Are blood clots a sign of miscarriage
Miscarriage | Warning Signs, Myths, Symptoms and Causes
Many women experience some bleeding in early pregnancy. About 1 in 5 recognised pregnancies end in miscarriage. Most are caused by a one-off fault in the genes. Always tell your doctor if you have vaginal bleeding when you are pregnant. Call an ambulance if the bleeding is very heavy or if you have severe tummy (abdominal) pain. Bleeding with pain can also be a sign of an ectopic pregnancy. This is less common than miscarriage but is serious and needs urgent medical care. Losing a pregnancy can be hard for both partners. However, most couples who experience this will go on to have a successful pregnancy next time.
What causes bleeding in early pregnancy?
What is a miscarriage?
Prof Lesley ReganMany women may have a small amount of bleeding (spotting) at the time of their missed period. This is sometimes called an 'implantation bleed'. It happens when the fertilised egg implants itself in the wall of your womb (uterus). It is harmless.
The most common cause of bleeding after the time of the missed period is miscarriage. Miscarriage is the loss of a pregnancy at any time up to the 24th week. A loss after this time is called a stillbirth. At least 8 miscarriages out of 10 actually occur before 13 weeks of pregnancy. These are called early miscarriages. A late miscarriage is one that happens from 13 weeks to 24 weeks of pregnancy.
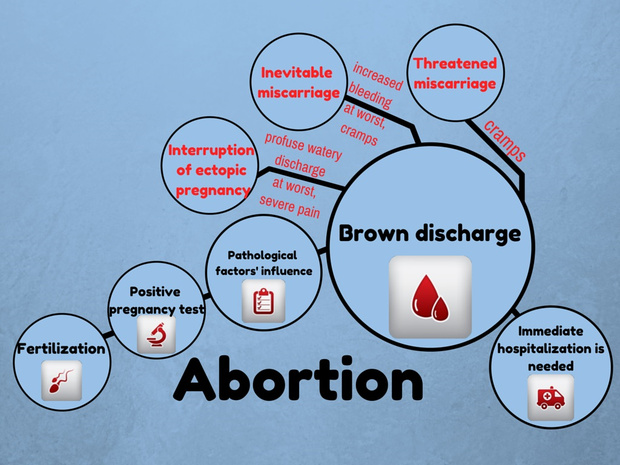
A less common cause of bleeding in pregnancy is an ectopic pregnancy. This is a pregnancy that occurs outside the womb. It occurs in about 1 in 100 pregnancies.
Always tell your doctor if you have vaginal bleeding when you are pregnant
How to support a friend after a miscarriage or stillbirth
If a friend or family member suffers a miscarriage or stillbirth, it's natural to want to offer ...
How common is miscarriage?
Miscarriage accounts for over 40,000 hospital admissions in the UK each year. About 1 in 4 recognised pregnancies end in miscarriage.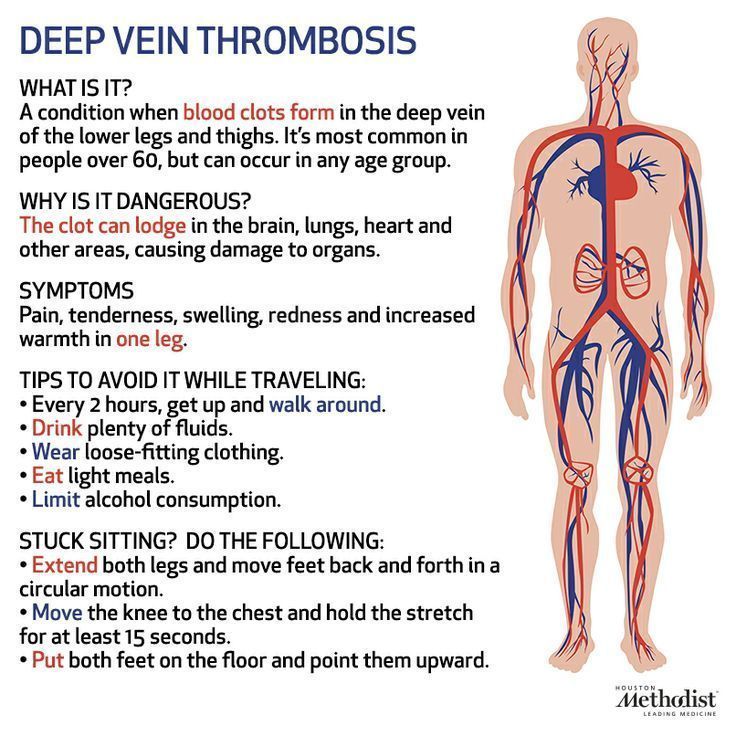 Far more pregnancies than this do not make it - as many as half. This is because in many cases a very early pregnancy ends before you miss a period and before you are even aware that you are pregnant.
Far more pregnancies than this do not make it - as many as half. This is because in many cases a very early pregnancy ends before you miss a period and before you are even aware that you are pregnant.
The vast majority of women who miscarry go on to have a successful pregnancy next time. Recurrent miscarriages (three or more miscarriages in a row) occur in about 1 in 100 women.
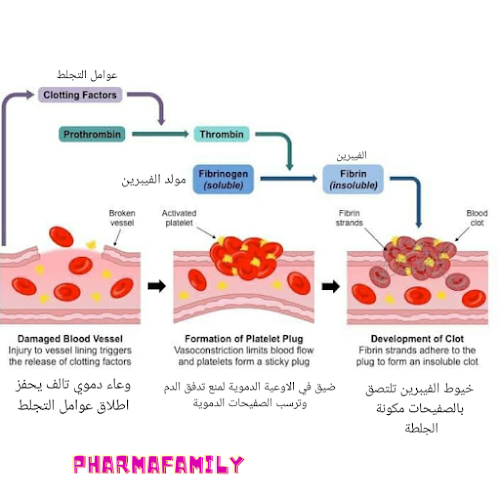
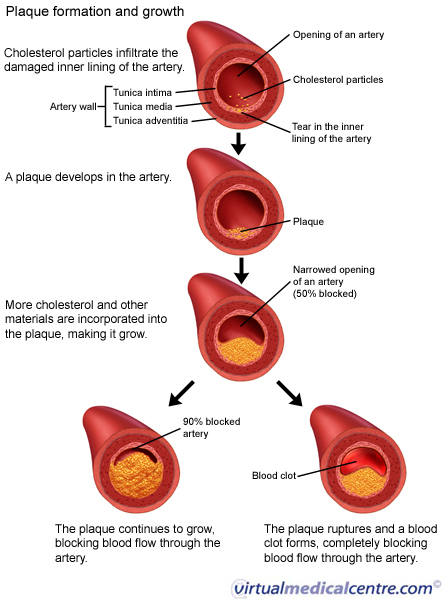
What causes miscarriage?
It is thought that most early miscarriages are caused by a one-off problem with the chromosomes of the developing baby (fetus) in the womb. Chromosomes are the structures that contain the genetic information that we inherit from our parents. If a baby (fetus) doesn't have the correct chromosomes it can't develop properly and so the pregnancy will end. This is usually a one-off mistake and rarely occurs again. Such genetic mistakes become more common when the mother is older - that is, over 35 years old. This means women aged over 35 years who are having children are more likely to have a miscarriage. This may also be why, if your partner is aged over 45 years, you are more likely to have a miscarriage, even if you are under 35 years old.
