Causes group b strep
Group B Strep In Pregnancy: Test, Risks & Treatment
Overview
What is group B strep?
Group B strep infection (also GBS or group B Streptococcus) is caused by bacteria typically found in a person's vagina or rectal area. About 25% of pregnant people have GBS, but don't know it because it doesn't cause symptoms. A pregnant person with GBS can pass the bacteria to their baby during vaginal delivery. Infants, older adults or people with a weakened or underdeveloped immune system are more likely to develop complications from group B strep.
Most newborns who get GBS don't become sick. However, the bacteria can cause severe and even life-threatening infections in a small percentage of newborns. Healthcare providers screen for group B strep as part of your routine prenatal care. If you test positive, your provider will treat you with antibiotics.
How do you get group B strep?
GBS bacteria naturally occur in areas of your body like your intestines and genital and urinary tracts. Adults can't get it from person-to-person contact or from sharing food or drinks with an infected person. Experts aren't entirely sure why the bacteria spreads, but they know that it’s potentially harmful in babies and people with weakened immune systems.
When do you get tested for group B strep?
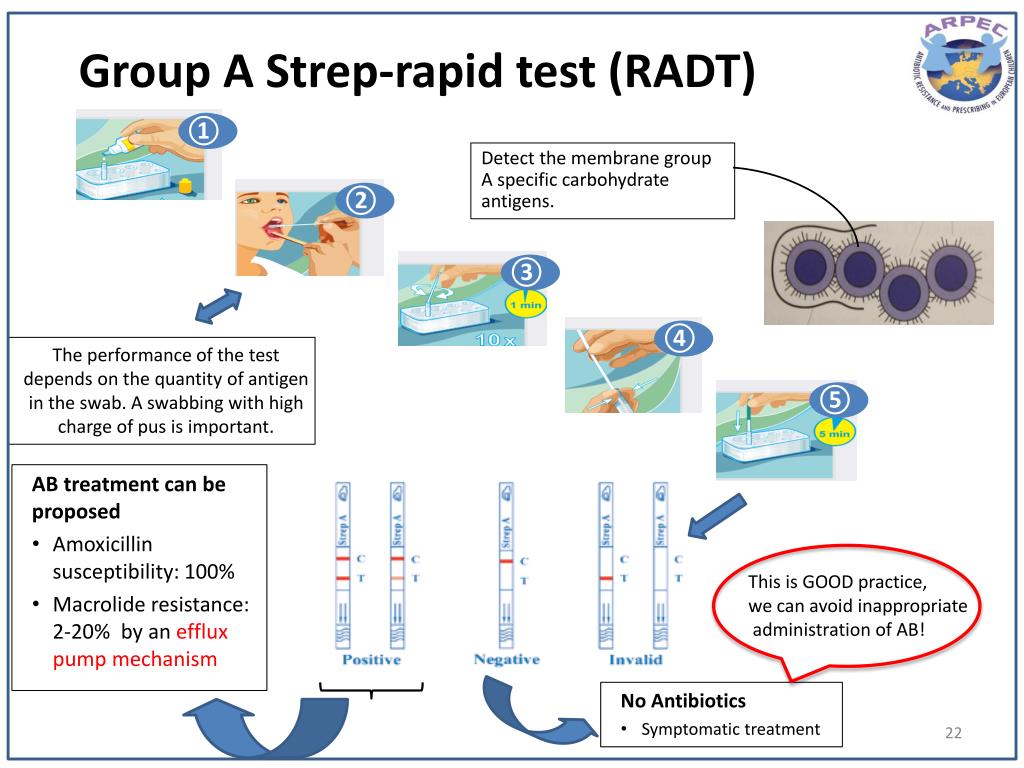
The Centers for Disease Control and Prevention (CDC) recommends routine screening for group B strep in all pregnancies. You're screened for GBS between 36 and 37 weeks of pregnancy. Group B strep testing involves your provider taking a swab of your vagina and rectum and then sending it to a lab for analysis.
Can Group B strep affect a developing fetus?
GBS doesn't affect the fetus baby while it's still inside your uterus. However, your baby can get GBS from you during labor and delivery. Taking antibiotics for GBS reduces your chances of passing it to your baby.
How does a baby get GBS?
There are two main types of Group B strep in babies:
- Early-onset infection: Most (75%) babies with GBS become infected in the first week of life.
 GBS infection is usually apparent within a few hours after birth. Premature babies face greater risk if they become infected, but most babies who get GBS are full-term.
GBS infection is usually apparent within a few hours after birth. Premature babies face greater risk if they become infected, but most babies who get GBS are full-term. - Late-onset infection: GBS infection can also occur in infants one week to three months after birth. Late-onset infection is less common and is less likely to result in a baby's death than early-onset infection.
How common is GBS?
Group B strep screening during pregnancy has decreased the number of cases. According to the CDC, about 930 babies get early-onset GBS, and 1,050 get late-onset GBS. About 4% of babies who develop GBS will die from it.
Symptoms and Causes
What are the symptoms of group B strep?
Most adults don't experience symptoms of group B strep. It can cause symptoms in older people or people with certain medical conditions, but this is rare. These symptoms include:
- Fever, chills and fatigue.
- Difficulty breathing.
- Chest pains.
- Muscle stiffness.
Newborns with GBS have symptoms like:
- Fever.
- Difficulty feeding.
- Irritability.
- Breathing difficulties.
- Lack of energy.
These symptoms can become serious quickly because newborns lack immunity. Group B strep infection can lead to severe problems like sepsis, pneumonia and meningitis in infants.
Can I pass group B strep to my partner?
Other people that live with you, including other children, aren't at risk of getting sick.
Diagnosis and Tests
Will I be tested for group B strep?
Yes, your healthcare provider will test you for GBS late in your pregnancy, around weeks 36 to 37.
Your obstetrician uses a cotton swab to obtain samples of cells from your vagina and rectum. This test doesn't hurt and takes less than a minute. Then, the sample is sent to a lab where it's analyzed for group B strep. Most people receive their results within 48 hours. A positive culture result means you're a GBS carrier, but it doesn't mean that you or your baby will become sick.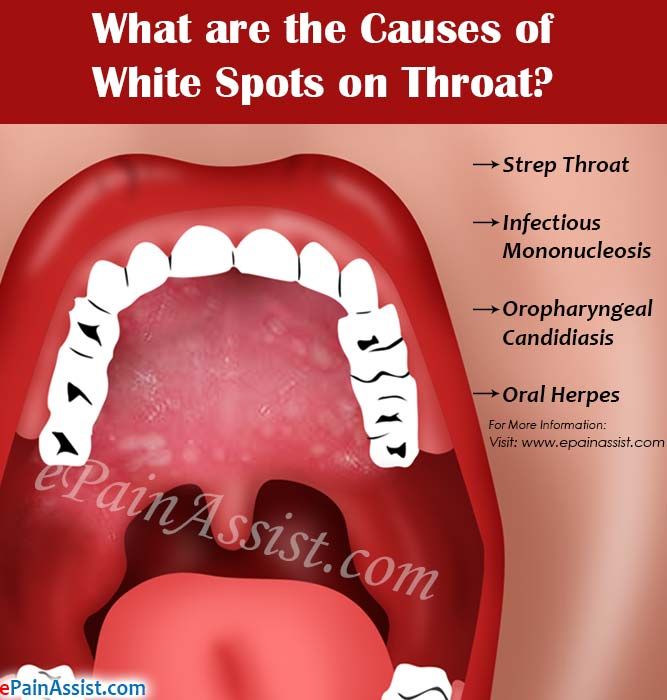
If you’re using a midwife, you might be given instructions on how to test yourself at home and submit the swab to a lab.
Is Group B strep an STI?
No, group B strep isn't an STI (sexually transmitted infection). The type of bacteria that causes GBS naturally lives in your vagina or rectum. It doesn't cause symptoms for most people.
