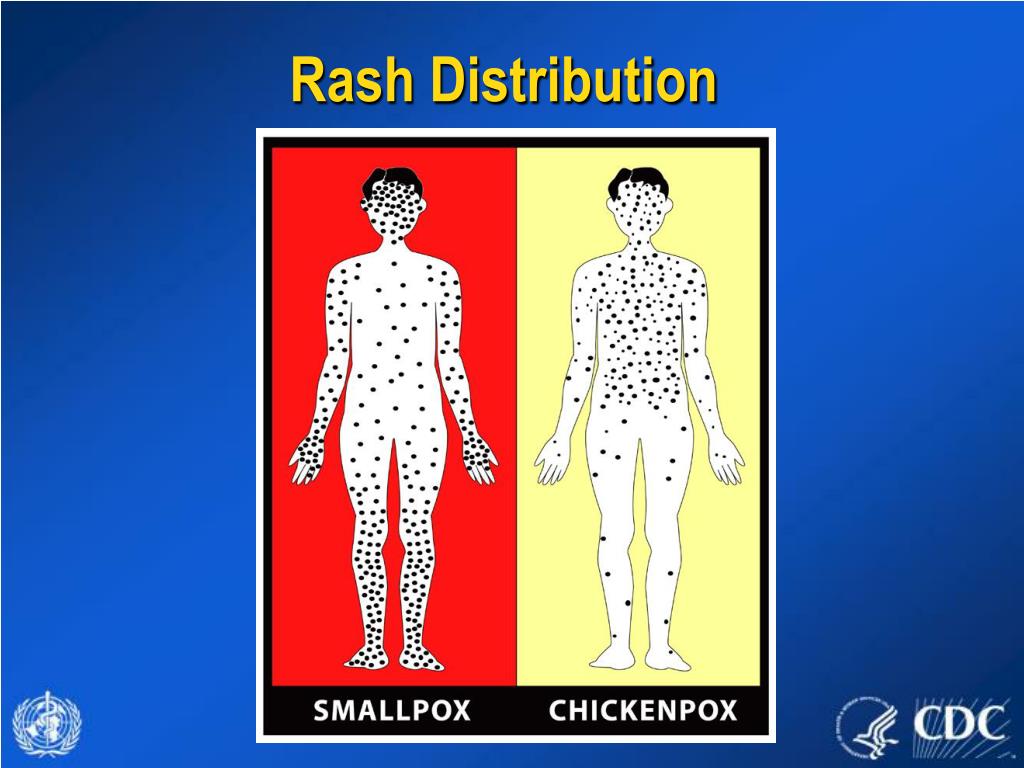 You can also discuss your record of your symptoms. To diagnose your allergy, your doctor may refer you to a clinical immunology/allergy specialist.
You can also discuss your record of your symptoms. To diagnose your allergy, your doctor may refer you to a clinical immunology/allergy specialist.
If your symptoms appear rapidly after eating or drinking milk or dairy products, the allergy may be easier to diagnose, whereas symptoms that take longer to appear make diagnosis more difficult.
Allergists can test for allergies using a number of methods depending on the type of potential allergy. To test for an allergy, the allergist may:
- do a skin prick test
- do a blood test
- ask you to temporarily avoid all milk or products containing milk (elimination diet), then follow up with the introduction of milk back into your diet (food challenge) under strict medical supervision.
A number of methods claim to test for allergies but have not been medically or scientifically proven. They can be costly and could lead to dangerous avoidance of certain foods. The Australasian Society of Clinical Immunology and Allergy (ASCIA) recommends that you do not use certain methods to have potential allergies tested, including:
- cytotoxic food testing
- electrodermal testing
- hair analysis
- iridology
- kinesiology
- pulse testing
- reflexology
- Vega testing.

Always speak with your doctor if you are thinking of using a complementary medicine or therapy for allergies.
Treatment for cow’s milk allergy
If you or your child have been diagnosed with milk allergy, treatment involves total avoidance of milk or products containing milk. This can be difficult to achieve.
The Australasian Society of Clinical Immunology and Allergy (ASCIA) advises that children who are allergic to cow’s milk are often allergic to goat’s milk, and so substitution with a milk of animal origin may not be possible.