This may also be why, if your partner is aged over 45 years, you are more likely to have a miscarriage, even if you are under 35 years old.
You are also at a greater risk of having a miscarriage if you:
- Smoke. The risk increases the more cigarettes you smoke.
- Drink too much alcohol. Even drinking four units of alcohol a week (one unit is half a pint of beer or a small glass of wine) has been shown to increase the risk of miscarriage.
- Use recreational drugs.
- Have had fertility problems or it has taken a long time to conceive.
- Have any abnormalities of your womb (uterus) or a weakness of the neck of your womb (the cervix).
- Have certain medical conditions (for example, systemic lupus erythematosus, antiphospholipid syndrome).
- Have diabetes mellitus that is not well controlled.
- Have particular infections like listeria and German measles (rubella).
Investigations into the cause of a miscarriage are not usually carried out unless you have three or more miscarriages in a row. This is because most women who miscarry will not miscarry again. Even two miscarriages are more likely to be due to chance than to some underlying cause. Even after three miscarriages in a row, more than seven women out of every ten will not have a miscarriage next time around.
This is because most women who miscarry will not miscarry again. Even two miscarriages are more likely to be due to chance than to some underlying cause. Even after three miscarriages in a row, more than seven women out of every ten will not have a miscarriage next time around.
Some myths about the cause of miscarriage
After a miscarriage it is common to feel guilty and to blame the miscarriage on something you have done, or failed to do. This is almost always not the case. In particular, miscarriage is not caused by lifting, straining, working too hard, constipation, straining at the toilet, sex, eating spicy foods or taking normal exercise.
There is also no proof that waiting for a certain length of time after a miscarriage improves your chances of having a healthy pregnancy next time.
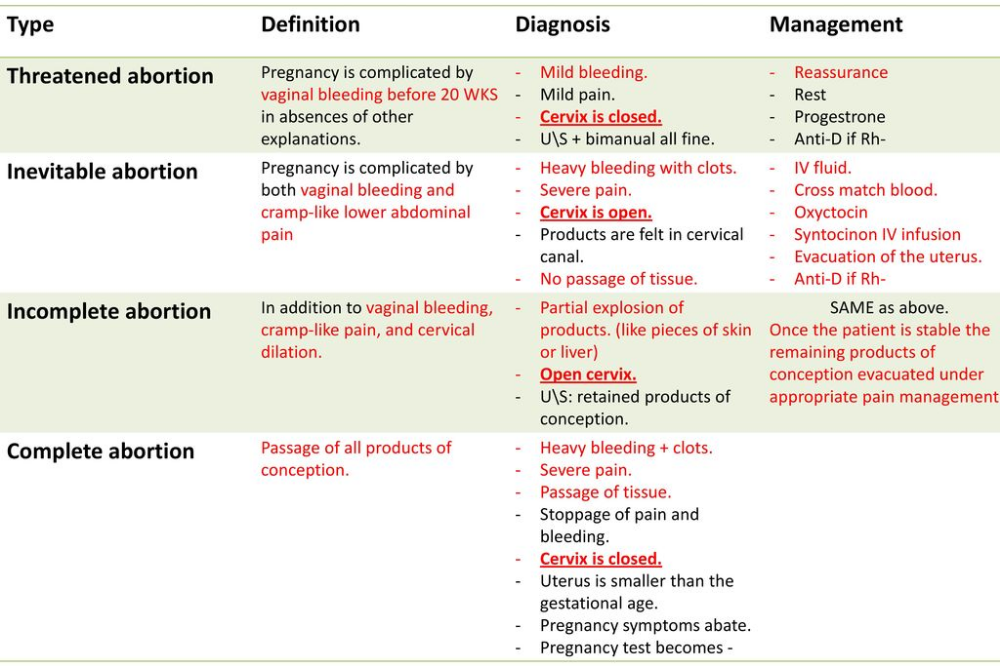
What is a threatened miscarriage?
It is common to have some light vaginal bleeding at some point in the first 12 weeks of pregnancy. This does not always mean that you are going to miscarry. Often the bleeding settles and the developing infant is healthy. This is called a threatened miscarriage. You do not usually have pain with a threatened miscarriage. If the pregnancy continues, there is no harm done to the baby.