Management and Treatment
What happens if you test positive for group B strep during pregnancy?
Healthcare providers prevent GBS infection in your baby by treating you with intravenous (IV) antibiotics during labor and delivery. The most common antibiotic to treat group B strep is penicillin or ampicillin. Giving you an antibiotic at this time helps prevent the spread of GBS from you to your newborn. It's not effective to treat GBS earlier than at delivery. The antibiotics work best when given at least four hours before delivery. About 90% of infections are prevented with this type of treatment.
One exception to the timing of treatment is when GBS is detected in urine.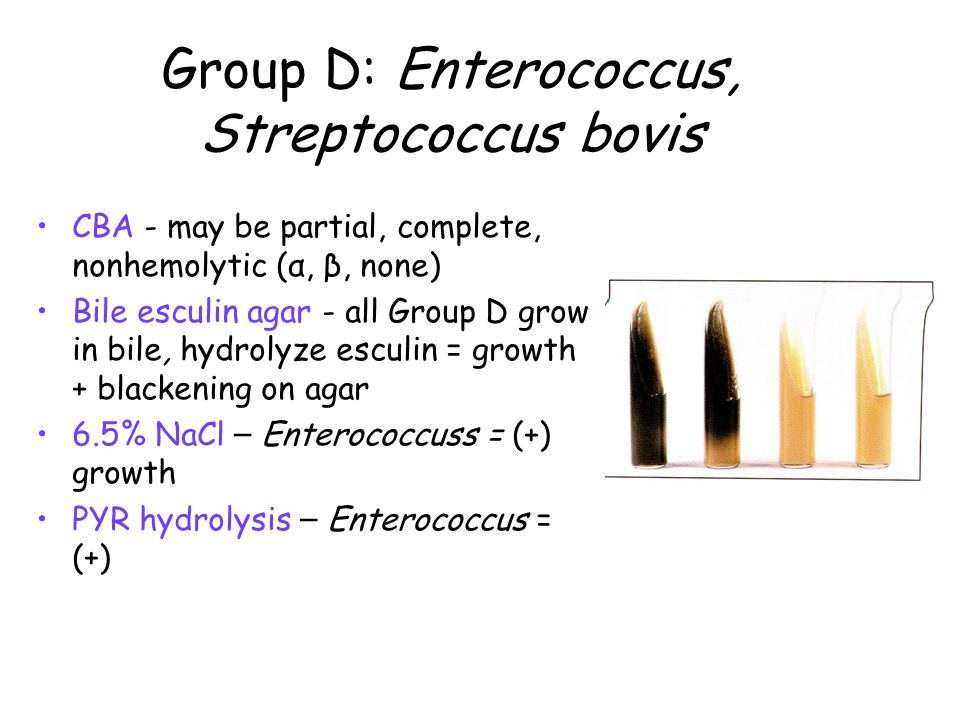 When this is the case, oral antibiotic treatment begins when GBS is identified (regardless of the stage of pregnancy). Antibiotics should still be given through an IV during labor.
When this is the case, oral antibiotic treatment begins when GBS is identified (regardless of the stage of pregnancy). Antibiotics should still be given through an IV during labor.
Any pregnant person who has previously given birth to a baby who developed a GBS infection or who has had a urinary tract infection in this pregnancy caused by GBS will also be treated during labor.
How is group B strep treated in newborns?
Some babies still get GBS infections despite testing and antibiotic treatment during labor. Healthcare providers might take a sample of the baby's blood or spinal fluid to see if the baby has GBS infection. If your baby has GBS, they're treated with antibiotics through an IV.
Prevention
How can I reduce my risk of group B strep?
Anyone can get GBS. Some people are at higher risk due to certain medical conditions or age. The following factors increase your risk for having a baby born with group B strep:
- You tested positive for GBS.
- You develop a fever during labor.
- More than 18 hours pass between your water breaking and your baby being born.
- You have medical conditions like diabetes, heart disease or cancer.
Getting screened for GBS and taking antibiotics (if you're positive) is the best way to protect your baby from infection.
Outlook / Prognosis
What are long term problems of Group B strep in newborns?
Infants with GBS can develop meningitis, pneumonia or sepsis. These illnesses can be life-threatening. Most infants don't develop any long-term issues; however, about 25% of babies with meningitis caused by GBS develop cerebral palsy, hearing problems, learning disabilities or seizures.
Can I get tested for group B strep again?
No, once you test positive for GBS, you're considered positive for the rest of your pregnancy. You will not get re-tested.
Do I need treated for group B strep if I am having a c-section?
No, you don't need antibiotics if you're having a c-section delivery.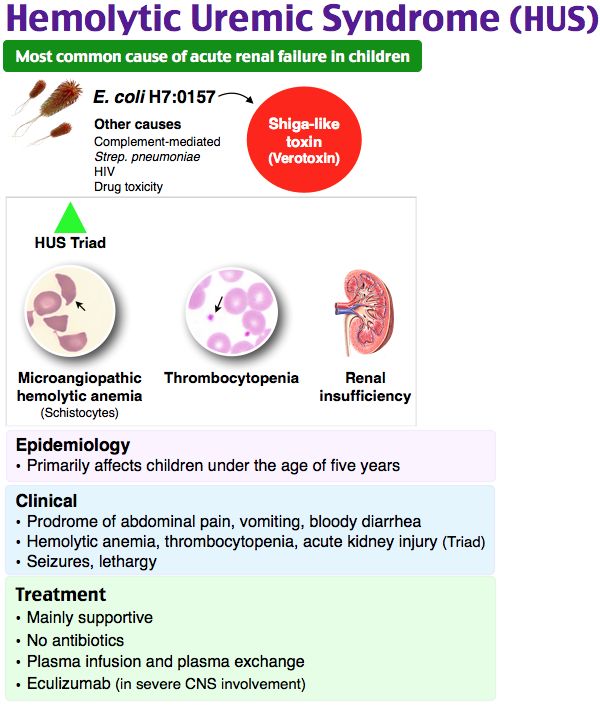 However, you'll still be tested for GBS because labor could start before your scheduled c-section. If your water breaks and you're GBS positive, your baby is at risk of contracting the disease.
However, you'll still be tested for GBS because labor could start before your scheduled c-section. If your water breaks and you're GBS positive, your baby is at risk of contracting the disease.
Living With
When should I see my healthcare provider if I’m positive for group B strep?
In some cases, GBS causes infections during pregnancy. Symptoms of infection include fever, pain and increased heart rate. Let your provider know if you have any of those symptoms as it could lead to preterm labor.
GBS can also cause urinary tract infection (UTI), which requires oral antibiotics.
Talk to your provider about what you can expect during labor and delivery if you have group B strep.
