Constipation while breastfeeding
Postpartum Constipation: Causes, Treatments, and More
Bringing your new baby home means big and exciting changes in your life and daily routine. Who knew such a tiny human would need so many diaper changes! Speaking of poop, while your little one seems to have a bowel moment every hour, you might be feeling a little backed up.
Postpartum constipation is a common part of having a baby that no one talks about. It doesn’t matter how your pregnancy went, or how you gave birth — you’ll likely have a touch of constipation.
There are several reasons why your bowel movements might not be regular right now. Don’t worry, most are temporary and easy to resolve. Let’s look at the many causes of post-delivery constipation and what you can do to get things moving.
Just like the many miraculous changes in your body during pregnancy, your post-baby body is still changing. As you know, things don’t bounce back just because you’ve given birth. You’re still in recovery and healing mode from this wonderful adventure!
The postpartum period is typically considered the first 42 days after birth. Expect things to slowly get better, but don’t rush yourself.
Some causes of postpartum constipation go away on their own. Others will need a little more nudging until your digestive system is cranking again.
You might have postpartum constipation because:
Your body is still healing
Your baby’s adorable little smile every time you gaze into their eyes almost makes you forget the trauma of delivery, but your body still remembers!
As you heal from the birth you might still have stitches at the episiotomy site if you had a vaginal delivery or the surgical site if you had a cesarean delivery.
This can make you unconsciously (or on purpose) avoid pushing even a little when you really need to go, because it hurts! Even peeing might sting a little for a few days after.
Clenching the round sphincter muscles in your bottom can also happen without you realizing. This natural physical reaction can lead to constipation.
The added weight gain and pressure of carrying a growing baby might have given you hemorrhoids during pregnancy. This can cause pain and blockages that can cause constipation or make it worse.
This can cause pain and blockages that can cause constipation or make it worse.
Pushing during your delivery might have also stretched out or damaged your pelvic floor muscles or the anal sphincter muscles. This can make pushing out poop a bit difficult. Don’t worry this is temporary!
Changes in sleep patterns
As you realized from baby’s first day home, their schedule rules yours. This might mean you’ll be up and feeding your little one at 3 a.m. because they’re wide awake and hungry.
Lack of sleep and fatigue are common problems for new parents. You expected this, but probably didn’t realize the havoc it would play on your mind and body.
Changes in sleep patterns and fatigue can also change your bowel habits. A lack of sleep also leads to more stress, which doesn’t help the constipation.
Stress
Meeting your new little one is joyful and life changing. But bringing a new baby home can be stressful. Especially if this is your first child, there will be unexpected and difficult changes in every part of your day (and night).
It’s perfectly normal to feel stress and anxiety, while also enjoying being with your baby. These feelings — and your lack of sleep — can spike stress hormones like cortisol. High amounts of stress hormones can cause diarrhea in some people and constipation in others. Either way, they mess with your digestive system!
Dehydration and diet
In the flurry of activity of taking care of baby, your own self-care can get neglected. It’s normal to lose some sleep and have to rush through meals because your little bundle of joy is screaming at the top of their lungs.
However, taking care of your health is important for you and baby. Not drinking plenty of water and other liquids throughout the day can lead to dehydration. This is even more important if you’re breastfeeding.
Changes in your diet while you’re breastfeeding can also affect bowel movements.
For example, if you’ve cut out caffeine things may slow down. And if you don’t have time to eat crunchy salads and other high-fiber foods, you might be low in fiber. This can also cause constipation.
This can also cause constipation.
Moving around less
Cuddling and feeding your little one in a plush rocker or armchair is a wonderful bonding experience for you and baby. You also need this time to put your feet up and rest.
However, less standing, walking, and general activity can also slow down your digestive tract. The intestines are muscles and like your other muscles, they need plenty of exercise to keep them strong and help movement.
Lower activity levels while you’re pregnant and after delivery can temporarily cause constipation.
Medications
Having a baby might have shown you how amazing your body is, but you’re still not a superhero. Well, you are, but not the comic book kind.
You might need pain medications to help you cope with healing stitches, tearing, muscle sprains, and other aches. Unfortunately, constipation is a common side effect of some pain meds.
