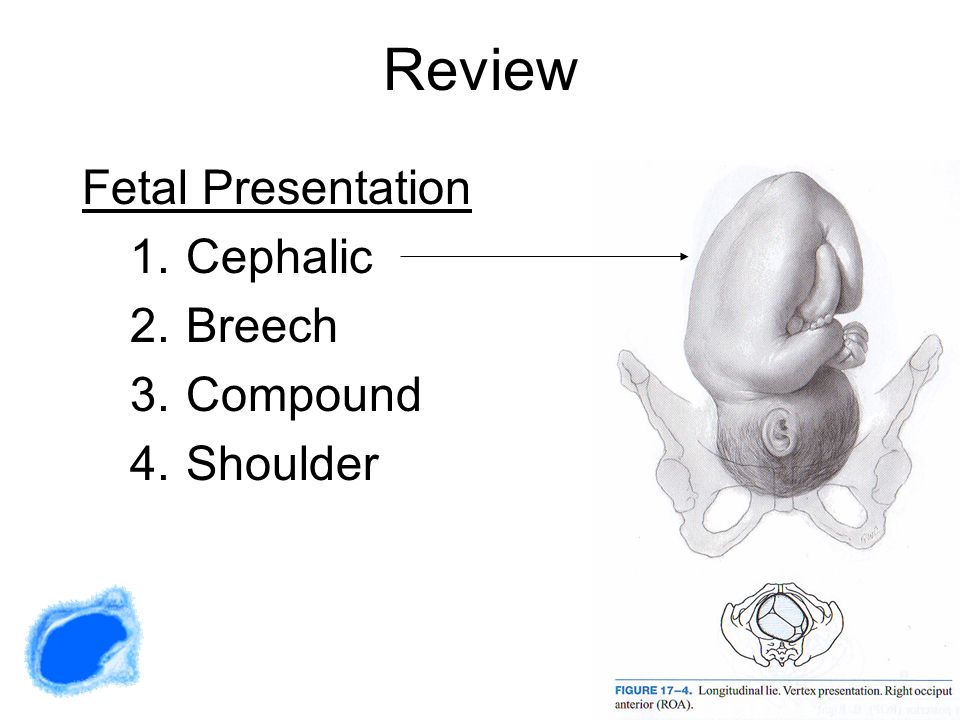
Cephalic presentation in pregnancy
Understanding Your Baby's Presentation at Birth
You know your busy bean is exploring their digs because sometimes you can feel those little feet kick you in the ribs (ouch!) to help propel them along. Just think of them as a little astronaut attached to you — the mother ship — with their oxygen (umbilical) cord.
Your baby may start moving around before you’re barely 14 weeks pregnant. However, you probably won’t feel anything until about the 20th week of pregnancy.
If your baby is bouncing around or turning in your womb, it’s a good sign. A moving baby is a healthy baby. There are even cute names for when you first feel your baby moving, like “fluttering” and “quickening.” Your baby’s movement is most important in the third trimester.
By this time, your growing baby may not be moving that much because the womb isn’t as roomy as it used to be. But your baby can probably still do acrobatic flips and turn himself upside down. Your doctor will closely monitor where your baby’s head is as your due date nears.
Your baby’s position inside you can make all the difference in how you give birth. Most babies automatically get into the head-first cephalic position just before they are born.
If you’re getting closer to your exciting due date, you might have heard your doctor or midwife mention the term cephalic position or cephalic presentation. This is the medical way of saying that baby is bottom and feet up with their head down near the exit, or birth canal.
It’s difficult to know which way is up when you’re floating in a warm bubble, but most babies (up to 96 percent) are ready to go in the head-first position before birth. The safest delivery for you and your baby is for them to squeeze through the birth canal and into the world headfirst.
Your doctor will start checking your baby’s position at week 34 to 36 of your pregnancy. If your baby is not head down by week 36, your doctor might try to gently nudge them into position.
Keep in mind, though, that positions can continue to change, and your baby’s position really doesn’t come into play until you’re ready to deliver.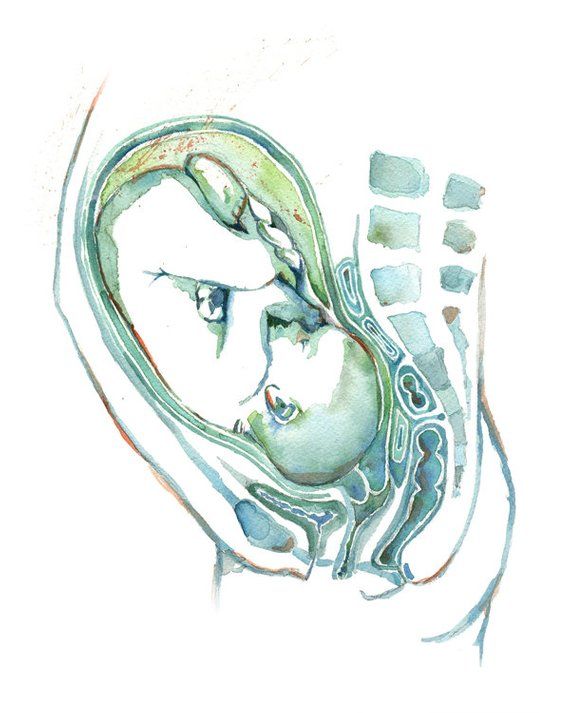
There are two kinds of cephalic (head-down) positions that your little one might assume:
- Cephalic occiput anterior. Your baby is head down and facing your back. Almost 95 percent of babies in the head-first position face this way. This position is considered to be the best for delivery because its easiest for the head to “crown” or come out smoothly as you give birth.
- Cephalic occiput posterior. Your baby is head down with their face turned toward your belly. This can make delivery a bit harder because the head is wider this way and more likely to get stuck. Only about 5 percent of cephalic babies face this way. This position is sometimes called a “sunny side up baby.”
Some babies in the head-first cephalic position might even have their heads tilted back so they move through the birth canal and enter the world face first. But this is very rare and most common in preterm (early) deliveries.
Your baby might settle into a breech (bottom-down) position or even a transverse (sideways) position.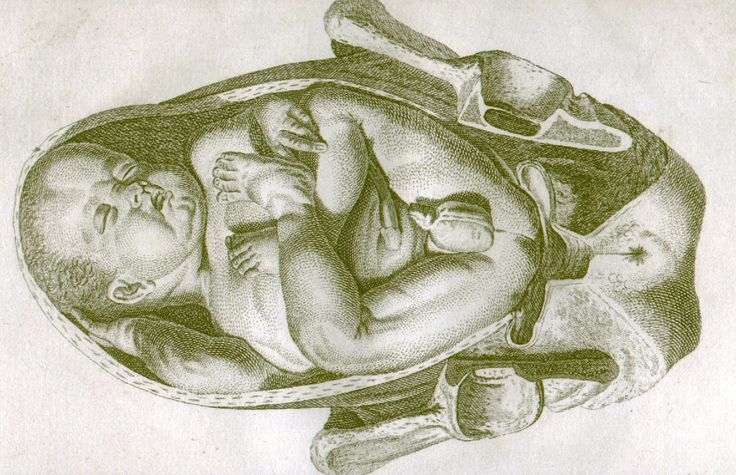
Breech
A breech baby can cause complications for both mom and baby. This is because the birth canal has to open wider if your baby decides to come out bottom first. It’s also easier for their legs or arms to get tangled up a bit as they slide out. However, only about four percent of babies are in the bottom-first position when it’s time for delivery.
There are also different kinds of breech positions your baby could be in:
- Frank breech. This is when your baby’s bottom is down and their legs are straight up (like a pretzel) so their feet are close to their face. Babies are definitely flexible!
- Complete breech. This is when your baby is settled into an almost legs crossed position with their bottom down.
- Incomplete breech. If one of your baby’s legs are bent (like sitting cross-legged) while the other one is trying to kick toward their head or another direction, they’re in an incomplete breech position.
- Footling breech. Just like it sounds, this is one when or both of baby’s feet are down in the birth canal so they would exit foot first.
Transverse
A sideways position where your baby is lying horizontally across your stomach is also called a transverse lie. Some babies start like this close to your due date but then decide to shift all the way into the head-first cephalic position.
So if your baby is settled across your stomach like they’re swinging in a hammock, they may just be tired and taking a break from all the moving before another shift.
In rare cases, a baby can get wedged sideways in the womb (and not because the poor thing didn’t try moving). In these cases, your doctor might recommend a cesarean section (C-section) for your delivery.
Your doctor can find out exactly where your baby is by:
- A physical exam: feeling and pressing over your belly to get an outline of your baby
- An ultrasound scan: provides an exact image of your baby and even which way they’re facing
- Listening to your baby’s heartbeat: honing in on the heart gives your doctor a good estimate of where your baby is settled inside your womb
If you’re already in labor and your baby is not turning into a cephalic presentation — or suddenly decides to acrobat into a different position — your doctor might be concerned about your delivery.
Other things that your doctor has to check include where the placenta and umbilical cord are inside your womb. A moving baby can sometimes get their foot or hand caught in their umbilical cord. Your doctor might have to decide on the spot whether a C-section is better for you and your baby.
You might be able to tell what position your baby is in by where you feel their little feet practice their soccer kick. If your baby is in a breech (bottom-first) position, you might feel kicking in your lower stomach or groin area. If your baby is in the cephalic (head-down) position, they might score a goal in your ribs or upper stomach.
If you rub your belly, you might be able to feel your baby well enough to figure out what position they’re in. A long smooth area is likely your little one’s back, a round hard area is their head, while bumpy parts are legs and arms. Other curved areas are probably a shoulder, hand, or foot. You might even see the impression of a heel or hand against the inside of your belly!
What is lightening?