A note from Cleveland Clinic
Try not to panic if your healthcare provider tells you you're positive for group B strep during pregnancy. It's caused by bacteria that occur naturally in your body, not by anything you did wrong. The chances of you passing group B strep to your baby are quite low, especially if you take antibiotics during labor.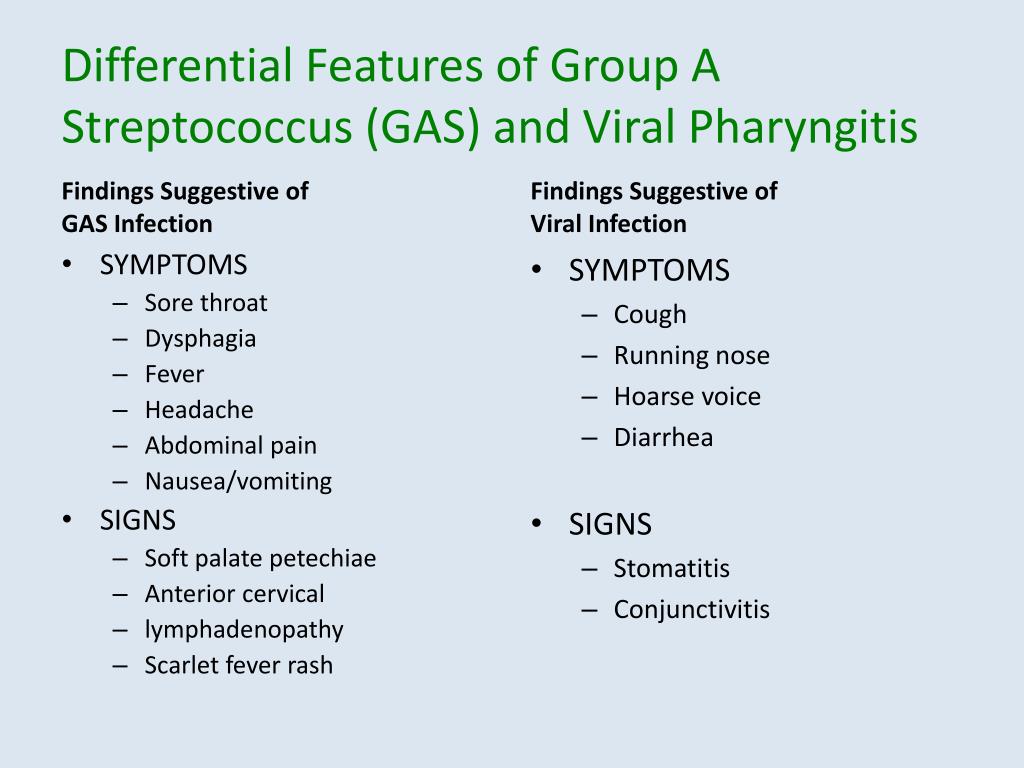 Talk to your provider about group B strep and share any concerns you have. In most cases, testing positive for GBS causes no problems, and your baby is healthy.
Talk to your provider about group B strep and share any concerns you have. In most cases, testing positive for GBS causes no problems, and your baby is healthy.
Group B strep disease - Symptoms and causes
Overview
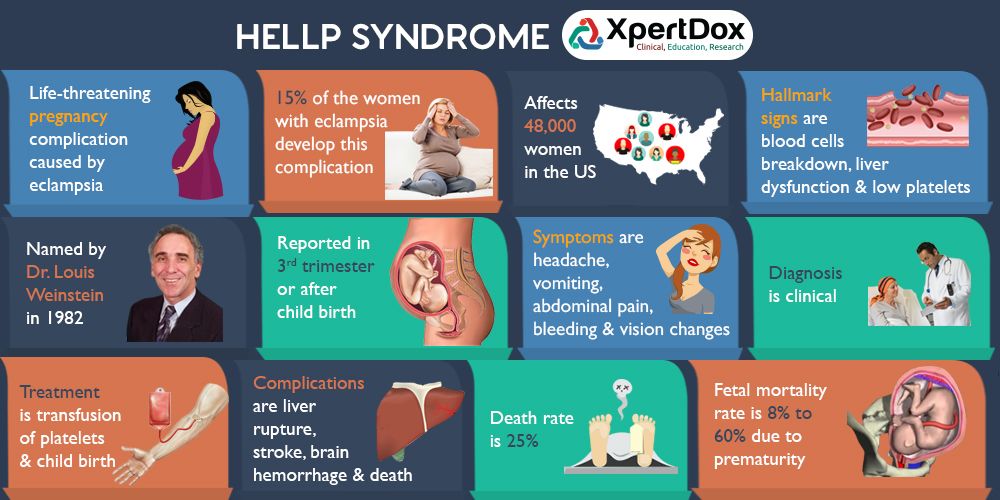
Group B strep (streptococcus) is a common bacterium often carried in the intestines or lower genital tract. The bacterium is usually harmless in healthy adults. In newborns, however, it can cause a serious illness known as group B strep disease.
Group B strep can also cause dangerous infections in adults with certain chronic medical conditions, such as diabetes or liver disease. Older adults are at increased risk of illness due to group B strep, too.
If you're a healthy adult, there's nothing you need to do about group B strep. If you're pregnant, get a group B strep screening test during your third trimester. If you have group B strep, antibiotic treatment during labor can protect your baby.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Infants
Most babies born to women carrying group B strep are healthy. But the few who are infected by group B strep during labor can become critically ill.
But the few who are infected by group B strep during labor can become critically ill.
In infants, illness caused by group B strep can be within six hours of birth (early onset) — or weeks or months after birth (late onset).
Signs and symptoms might include:
- Fever
- Low body temperature
- Difficulty feeding
- Sluggishness, limpness or weak muscle tone
- Difficulty breathing
- Irritability
- Jitteriness
- Seizures
- Rash
- Jaundice
Adults
Many adults carry group B strep in their bodies — usually in the bowel, vagina, rectum, bladder or throat — and have no signs or symptoms.
In some cases, however, group B strep can cause a urinary tract infection or other more-serious infections. Signs and symptoms of infections that may be caused by group B strep include the following.
Urinary tract infection
- A strong, persistent urge to urinate
- A burning sensation or pain when urinating
- Passing frequent, small amounts of urine
- Urine that appears red, bright pink or cola colored — a sign of blood in the urine
- Pelvic pain
Blood infection (bacteremia)
- Fever
- Chills
- Confusion or lack of alertness
Pneumonia
- Fever
- Chills
- Cough
- Shortness of breath
- Chest pain when you breathe or cough
Skin or soft-tissue infection
- Swelling, warmth or redness in the area of the infection
- Pain in the area of the infection
- Lesions with pus or drainage
Bone or joint infection
- Fever
- Chills
- Swelling, warmth or redness over the area of the infection
- Pain in the area of the infection
- Stiffness or inability to use a limb or joint
When to see a doctor
If you have signs or symptoms of group B strep infection — particularly if you're pregnant, you have a chronic medical condition or you're older than 65 — contact your doctor right away.
If you notice your infant has signs or symptoms of group B strep disease, contact your baby's doctor immediately.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices.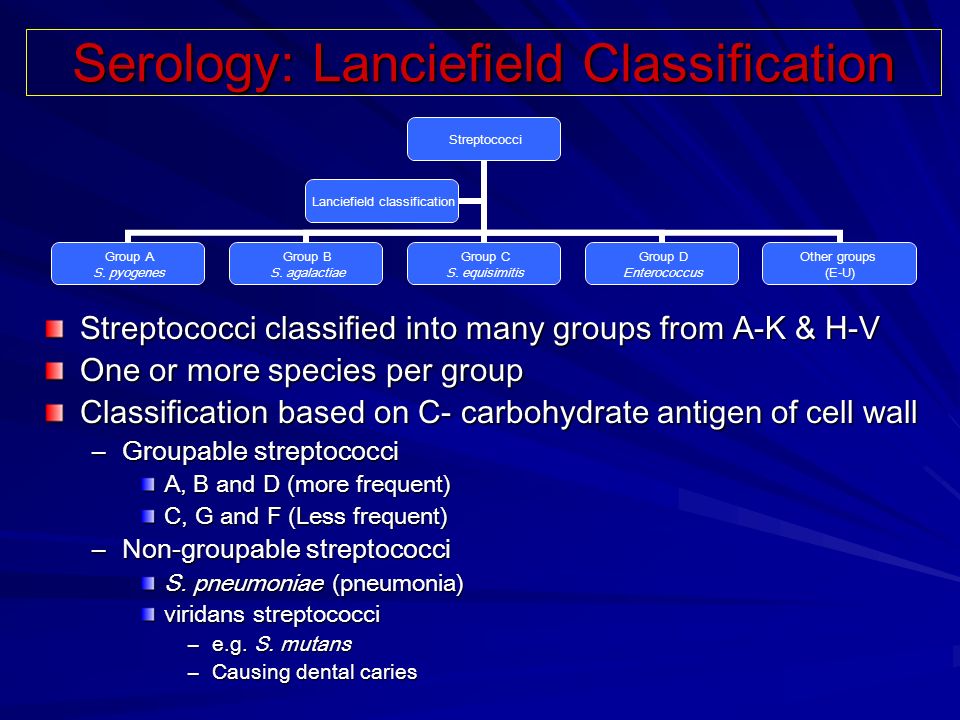 You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Many healthy people carry group B strep bacteria in their bodies. You might carry the bacteria in your body for a short time — it can come and go — or you might always have it. Group B strep bacteria aren't sexually transmitted, and they're not spread through food or water. How the bacteria are spread to anyone other than newborns isn't known.