Often the bleeding settles and the developing infant is healthy. This is called a threatened miscarriage. You do not usually have pain with a threatened miscarriage. If the pregnancy continues, there is no harm done to the baby.
In some cases, a threatened miscarriage progresses to a miscarriage.
What are the symptoms of miscarriage?
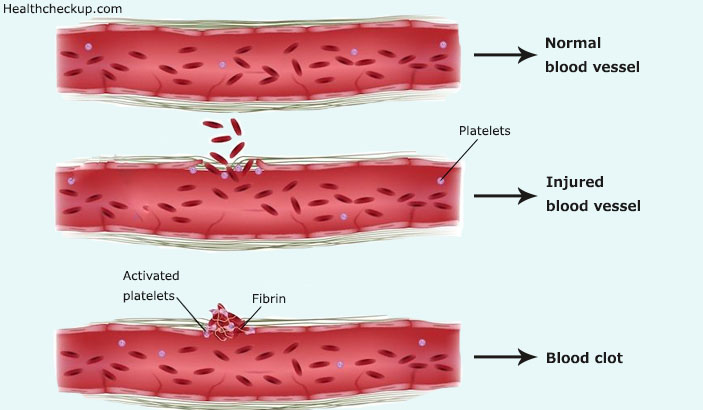
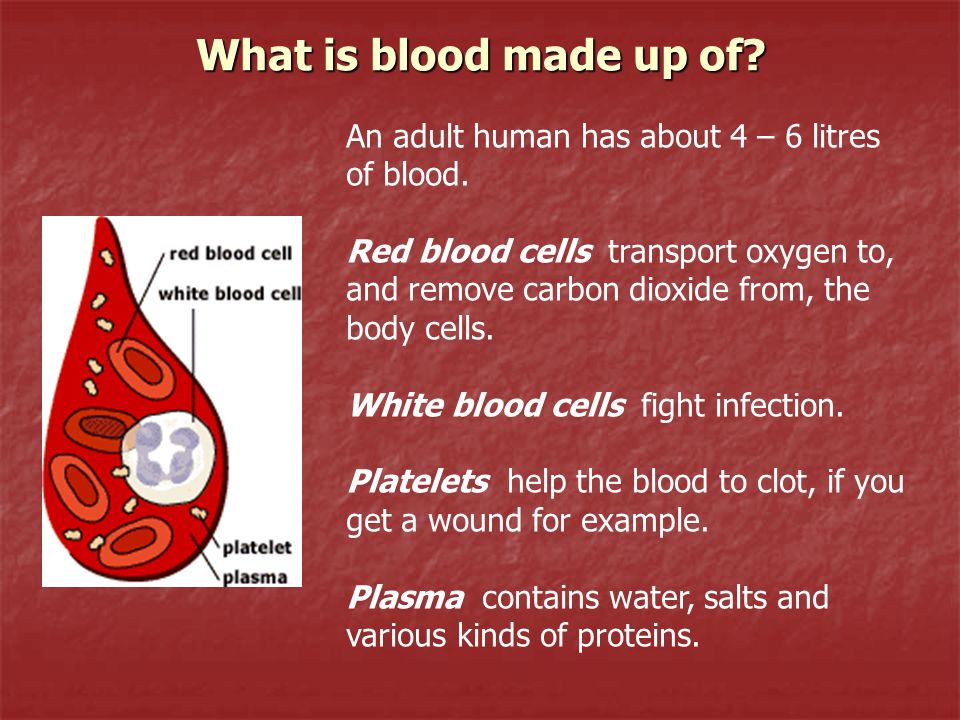
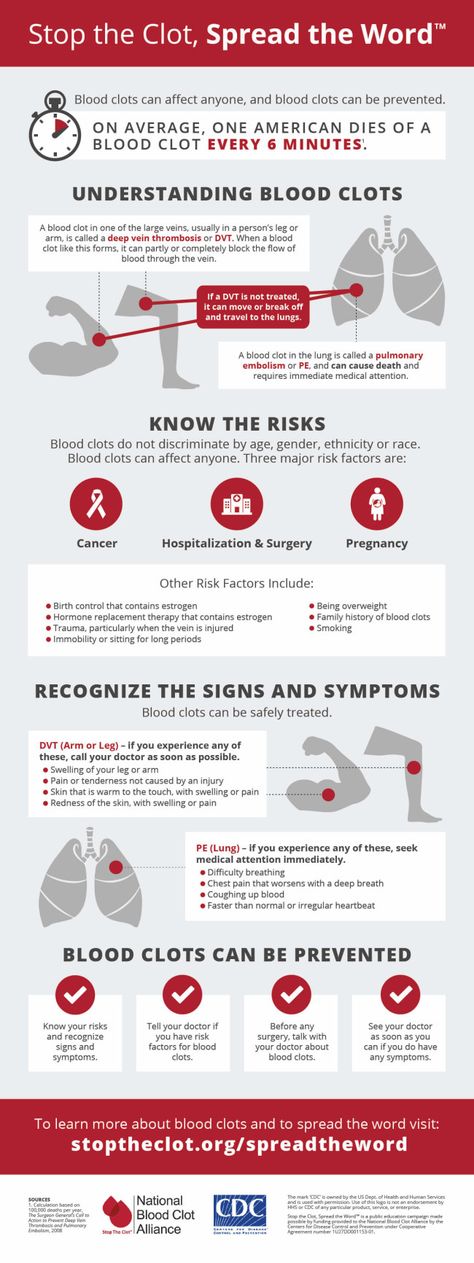
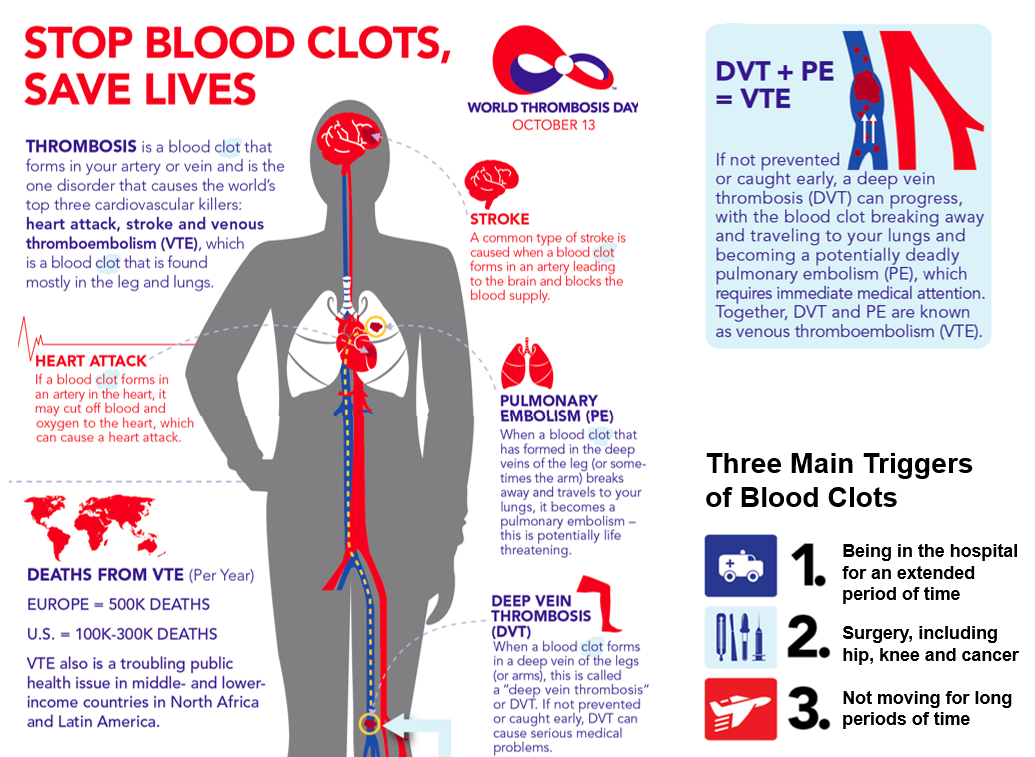
The usual symptoms of miscarriage are vaginal bleeding and lower tummy (abdominal) cramps. You may then pass something from the vagina, which often looks like a blood clot or clots. In many cases, the bleeding then gradually settles. The time it takes for the bleeding to settle varies. It is usually a few days but can last two weeks or more. For most women, the bleeding is heavy with clots but not severe - it is more like a heavy period. However, the bleeding can be extremely heavy in some cases.
In some cases of miscarriage, there are no symptoms. The baby stops developing or dies but it remains in the womb. You may have no pain or bleeding. You may no longer experience symptoms to suggest you are pregnant (for example, morning sickness or breast tenderness). This type of miscarriage may not be found until you have a routine ultrasound scan. This may be referred to by doctors as a missed miscarriage (also called early fetal demise, an empty sac or a blighted ovum).
You may no longer experience symptoms to suggest you are pregnant (for example, morning sickness or breast tenderness). This type of miscarriage may not be found until you have a routine ultrasound scan. This may be referred to by doctors as a missed miscarriage (also called early fetal demise, an empty sac or a blighted ovum).
The typical pain with a miscarriage is crampy lower tummy pain. If you have severe, sharp, or one-sided tummy pain, this may suggest ectopic pregnancy. This is a pregnancy that develops outside the womb. The symptoms of an ectopic pregnancy usually occur at around 6-8 weeks of pregnancy. There may be very little blood lost, or the blood may look almost black. Other symptoms may also occur such as diarrhoea, feeling faint and pain when you open your bowels. Sometimes there are no symptoms until you collapse because of heavy bleeding into the inside of your tummy (internal bleeding). This is called a ruptured ectopic pregnancy and is a potentially life-threatening situation that needs emergency surgery. You should call an ambulance or go to your nearest Accident and Emergency department if you are worried that you may have an ectopic pregnancy.