Your baby will likely naturally drop into a cephalic (head-down) position sometime between weeks 37 to 40 of your pregnancy.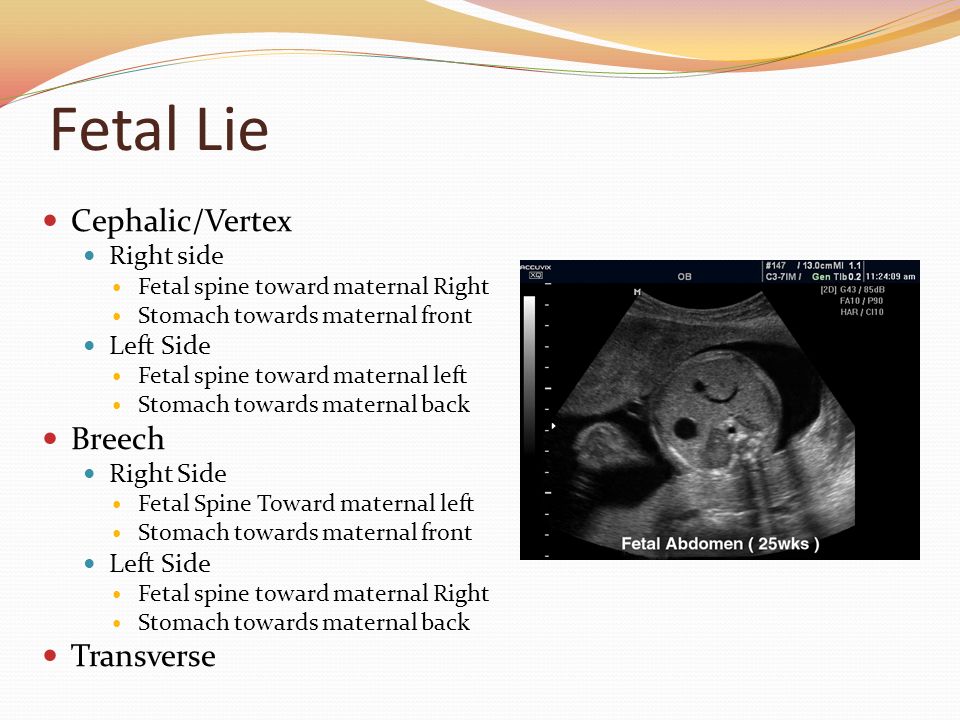 This strategic positional change by your brilliant little one is called “lightening.” You might feel a heavy or full sense in your lower stomach — that’s baby’s head!
This strategic positional change by your brilliant little one is called “lightening.” You might feel a heavy or full sense in your lower stomach — that’s baby’s head!
You might also notice that your belly button is now more of an “outie” than an “innie.” That’s also your baby’s head and upper body pushing against your stomach.
As your baby gets into cephalic position, you might suddenly notice that you can breathe more deeply because they’re not pushing up any longer. However, you might have to pee even more often because your baby is pushing against your bladder.
Stroking your belly helps you feel your baby, and your baby feels you right back. Sometimes stroking or tapping your stomach over the baby will get them to move. There are also some at-home methods for turning a baby, like inversions or yoga positions.
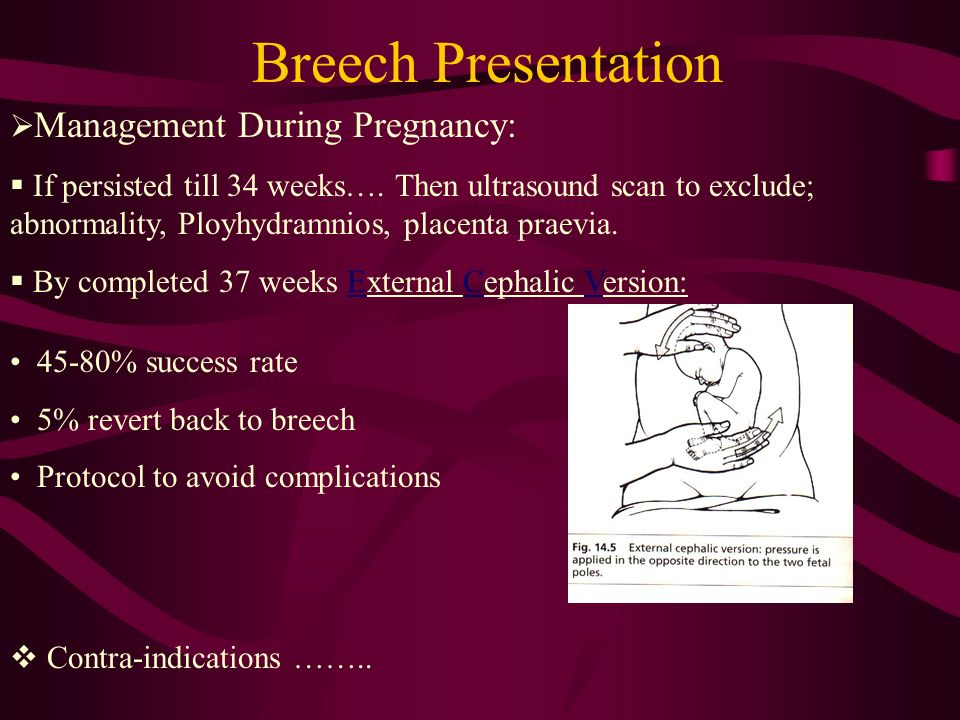
Doctors use a technique called external cephalic version (ECV) to get a breech baby into cephalic position. This involves massaging and pushing on your belly to help nudge your baby in the right direction. In some cases, medications that help you and your muscles relax can help turn your baby.
In some cases, medications that help you and your muscles relax can help turn your baby.
If your baby is already in cephalic position but not quite facing the right way, a doctor can sometimes reach through the vagina during labor to help gently turn baby the other way.
Of course, turning a baby also depends on how large they are — and how petite you are. And if you’re pregnant with multiples, your babies can be changing positions even during birth as the space in your womb opens up.
About 95 percent of babies drop down into the head-first position a few weeks or days before their due date. This is called the cephalic position, and it’s safest for mom and baby when it comes to giving birth.
There are different kinds of cephalic positions. The most common and safest one is where baby is facing your back. If your little one decides to change positions or refuses to float head down in your womb, your doctor might be able to coax him into the cephalic position.
Other baby positions like breech (bottom first) and transverse (sideways) might mean that you must have a C-section delivery. Your doctor will help you decide what’s best for you and your little one when it’s time for delivery.
Your doctor will help you decide what’s best for you and your little one when it’s time for delivery.
Understanding Your Baby's Presentation at Birth
You know your busy bean is exploring their digs because sometimes you can feel those little feet kick you in the ribs (ouch!) to help propel them along. Just think of them as a little astronaut attached to you — the mother ship — with their oxygen (umbilical) cord.
Your baby may start moving around before you’re barely 14 weeks pregnant. However, you probably won’t feel anything until about the 20th week of pregnancy.
If your baby is bouncing around or turning in your womb, it’s a good sign. A moving baby is a healthy baby. There are even cute names for when you first feel your baby moving, like “fluttering” and “quickening.” Your baby’s movement is most important in the third trimester.
By this time, your growing baby may not be moving that much because the womb isn’t as roomy as it used to be.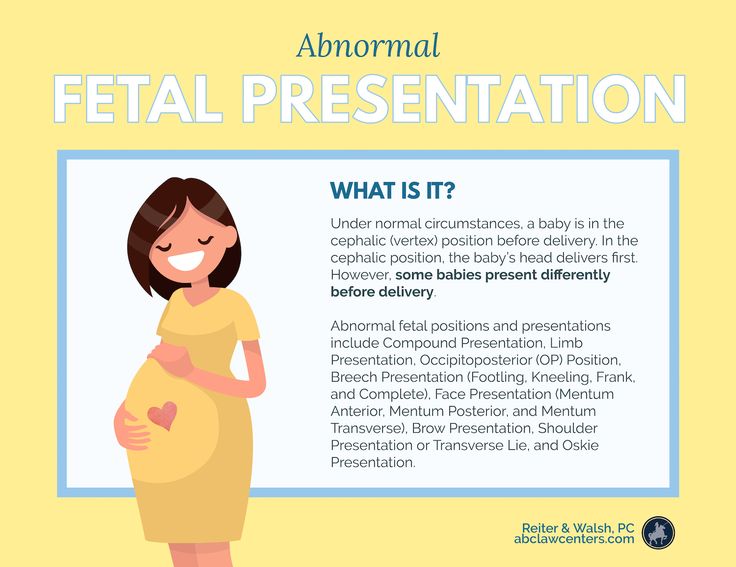 But your baby can probably still do acrobatic flips and turn himself upside down. Your doctor will closely monitor where your baby’s head is as your due date nears.
But your baby can probably still do acrobatic flips and turn himself upside down. Your doctor will closely monitor where your baby’s head is as your due date nears.
Your baby’s position inside you can make all the difference in how you give birth. Most babies automatically get into the head-first cephalic position just before they are born.
If you’re getting closer to your exciting due date, you might have heard your doctor or midwife mention the term cephalic position or cephalic presentation. This is the medical way of saying that baby is bottom and feet up with their head down near the exit, or birth canal.
It’s difficult to know which way is up when you’re floating in a warm bubble, but most babies (up to 96 percent) are ready to go in the head-first position before birth. The safest delivery for you and your baby is for them to squeeze through the birth canal and into the world headfirst.
Your doctor will start checking your baby’s position at week 34 to 36 of your pregnancy.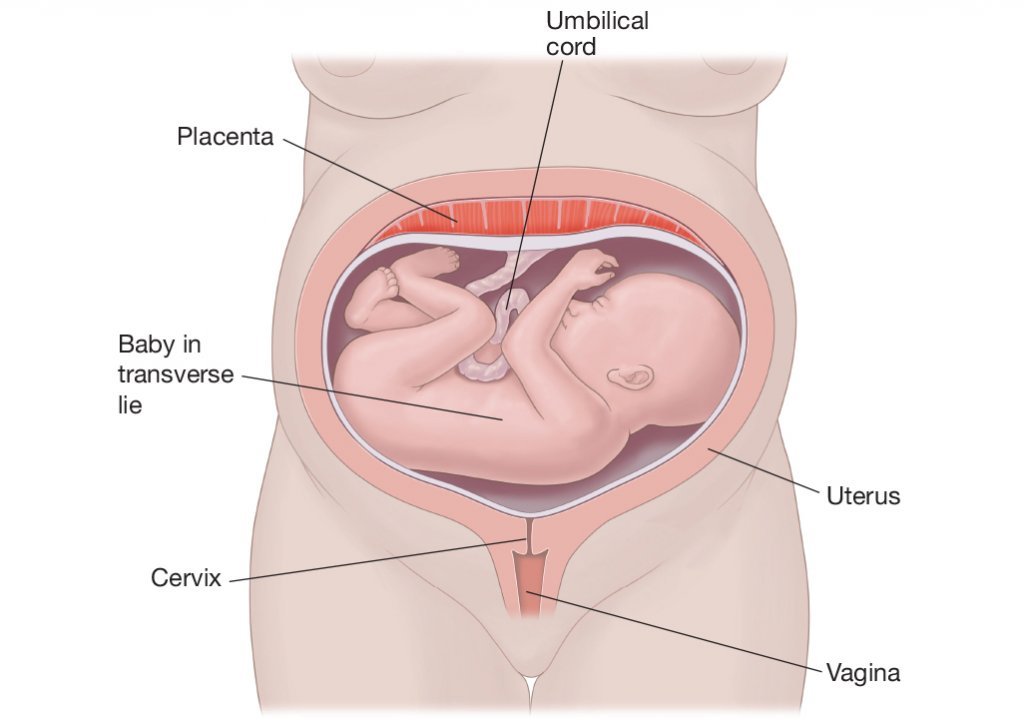 If your baby is not head down by week 36, your doctor might try to gently nudge them into position.