Group B strep can spread to a baby during a vaginal delivery if the baby is exposed to — or swallows — fluids containing group B strep.
Risk factors
Infants
An infant is at increased risk of developing group B strep disease if:
- The mother carries group B strep in her body
- The baby is born prematurely (earlier than 37 weeks)
- The mother's water breaks 18 hours or more before delivery
- The mother has an infection of the placental tissues and amniotic fluid (chorioamnionitis)
- The mother has a urinary tract infection during the pregnancy
- The mother's temperature is greater than 100.
 4 F (38 C) during labor
4 F (38 C) during labor - The mother previously delivered an infant with group B strep disease
Adults
Adults age 65 and older are at increased risk of group B strep. You're also at increased risk of if you have a condition that impairs your immune system or other serious diseases, including the following:
- Diabetes
- HIV infection
- Liver disease
- Heart disease
- Cancer or history of cancer
Complications
Group B strep infection can lead to life-threatening disease in infants, including:
- Pneumonia
- Inflammation of the membranes and fluid surrounding the brain and spinal cord (meningitis)
- Infection in the bloodstream (bacteremia)
If you're pregnant, group B strep can cause the following:
- Urinary tract infection
- Infection of the placenta and amniotic fluid (chorioamnionitis)
- Infection of the membrane lining the uterus (endometritis)
- Bacteremia
If you're an older adult or you have a chronic health condition, group B strep bacteria can lead to any of the following conditions:
- Skin infection
- Bacteremia
- Urinary tract infection
- Pneumonia
- Bone and joint infections
- Infection of the heart valves (endocarditis)
- Meningitis
Prevention
If you're pregnant, the American College of Obstetricians and Gynecologists recommends a group B strep screening during weeks 36 to 37 of pregnancy.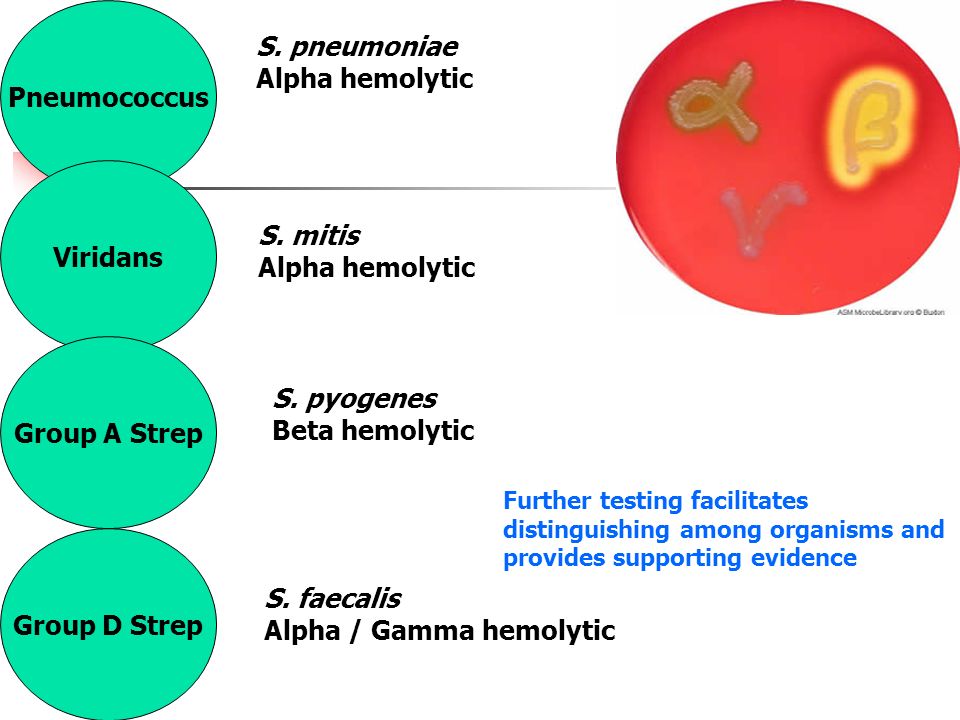 Your doctor will take swab samples from your vagina and rectum and send them to a lab for testing.
Your doctor will take swab samples from your vagina and rectum and send them to a lab for testing.
A positive test indicates that you carry group B strep. It doesn't mean that you're ill or that your baby will be affected, but that you're at increased risk of passing the bacteria to your baby.
To prevent group B bacteria from spreading to your baby during labor or delivery, your doctor can give you an IV antibiotic — usually penicillin or a related drug — when labor begins.
If you're allergic to penicillin or related drugs, you might receive clindamycin or vancomycin as an alternative. Because the effectiveness of these alternatives is not well understood, your baby will be monitored for up to 48 hours.
Taking oral antibiotics ahead of time won't help because the bacteria can return before labor begins.
Antibiotic treatment during labor is also recommended if you:
- Have a urinary tract infection
- Delivered a previous baby with group B strep disease
- Develop a fever during labor
- Haven't delivered your baby within 18 hours of your water breaking
- Go into labor before 37 weeks and haven't been tested for group B strep
Vaccine in development
Although it's not available yet, researchers are working on a group B strep vaccine that could help prevent group B strep infections in the future.