To avoid milk and milk products, read food labels and avoid foods that contain milk or milk products such as:
- butter
- buttermilk
- casein and caseinate
- cheese
- chocolate
- cow's or goat's milk – including ‘A2 milk’
- cream
- crème fraiche
- ghee
- ice cream
- margarines that contain milk products
- milk powder
- nougat
- whey
- yoghurt.
ASCIA has more information about dietary avoidance of cow’s milk for food allergy.
Eliminate milk and milk products from your baby or young child’s diet only under strict medical supervision. Your doctor will need to advise on replacement sources of calcium and protein, which are especially important nutrients for children. Replacement formulas for babies also needs to be carefully supervised. For example, some children with cow’s milk allergy will not be able to tolerate soy milk products.
Emergency treatment for severe allergic reactions (anaphylaxis)
If you are at risk of a severe allergic reaction (anaphylaxis), carry an adrenaline injector such as an EpiPen® or Anapen®, an Australasian Society of Clinical Immunology and Allergy (ASCIA) Action Plan for Anaphylaxis and a means of calling for medical assistance, such as a mobile telephone.
Emergency responses for a severe allergic reaction are:
- Lay the person flat – do not allow them to stand or walk.

- Administer adrenaline with an injector into the outer mid-thigh.
- Always dial triple zero (000) to call an ambulance in a medical emergency.
- Further doses of adrenaline may be given if there is no response after 5 minutes.
- Give adrenaline first, then asthma reliever puffer, if required.
If you are at risk of a severe allergic reaction (anaphylaxis) make sure you:
- Have an ASCIA Action Plan for Anaphylaxis.
- Carry an adrenaline injector (such as an EpiPen® or Anapen®) to treat a severe allergic reaction.
- Consider wearing medical identification jewellery – this increases the likelihood that adrenaline will be administered in an emergency.
- Avoid medication (where possible) that may increase the severity of allergic reaction or complicate its treatment such as beta blockers.
- Avoid the food which causes your allergic reaction.
- Tell food staff about your allergy when eating out.
- Seek medical advice from a doctor or clinical immunology/allergy specialist.
Adrenaline injectors are also available over the counter from a pharmacy.
Where to get help
- In an emergency, always call triple zero (000)
- Emergency department of your nearest hospital
- Your GP (doctor)
- NURSE-ON-CALL Tel. 1300 60 60 24 – for health information and advice (24 hours, 7 days)
- St John Ambulance Australia Tel. 1300 360 455
- Australasian Society of Clinical Immunology and Allergy (ASICA)
- Cow’s milk allergy
- Locate a specialist
- Allergy and Anaphylaxis Australia
Milk allergy - Symptoms and causes
Overview
Milk allergy is an atypical immune system response to milk and products containing milk. It's one of the most common food allergies in children. Cow's milk is the usual cause of milk allergy, but milk from sheep, goats, buffalo and other mammals also can cause a reaction.
An allergic reaction usually occurs soon after you or your child consumes milk. Signs and symptoms of milk allergy range from mild to severe and can include wheezing, vomiting, hives and digestive problems. Milk allergy can also cause anaphylaxis — a severe, life-threatening reaction.
Signs and symptoms of milk allergy range from mild to severe and can include wheezing, vomiting, hives and digestive problems. Milk allergy can also cause anaphylaxis — a severe, life-threatening reaction.
Avoiding milk and milk products is the primary treatment for milk allergy. Fortunately, most children outgrow milk allergy. Those who don't outgrow it may need to continue to avoid milk products.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Product for Nursing from Mayo Clinic Store
Symptoms
Milk allergy symptoms, which differ from person to person, occur a few minutes to a few hours after you or your child drinks milk or eats milk products.
Immediate signs and symptoms of milk allergy might include:
- Hives
- Wheezing
- Itching or tingling feeling around the lips or mouth
- Swelling of the lips, tongue or throat
- Coughing or shortness of breath
- Vomiting
Signs and symptoms that may take more time to develop include:
- Loose stools or diarrhea, which may contain blood
- Abdominal cramps
- Runny nose
- Watery eyes
- Colic, in babies
Milk allergy or milk intolerance?
A true milk allergy differs from milk protein intolerance and lactose intolerance. Unlike milk allergy, intolerance doesn't involve the immune system. Milk intolerance requires different treatment from true milk allergy.
Unlike milk allergy, intolerance doesn't involve the immune system. Milk intolerance requires different treatment from true milk allergy.
Common signs and symptoms of milk protein intolerance or lactose intolerance include digestive problems, such as bloating, gas or diarrhea, after consuming milk or products containing milk.