If your baby is not head down by week 36, your doctor might try to gently nudge them into position.
Keep in mind, though, that positions can continue to change, and your baby’s position really doesn’t come into play until you’re ready to deliver.
There are two kinds of cephalic (head-down) positions that your little one might assume:
- Cephalic occiput anterior. Your baby is head down and facing your back. Almost 95 percent of babies in the head-first position face this way. This position is considered to be the best for delivery because its easiest for the head to “crown” or come out smoothly as you give birth.
- Cephalic occiput posterior. Your baby is head down with their face turned toward your belly. This can make delivery a bit harder because the head is wider this way and more likely to get stuck. Only about 5 percent of cephalic babies face this way. This position is sometimes called a “sunny side up baby.”
Some babies in the head-first cephalic position might even have their heads tilted back so they move through the birth canal and enter the world face first. But this is very rare and most common in preterm (early) deliveries.
But this is very rare and most common in preterm (early) deliveries.
Your baby might settle into a breech (bottom-down) position or even a transverse (sideways) position.
Breech
A breech baby can cause complications for both mom and baby. This is because the birth canal has to open wider if your baby decides to come out bottom first. It’s also easier for their legs or arms to get tangled up a bit as they slide out. However, only about four percent of babies are in the bottom-first position when it’s time for delivery.
There are also different kinds of breech positions your baby could be in:
- Frank breech. This is when your baby’s bottom is down and their legs are straight up (like a pretzel) so their feet are close to their face. Babies are definitely flexible!
- Complete breech. This is when your baby is settled into an almost legs crossed position with their bottom down.
- Incomplete breech.
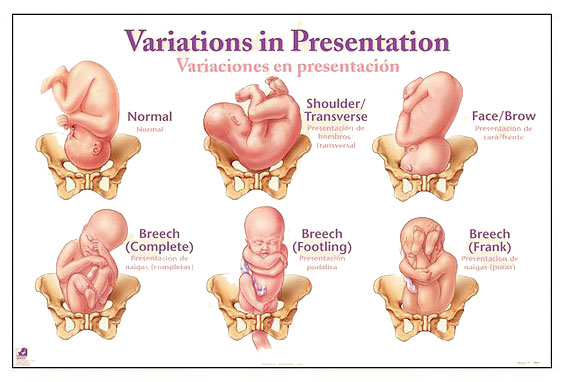 If one of your baby’s legs are bent (like sitting cross-legged) while the other one is trying to kick toward their head or another direction, they’re in an incomplete breech position.
If one of your baby’s legs are bent (like sitting cross-legged) while the other one is trying to kick toward their head or another direction, they’re in an incomplete breech position. - Footling breech. Just like it sounds, this is one when or both of baby’s feet are down in the birth canal so they would exit foot first.
Transverse
A sideways position where your baby is lying horizontally across your stomach is also called a transverse lie. Some babies start like this close to your due date but then decide to shift all the way into the head-first cephalic position.
So if your baby is settled across your stomach like they’re swinging in a hammock, they may just be tired and taking a break from all the moving before another shift.
In rare cases, a baby can get wedged sideways in the womb (and not because the poor thing didn’t try moving). In these cases, your doctor might recommend a cesarean section (C-section) for your delivery.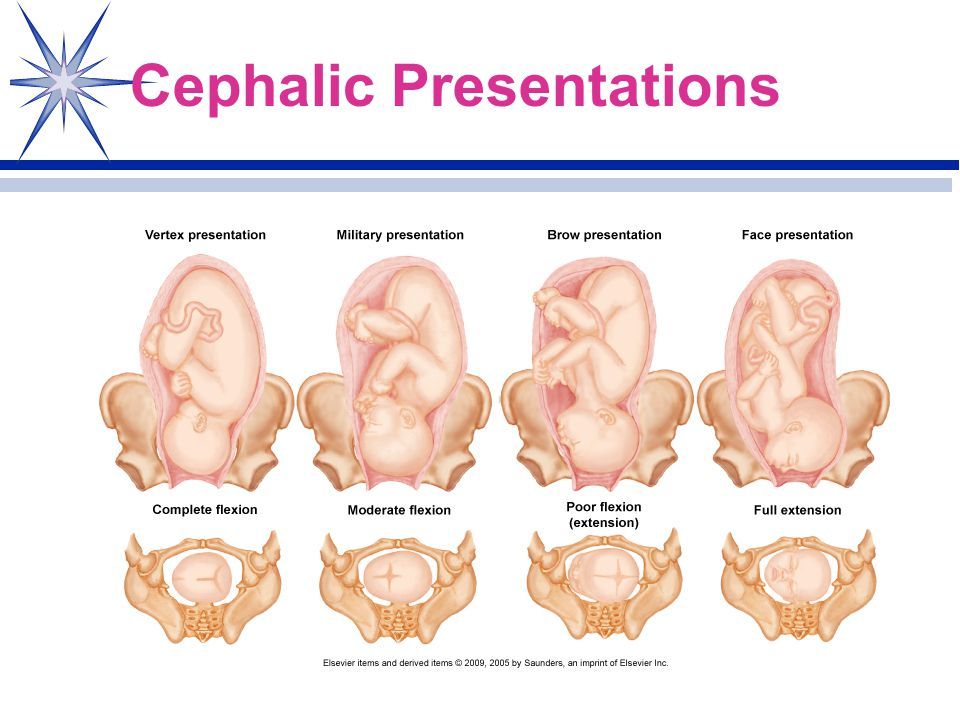
Your doctor can find out exactly where your baby is by:
- A physical exam: feeling and pressing over your belly to get an outline of your baby
- An ultrasound scan: provides an exact image of your baby and even which way they’re facing
- Listening to your baby’s heartbeat: honing in on the heart gives your doctor a good estimate of where your baby is settled inside your womb
If you’re already in labor and your baby is not turning into a cephalic presentation — or suddenly decides to acrobat into a different position — your doctor might be concerned about your delivery.
Other things that your doctor has to check include where the placenta and umbilical cord are inside your womb. A moving baby can sometimes get their foot or hand caught in their umbilical cord. Your doctor might have to decide on the spot whether a C-section is better for you and your baby.
You might be able to tell what position your baby is in by where you feel their little feet practice their soccer kick.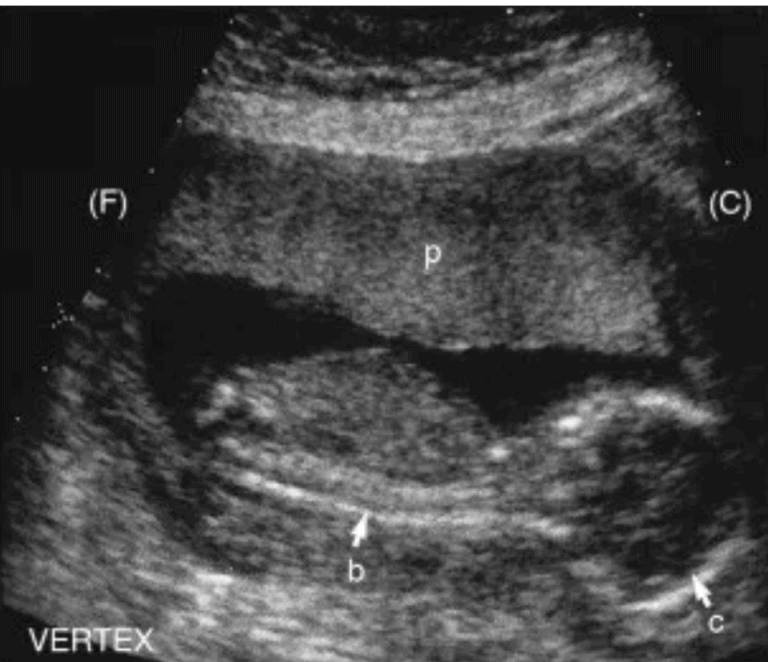 If your baby is in a breech (bottom-first) position, you might feel kicking in your lower stomach or groin area. If your baby is in the cephalic (head-down) position, they might score a goal in your ribs or upper stomach.
If your baby is in a breech (bottom-first) position, you might feel kicking in your lower stomach or groin area. If your baby is in the cephalic (head-down) position, they might score a goal in your ribs or upper stomach.
If you rub your belly, you might be able to feel your baby well enough to figure out what position they’re in. A long smooth area is likely your little one’s back, a round hard area is their head, while bumpy parts are legs and arms. Other curved areas are probably a shoulder, hand, or foot. You might even see the impression of a heel or hand against the inside of your belly!
What is lightening?
Your baby will likely naturally drop into a cephalic (head-down) position sometime between weeks 37 to 40 of your pregnancy. This strategic positional change by your brilliant little one is called “lightening.” You might feel a heavy or full sense in your lower stomach — that’s baby’s head!
You might also notice that your belly button is now more of an “outie” than an “innie.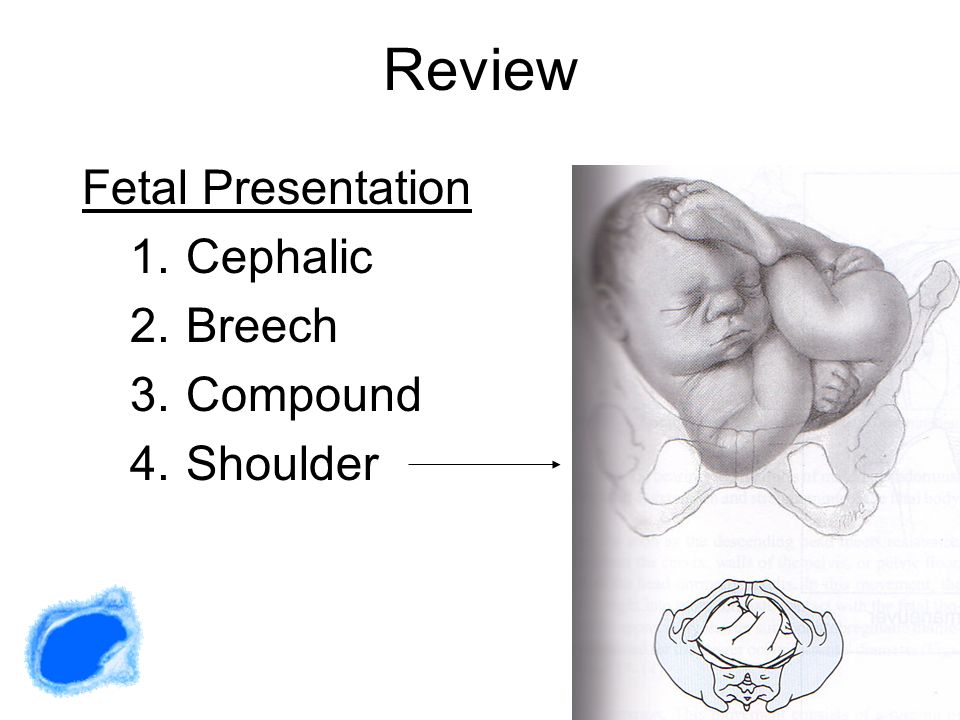 ” That’s also your baby’s head and upper body pushing against your stomach.