By Mayo Clinic Staff
Related
Products & Services
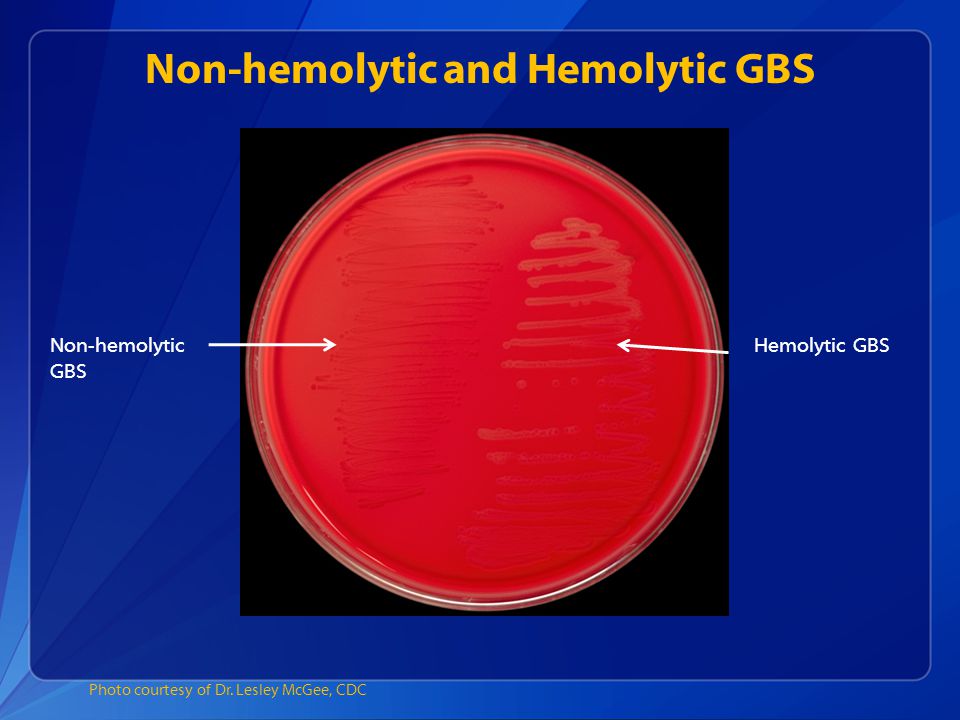
Blood test for streptococcus in the laboratory
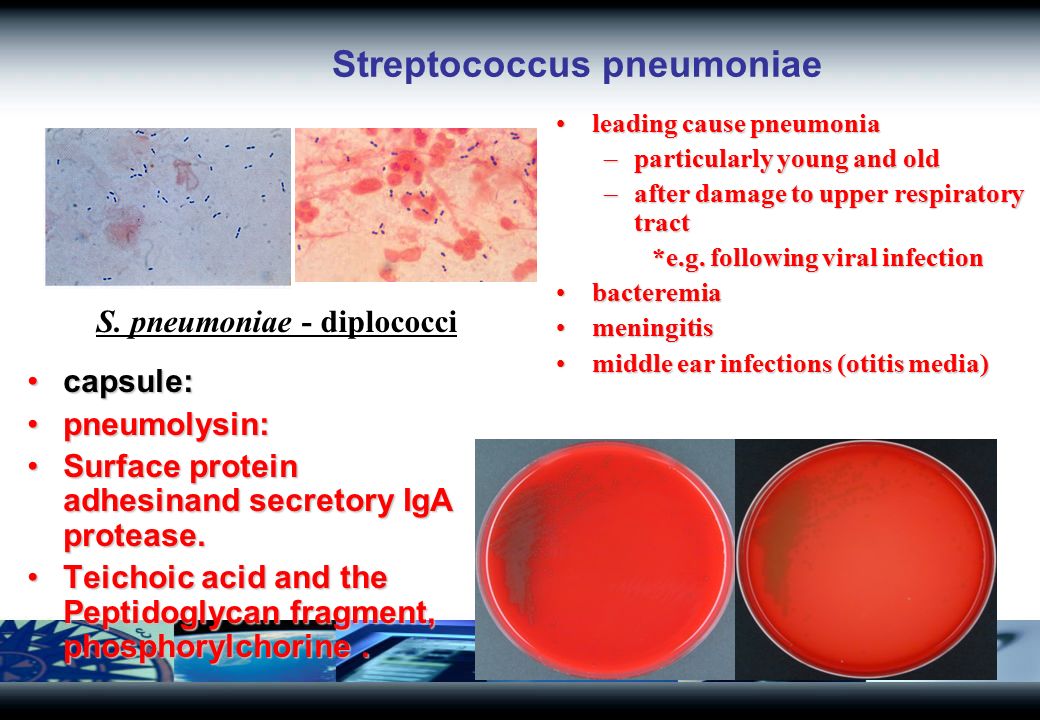
Serogroup B streptococci (GBS) have long been known to cause mastitis in cattle and small cattle and have been named Streptococcus agalactiae . Previously, until 1937 inclusive, this microorganism was considered as a commensal of the human body. Since the 60s, this species, as a human pathogen, has occasionally begun to be isolated in a variety of nosological forms of infection: endocarditis, pyelonephritis, meningitis, pneumonia, abscess, peritonitis, generic sepsis, neonatal sepsis, pharyngitis, etc. Within 1970s–1980s GBS is becoming one of the most common causative agents of purulent-septic infections in newborns and mothers in the United States and Western Europe. In the early 90s, the first publications about the role of this type of streptococcus in the pathology of pregnancy and pyoinflammatory diseases of newborns also appeared in our country.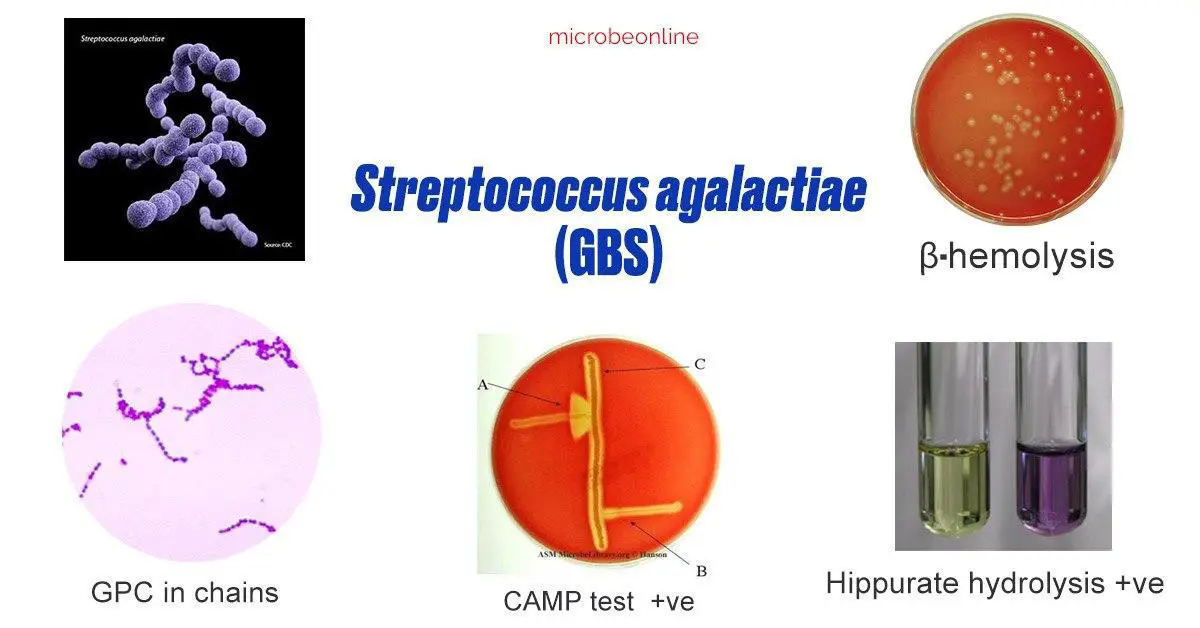 To date, official registration of diseases caused by this microorganism in the Russian Federation has not been carried out.
To date, official registration of diseases caused by this microorganism in the Russian Federation has not been carried out.