Anaphylaxis
Milk allergy can cause anaphylaxis, a life-threatening reaction that narrows the airways and can block breathing. Milk is the third most common food — after peanuts and tree nuts — to cause anaphylaxis.
If you or your child has a reaction to milk, tell your health care provider, no matter how mild the reaction. Tests can help confirm milk allergy, so you can avoid future and potentially worse reactions.
Anaphylaxis is a medical emergency and requires treatment with an epinephrine (adrenaline) shot (EpiPen, Adrenaclick, others) and a trip to the emergency room. Signs and symptoms start soon after milk consumption and can include:
- Constriction of airways, including a swollen throat that makes it difficult to breathe
- Facial flushing
- Itching
- Shock, with a marked drop in blood pressure
When to see a doctor
See your provider or an allergist if you or your child experiences milk allergy symptoms shortly after consuming milk. If possible, see your provider during the allergic reaction to help make a diagnosis. Seek emergency treatment if you or your child develops signs or symptoms of anaphylaxis.
If possible, see your provider during the allergic reaction to help make a diagnosis. Seek emergency treatment if you or your child develops signs or symptoms of anaphylaxis.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
All true food allergies are caused by an immune system malfunction. If you have milk allergy, your immune system identifies certain milk proteins as harmful, triggering the production of immunoglobulin E (IgE) antibodies to neutralize the protein (allergen). The next time you come in contact with these proteins, IgE antibodies recognize them and signal your immune system to release histamine and other chemicals, causing a range of allergic signs and symptoms.
There are two main proteins in cow's milk that can cause an allergic reaction:
- Casein, found in the solid part (curd) of milk that curdles
- Whey, found in the liquid part of milk that remains after milk curdles
You or your child may be allergic to only one milk protein or to both. These proteins may be hard to avoid because they're also in some processed foods. And most people who react to cow's milk will react to sheep, goat and buffalo milk.
These proteins may be hard to avoid because they're also in some processed foods. And most people who react to cow's milk will react to sheep, goat and buffalo milk.
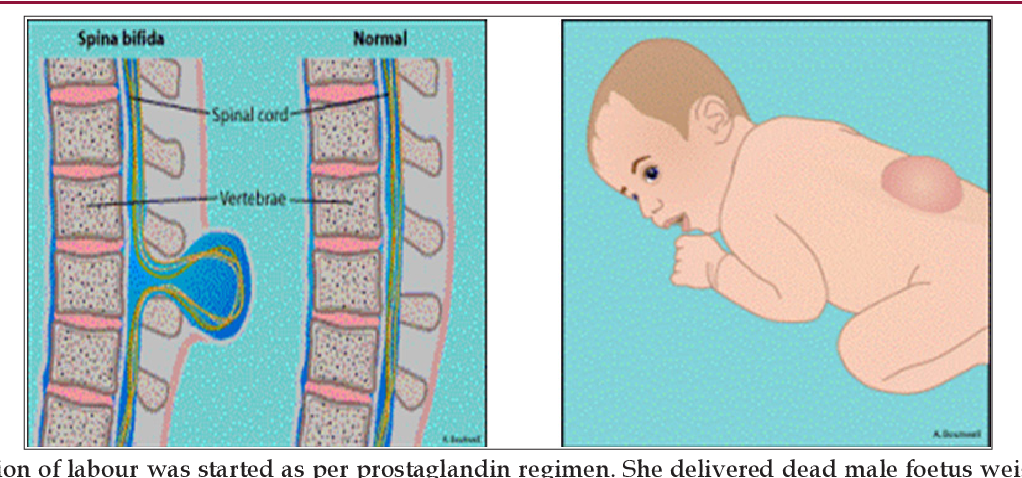
Food protein-induced enterocolitis syndrome (FPIES)
A food allergen can also cause what's sometimes called a delayed food allergy. Although any food can be a trigger, milk is one of the most common. The reaction, commonly vomiting and diarrhea, usually occurs within hours after eating the trigger rather than within minutes.
Unlike some food allergies, FPIES usually resolves over time. As with milk allergy, preventing an FPIES reaction involves avoiding milk and milk products.
Risk factors
Certain factors may increase the risk of developing milk allergy:
- Other allergies. Many children who are allergic to milk also have other allergies.
 Milk allergy may develop before other allergies.