” That’s also your baby’s head and upper body pushing against your stomach.
As your baby gets into cephalic position, you might suddenly notice that you can breathe more deeply because they’re not pushing up any longer. However, you might have to pee even more often because your baby is pushing against your bladder.
Stroking your belly helps you feel your baby, and your baby feels you right back. Sometimes stroking or tapping your stomach over the baby will get them to move. There are also some at-home methods for turning a baby, like inversions or yoga positions.
Doctors use a technique called external cephalic version (ECV) to get a breech baby into cephalic position. This involves massaging and pushing on your belly to help nudge your baby in the right direction. In some cases, medications that help you and your muscles relax can help turn your baby.
If your baby is already in cephalic position but not quite facing the right way, a doctor can sometimes reach through the vagina during labor to help gently turn baby the other way.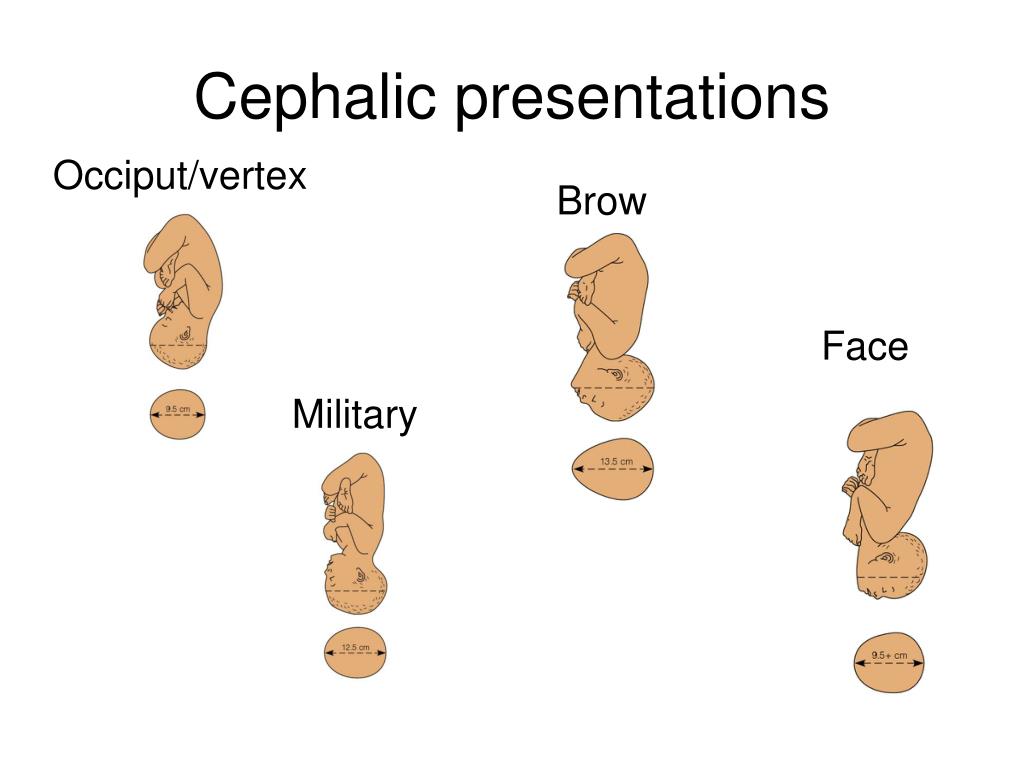
Of course, turning a baby also depends on how large they are — and how petite you are. And if you’re pregnant with multiples, your babies can be changing positions even during birth as the space in your womb opens up.
About 95 percent of babies drop down into the head-first position a few weeks or days before their due date. This is called the cephalic position, and it’s safest for mom and baby when it comes to giving birth.
There are different kinds of cephalic positions. The most common and safest one is where baby is facing your back. If your little one decides to change positions or refuses to float head down in your womb, your doctor might be able to coax him into the cephalic position.
Other baby positions like breech (bottom first) and transverse (sideways) might mean that you must have a C-section delivery. Your doctor will help you decide what’s best for you and your little one when it’s time for delivery.
Pathological position of the fetus - causes, symptoms of the disease, diagnosis and methods of treatment
I confirm More
- INVITRO
- Library
- Directory of diseases
- Pathological...
Pregnancy
Low water
Polyhydramnios
Caesarean section
1112 March 23
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.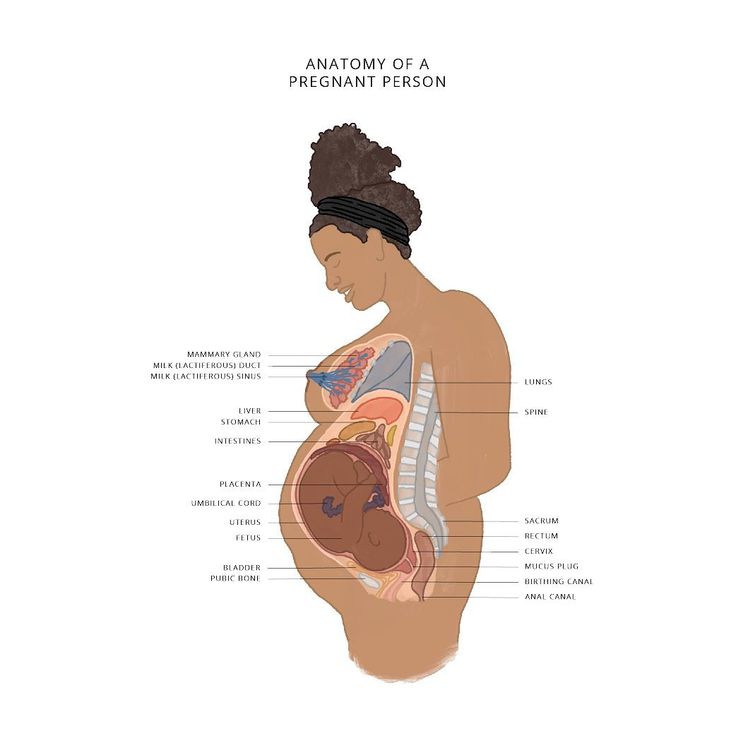
Pathological position of the fetus: causes, symptoms, diagnosis and treatment.
Definition
During pregnancy, the fetus can change its position in the uterus many times, as long as there is enough room for it to move. In a normal pregnancy, by the 22-24th week, the fetus is set head down, until about the 32-34th week, its position remains unstable, but then the fetus is fixed.
The position of the fetus is the ratio of its axis passing through the head and buttocks to the longitudinal axis of the uterus.
If the axes of the fetus and uterus coincide, this is called the longitudinal position of the fetus, if the fetus lies across the uterus - the transverse position. In addition, an oblique position is distinguished - the middle between the longitudinal and transverse.
When the fetus is located longitudinally in the uterus, it can be turned towards the entrance to the small pelvis with the head or pelvic end (buttocks, legs).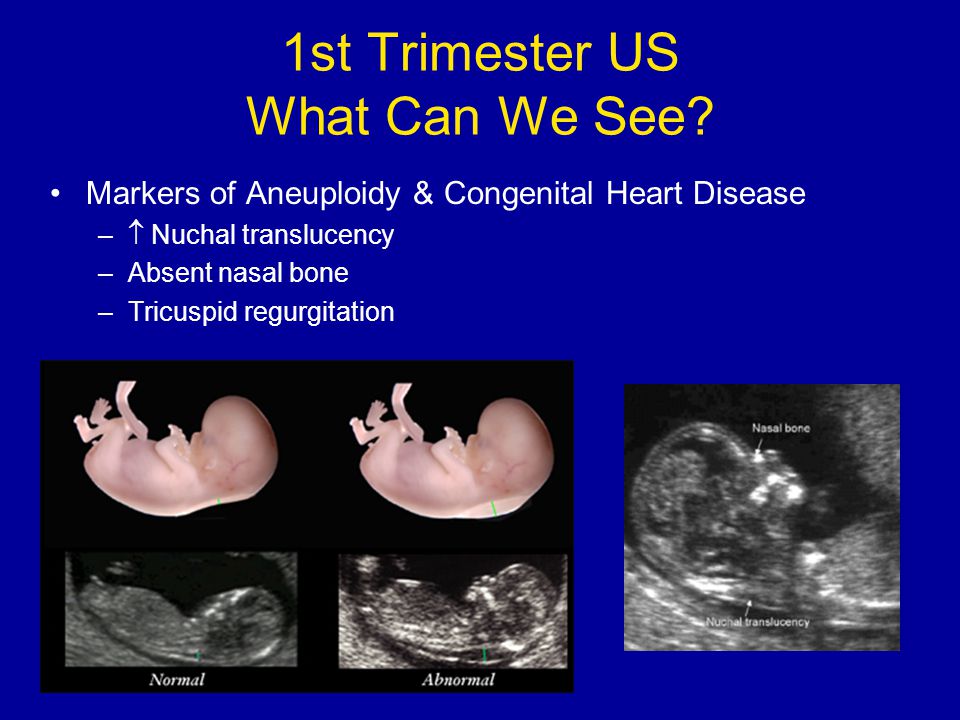 This is the presentation - head or pelvic. In the transverse position, the presenting part is not defined.
This is the presentation - head or pelvic. In the transverse position, the presenting part is not defined.
In 95-97% of cases, the presenting part is the head. Breech presentation, when the buttocks or legs of the fetus are above the entrance to the small pelvis, and its head is at the bottom of the uterus, is determined in 3-5% of cases. Oblique and transverse positions (the so-called incorrect positions of the fetus) are detected in 0.3-0.7% of full-term pregnancies, but 10 times more often in multiple births (starting from 4 births) than in primiparas. With a gestation period of less than 32 weeks, while the fetus has enough space to move, the incorrect position of the fetus in the uterus is observed 6 times more often than with a full-term pregnancy.