You should call an ambulance or go to your nearest Accident and Emergency department if you are worried that you may have an ectopic pregnancy.
Do I need to go to hospital?
You should always report any bleeding in pregnancy to your doctor. It is important to get the correct diagnosis, as miscarriage is not the only cause of vaginal bleeding. However, if you are bleeding very heavily or have severe tummy (abdominal) pain when you are pregnant, call for an ambulance immediately.
Editor's note
Dr Sarah Jarvis, November 27th 2021
NICE guidance on miscarriage
The National Institute for Health and Care Excellence (NICE) has updated its recommendations on investigations and treatments in miscarriage. Your doctor will use this guidance to advise on next steps.
The first recommendation is for women who:
- Have a threatened miscarriage; and
- Have had an ultrasound scan which confirms the baby's heartbeat; and
- Have never had a miscarriage before.
If this applies to you, the new guidance recommends that you may not need to be referred straightaway for a scan. However, if your bleeding gets worse or goes on for at least two weeks, you should contact your doctor again. If your bleeding stops, you can continue routine antenatal care.
If you have a scan to confirm your pregnancy but have had a previous miscarriage, you should be offered vaginal progesterone pessaries to use until you have completed 16 weeks of pregnancy.
Most women with bleeding in early pregnancy are seen by a doctor who specialises in pregnancy - an obstetrician. This is often in an Early Pregnancy Assessment Unit at your local hospital. It is usual to have an ultrasound scan. This is usually done by inserting a small probe inside your vagina. This helps to determine whether the bleeding is due to:
- A threatened miscarriage (a heartbeat will be seen inside the womb (uterus)).
- A miscarriage (no heartbeat is seen).
- Some other cause of bleeding (such as an ectopic pregnancy - see above).

If it is unclear from your ultrasound scan whether the pregnancy is healthy or not then you may be asked to return for a repeat scan in one to two weeks.
The usual symptoms of miscarriage are vaginal bleeding and lower tummy (abdominal) cramps
Do I need any treatment?
Once the cause of bleeding is known, your doctor will advise on your treatment options.
Natural or expectant management
Many women now opt to 'let nature take its course'. This is called expectant management. In most cases the remains of your pregnancy are passed out naturally and the bleeding will stop within a few days after this, although can take up to 14 days to occur. However, if your bleeding worsens and becomes heavier or does not settle then you may be offered alternative treatment. Expectant management may not be offered if you have had a miscarriage in the past or if you have a bleeding disorder or any evidence of infection. You may decide that you would prefer to have a definitive treatment rather than taking this approach.
If your bleeding and pain settle then you should perform a pregnancy test after three weeks. If this is positive then you will need to see your doctor for an assessment.
Treatment with medicines
In some cases you may be offered what doctors call medical treatment for your miscarriage. That is, you may be offered a tablet to take either by mouth or to insert into your vagina. The medicine helps to empty your womb (uterus) and can have the same effect as an operation. You do not usually need to be admitted to hospital for this. Some women experience quite severe tummy (abdominal) cramps with this treatment.
You may continue to bleed for up to three weeks when medical treatment is used. However, the bleeding should not be too heavy. Many women prefer this treatment because it usually means that they do not need to be admitted to hospital and do not need an operation.
You should perform a pregnancy test three weeks after receiving medical treatment. If this is positive then you will need to see your doctor for an assessment.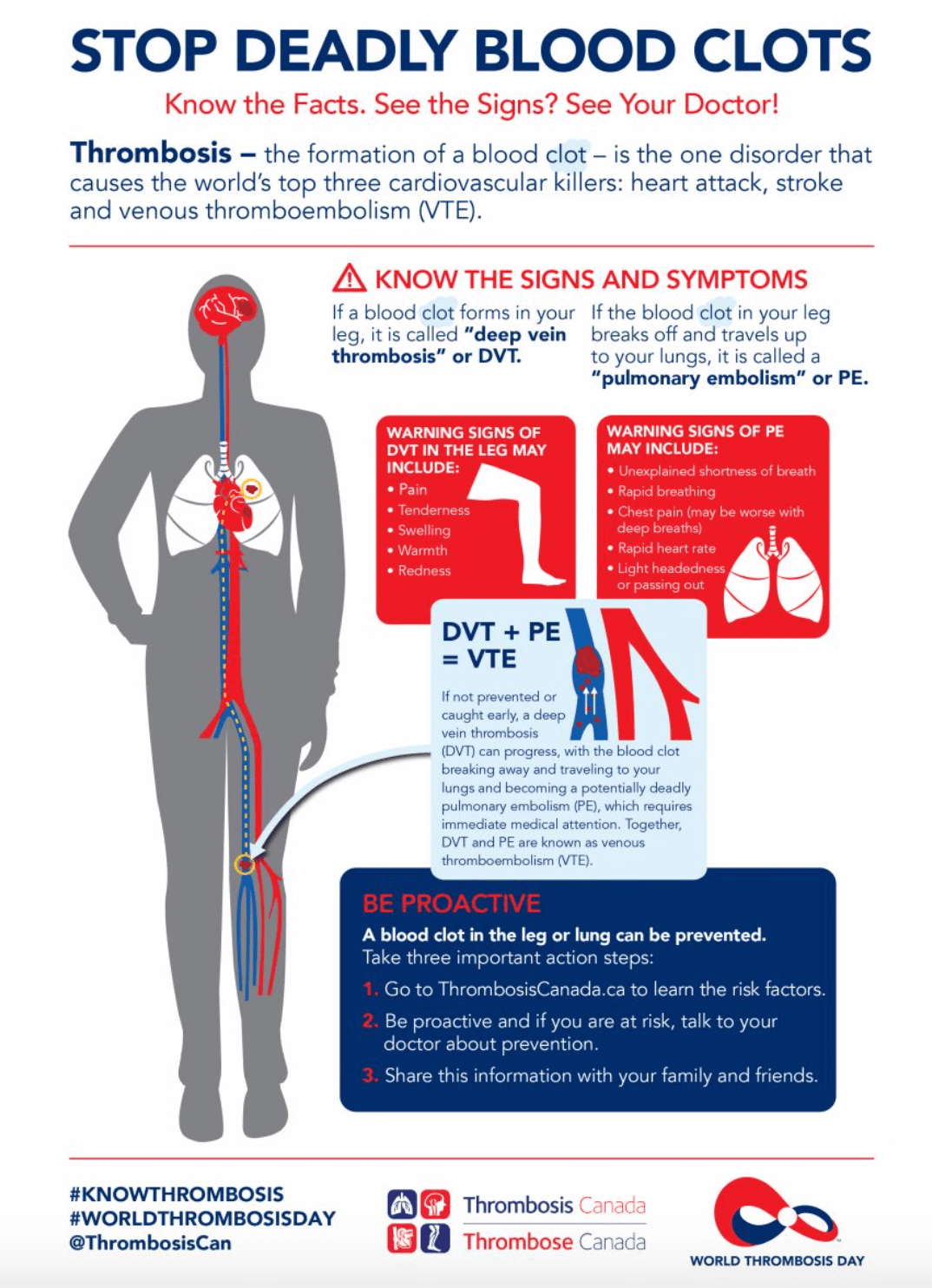
An operation may be offered to you, however, if the bleeding does not stop within a few days, or if the bleeding is severe.