Milk allergy may develop before other allergies. - Atopic dermatitis. Children who have atopic dermatitis — a common, chronic inflammation of the skin — are much more likely to develop a food allergy.
- Family history. A person's risk of a food allergy increases if one or both parents have a food allergy or another type of allergy or allergic disease — such as hay fever, asthma, hives or eczema.
- Age. Milk allergy is more common in children. As they age, their digestive systems mature, and their bodies are less likely to react to milk.
Complications
Children who are allergic to milk are more likely to develop certain other health problems, including:
- Nutritional deficiencies. Because of dietary restrictions and feeding challenges, children with milk allergy may have slowed growth as well as vitamin and mineral deficiencies.
- Reduced quality of life.
 Many common, and sometimes unexpected, foods contain milk, including some salad dressings or even hot dogs. If you or your child is severely allergic, avoiding milk exposure may increase stress or anxiety levels when it comes to making food choices.
Many common, and sometimes unexpected, foods contain milk, including some salad dressings or even hot dogs. If you or your child is severely allergic, avoiding milk exposure may increase stress or anxiety levels when it comes to making food choices.
Prevention
There's no sure way to prevent a food allergy, but you can prevent reactions by avoiding the food that causes them. If you know you or your child is allergic to milk, avoid milk and milk products.
Read food labels carefully. Look for casein, a milk derivative, which can be found in some unexpected places, such as in some canned tuna, sausage or nondairy products. Question ingredients when ordering in restaurants.
Sources of milk
Obvious sources of allergy-causing milk proteins are found in dairy products, including:
- Whole milk, low-fat milk, skim milk, buttermilk
- Butter
- Yogurt
- Ice cream, gelato
- Cheese and anything that contains cheese
- Half-and-half
Milk can be harder to identify when it's used as an ingredient in processed foods, including baked goods and processed meats. Hidden sources of milk include:
Hidden sources of milk include:
- Whey
- Casein
- Ingredients spelled with the prefix "lact" — such as lactose and lactate
- Candies, such as chocolate, nougat and caramel
- Protein powders
- Artificial butter flavor
- Artificial cheese flavor
- Hydrolysates
Even if a food is labeled "milk-free" or "nondairy," it may contain allergy-causing milk proteins — so you have to read the label carefully. When in doubt, contact the manufacturer to be sure a product doesn't contain milk ingredients.
When eating out, ask how foods have been prepared. Does your steak have melted butter on it? Was your seafood dipped in milk before cooking?
If you're at risk of a serious allergic reaction, talk with your health care provider about carrying and using emergency epinephrine (adrenaline). If you have already had a severe reaction, wear a medical alert bracelet or necklace that lets others know you have a food allergy.
Milk alternatives for infants
In children who are allergic to milk, breastfeeding and the use of hypoallergenic formula can prevent allergic reactions.
- Breastfeeding is the best source of nutrition for your infant. Breastfeeding for as long as possible is recommended, especially if your infant is at high risk of developing milk allergy.
-
Hypoallergenic formulas are produced by using enzymes to break down (hydrolyze) milk proteins, such as casein or whey. Further processing can include heat and filtering. Depending on their level of processing, products are classified as either partially or extensively hydrolyzed. Or they may also be called elemental formulas.
Some hypoallergenic formulas aren't milk based, but instead contain amino acids. Besides extensively hydrolyzed products, amino-acid-based formulas are the least likely to cause an allergic reaction.
- Soy-based formulas are based on soy protein instead of milk.
 Soy formulas are fortified to be nutritionally complete — but, unfortunately, some children with a milk allergy also develop an allergy to soy.
Soy formulas are fortified to be nutritionally complete — but, unfortunately, some children with a milk allergy also develop an allergy to soy.
If you're breastfeeding and your child is allergic to milk, cow's milk proteins passed through your breast milk may cause an allergic reaction. You may need to exclude from your diet all products that contain milk. Talk to your health care provider if you know — or suspect — that your child has milk allergy and develops allergy signs and symptoms after breastfeeding.
If you or your child is on a milk-free diet, your health care provider or dietitian can help you plan nutritionally balanced meals. You or your child may need to take supplements to replace calcium and nutrients found in milk, such as vitamin D and riboflavin.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Atopic dermatitis in adults: causes and treatment
Atopic dermatitis is treated by a dermatologist
Mild forms of atopic dermatitis can be observed by a general practitioner (pediatrician, internist). If the allergic nature of the disease is suspected or proven, consultation or observation of an allergist is necessary.