Pathological positions include breech presentation, transverse, oblique and unstable position of the fetus.
Causes of the pathological position of the fetus
The exact causes of the pathological position of the fetus are not well understood.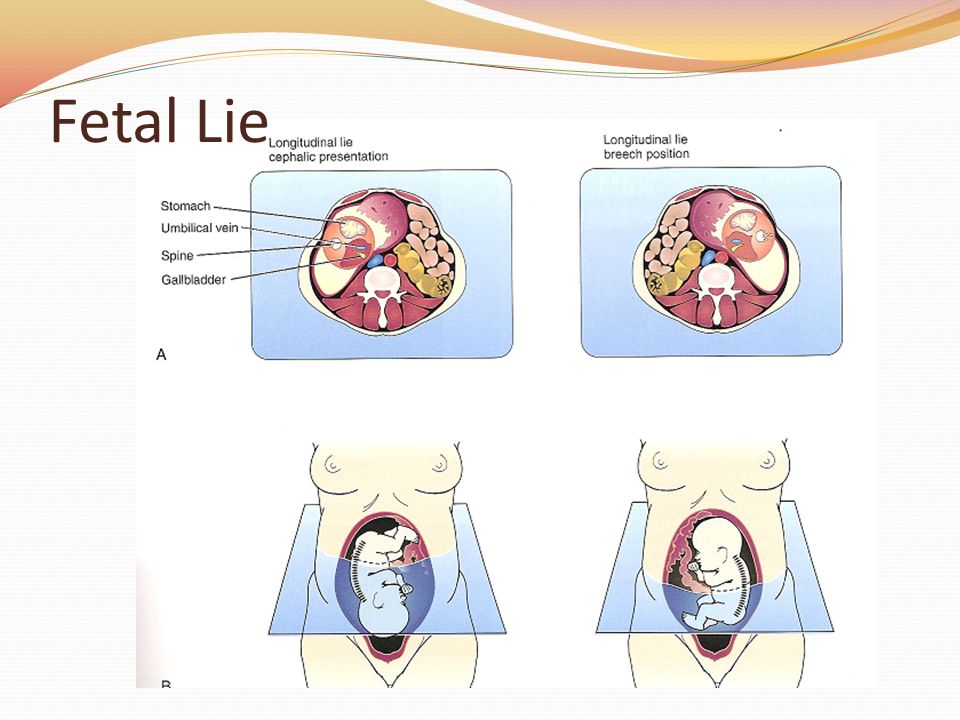 Factors that contribute to the occurrence of breech presentation, transverse and oblique positions can be divided into maternal, fetal and placental.
Factors that contribute to the occurrence of breech presentation, transverse and oblique positions can be divided into maternal, fetal and placental.
Maternal causes include:
- anomalies in the development of the uterus (bicornuate, saddle uterus, uterine septum),
- uterine tumors,
- narrow pregnant pelvis,
- pelvic tumors,
- decreased or increased uterine tone,
- a large number of births in a woman,
- uterine scar after caesarean section.
Fetal causes:
- prematurity,
- multiple pregnancy,
- intrauterine growth retardation,
- congenital fetal anomalies (anencephaly, hydrocephalus),
- abnormal fetal articulation (relation of limbs to head and torso),
- features of the vestibular apparatus of the fetus.
Placental causes:
- placenta previa,
- oligohydramnios or polyhydramnios,
- short cord.
Classification of the pathological position of the fetus
Breech presentation is divided into breech (80-90%) and foot (10-15%). Breech presentation is pure (63-68%) and mixed (20-23%), and foot presentation is complete, incomplete (more common than complete) and knee (rare).
In a purely breech presentation, the buttocks are facing the entrance to the pelvis, and the legs are extended along the body, i.e., bent at the hip and extended at the knee joints, feet are located in the area of the chin and face. With a mixed breech presentation, the buttocks are facing the entrance to the pelvis along with the legs, bent at the hip and knee joints, somewhat unbent at the ankle joints, that is, the fetus is in the “squatting” position.
In full foot presentation, the fetus is turned towards the entrance to the pelvis with both legs slightly extended at the hip and bent at the knee joints; knee joints, located above; in the case of a knee presentation, the legs are unbent at the hip joints and bent at the knee, and the knees are presented to the entrance to the pelvis.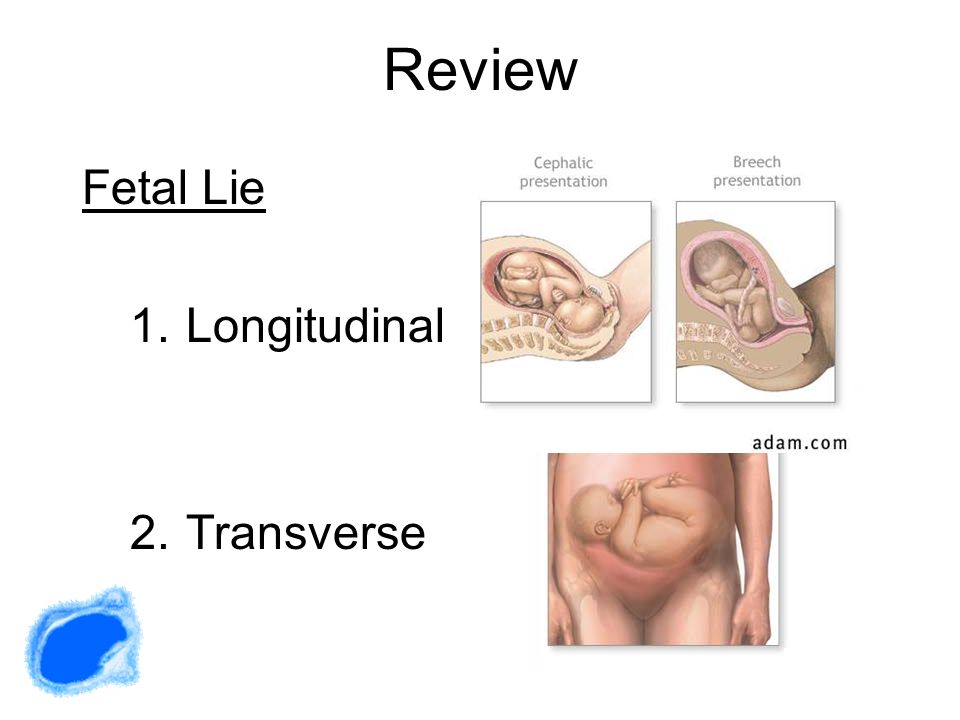
Incorrect include transverse and oblique positions, as well as the unstable position of the fetus.
Transverse is the position of the fetus, in which the axis of its trunk intersects the axis of the uterus at a right angle, and large parts of the fetus are located above the iliac crests. An oblique is a position in which the axis of the fetal body intersects the axis of the uterus at an acute angle, and the underlying large part of the fetus is located in one of the iliac cavities of the large pelvis. The oblique position is considered a transitional state, because at the end of the gestation period and during childbirth, it turns into a longitudinal or transverse position.
The oblique position is usually unstable, temporary, which is why it is often called unstable.
Also, in case of incorrect positions, the position of the fetus is determined by the head: if the head is located to the left of the midline of the pregnant woman's body, this is the first position, if to the right, the second. The view is determined by the back: if it is facing anteriorly - front view, backwards - rear. The location of the back of the fetus in relation to the bottom of the uterus and the entrance to the small pelvis matters.
The view is determined by the back: if it is facing anteriorly - front view, backwards - rear. The location of the back of the fetus in relation to the bottom of the uterus and the entrance to the small pelvis matters.
Symptoms of abnormal fetal position
Usually, with a pathological position of the fetus, the pregnant woman does not have specific complaints, however, she may be disturbed by discomfort in the hypochondria, and in the case of a mixed breech or foot presentation of the fetus, a woman may feel the fetus move mainly in the lower abdomen.
Diagnosis of abnormal fetal position
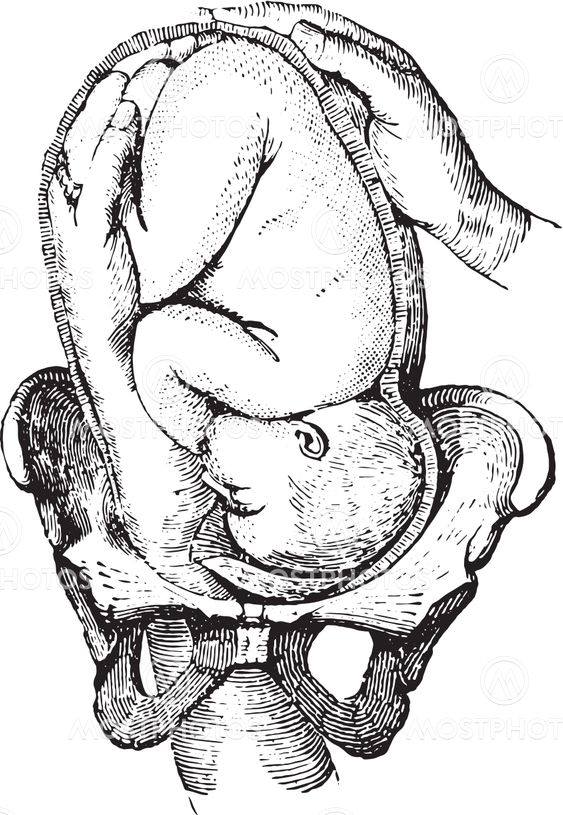
Diagnosis of abnormal fetal position is usually made at 32-34 weeks of gestation. A preliminary diagnosis is established on a gynecological examination. With breech presentation, there is a high standing of the fundus of the uterus. This indicator is determined by the gynecologist at each visit, starting from the 20th week of pregnancy - it reflects the height to which the widest, domed part of the uterus (its bottom) has risen relative to the pubis.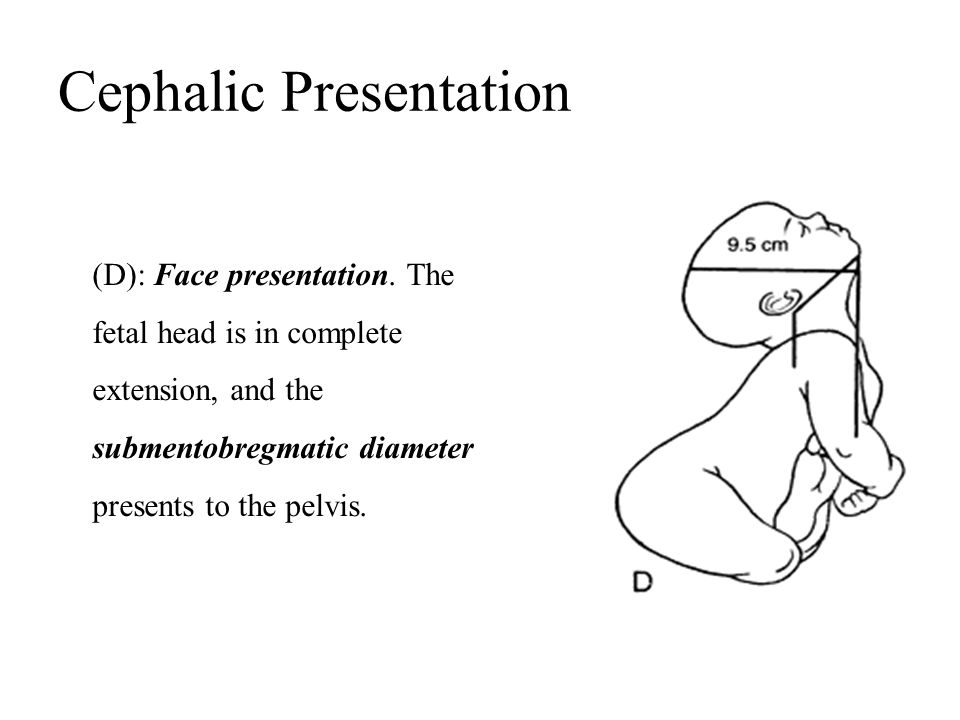 This indicator indirectly indicates whether the pregnancy is proceeding normally. In breech presentation, the pelvic end of the fetus is located high above the entrance to the pelvis, which causes a high standing of the uterine fundus. The fetal head is located in the bottom of the uterus, the buttocks are above the entrance to the pelvis, the doctor can determine this by palpation. The fetal heartbeat is heard at or above the umbilicus.