Treatment with an operation
If the options above are not suitable or are not successful then it is likely you will be offered an operation. The operation most commonly performed to remove the remains of your pregnancy is called surgical management of miscarriage (SMM). In this operation, the neck of your womb (the cervix) is gently opened and a narrow suction tube is placed into your womb to remove the remains of your pregnancy. This operation takes around 10 minutes.
This may be performed without the need for a general anaesthetic in some cases. This is called a manual vacuum aspiration (MVA). Your doctor will be able to discuss the procedure in more detail with you.
A few women develop an infection after having this operation. If you experience a high temperature (fever), any offensive-smelling vaginal discharge or abdominal pains then you should see a doctor promptly. Any infection is usually treated successfully with antibiotics.
Any infection is usually treated successfully with antibiotics.
Feelings
Many women and their partners find that miscarriage is distressing. Feelings of shock, grief, depression, guilt, loss and anger are common.
It is best not to bottle up feelings but to discuss them as fully as possible with your partner, friends, a doctor or midwife, or anyone else who can listen and understand. As time goes on, the sense of loss usually becomes less. However, the time this takes varies greatly. Pangs of grief sometimes recur out of the blue. The time when the baby was due to be born may be particularly sad.
Bleeding, Clots, Timing, and Other Signs
Miscarriage is fairly common in the first trimester. It happens in about 10 percent of known pregnancies.
In some cases, miscarriage can occur before you know you’re pregnant. If this happens, you might not notice anything different from your usual period.
The further along you are in a pregnancy, the less likely it is that a miscarriage will feel like a period.
Continue reading to learn more about early miscarriage, including specific symptoms to watch for, when you should see a doctor, and more.
The most common symptoms of early miscarriage are cramping and bleeding.
However, spotting or light bleeding during early pregnancy aren’t always a sign of miscarriage. If this happens, watch for any other unusual symptoms.
Other symptoms of miscarriage
- cramping in your abdomen or lower back (This could start out like period cramps, but the pain typically worsens over time.)
- nausea
- diarrhea
- passing fluids, larger-than-normal blood clots, or tissue from your vagina
Timing
A miscarriage can happen any time after fertilization. If you didn’t know you were pregnant, it would be easy to mistake it for a period.
Both a period and a miscarriage can cause spotting to heavy bleeding.
After the first eight weeks or so, it’s less likely that you’ll mistake a miscarriage for a period.
Duration
You know how long and heavy your typical period is.
During a miscarriage, bleeding gets heavier and lasts longer than a period.
As your cervix starts to dilate, cramping may become more painful than typical period cramping.
Characteristics
Bleeding during miscarriage can appear brown and resemble coffee grounds. Or it can be pink to bright red.
It can alternate between light and heavy or even stop temporarily before starting up again.
If you miscarry before you’re eight weeks pregnant, it might look the same as a heavy period. Later, you’re more likely to notice fetal or placental tissue.
Menstruation products
Heavy bleeding, pieces of tissue, or large blood clots on your menstruation products could mean that you’re having more than a heavy period.
See a doctor if you’re soaking through a tampon or pad every hour for more than two consecutive hours.
You should call a doctor or other healthcare provider any time you experience unexpected pain or excessive bleeding.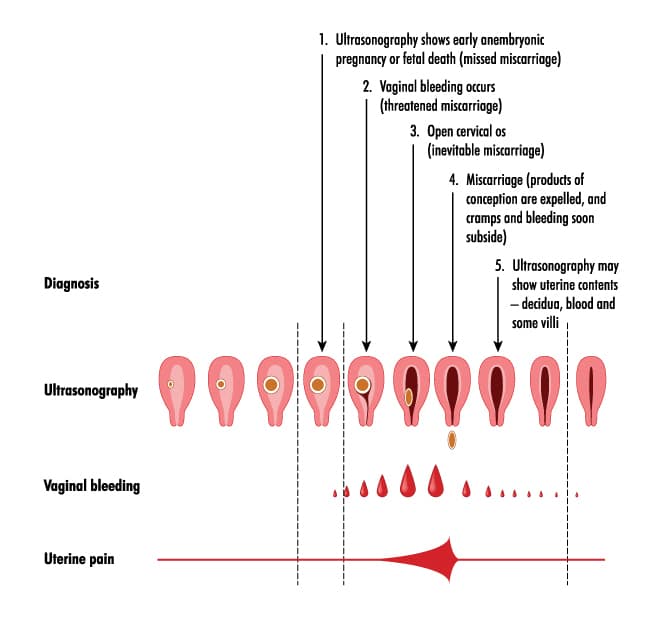
These symptoms can result from an ectopic pregnancy. This occurs when a fertilized egg has implanted outside the uterus, possibly inside a fallopian tube. It’s a medical emergency.
You should also call a doctor if you experience bleeding alongside:
- mucus
- tissue
- blood clots
- what feels like uterine contractions
If you believe you’re having a miscarriage, ask your doctor the following:
- Should I collect a sample of blood or tissue? (This isn’t always necessary.)
- Should I go to an emergency room or make an office appointment?
- Is it fine to drive myself, or do you recommend against it?
If it appears that you’ve had a miscarriage, your doctor will want to perform a physical exam.
Be sure to discuss all your symptoms, including the amount of:
- bleeding
- clotting
- pain
- any tissue that may have been expelled
Testing may include:
- an ultrasound to check the uterus for signs of an embryo or a heartbeat
- a blood test to check for human chorionic gonadotropin (hCG), a substance that indicates pregnancy
There’s no way to stop a miscarriage in progress.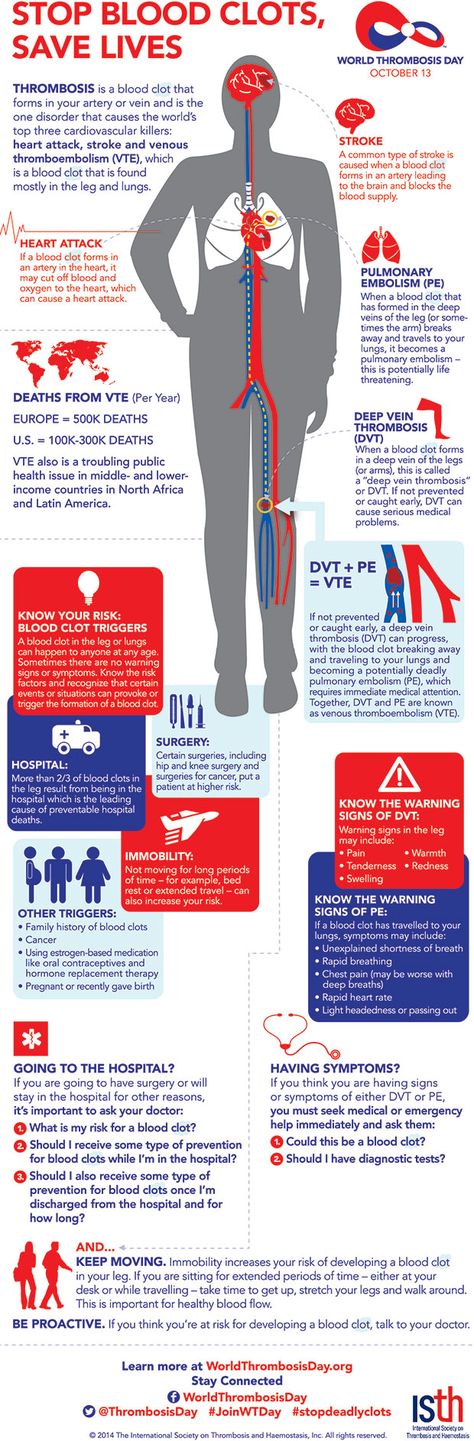 If your doctor determines that you’ve experienced a miscarriage, they’ll want to check for:
If your doctor determines that you’ve experienced a miscarriage, they’ll want to check for:
- signs of infection
- uncontrollable bleeding
- tissue that may be left in your uterus
It can take two weeks or more to completely expel the tissue naturally. Your doctor will review with you typical bleeding patterns to expect. If you have heavy bleeding lasting several days or any signs of infection, you may need medical treatment.