Antibiotics usually trigger diarrhea but they can sometimes also cause constipation. This is because they get rid of some of the good bacteria that help digestion, along with the bad bacteria.
This is because they get rid of some of the good bacteria that help digestion, along with the bad bacteria.
Even if you’re no longer taking any meds or pain medications, it can take a few days to weeks for your bowels to balance out.
Postnatal vitamins
Just like pregnancy vitamins help keep your nutrition balanced, postpartum vitamins help keep you energized and nourished. Some postpartum supplements include iron and other nutrients that can sometimes cause constipation.
Or you might need iron supplements because you’re slightly anemic after having your baby. You can lose a bit of blood whether you have a vaginal birth or a C-section. This is normal and your body churns out more red blood cells in a few days.
Taking iron supplements for a little while can often help, but since iron leads to constipation you may need to adjust your diet and water intake.
If you’re constipated after delivering your baby, you might need to make just a few tweaks to get things moving.
Home remedies for constipation of all kinds include:
- Hydrate with plenty of water and other liquids.
- Add more fiber to your diet, like whole grains, bran, lentils, beans.
- Eat foods that are natural laxatives, like prunes.
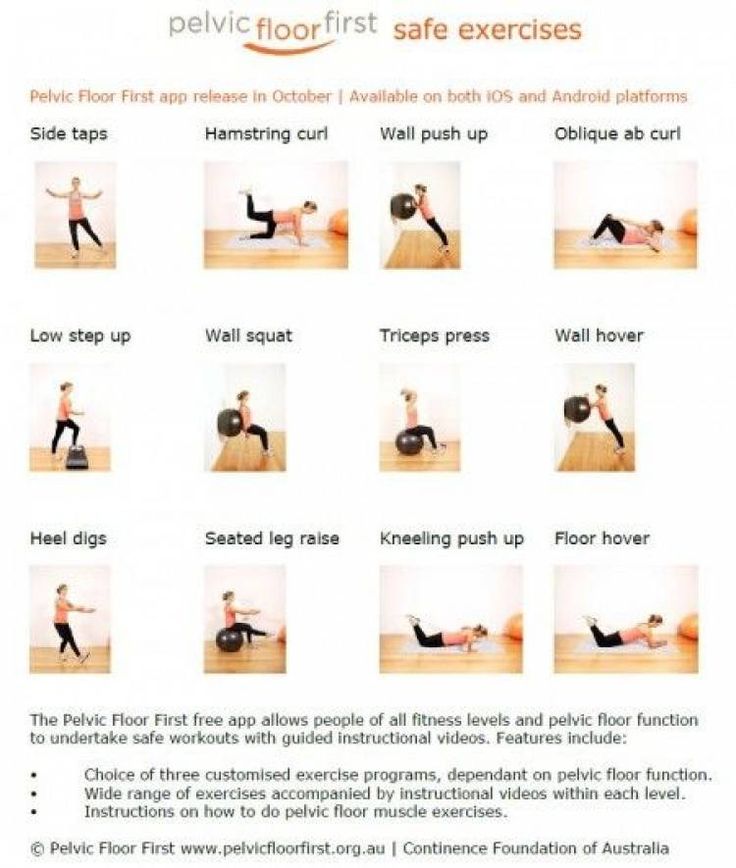
- Move around as much as possible and engage in gentle exercise by doing squats if it is not painful.
- Try over-the-counter laxatives and softeners like psyllium and methylcellulose, bisacodyl, senna, or castor oil.
- Use a stool to elevate your feet in a squatting position while sitting on the toilet to help you push more easily.
- Try calming exercises and relaxation techniques like meditation or a warm bath to help cope with stress.
- Ask friends and family for help with your baby to give yourself some time for self-care and to sleep!
When to see a doctor about postpartum constipation
See your doctor right away if you haven’t had a bowel movement for 4 days after giving birth. You might need a stronger laxative to help rev your digestive tract and relieve constipation. Your doctor might suggest stool softeners like docusate sodium (Colace).
Your doctor might suggest stool softeners like docusate sodium (Colace).
If you don’t already have an OB-GYN, the Healthline FindCare tool can help you find a physician in your area.
Talk to your doctor if you are taking any medication or supplements that might be causing your postpartum constipation. These include pain medications, antibiotics, iron tablets, or a multivitamin. Ask your doctor if it’s OK to stop or change a medication to help get rid of the constipation.