If the allergic nature of the disease is suspected or proven, consultation or observation of an allergist is necessary.
In different countries, atopic dermatitis may be referred to as atopic eczema, eczema, neurodermatitis, neurodermatitis.
What is atopic dermatitis
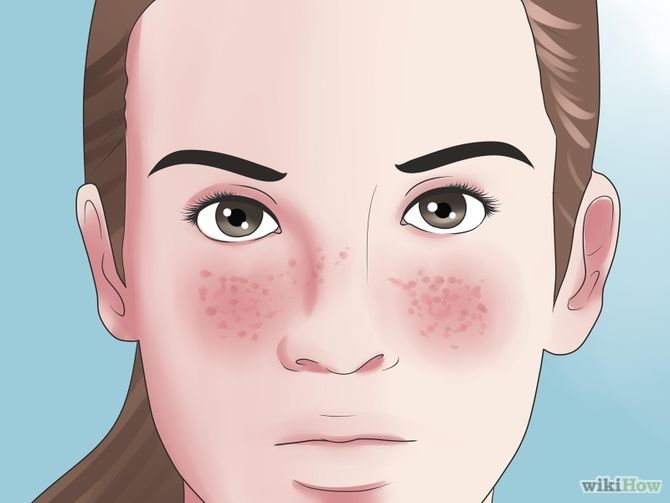
Atopic dermatitis is an inflammatory skin disease that is manifested by redness, rashes, peeling.
As a rule, atopic dermatitis is accompanied by severe itching. It is characterized by a chronic or recurrent (periods of exacerbations alternate with periods of remission) course. In some cases, a state of prolonged and stable remission is possible.
Forms and complications of atopic dermatitis
Atopic dermatitis rashes can look different depending on age. There are infant, child and adult forms of the disease. In addition, two forms of atopic dermatitis are currently distinguished depending on the presence of atopy - atopic and non-atopic.
In the atopic form, there is a connection of exacerbations with food, house dust allergens, less often pollen. Often there are other atopic diseases: bronchial asthma, allergic rhinitis - both in the patient himself and in his close relatives.
The existence of other forms of atopic dermatitis is also assumed, since in different patients the disease can have a different set of symptoms and proceed in different ways. However, clear markers that allow us to judge what scenario the disease will follow in a particular case have not yet been identified.
Atopic dermatitis can be complicated by the addition of an infection - bacterial, fungal or viral. If the picture of the rash has changed, the general condition is disturbing (fever, lethargy, headache, etc.), you should consult a doctor.
Causes of disease
There is no single reason for the development of atopic dermatitis. The occurrence of the disease is facilitated by a whole range of conditions: genetic characteristics and environmental factors. These include a violation of the protective function of the skin (it becomes more vulnerable to the effects of detergents or other irritants), features of the immune system, climatic conditions (temperature, humidity, dust, tobacco smoke and other impurities in the environment). The possible impact of the microbiome is being studied.
These include a violation of the protective function of the skin (it becomes more vulnerable to the effects of detergents or other irritants), features of the immune system, climatic conditions (temperature, humidity, dust, tobacco smoke and other impurities in the environment). The possible impact of the microbiome is being studied.
Symptoms
- Eruptions on the skin
- Itching
- Dryness and flaking of the skin
Stages of atopic dermatitis
Atopic dermatitis proceeds with stages of exacerbation (there are clinical manifestations, complaints) and remission (there are no manifestations of the disease).