This indicator indirectly indicates whether the pregnancy is proceeding normally. In breech presentation, the pelvic end of the fetus is located high above the entrance to the pelvis, which causes a high standing of the uterine fundus. The fetal head is located in the bottom of the uterus, the buttocks are above the entrance to the pelvis, the doctor can determine this by palpation. The fetal heartbeat is heard at or above the umbilicus.
The transverse and oblique position of the fetus can also be suspected by the doctor during the examination. In the transverse position, the belly of the pregnant woman acquires a transverse-oval shape, the bottom of the uterus is lower than in the longitudinal position, there is no large presenting part - the head or pelvic end, and small parts of the fetus, for example, a handle or shoulder, are presented at the entrance to the small pelvis. The fetal heartbeat is best heard in the navel.
In an oblique position, the abdomen visually acquires an oblique-oval shape, the abdominal circumference is greater than normal, the fundus of the uterus is low.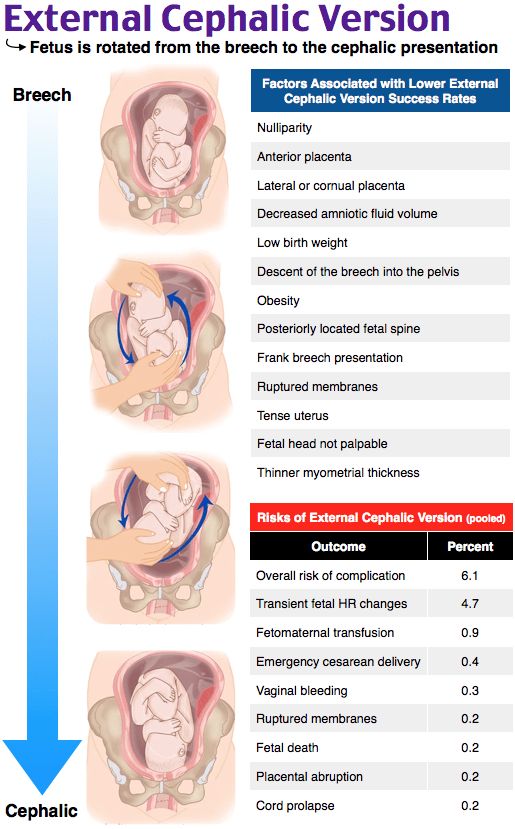 The large presenting part is located below the level of the iliac crest, in one of the iliac fossae of the large pelvis, the fetal heartbeat, as in the transverse position, is better heard in the navel.
The large presenting part is located below the level of the iliac crest, in one of the iliac fossae of the large pelvis, the fetal heartbeat, as in the transverse position, is better heard in the navel.
If the doctor suspects an abnormal position of the fetus, an ultrasound examination is mandatory. When performing ultrasound, reasons that could lead to an incorrect position of the fetus are excluded: severe fetal malformations or an abnormal location of the placenta.
Screening ultrasound of the 3rd trimester of pregnancy (30-34 weeks) with Doppler evaluation of blood flow parameters
Ultrasound examination for functional assessment of intrauterine development of the fetus, its estimated height and weight, as well as blood circulation.
RUB 3,890 Sign up
Which doctors to contact
As in a normal pregnancy, the doctor - obstetrician-gynecologist.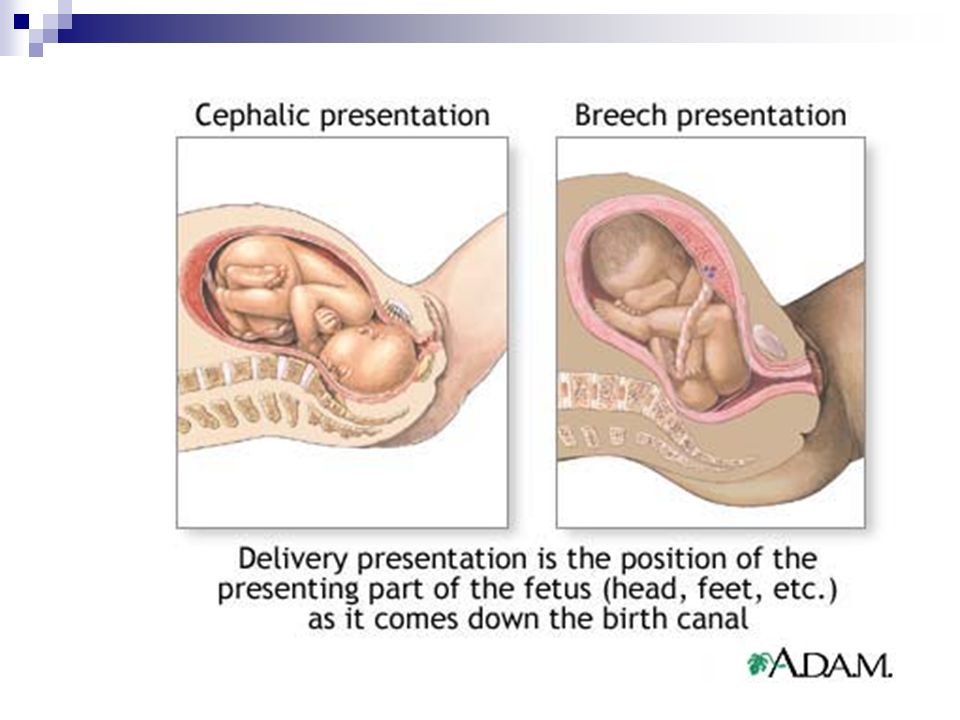
Treatment of abnormal fetal position
Until a certain time, breech presentation requires expectant observation, since the fetus can turn in the right direction on its own. In some cases, doctors may recommend that a pregnant woman perform a set of exercises that help change the breech presentation to the head.
In breech presentation, to reduce the likelihood of a caesarean section and in the absence of contraindications for natural childbirth, the patient may be advised to externally rotate the fetus on the head. Indications and contraindications are determined by the doctor. This procedure is performed by an obstetrician-gynecologist in an obstetric hospital, at a period of ≥36 weeks of gestation in primiparas and ≥37 weeks of gestation in multiparous.
The efficiency of cephalic rotation ranges from 30 to 80%, and in 5% of cases spontaneous reverse rotation of the fetus is observed.
Depending on the situation and the health of the woman and the fetus, the doctor recommends a natural birth or a caesarean section.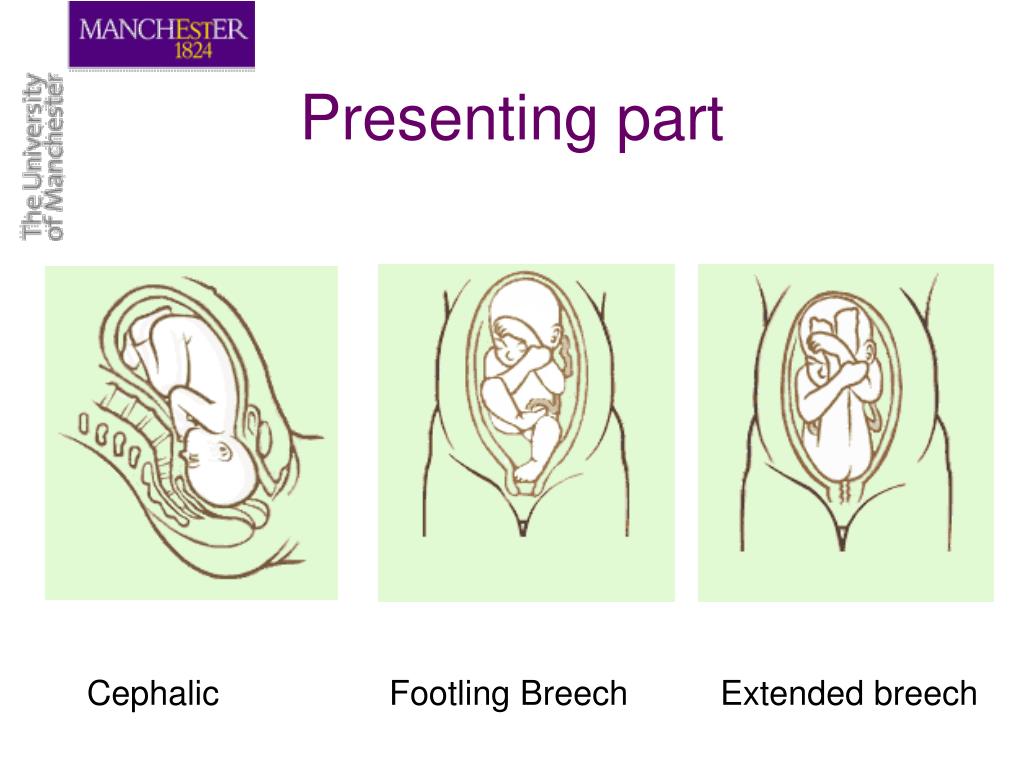
In case of abnormal position of the fetus up to 36 weeks of pregnancy in the absence of contraindications (a scar on the uterus, threatening premature birth, uterine fibroids, placenta previa and low location, somatic pathology of the pregnant woman, etc.), corrective exercises are recommended. The transverse and oblique positions of the fetus are an absolute indication for a caesarean section, it is dangerous to give birth naturally in these cases.