If your doctor isn’t sure that all of the pregnancy tissue has been cleared from your uterus, they may order an ultrasound to confirm.
Your doctor can prescribe medication, such as misoprostol (Cytotec), to increase uterine contractions to help you expel the tissue.
You’ll experience cramping and bleeding as you pass tissue and blood.
Most people pass the tissue within 24 hours after taking the drug. For others, it can take a few days to complete. Either way, it doesn’t require a hospital stay.
Your doctor may be able to prescribe pain medication to help ease your symptoms.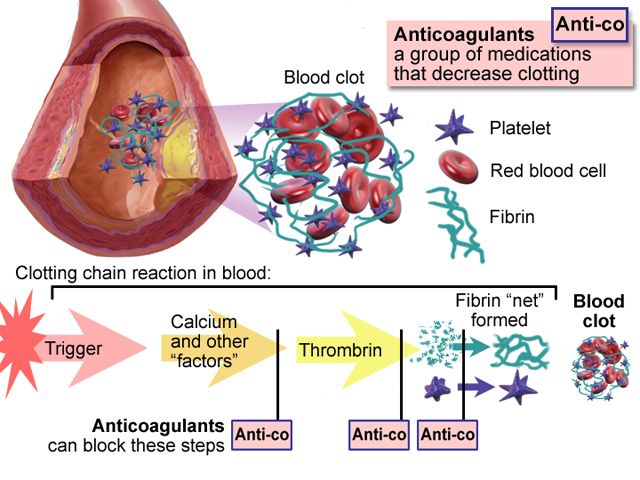
If your blood type is Rh negative, you’ll need an injection of Rh immunoglobulin. This may help prevent complications in a future pregnancy.
There are also a few surgical options to remove tissue from the uterus. This includes:
- Vacuum aspiration. Your doctor inserts a thin tube that contains a suction device into your uterus. This can be done with local anesthesia in your doctor’s office.
- Dilation and curettage (D&C). Your doctor dilates your cervix, and then uses an instrument called a curette to scrape your uterine lining. This can be done at a surgical center or operating room on an outpatient basis. Regional or general anesthesia can be used.
Both of these treatments have been well-studied and are considered safe. They each carry a very small risk of serious complications.
If you’ve experienced a miscarriage, it’s important to understand that it isn’t your fault.
In many cases, doctors are unable determine the cause.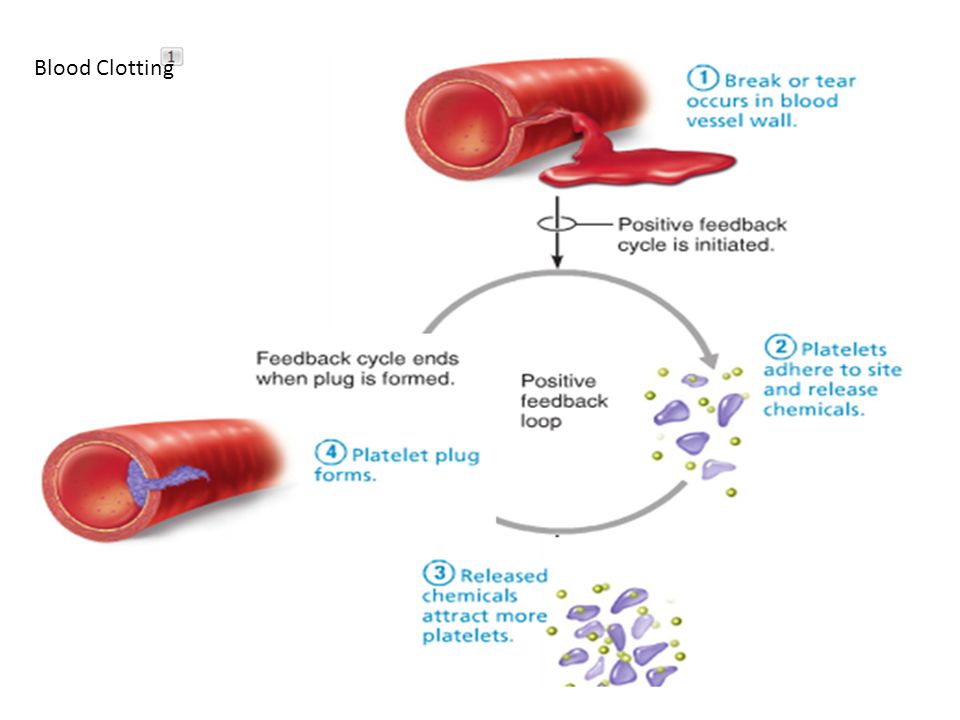 Here are some things that can contribute to miscarriage:
Here are some things that can contribute to miscarriage:
During the first trimester
As many as 80 percent of miscarriages occur in the first trimester.
When a miscarriage occurs in the first five weeks after fertilization, it’s called a “chemical pregnancy.” It’s so early that you might not have known you were pregnant.
Although your period may seem heavier than usual, there might not be any other noticeable sign of miscarriage.
Miscarriages in the first trimester often have to do with chromosome abnormalities that interfere with normal development. Missing or extra chromosomes are linked to 50 percent of all miscarriages.
Sometimes, a fertilized egg simply doesn’t develop into an embryo (blighted ovum).
It may help to know that having sex, exercising, morning sickness, and previous use of oral contraceptives don’t cause miscarriage. Even an accidental fall doesn’t necessarily cause it.