In some patients, remissions are short-term and may last only a few days after treatment is discontinued. This course of atopic dermatitis is called severe and requires long-term maintenance treatment. In other cases, the course is more favorable, and remissions can persist for many years.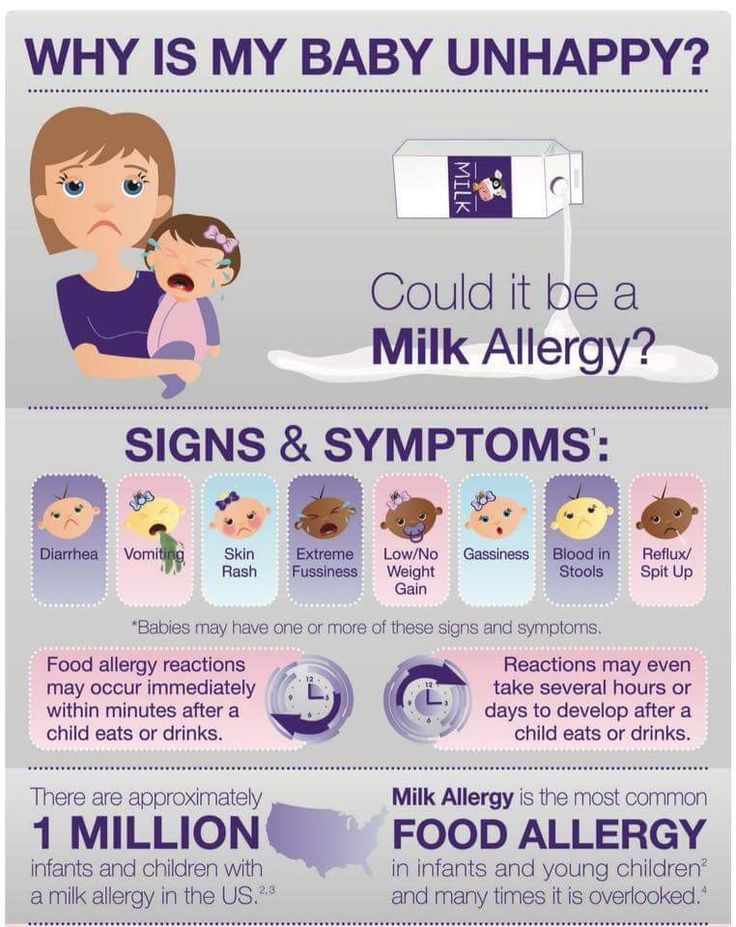
Treatment of atopic dermatitis
A feature of the treatment of atopic dermatitis is a stepwise approach from simpler methods of external therapy and skin care to complex innovative techniques.
Means and methods of treatment of atopic dermatitis
In the treatment of atopic dermatitis are used:
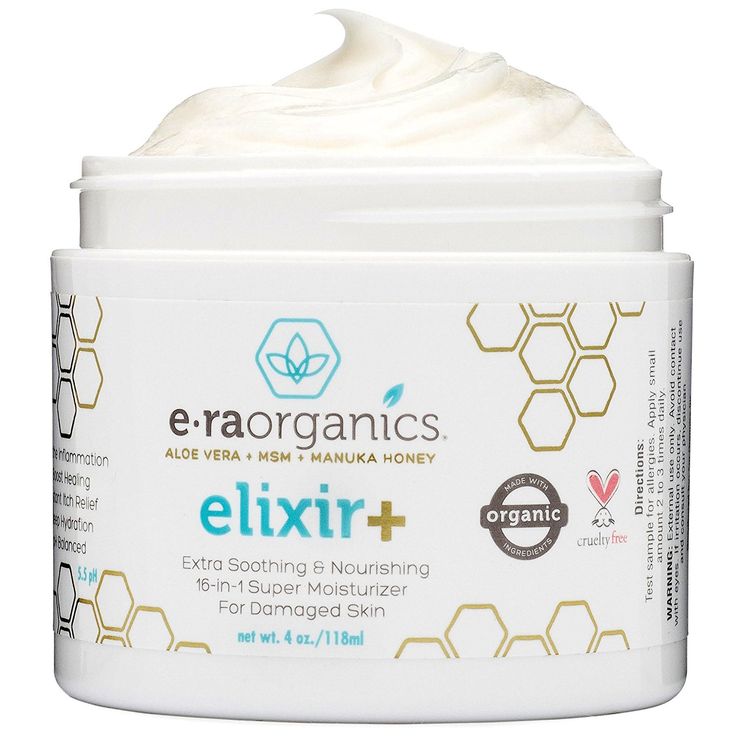
- Emollient and moisturizing creams and ointments are the mainstay of atopic dermatitis treatment. These products keep the skin hydrated and soft.
- Steroid creams and ointments are applied to the skin to help relieve redness and itching. In severe cases, steroid tablets or injections may be required, but your doctor will keep the course of treatment as short as possible, since the high effectiveness of injections is combined with a high risk of side effects.
- Medications that affect the immune system are highly effective but have side effects and may be used when safer treatments have failed.
- Antihistamines may be used in patients who report improvement in pruritus.
- To increase the effectiveness of therapy, it is possible to carry out wet wraps (Wet Dressing, Wet Wrap Therapy).