Postpartum constipation is a common issue for new moms. All the changes, stretching, and shifting in your body during pregnancy and delivery can take some time to readjust after you have had your baby.
Most postpartum constipation gets better on its own. You might only need minor changes to your daily diet and exercise plan. Home treatments can help.
In more serious cases, your doctor may need to stop or change certain medications. You might also need stronger, prescription medications to help get rid of the constipation.
Constipation Treatment in Breastfeeding Mothers
This information can also be viewed as a PDF by clicking here.
The information provided is taken from various reference sources. It is provided as a guideline. No responsibility can be taken by the author or the Breastfeeding Network for the way in which the information is used. Clinical decisions remain the responsibility of medical and breastfeeding practitioners. The data presented here is intended to provide some immediate information but cannot replace input from professionals.
Constipation is defined as difficulty in passing bowel motions, which may be described as hard, infrequent or changed in volume and/or consistency. Frequently constipation is caused by a change in diet or by medication. Individual experiences of bowel motions are subjective but constipation affects many people at some time in their lives. It is common towards the end of pregnancy and following pain relief for childbirth when it may be particularly difficult due to perineal stitches. For further information see www.patient.co.uk/health/constipation-in-adults-leaflet
For further information see www.patient.co.uk/health/constipation-in-adults-leaflet
The first remedy should be to increase fruit, vegetable and fibre intake, along with additional water consumption. Exercise may also help to relieve symptoms. If the mother is taking an analgesic (pain relief) medication containing codeine e.g. co-codamol, co-dydramol, this should be stopped and paracetamol and/or a non-steroidal drug such as ibuprofen or diclofenac substituted. If codeine is needed it can be given as a separate tablet of codeine phosphate 15milligrammes and added in as needed to relieve the pain. However, where a medication is required to resolve constipation during breastfeeding, osmotic or bulk laxatives are preferable, at least initially, to stimulant laxatives. Bulk Laxatives are particularly useful where stools are small and hard. However there may be a delay of up to 72 hours before they exert their full effect. Bulk laxatives absorb water within the gut and swell to produce a greater volume of soft stool which is easier to pass e. g. Fybogel®, Regulan®, Isogel®, Normacol®. Absorption of bulk laxatives is minimal and they can all be used during breastfeeding.
g. Fybogel®, Regulan®, Isogel®, Normacol®. Absorption of bulk laxatives is minimal and they can all be used during breastfeeding.
Osmotic laxatives work by increasing the amount of fluid in the large bowel. These also have a delay in action but it is generally shorter than bulk laxatives. They help to produce softer bowel movements, which are easier to pass. E.g. Magnesium Hydroxide, Magnesium Sulphate, Lactulose, Movicol ®. Passage of osmotic laxatives into breastmilk is low and they can all be used during breastfeeding.
Stimulant laxatives should not be used routinely by anyone as they can lead to a reliance on their action. They may cause evacuation of all bowel contents, which then need to re-build before a regular normal bowel action is resumed. They are however, useful for occasional use. They have a more rapid onset of action than bulk or osmotic laxatives, and are usually given at night to help produce a bowel motion the following morning e.g. Senna (Senokot® Ex Lax®,) Bisacodyl (Dulcolax®), Sodium Picosulphate (Laxoberal®, Picolax®).
Side effects in breastfeeding infants have not been proven although loose bowel motions have been reported even with undetectable levels of senna in breastmilk.
- British National Formulary
- Hale T. W Medications in Mothers Milk
- Jones W Breastfeeding and Medication 2018 Routledge
- Lactmed website http://toxnet.nlm.nih.gov/cgi-bin/sis/htmlgen?LACT
- Martindale, the Extra Pharmacopia 2007
©Dr Wendy Jones MBE, MRPharmS and the Breastfeeding Network Sept 2019
Feeding a nursing mother with constipation
Co-author, editor and medical expert - Klimovich Elina Valerievna.
Views: 51 998
The date of the last update: 07.10.2022 G.
Average reading time: 7 minutes
Content:
Power should be diverse and full of
What follows must be included in your diet?
Drink enough fluids
What to do if the child is allergic
What should be excluded from your diet?