Streptococci of this species, according to the modern nomenclature according to the Bergay determinant, are included in the genus Streptococcus family Sreptococcaeae species S.agalactiae . The modern classification of streptococci is based on the division into serological groups according to the Lensfield classification. S.agalactiae are assigned to serogroup B and are its only representatives. GBS is a heterogeneous population consisting of a number of serotypes and their combinations. Currently, 9 serotypes have been identified, designated by Roman numerals: I, II, III, IV, V, VI, VII, VIII. Type I is divided into subtypes Ia and Ib. nine0005
The habitat of the pathogen is the human body, large and small cattle, the possibility of its transmission from animals to humans and vice versa has not been proven.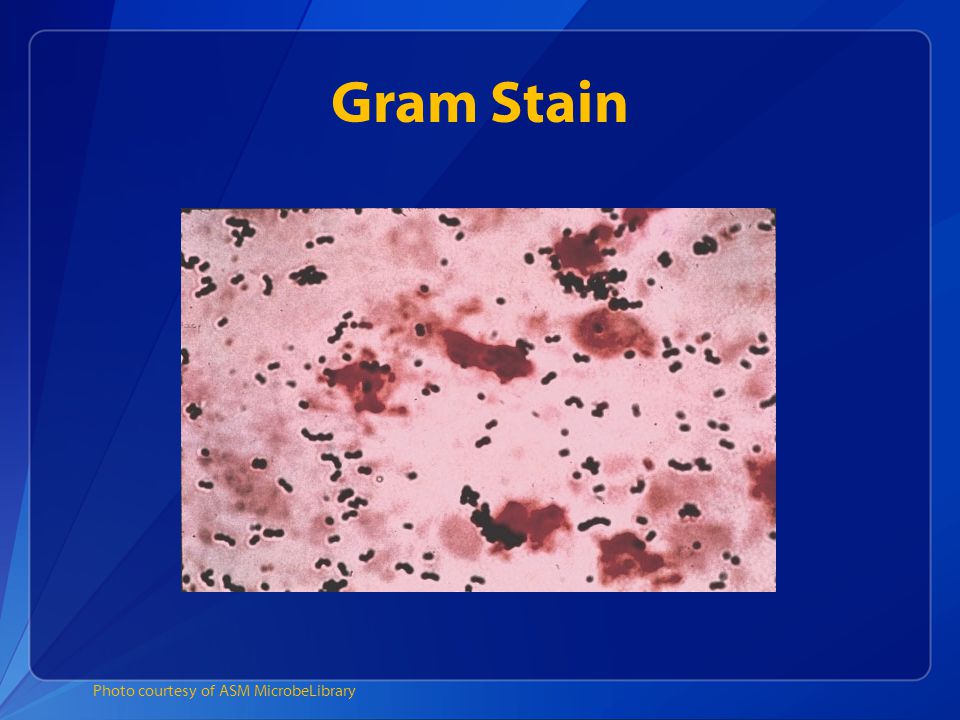 The localization of GBS in humans is the gastrointestinal tract (colon), vagina, urethra, sometimes the microorganism can colonize the pharynx. Pathogenicity factors: the ability to adhere and invade, resistance to phagocytosis, hemolysin, hyaluronidase, peptidase (impairs the chemotaxis of polymorphonuclear leukocytes to the site of GBS infection).
The localization of GBS in humans is the gastrointestinal tract (colon), vagina, urethra, sometimes the microorganism can colonize the pharynx. Pathogenicity factors: the ability to adhere and invade, resistance to phagocytosis, hemolysin, hyaluronidase, peptidase (impairs the chemotaxis of polymorphonuclear leukocytes to the site of GBS infection).
GBS can cause severe infections in people. The most sensitive to them are newborns, pregnant women, diabetics, chronic patients, children with dystrophy, the elderly, people with reduced immunity. Spontaneous abortions, preterm labor, chorioamnionitis, pyelonephritis, urinary tract infections, endocarditis, sepsis, as well as complications after caesarean section, meningitis, mastitis and endometritis in puerperas can be associated with GBS. In neonates, GBS mainly causes sepsis, meningitis, and pneumonia. Transmission of the pathogen to the newborn can occur intranatally and postnatally. According to foreign sources, in recent years there has been a relative increase in the number of diseases caused by GBS in the elderly against the background of a slight decrease in the incidence among newborns. The observed phenomenon is associated, on the one hand, with the active prevention of this infection in maternity hospitals, and, on the other hand, with an increase in the number of elderly patients with reduced immunity. In the latter, GBS usually causes infection of the skin and bones, sepsis without a clear source of its origin, urosepsis, pneumonia, and peritonitis. Often these infections occur repeatedly in such patients. nine0005
The observed phenomenon is associated, on the one hand, with the active prevention of this infection in maternity hospitals, and, on the other hand, with an increase in the number of elderly patients with reduced immunity. In the latter, GBS usually causes infection of the skin and bones, sepsis without a clear source of its origin, urosepsis, pneumonia, and peritonitis. Often these infections occur repeatedly in such patients. nine0005
An important role in the development of GBS infections in newborns is played by factors predisposing to the disease, the so-called “risk factors”, which can be conditionally divided into two groups:
- associated with the peculiarities of childbirth or colonization of mothers with GBS;
- directly related to newborns.
The first group includes the presence of GBS on the mucous membrane of the cervix in pregnant women, the massiveness of colonization (isolation of the pathogen simultaneously from several examined loci), cases of GBS infections in children in anamnesis in parturient women, premature birth, a long anhydrous period, fever during childbirth, chorioamnionitis , bacteriuria due to GBS.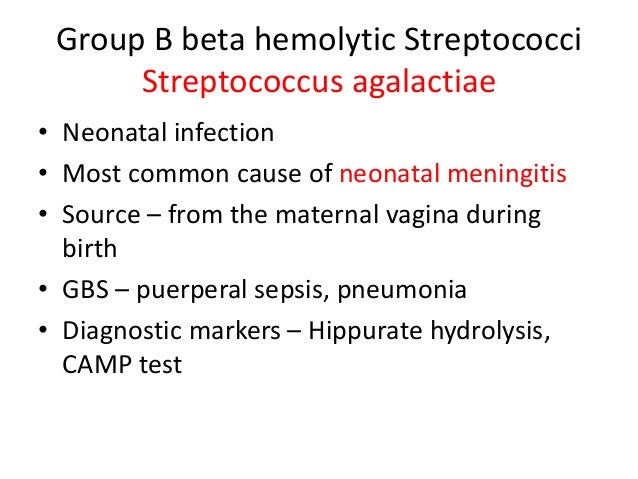 nine0005
nine0005
The second group includes the fact and massive colonization of newborns with GBS, prematurity and low birth weight, birth by caesarean section, intrauterine instrumental examination of the fetus, lasting more than 12 hours.
Penicillin is still the most effective and widely used drug for the treatment of infections caused by streptococci. Along with serogroup A streptococci, GBS retain their sensitivity to this antibiotic, although GBS strains in a small number of cases are resistant to penicillin G. In addition to penicillin, streptococci have been found to be highly sensitive to ampicillin, erythromycin, clindamycin, lincomycin, oxacillin and meroponem. The first three generations of cephalosprins, with the exception of cefoxitin and moxalactam, have a wider spectrum of activity than penicillin. The high sensitivity of GBS to a number of relatively new drugs with a wide spectrum of activity was also noted: thienamycin, mezlocillin, azlocillin and piperacillin. GBS strains have been found to be frequently resistant to aminoglycoses, nalidixic acid, tetracycline, chloramphenicol, bacitracin, trimethoprim, and metromnidazole. Nevertheless, the combined use of aminoglycosides with penicillin or ampicillin in experimental studies on laboratory animals revealed a synergistic effect of such combinations. In recent years, foreign literature reports on the isolation of GBS strains resistant to beta-lactam antibiotics. The nature of this phenomenon is associated with the appearance in the cells of microorganisms of the genes responsible for the synthesis of penicillin-binding proteins (PBPs). According to a number of foreign researchers, the number of GBS strains resistant to erythromycin can range from 5.9up to 32.0% and the number of strains resistant to clindamycin from 6.9 to 14.3%. The use of therapeutic bacteriophages for the prevention and treatment of GBS infection is currently impossible due to the lack of active specific bacteriophages.
GBS strains have been found to be frequently resistant to aminoglycoses, nalidixic acid, tetracycline, chloramphenicol, bacitracin, trimethoprim, and metromnidazole. Nevertheless, the combined use of aminoglycosides with penicillin or ampicillin in experimental studies on laboratory animals revealed a synergistic effect of such combinations. In recent years, foreign literature reports on the isolation of GBS strains resistant to beta-lactam antibiotics. The nature of this phenomenon is associated with the appearance in the cells of microorganisms of the genes responsible for the synthesis of penicillin-binding proteins (PBPs). According to a number of foreign researchers, the number of GBS strains resistant to erythromycin can range from 5.9up to 32.0% and the number of strains resistant to clindamycin from 6.9 to 14.3%. The use of therapeutic bacteriophages for the prevention and treatment of GBS infection is currently impossible due to the lack of active specific bacteriophages.