Wet Dressing, Wet Wrap Therapy
Treatment with Wet Wrap Therapy helps to quickly clear the skin of rashes and can be used both in a medical institution or hospital, and at home. The effect is associated with improved penetration of the drug used, deeper and longer hydration, and a decrease in skin water loss. Dressings provide protection against scratching, which leads to the formation of an itch-scratch cycle, preventing scratches that further increase itching, which improves skin healing. Cooling the surface of inflamed skin by evaporating water from the dressings helps reduce inflammation, itching, and soreness.
For severe eczema, wet wraps are prescribed in a medical facility. They can also be used at home to maintain good health or at the first sign of deterioration and reduce the need for medical attention and the likelihood of hospitalization.
There are various modifications of Wet Wrap Therapy, the essence of the method is the use of external drugs (emollients or steroids) under two layers of dressings. The bottom layer is warm and moist, on top of which a second dry layer is made. For a bandage, you can use a regular bandage, special tubular bandages or special clothing. The bottom layer must be periodically moistened with ordinary warm water, preventing it from drying out. The use of topical steroids under a wet dressing can increase the effectiveness of treatment. The procedure can be carried out 1-2 times a day, daily, during the period of exacerbation. With a decrease in exacerbation, the procedure can be done less frequently, conducting 1-2 times a week during the remission period. With good tolerance, the bandage with the medicine can be left overnight, remembering to periodically moisten the bottom layer of tissue.
The procedure takes quite a long time, and in the early stages (especially in patients with severe skin lesions) may require the participation of medical personnel. After training and improvement in the condition, the procedure can be continued at home.
After training and improvement in the condition, the procedure can be continued at home.
Benefits of atopic dermatitis treatments
- Wet wraps . Wet wraps make external therapy more effective by increasing the penetration of hormonal ointments or creams (topical steroids) into the deeper layers of the skin, better coverage of the skin surface with emollient components, reducing water loss and creating a mechanical obstacle to combing. This allows you to reduce the duration of use, use hormonal ointments of less activity, quickly reduce dry skin and itching. In some cases, it avoids the appointment of systemic therapy with corticosteroid hormones or immunosuppressive agents.
- Immunosuppressive agents used in the treatment of atopic dermatitis may be topical (as ointments and creams) and systemic (as injections or tablets). Preparations of this group are used externally with insufficient effectiveness of corticosteroid hormones, with the localization of rashes in areas where the use of external hormonal ointments or creams is best avoided (for example, the face, large skin folds).
 In severe condition (large area of skin lesions, lack of effect from previous treatment), drugs of this group can be administered orally under the strict supervision of a doctor. Immunosuppressive treatment allows you to quickly achieve improvement in the condition, reduce the frequency and duration of application of drugs to the skin (intensive and frequent use of ointments with a large area of rashes can also be a factor that reduces the patient's quality of life). It has fewer side effects than corticosteroids and therefore can be used effectively for a longer time.
In severe condition (large area of skin lesions, lack of effect from previous treatment), drugs of this group can be administered orally under the strict supervision of a doctor. Immunosuppressive treatment allows you to quickly achieve improvement in the condition, reduce the frequency and duration of application of drugs to the skin (intensive and frequent use of ointments with a large area of rashes can also be a factor that reduces the patient's quality of life). It has fewer side effects than corticosteroids and therefore can be used effectively for a longer time.
How is atopic dermatitis treated at Rassvet Clinic?
In order to prescribe the necessary treatment, a dermatologist will examine your skin and ask questions about your condition. It is important to tell your doctor what factors you feel are causing the condition to worsen; what treatment you have already received before, whether it was effective; which medications worked best and which didn't work.
The diagnosis of "atopic dermatitis" is established on the basis of a doctor's examination; there are no specific laboratory diagnostic tests.
Additional studies may be required to clarify the form of the disease. If your doctor is in doubt as to whether your condition is consistent with the diagnosis of atopic dermatitis, a diagnostic skin biopsy (removal of a piece of skin) and a histological examination (examination of the obtained material under a microscope) may be required.
Treatment of atopic dermatitis, depending on the severity of the condition, is carried out according to a stepwise scheme. This means that during periods of improvement, the intensity of treatment may decrease, and in case of deterioration or insufficient effect, more active methods of treatment are added.