Proper nutrition helps nursing mothers take care of the health and well-being of the child and recover faster after childbirth and avoid common problems that many women face.
The diet of a nursing mother should be varied and complete
One of the most common myths about breastfeeding is the need for a woman to follow a strict diet. Recently, being pregnant, she did not deny herself all sorts of goodies and useful things, and now, on the advice of doctors, relatives or friends, she already looks at every product with fear for fear of harming the child. Often, such a period for a young mother lasts long enough, leading to the development of anemia, constipation, and even psychological discomfort.
However, food allergies, which dieters constantly talk about, are connected not so much with the mother's diet, but with heredity and the nature of the child's feeding. Therefore, many women do not have to adhere to too strict rules.
A woman's diet during breastfeeding may not differ much from before. Pregnancy, childbirth and breastfeeding are natural physiological processes, the success of which does not always depend on diet. If we talk about nutrition in this case, then we should not talk about restrictions, but about recommendations. Undoubtedly, nutrition should be varied, complete and as natural as possible. However, this applies not only to the period of breastfeeding, but also to pregnancy.
Undoubtedly, nutrition should be varied, complete and as natural as possible. However, this applies not only to the period of breastfeeding, but also to pregnancy.
Top of page
What should be included in the diet of a breastfeeding mother?
Use:
- lean meat,
- eggs,
- fish,
- dairy products,
- various cereals,
- rice,
- buckwheat,
- potatoes,
- cauliflower,
- bread,
- cheese,
- greens,
- fruits and berries,
- muesli,
- juices.
In this case, it is necessary to carry out heat treatment of milk and dairy products. Whole cow's milk is desirable to alternate with fermented milk products. It is very important that the diet of a nursing woman contains a sufficient amount of dietary fiber . They stimulate intestinal motility, avoiding such a delicate problem of the postpartum period as constipation in a nursing mother. If it still cannot be solved, you can use a product approved for use during lactation - MICROLAX ® .* The micro enema works gently and after 5-15 minutes you can feel relief.
If it still cannot be solved, you can use a product approved for use during lactation - MICROLAX ® .* The micro enema works gently and after 5-15 minutes you can feel relief.
For a long time, breastfeeding mothers were advised to exclude from their diet foods that supposedly dramatically change the taste and smell of milk. They included sharp-smelling spices, onions and garlic, radish, celery, etc. But practice has shown that this is all fiction. They, of course, can affect the taste and smell of milk, but in no way on the baby's appetite and the frequency of attachment to the breast.
Another myth: a number of products can lead to the formation of intestinal colic in a child, bloating and disturbed stools. These traditionally include cabbage, legumes, strong tea, cocoa, milk, cream, black bread, cucumbers, spices, grapes, carbonated drinks. In fact, there is no direct relationship between the mother's diet and the composition of milk. Milk is synthesized from blood and lymph components, not stomach contents. And infantile colic is a frequent phenomenon, and rarely anyone manages to avoid them.
And infantile colic is a frequent phenomenon, and rarely anyone manages to avoid them.
Of course, every mother-child pair is different. If you notice a negative reaction of the child (increased gas formation, restless sleep, etc.) when you use any product, it would be wise to exclude it from the diet.
Back to content
Drink plenty of fluids
Try to drink plenty of fluids . This is especially true for mothers who want to increase lactation. Drink teas, fruit drinks, compotes or plain drinking water. Introduce new drinks gradually, observing the reaction of the child's body. If no changes are observed, then you can increase the volumes daily and fix them in your diet. It is recommended to drink 8-10 glasses of liquid per day, if desired, this amount can be increased. In addition, it favorably affects the functioning of the intestines, avoiding constipation, which most women suffer in the first months after childbirth.
Back to content
What to do if the child is allergic
If at least one of the parents has allergies, then you will have to follow a certain diet. In this case, the child may have a tendency to diathesis, which can manifest itself already during the first months of life. As a rule, the following products are excluded from the mother's diet :
In this case, the child may have a tendency to diathesis, which can manifest itself already during the first months of life. As a rule, the following products are excluded from the mother's diet :
- cow's milk,
- nuts, coffee,
- cocoa,
- chocolate,
- strawberries,
- raspberry,
- citrus fruits,
- sweets,
- chicken,
- pork,
- fish,
- eggs, etc.