Indications for examination.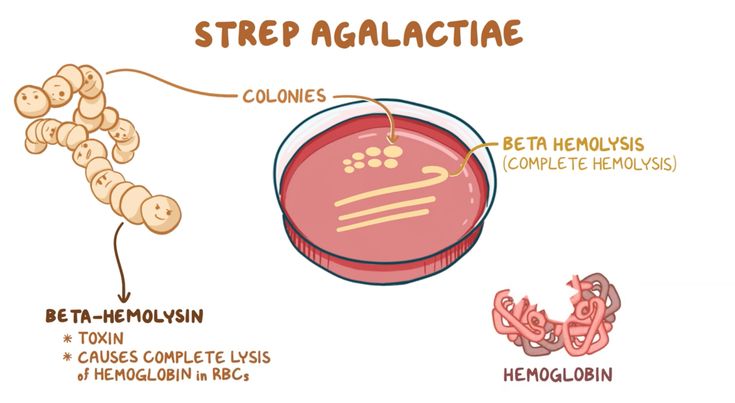 Birth of a child with a history of GBS infection in a woman in labor, GBS bacteriuria during this pregnancy, threatened preterm labor, fever during labor (≥ 38°C), waterless period lasting more than 18 hours. nine0005
Birth of a child with a history of GBS infection in a woman in labor, GBS bacteriuria during this pregnancy, threatened preterm labor, fever during labor (≥ 38°C), waterless period lasting more than 18 hours. nine0005
Material for research. Blood, CSF, sputum, fetal fluid, joint fluid, tissue fragments, oropharyngeal swabs, vaginal swabs/scrapes, rectal swabs.
Etiological diagnosis includes isolation of the pathogen and identification of its DNA.
Comparative characteristics of laboratory diagnostic methods. Isolation of the pathogen in the diagnosis of GBS infections is the "gold standard" and is an important step in a series of diagnostic measures. A standard culture is used using, for example, 5% blood agar. Timely isolation of the pathogen with the determination of sensitivity to antibiotics largely determines the effectiveness of the treatment and prevention of this disease. nine0005
If an infection is suspected, a variety of biological material is examined. In the case of determining the carriage of GBS in pregnant women, smears from the mucous membrane of the vagina and rectum are examined for 35–37 weeks. pregnancy. If it is not possible to inoculate immediately, transport media may be used. The time needed to isolate and identify GBS is usually 4 to 5 days.
In the case of determining the carriage of GBS in pregnant women, smears from the mucous membrane of the vagina and rectum are examined for 35–37 weeks. pregnancy. If it is not possible to inoculate immediately, transport media may be used. The time needed to isolate and identify GBS is usually 4 to 5 days.
Identification of a specific DNA fragment S.agalactiae by PCR is carried out in the study of various biological material. Scrapings of epithelial cells from the side walls of the vagina, perianal smears at 34–36 weeks of gestation are examined to detect colonization of the vagina and/or rectum by S.agalactiae; blood, CSF of a newborn - for the diagnosis of septic conditions; swabs from the oropharynx - in newborns with clinical symptoms of pneumonia to confirm the diagnosis. The advantage of this study is that it allows testing within a few hours and thereby accelerates clinical decision-making on the prevention and treatment of the disease. The diagnostic sensitivity of the study is 81%, the diagnostic specificity is 97.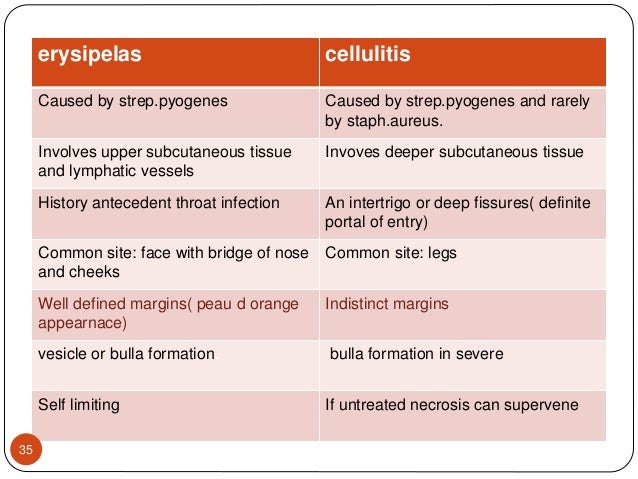 6%. Detection of S.agalactiae DNA by PCR can be performed in a qualitative and quantitative format. The quantitative format of the test allows the study to be used to assess the degree of GBS colonization of a selected locus. However, the detection of a specific DNA fragment S.agalactiae by PCR does not allow the detection of viable microorganisms and, accordingly, their sensitivity to antibiotics.
6%. Detection of S.agalactiae DNA by PCR can be performed in a qualitative and quantitative format. The quantitative format of the test allows the study to be used to assess the degree of GBS colonization of a selected locus. However, the detection of a specific DNA fragment S.agalactiae by PCR does not allow the detection of viable microorganisms and, accordingly, their sensitivity to antibiotics.
Streptococcal infection: Causes of streptococcal infection, Symptoms, Treatment of diseases caused by streptococcal infection
Streptococcal infection is a group of infectious diseases caused by different types of streptococcal flora. The infection affects the upper skin, mainly the skin of the face, hands, neck, as well as the respiratory organs. Streptococcal infection causes diseases such as streptoderma, pneumonia, glomerulonephritis, vasculitis, tonsillitis, rheumatism, erysipelas, scarlet fever, etc.
Attention!
Here you can choose a doctor who treats Streptococcal Infection If you are not sure about the diagnosis, make an appointment with a general practitioner or general practitioner to clarify the diagnosis.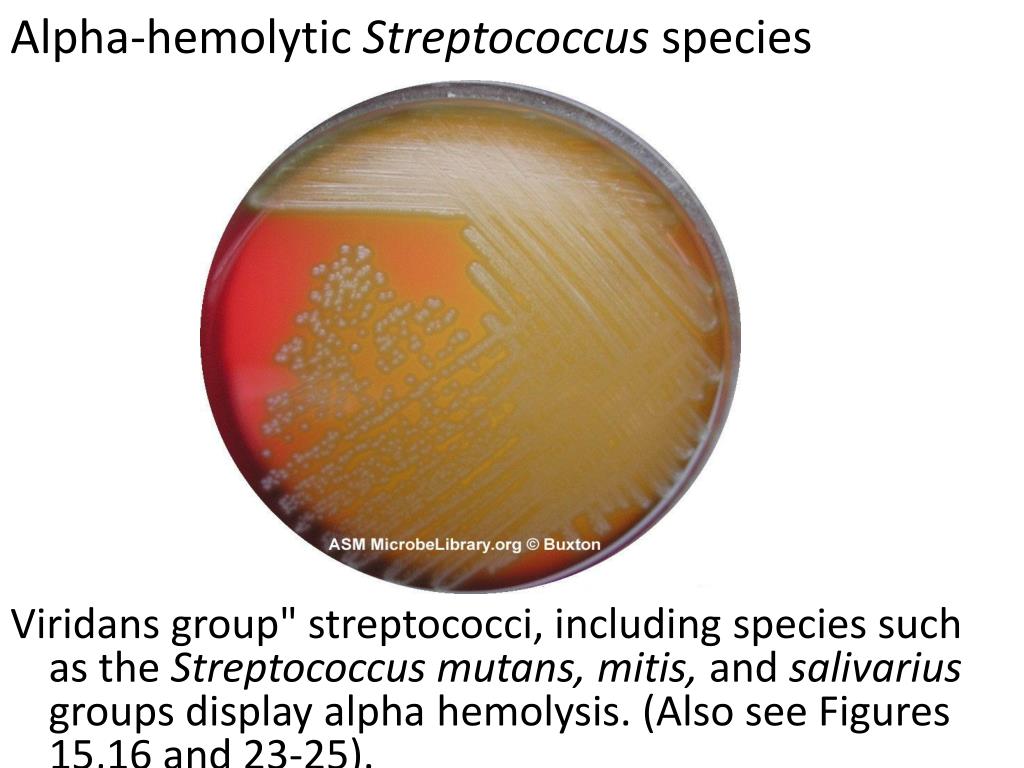 nine0005
nine0005
Causes of streptococcal infection
Symptoms
Diagnostics
Treatment of diseases caused by streptococcal infection
Streptococcus - a genus of bacterial organisms, which is present in the human organism. There are more than 15 subtypes of bacteria, but the most common are: alpha, beta and gamma. With an acceptable value of alpha and gamma, streptococci are part of the normal microflora of the gastrointestinal tract, oral cavity, larynx and respiratory system of a person, they do not carry harm to the body. Beta streptococci are dangerous to human health, and they cause a wide range of human diseases. nine0005
Hemolytic streptococcus (group A) is a common bacterium found in the body. The predominant number of infections develops precisely due to group A streptococcus. In this regard, a person has a high susceptibility to streptococcus and, accordingly, under favorable conditions for the bacterium, it actively multiplies in the human body. Group A bacteria most often cause:
Group A bacteria most often cause:
- angina;
- pharyngitis;
- impetigo; nine0023 face;
- scarlet fever;
- pneumonia;
- glomerulonephritis;
- vasculitis;
- rheumatism;
- bronchitis;
- periodontitis.