Complications
Breech presentations have higher perinatal morbidity and mortality than cephalic presentations. This is due to a number of reasons: prematurity, hypoxia, birth trauma, damage to the abdominal cavity and spinal cord, abnormalities in the development of the fetus, etc. Perinatal losses in breech presentation with various methods of delivery are 3–5 times higher than with cephalic presentation.
Childbirth with abnormal fetal positions is accompanied by a number of life-threatening complications for the mother and fetus: early outflow of water, prolapse of small parts of the fetus, rupture of the uterus, bleeding from the genital tract with abnormalities in the location of the placenta.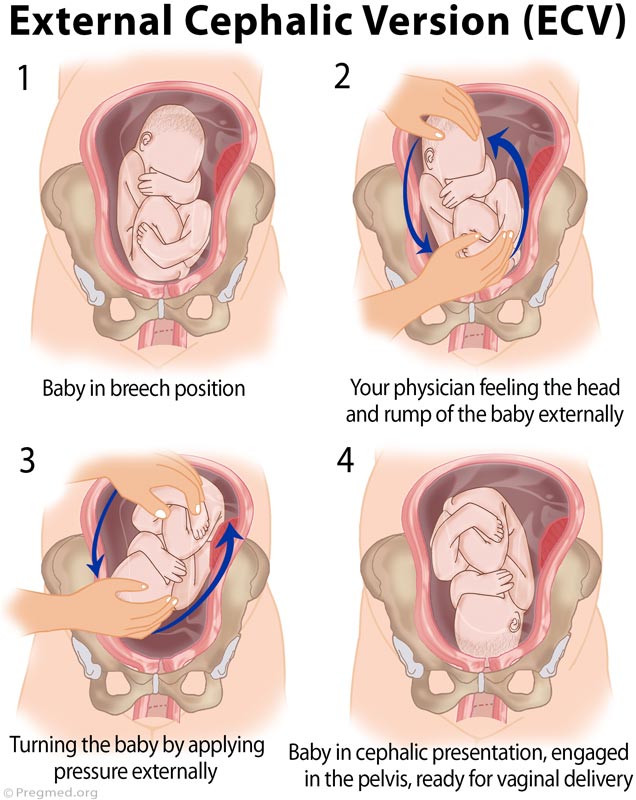
With an unstable or transverse position of the fetus, perinatal mortality reaches 24%.
Prolapse of the umbilical cord loops occurs 20 times more often than in the longitudinal position and head presentation of the fetus. Maternal mortality associated with ascending infection with premature outflow of water, bleeding with an abnormal location of the placenta, complications of surgical aids and uterine rupture, reaches 10%.
Prevention of abnormal fetal position
Currently, there are no effective methods to prevent fetal malposition.
Sources:
- Clinical guidelines "breech presentation of the fetus". Developed by: Russian Society of Obstetricians and Gynecologists. – 2020.
- Pathological childbirth (narrow pelvis, incorrect position of the fetus, anomalies of the contractile activity of the uterus): textbook / O.E. Baryaeva, V.V. Florensov, M.Yu. Akhmetov. FGBOU VO IGMU of the Ministry of Health of Russia, Department of Obstetrics and Gynecology with a course in gynecology of children and adolescents.
 - Irkutsk: IGMU. – 2020. – 88 from
- Irkutsk: IGMU. – 2020. – 88 from
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
-
Pulmonary embolism (PE, pulmonary thromboembolism)
1063 November 23
-
Epidermophytosis
377 November 22
-
Liver dystrophy
5994 November 18th
Show more
Diabetes mellitus
Pregnancy
Edema
Hypertension
Proteinuria
Convulsions
Eclampsia
Preeclampsia
Preeclampsia
Preeclampsia: causes, symptoms, diagnosis and treatment.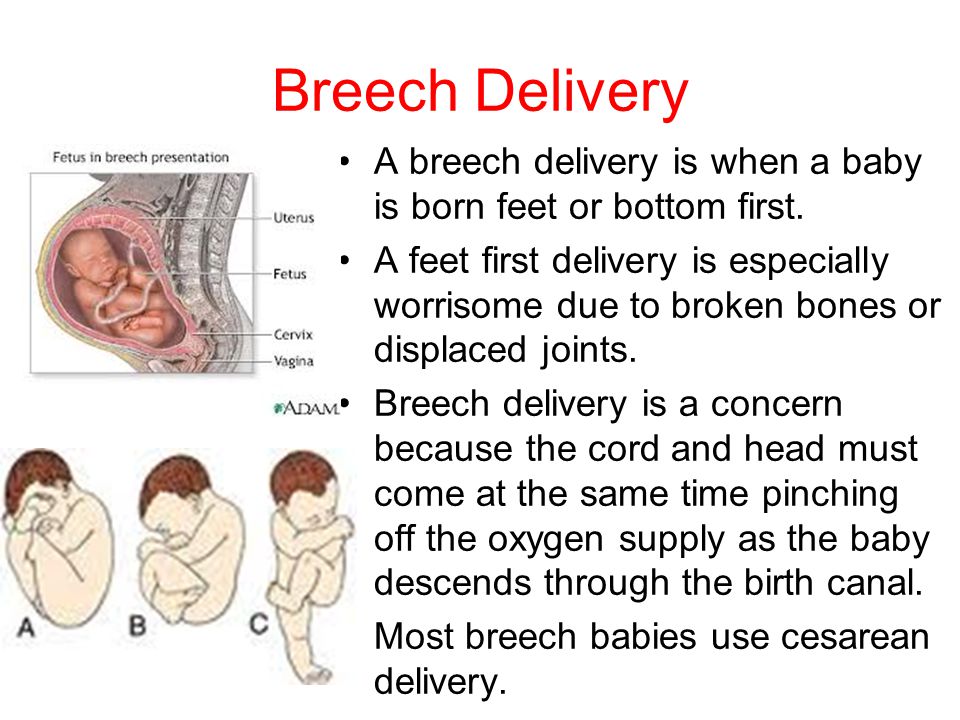
More
Arthritis
Encephalitis
Pregnancy
Rash
Meningitis
Lymphadenopathy
Rubella (German measles, Rubella, Measles)
Rubella: causes, symptoms, diagnosis and treatment.
More
Vomiting
Nausea
Preeclampsia
Pregnancy
Dehydration
Dehydration
Toxicosis of pregnancy
Toxicosis of pregnancy is considered a complication of pregnancy and manifests itself mainly in its first half.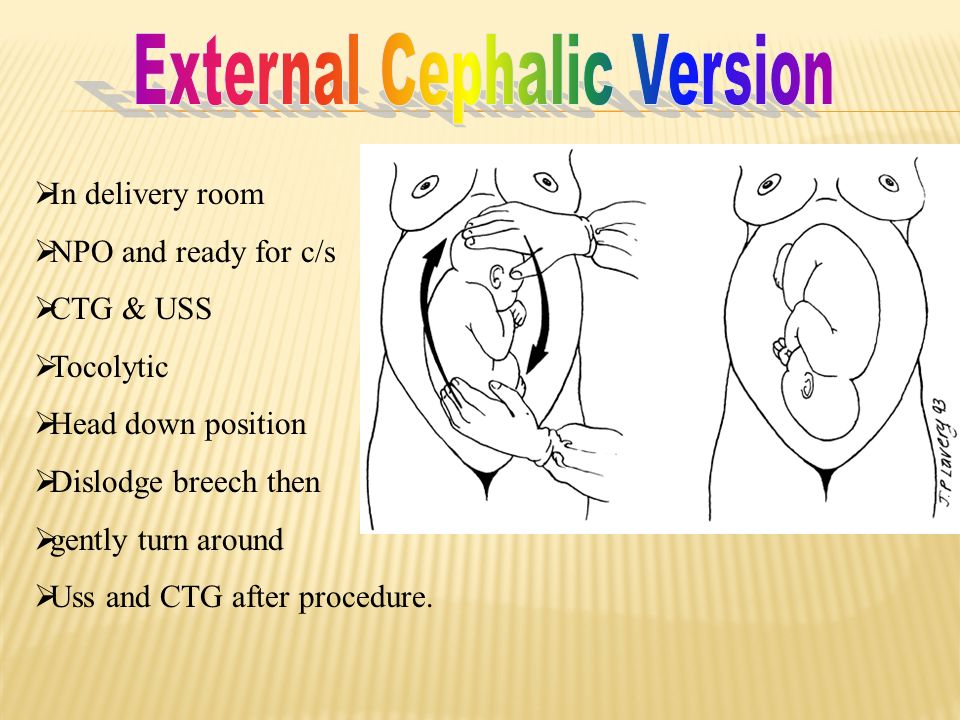
More
ECO
Thrombophilia
Pregnancy
Thrombosis: extended panel 114GP
Thrombosis, extended panel: indications for prescribing, rules for preparing for the analysis, interpretation of the results and norm indicators.