In some cases, this list may be longer or, conversely, shorter. After a while, the products are separately introduced into the diet. At the same time, all precautions are observed and the condition of the baby is monitored. If he develops an allergic reaction, the product should be excluded from food for 1 month, and then try again. Try not to completely give up any products. Experts believe that the gradual introduction of allergens through breast milk allows you to avoid allergies in the future.
Back to content
What should be excluded from the diet of a nursing mother in case of constipation?
There are a number of foods that should be avoided from a breastfeeding mother's diet . These include
These include
- canned, fatty, smoked and fried foods,
- semi-finished products.
Although, this rule is relevant not only during lactation, but also in the future. In addition, some foods are potential allergens, so you should use them with caution. These include:
- condensed milk,
- chocolate,
- honey,
- processed cheese,
- carbonated drinks,
- red berries,
- citrus fruits,
- hot spices, etc.
The consumption of alcoholic beverages should also be limited. In moderate amounts, they can reduce lactation and inhibit the milk ejection reflex. With regular use, alcohol has a negative effect on the weight gain of the child, as well as on his sleep and motor development. It is better to completely abandon alcoholic beverages.
Be wary of herbal teas too. Try not to drink teas containing hawthorn (it stimulates heart activity and lowers blood pressure), sweet clover (worsens blood clotting), ginseng (may cause insomnia, sore breasts), chamomile, mint, sage, hop cones (reduce milk production).
Back to Contents
The information in this article is for reference only and does not replace professional medical advice. For diagnosis and treatment, contact a qualified specialist.
* THERE ARE CONTRAINDICATIONS, IT IS NECESSARY TO CONSULT WITH A SPECIALIST
How to help a baby if he has colic
Co-author, editor and medical expert - Klimovich Elina Valerievna.
Number of views: 71,584
Date last updated: 10/21/2022
Average time to read: 8 minutes
in the first months of a baby's life. The term itself comes from the Greek word "colicos", "colon pain". Today it is believed that intestinal colic is evidenced by sudden loud bouts of crying in a child who is well fed and at the same time completely healthy.
Content:
What is the reason?
Features of the appearance of colic in babies
What to do between attacks of colic?
What is the reason?
Improper feeding
This is the most common cause. Colic that occurs against the background of violations of the
Colic that occurs against the background of violations of the
feeding regimen and technique is associated with excessive swallowing of air along with milk and, as a result, the accumulation of gases in the baby's intestines.
When breastfeeding, it is important to monitor whether the baby is fully grasping the areola, how eagerly he sucks, whether the intensity of the mother's milk flow is normal (colic can occur if the intensity is too high).
If the baby is bottle-fed, the occurrence of colic may be due to improper preparation of mixtures, use of inappropriate nipples for age, incorrect position of the bottle during feeding.
The reason for the development of intestinal colic can also be the transition to artificial feeding, frequent changes in mixtures, overfeeding or, conversely, malnutrition of the baby.
Functional immaturity of the digestive tract
This is the second traditional cause of intestinal colic at an early age. Immaturity can also relate to the nervous regulation of the intestines and enzymatic systems. Both that, and another leads to strengthening of fermentation processes. The most pronounced is functional immaturity in premature babies and may be associated with an unfavorable course of pregnancy and childbirth. Other factors: smoking, alcohol consumption by the mother (including during breastfeeding), antibiotics and other drugs in the postpartum period.
Immaturity can also relate to the nervous regulation of the intestines and enzymatic systems. Both that, and another leads to strengthening of fermentation processes. The most pronounced is functional immaturity in premature babies and may be associated with an unfavorable course of pregnancy and childbirth. Other factors: smoking, alcohol consumption by the mother (including during breastfeeding), antibiotics and other drugs in the postpartum period.
Allergies, lactase deficiency, irritants
Lactase deficiency, various types of allergies (including cow's milk protein) are also common causes of colic in a child. Often in such cases, colic is accompanied by the appearance of signs of atopic dermatitis in the baby.