Group B streptococcus mainly affects the genitourinary system, because this type of bacteria is found in the urethra in men and in the vagina in women.
Causes of streptococcal infection
A pathogenic bacterium is transmitted in three ways:
- airborne - the spread of infection with saliva and mucus when sneezing, crying, coughing; nine0024
- household contact - direct contact with the carrier of the infection, even if he does not show symptoms of diseases, contact with household items in the house and public places;
- sexual - through unprotected intercourse.
The fastest way to spread streptococcus is by airborne droplets, so children who are in a large group (school, kindergarten, various classes) very often succumb to infection.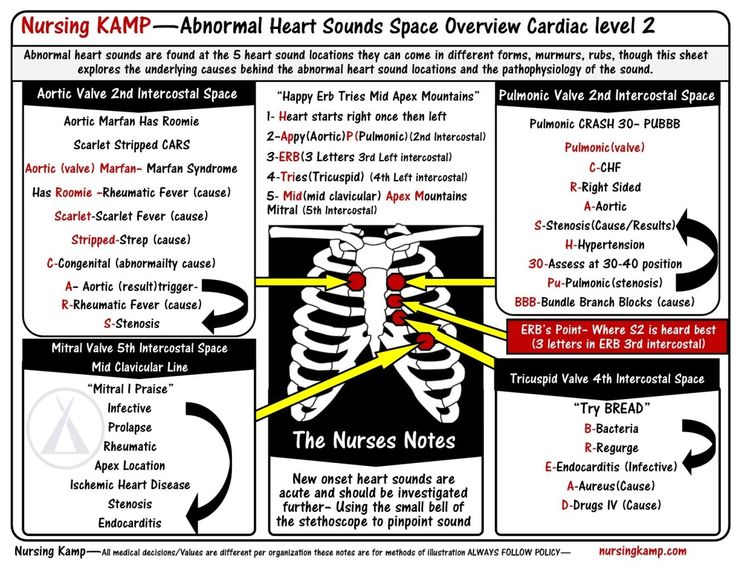
Streptococcal infection in children develops most often in the cold season (late autumn, winter). Due to the fact that children do not always observe hand hygiene, they can become infected in almost any environmental condition. nine0005
Often streptococcal infection occurs in newborns, this is due to the ability of streptococcus to penetrate into tissues and organs. At the time of childbirth, infection can occur through the amniotic fluid. The infection develops in the first few hours of life and leads to pneumonia, sepsis, and meningitis. The mortality rate with this development of infection is more than 50%.
In children aged 2 to 8 years, streptococcus often causes pneumonia as a complication of a previous infection: whooping cough, influenza, measles, chicken pox. Immunocompromised children who have suffered severe hypothermia are also susceptible to this disease. nine0005
Symptoms
In medical practice, in diseases, streptococcal infection is manifested by a variety of symptoms.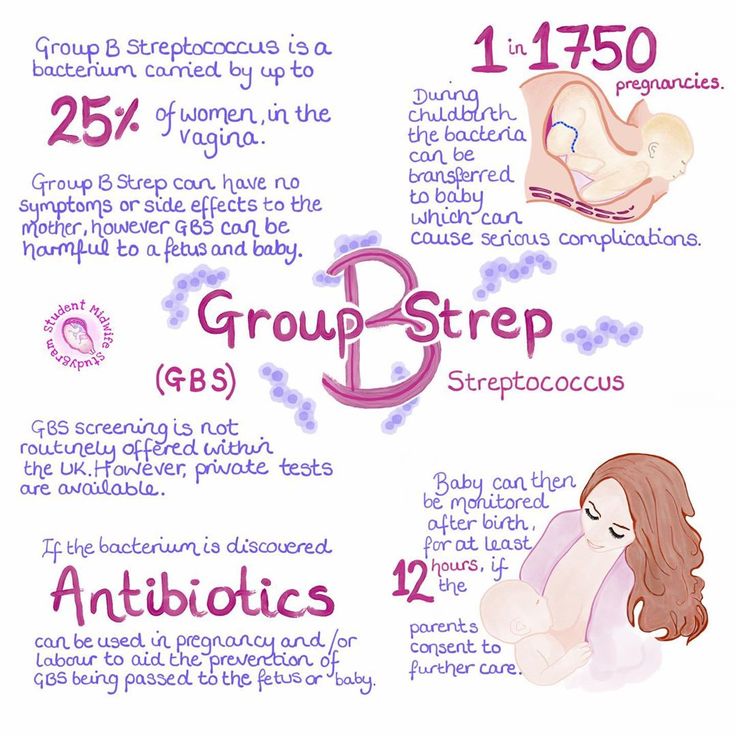 It depends on the specific disease that this type of pathogenic bacterium caused.
It depends on the specific disease that this type of pathogenic bacterium caused.
For the group of diseases of the respiratory tract, these are:
- sore throat;
- temperature increase;
- plaque formation with pus on tonsils;
- swollen lymph nodes.
Streptococcal skin infection is usually accompanied by: inflammatory processes on the skin; nine0005
- itching;
- redness;
- the appearance of vesicles, plaques on the skin;
- fever;
- chills;
- weakness.
Diseases of the genitourinary system caused by hemolytic streptococcus are most often asymptomatic. However, there may also be symptoms similar to those of diseases in this area:
- itching;
- selections;
- soreness in the organs of the genitourinary system. nine0024
Diagnosis
To identify bacteria of the genus streptococcus, a series of studies are carried out that allow you to determine the specific causative agent of the infection, its type and sensitivity to medicines. Traditionally, doctors (whose specialty depends on the affected area or organ) conduct a comprehensive diagnosis:
Traditionally, doctors (whose specialty depends on the affected area or organ) conduct a comprehensive diagnosis:
- bacteriological examination (inoculation of biological material) - a swab from the tonsils, lesions on the skin, sputum examination on the lungs; nine0024
- general analysis of urine, blood;
- microbiological examination for the level of sensitivity to antibiotics;
- examination of the affected organs by a narrow specialist.
Treatment of diseases caused by streptococcal infection
Treatment of streptococcal infection requires an initial correct diagnosis of the underlying disease, its differentiation from similar diseases.
When diagnosing the pathogenic bacterium streptococcus, treatment should be carried out by a narrow specialist depending on the affected organ: pulmonologist, dermatologist, gynecologist, urologist, etc.
Streptococcus on the skin is treated mainly at home under medical supervision.