According to the American College of Obstetricians and Gynecologists (ACOG), smoking and alcohol consumption in the first trimester may result in a slightly higher risk of miscarriage.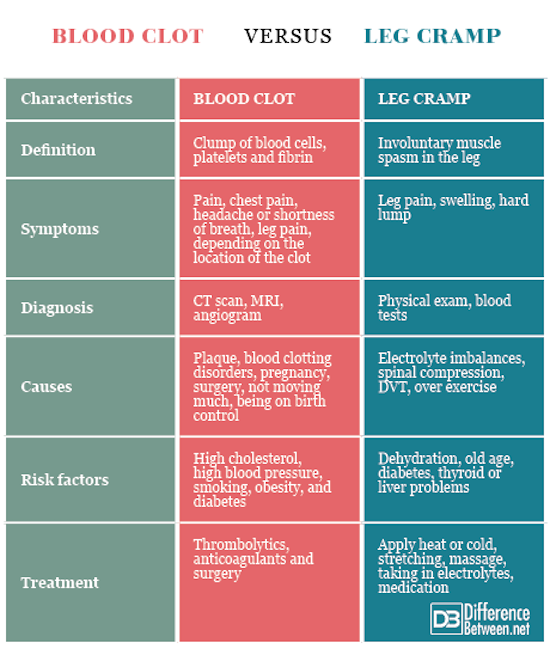 But the research on this is mixed.
But the research on this is mixed.
It’s also worth noting that drinking less than 200 milligrams of caffeine per day doesn’t appear to increase the risk of miscarriage.
Some things that may increase the risk of early miscarriage are:
- fibroids or other abnormalities of the uterus
- hyperthyroidism or hypothyroidism
- uncontrolled diabetes
- use of cocaine or similar drugs
During the second trimester
About 2 to 3 percent of miscarriages occur during the second trimester.
Some things that may increase the risk are:
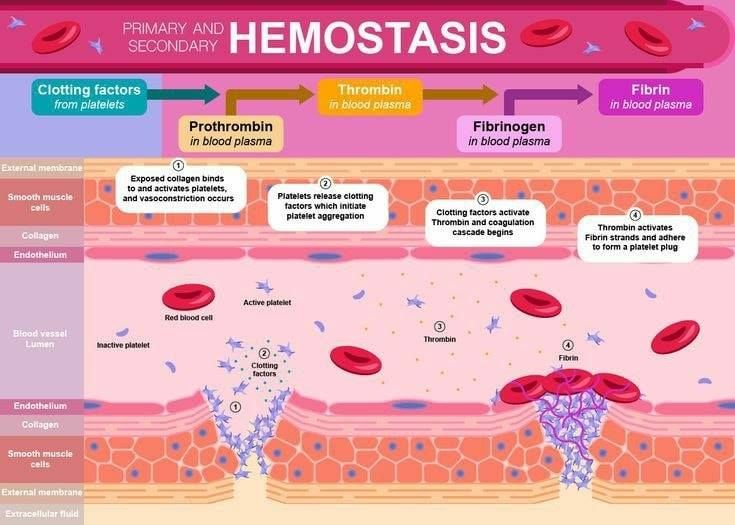
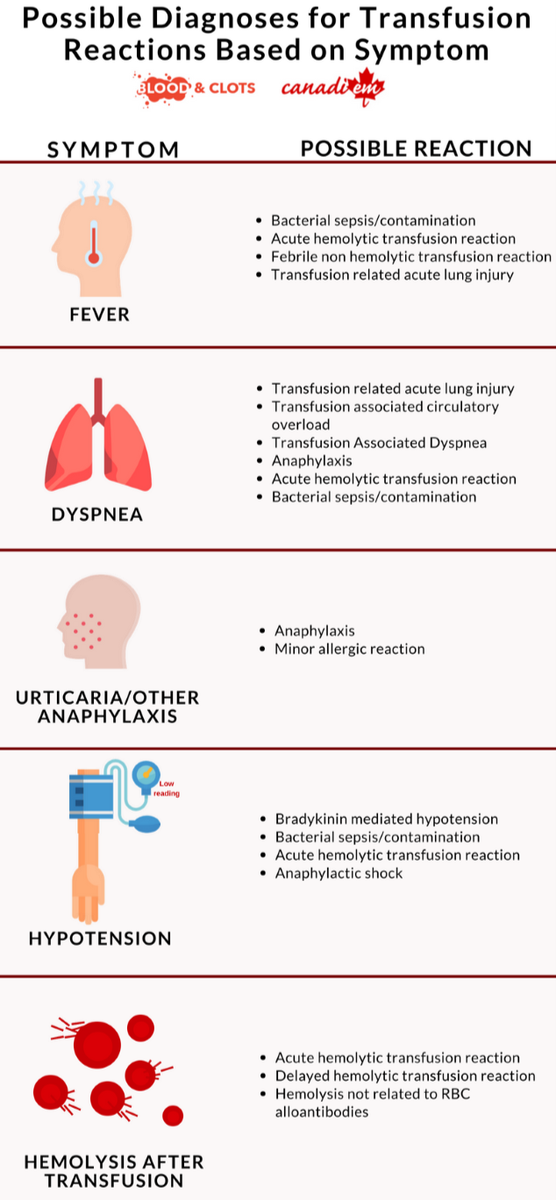
- conditions that can cause blood clots
- early preeclampsia or eclampsia
- fetal abnormalities
- fibroids or other abnormalities of the uterus
- infection of the uterus
- lupus
- prior surgery of the cervix
- trauma
- uncontrolled diabetes
- hyperthyroidism or hypothyroidism
- high blood pressure
- use of cocaine or similar drugs
During the third trimester
Losing a pregnancy starting from the 20th week of pregnancy and into the third trimester is considered stillbirth, not miscarriage.
In general, the risk of stillbirth increases with maternal age.
If you’ve experienced a miscarriage, it doesn’t mean you’ll have another, and it doesn’t mean you can’t have children.
Most people who experience a miscarriage can go on to have a successful pregnancy.
Miscarriage shouldn’t affect your ability to get pregnant. You can ovulate and become pregnant within two weeks of an early miscarriage.
If you don’t want to become pregnant again, you should use birth control right away.
About 1 percent of people have multiple miscarriages. If you’ve experienced several miscarriages, your doctor might recommend special testing.
Even if you’ve had three miscarriages in a row, there’s a 70 percent chance your next pregnancy will be successful.
Your doctor will probably advise you to avoid sex, tampons, and douches for two weeks. This will help prevent infection.