More
ECO
Miscarriage
Pregnancy
hCG, Human Chorionic Gonadotropin
Human Chorionic Gonadotropin (hCG, β-hCG, beta-hCG, Human Chorionic Gonadotropin): indications for prescription, rules for preparing for the test, interpretation of the results and normal indicators.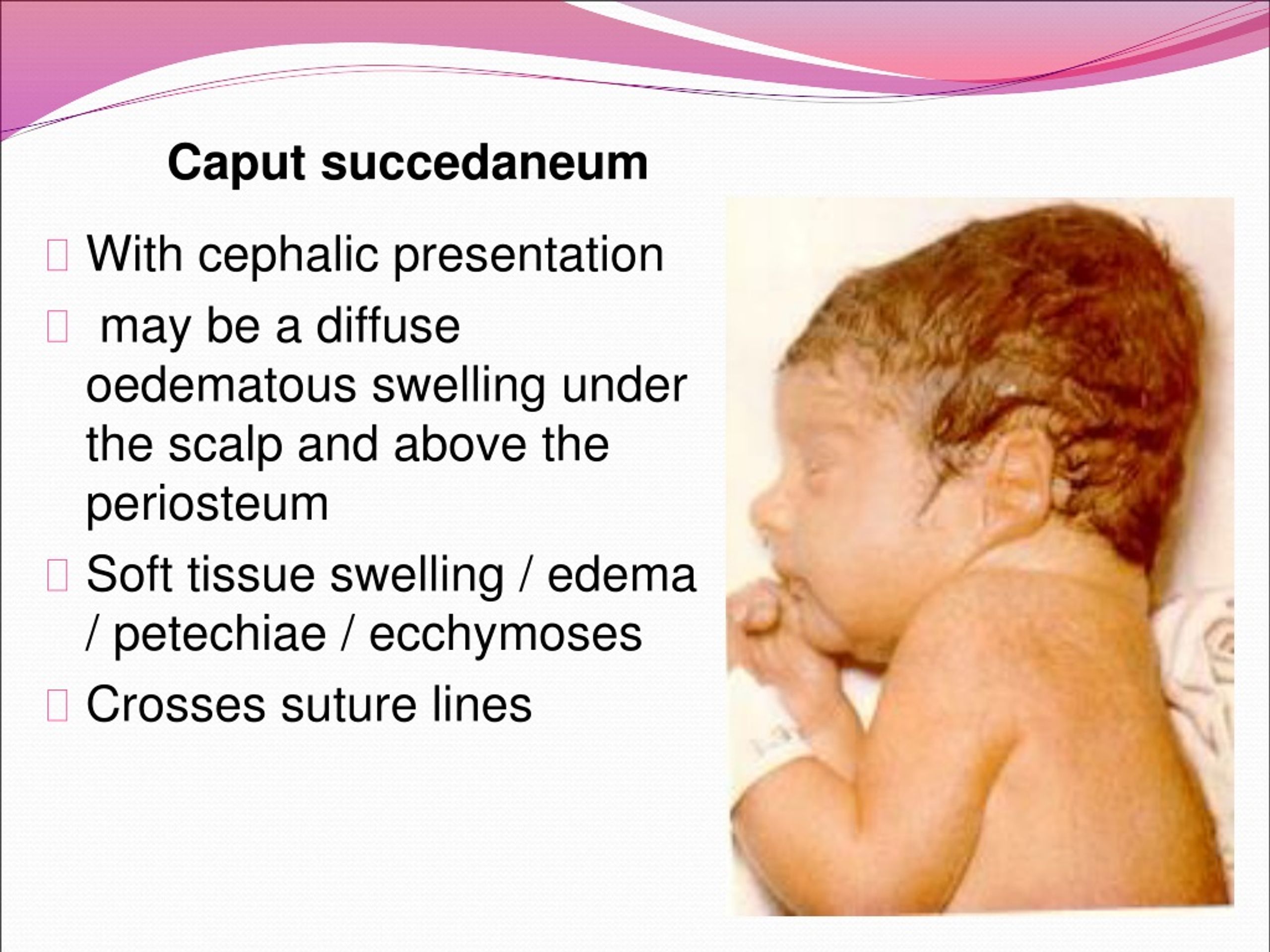
More
Nothing found
Try changing your query or select a doctor or service from the list.
Doctor not found
Try changing your query or select doctor from the list
Medical office not found
Try changing your request or select medical office from the list
Therapist Traumatologist-orthopedist Endocrinologist Urologist Gynecologist Ultrasound doctor Cardiologist Pediatrician
Nothing found
Try changing query
Thank you!
You have successfully made an appointment
Detailed information has been sent to your e-mail
Subscribe to our newsletters
Enter e-mail
I consent to processing of personal data
Subscribe
Fetal ultrasound, prevention and diagnosis
How the fetus is located in the womb depends on how labor will proceed.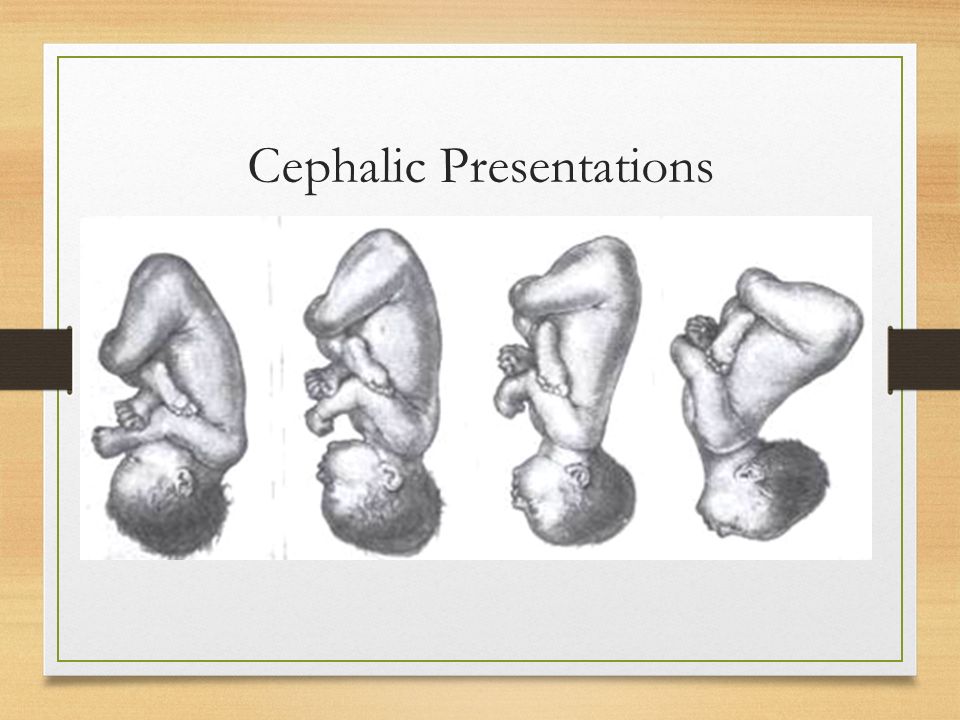 Throughout the entire period of pregnancy, the child not only actively grows, but also often changes the position of its body. The baby is especially mobile in the first two trimesters of pregnancy, then he has less and less space in the mother's uterus and changing his position becomes problematic for him. Fetal presentation is an extremely important factor that will determine how a woman will give birth - naturally or by caesarean section.
Throughout the entire period of pregnancy, the child not only actively grows, but also often changes the position of its body. The baby is especially mobile in the first two trimesters of pregnancy, then he has less and less space in the mother's uterus and changing his position becomes problematic for him. Fetal presentation is an extremely important factor that will determine how a woman will give birth - naturally or by caesarean section.
Information received no earlier than 32 weeks can be considered reliable, until this time the situation may change more than once. In order to find out where the baby's head is located, the gynecologist conducts an examination at each scheduled visit and determines the position of the fetus by palpation. For more accurate results, an ultrasound of the fetus is performed.
Types of fetal presentation
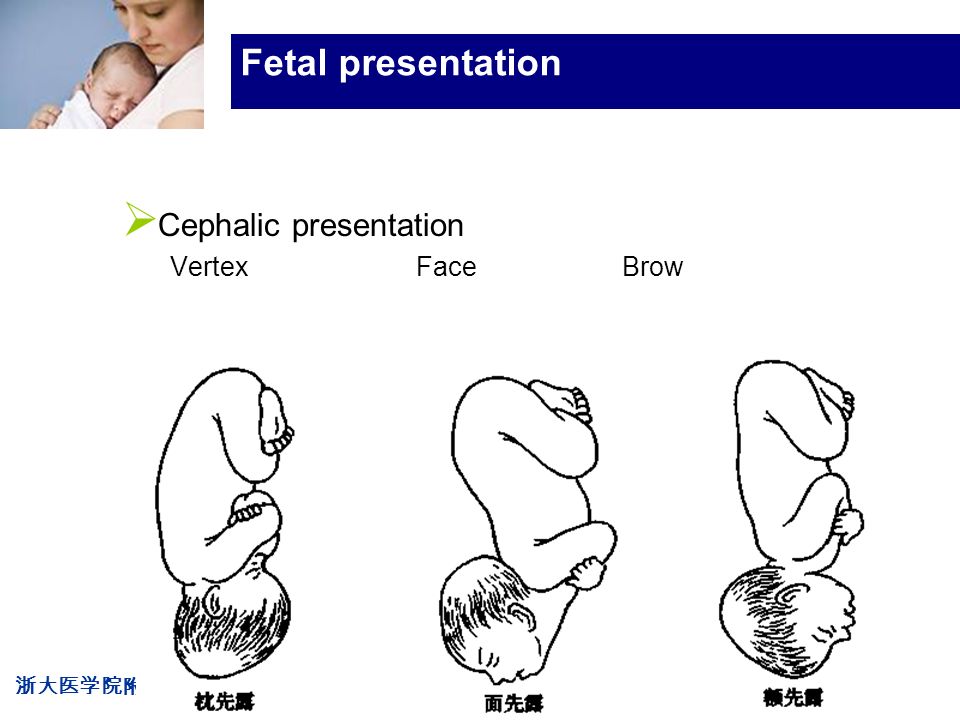
There are the following types of fetal presentation. Head - this is an option in which the head of the fetus is directed downward, that is, towards the entrance of the small pelvis. Depending on which part of the head is facing forward, this type of presentation is divided into several groups:
Depending on which part of the head is facing forward, this type of presentation is divided into several groups:
- Back of the head forward. In this case, this part of the head appears first - this option is considered the most successful, both for the mother and for the baby.
- Frontal - the baby will be born forehead forward.
- Facial - this option involves the appearance of the child with the back of the head back.
Pelvic position - at the entrance to the small pelvis is the lower part of the baby's body:
- Buttocks forward. The child is located in the uterus in such a way that its legs are approximately at the same level with the head, they are extended along the body, and the buttocks are directed to the base of the uterus.
- Foot presentation is a variant in which one or two of the child's legs are directed towards the entrance to the small pelvis.
- A mixed position is the case when both the legs and buttocks of the fetus are at the base of the uterus.
Head presentation is considered the best option for both mother and fetus. In this position, it will be easier for the child to pass through the birth canal, and it is easier for the woman to give birth. In addition, it is the safest option for natural childbirth.
Fetal pelvic position: possible causes and signs
Such a presentation of the fetus is not considered a pathology, but it is highly undesirable. There are a number of factors that can provoke this phenomenon, the main of which is a decrease in the tone of the uterus or its extreme excitability.
In addition, the reasons for this position of the baby in the womb may be the amount of amniotic fluid (high water or low water). Abnormal changes in the uterus, placenta previa, and some fetal malformations can cause the baby to take the wrong position. The woman herself practically does not feel that the child has taken a breech presentation - this does not cause discomfort or pain.
This fact can only be revealed by a specialist, based on examinations, the most accurate of which is ultrasound.