Dermatologist Rassvet recommendations for patients with atopic dermatitis
Tips from a dermatologist for a patient with atopic dermatitis and eczema:
Avoid dry skin, use thick, emollient, unscented creams.
Try to exclude factors contributing to the deterioration of the skin condition in atopic dermatitis and eczema:
- dry skin not softened with creams
- heat and profuse sweating
- very dry air
- stress and anxiety
- abrupt change in air temperature
- harsh soaps and cleansers
- perfume
- woolen and synthetic fabrics
Author:
Voronina Vera Removna
dermatologist
Publication date: August 6, 2019
Update date: October 4, 2022
Facial rosacea: symptoms and treatment
In case of eye damage, an ophthalmologist's consultation may be required.
What is rosacea
Rosacea is a chronic inflammatory skin disease. It is manifested by redness and the appearance of dilated vessels on the skin of the face; the appearance of red or pink, rising above the skin, rashes, which in typical cases are located in the central zone of the face (on the nose, chin, on the forehead and cheeks).
Rosacea can occur with periodic improvements and exacerbations.
Forms and complications of rosacea
Previously, several subtypes of the disease were distinguished in accordance with the most pronounced skin changes: erythemato-telangiectatic; papulo-pustular; phymatous; eye. The updated guidelines propose an individualized approach by assessing a set of skin changes in a particular patient.
Previously, conditions such as phimosis (thickening of tissues, usually on the skin of the nose) and eye lesions (ophthalmic rosacea) were considered complications of the disease. Currently, they are evaluated in the complex of detectable changes.
Causes
There are different opinions about the causes of rosacea. Vascular, immunological and hereditary mechanisms of the development of the disease are assumed, which are activated under the influence of various external influences. The starting role of microbes and microscopic mites living on the surface of the skin is considered; exposure to ultraviolet sunlight; possible influence of the bacterium Helicobacter pylori, which lives in the gastrointestinal tract and causes some diseases of the digestive system. The role of bacteria that inhabit the body of mites that live on the surface of the skin and are normal is also discussed, since in most cases the presence of mites on the skin does not lead to adverse consequences for humans in most cases.
The role of bacteria that inhabit the body of mites that live on the surface of the skin and are normal is also discussed, since in most cases the presence of mites on the skin does not lead to adverse consequences for humans in most cases.
None of these factors fully explains the mechanism of the development of the disease, probably the combination of several is important.
The cause of rosacea can be even a short application of hormonal creams and ointments to the skin of the face. A more frequent combination of rosacea with some common diseases (inflammatory diseases of the gastrointestinal tract, metabolic disorders, some tumors) was also revealed. Often rosacea occurs or worsens during menopause and menopause, in which case it may be useful to consult a gynecologist. However, such combinations do not occur in all patients, and the causal relationship remains unclear.
Symptoms of rosacea
- Reddening of the skin of the face
- Rashes
- Itching
- Feeling of discomfort and dryness.
Flow stages
Previously, it was believed that the disease develops according to the stages: redness of the skin, rashes, the formation of bumps and thickenings. Recent data show that the sequence of changes does not always follow a pattern and may differ from patient to patient.
Rosacea treatment
Depending on the individual characteristics of rosacea in a particular patient, agents are used that affect the state of blood vessels, inflammation, and skin microflora. In some cases, treatment is carried out using lasers or surgical techniques.
For all patients with rosacea, special skin care and the exclusion of provoking factors are required.
Features and benefits of rosacea treatment at Rassvet Clinic
Our clinic offers management of patients in accordance with the individual characteristics of rosacea, and not grouping according to previously recommended forms and stages of the disease. This allows for individualized treatment and skin care.
How rosacea is treated at Rassvet Clinic
Before prescribing the necessary treatment, the dermatologist will examine the skin and ask questions about your condition. Ask to talk about the factors that (subjectively) cause deterioration; previous treatment, its effectiveness; the action of drugs.
The diagnosis of rosacea is established on the basis of an examination by a dermatologist. There are no specific laboratory diagnostic tests.
If your doctor is in doubt as to whether your condition is consistent with a diagnosis of rosacea, a diagnostic skin biopsy and histological examination may be required.
At different stages of the disease, control of symptoms is achieved with the help of drugs with different mechanisms of action, they can be used for a long time. With a decrease in the effectiveness of drugs, the treatment regimen is adjusted by the attending physician.
The intensity of therapy may decrease as the condition improves.