According to another version, the cause of the disease may be the increased sensitivity of the baby to certain environmental factors, for example, when the child is too hot or too cold. Bright lights, weather changes, a wet diaper, etc. are also often annoying factors. Watch a video tutorial from JOHNSON'S Baby on how to change diapers correctly. There is an opinion of experts that intestinal colic can be a kind of indicator of the individuality of the child, that is, they give an idea of whether he will have a “difficult” or “easy” character.
are also often annoying factors. Watch a video tutorial from JOHNSON'S Baby on how to change diapers correctly. There is an opinion of experts that intestinal colic can be a kind of indicator of the individuality of the child, that is, they give an idea of whether he will have a “difficult” or “easy” character.
Up to content
Features of the appearance of colic in babies
Experts distinguish a certain regularity in the manifestation of colic. This is called the "rule of three" and is as follows:
- colic begins by 3 weeks after birth;
- duration is about 3 hours per day;
- colic occurs, as a rule, in babies in
- first three months of life.
Most often, intestinal colic occurs at the age of 2-4 weeks, and before this time, to get enough, the baby needs a small and easily digested amount of food. After reaching 2-4 weeks, the amount of food per day increases, which usually leads to digestive problems
How to identify?
Understanding whether your baby suffers from intestinal colic is easy. As a rule, attacks occur at the same time, mainly in the afternoon. This usually happens during feeding or immediately after it. An attack of colic is accompanied by increased gas formation. Among the external manifestations, reddening of the skin of the face, swelling and tension in the tummy are possible. At the same time, the baby can refuse the breast, clench his hands into fists, tighten his legs, knock his legs. The duration of colic can be from several minutes to 5-6 hours, with short breaks. In such cases, simple sedative measures are usually ineffective. Passing gas or stool can reduce pain. Despite the rather high frequency of colic recurrence, the general condition of the child does not worsen, and in the period between attacks the baby is calm, eats well and puts on weight.
As a rule, attacks occur at the same time, mainly in the afternoon. This usually happens during feeding or immediately after it. An attack of colic is accompanied by increased gas formation. Among the external manifestations, reddening of the skin of the face, swelling and tension in the tummy are possible. At the same time, the baby can refuse the breast, clench his hands into fists, tighten his legs, knock his legs. The duration of colic can be from several minutes to 5-6 hours, with short breaks. In such cases, simple sedative measures are usually ineffective. Passing gas or stool can reduce pain. Despite the rather high frequency of colic recurrence, the general condition of the child does not worsen, and in the period between attacks the baby is calm, eats well and puts on weight.
How can I help?
Pediatricians recommend the following measures to help relieve an attack of intestinal colic and relieve pain in nursing babies.
- Acute pain at the time of intestinal colic is relieved by providing warmth, changing body position and using mechanical means (gas tube, enema).
 The listed measures are applied sequentially: that is,
The listed measures are applied sequentially: that is, - if there is no effect from the previous action, the next one is executed.
- Carry your baby in your arms in a tummy-to-tummy or tummy-to-chest position to keep your baby warm. You can also put the baby on a warm diaper with his back up. Caution is important here, since contact with an overheated diaper can cause a burn on the delicate and thin skin of the baby.
- To relieve pain, you can massage the tummy in a clockwise direction.
Read MICROLAX ® visual material on how to properly massage your baby to relieve colic and help with constipation:
Laxative for children with colic
As a rule, the attack stops after passing flatus and defecation. Therefore, if the above measures were ineffective, you can use a vent tube or an enema. However, a regular enema can be painful for a child because it causes the intestinal walls to stretch due to the large volume of fluid. Given this fact, it is preferable to use a microclyster.
Given this fact, it is preferable to use a microclyster.
Back to Contents
What to do between colic attacks?
In the process of feeding
In the period between attacks during feeding, make sure that the baby's breast capture is correct (the areola should be completely captured). Feeding should take place in a calm environment, comfortable for both mother and baby.
A woman's diet should be varied, but moderate.
Avoid allergenic foods (citrus fruits, chocolate, strawberries, etc.), foods high in fiber (cabbage, brown bread, grapes, etc.), whole milk. It is recommended to reduce the amount of fatty foods and extractives (broths, seasonings) included in the diet, as well as sugar and all kinds of sweets.
After feeding
After the baby has had a meal, hold it upright, stroking it until the air swallowed with the milk is gone. Formula-fed babies with debilitating bouts of colic are usually recommended special therapeutic mixtures that facilitate bowel movements.