They may also want you to take a pregnancy test after about two weeks.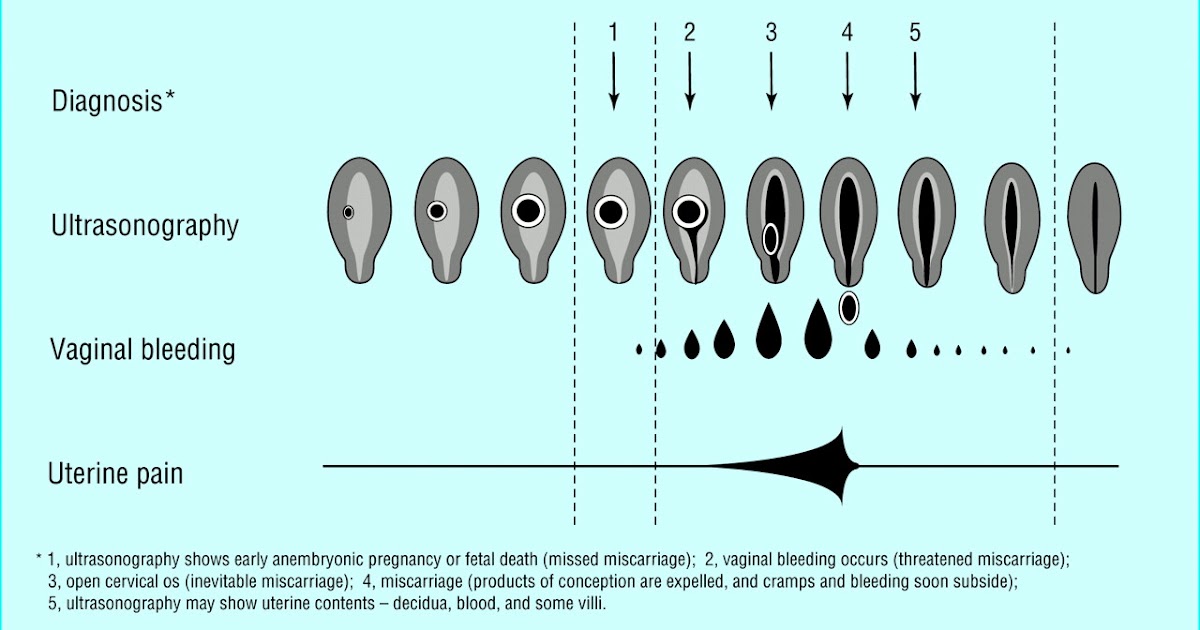 This can help them determine whether your hormone levels are back to normal.
This can help them determine whether your hormone levels are back to normal.
In the meantime, call your doctor if you:
- are bleeding heavier than expected or notice that the blood stays bright red
- are soaking through more than two maxi pads an hour for more than two hours
- notice a foul-smelling discharge
- experience abdominal tenderness or severe pain
- have persistent cramping
- develop a fever or chills
For the first few days, you may notice blood clots and tissue passing, but this should taper off after about a week. It will take about four to eight weeks for your regular period to return.
Mild exercise following an early miscarriage is usually fine, but check with your doctor. It may depend on how far along you were, as well as your overall health.
There are many emotions a person might have following a miscarriage. Some feel anger, sadness, or profound loss. Others might feel relieved.
These feelings may have to do with whether you knew you were pregnant or if you were trying to have a baby.
Pregnancy and miscarriage also cause hormone fluctuations, which can affect your emotions.
Everyone is different, so there’s no correct way to feel about experiencing a miscarriage. It may take some time for you to process everything.
You may find it helpful to talk to your partner, family, or friends about what you’re going through.
You may also consider looking into support groups for people who have experienced miscarriage. Sometimes it helps to talk to others who have been through the same thing.
Here are a few places to seek support:
- your doctor’s office or local hospital for referrals to support services
- clergy
- Compassionate Friends, which has a searchable database of local chapters
- March of Dimes Loss and Grief Forum
- Share Pregnancy & Infant Loss Support which offers online support and information on how to find local groups
If grief continues to worsen after a few weeks, talk to a doctor about your options for treatment.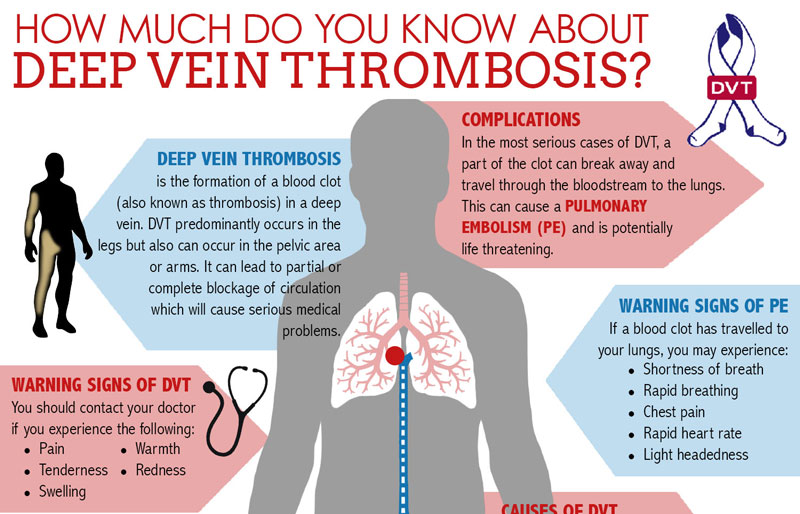 You may benefit from grief counseling or treatment for depression.
You may benefit from grief counseling or treatment for depression.
Miscarriage isn’t your fault.
Physical recovery generally takes a few weeks. Everyone has their own timetable for emotional recovery.
There’s no need to rush yourself or to pretend to “get over it” for anyone else’s sake.
And if you need it, reaching out for support is a reasonable thing to do. You aren’t alone in this.
Miscarriage, symptoms - Health Clinic 365 Yekaterinburg
Causes of miscarriage
Questions to the doctor about miscarriage
Diagnosis of miscarriage
Treatment and prevention of miscarriage
According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus. nine0003 Miscarriage is quite common, but this fact does not make things any easier. Miscarriage symptoms . Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include: It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common. In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage. nine0003 Some women who have a miscarriage develop an infection in the uterus. When to see a doctor. Call your doctor if: You can put a piece of tissue to be isolated in a clean container and take it to your doctor for examination. It is unlikely that the study will give any accurate results, but if it is determined that the fragments of the excreted tissue are from the placenta, the doctor will be able to conclude that the symptoms that appear are not associated with the presence of a tubal (ectopic) pregnancy. nine0003 You can get more detailed information about miscarriage from the gynecologists of the Health 365 clinic in Yekaterinburg. Gynecologist, initial appointment 2300 i Sometimes it happens that a pregnancy ends in a miscarriage. It's unpleasant and painful. But why is this happening and how to avoid such situations in the future? Find out more about this later. nine0003 Early miscarriage is the death of an embryo or fetus in the womb before the 22nd week of pregnancy. It is usually caused by genetic breakdowns, pathologies, injuries or stress. Such a nuisance is quite common and approximately 15-20% of all successful conceptions can end in miscarriage. To understand what's going on, you need to understand what a miscarriage looks like. The most common symptom is profuse bleeding with clots. Sometimes they can be mild at first, and then quite large. Sometimes a miscarriage can start suddenly. But it happens that before this there may be small pulling pains in the lower abdomen, lower back, smearing brown discharge. Women may not immediately realize that they have a miscarriage. Especially if the delay is only a few days, and the test was not done, then you might think that your period just started. But usually a woman who already knows about her pregnancy remembers how a spontaneous miscarriage occurs forever. In most cases, this is profuse bleeding with blood clots, mucus and severe pain in the abdomen. If you do not immediately take action, you may experience chills, fever, the skin will become pale. The patient may even lose consciousness. If a woman does not immediately see a doctor or call an ambulance, she may even die from blood loss, as sometimes such bleeding is incredibly serious. Spontaneous miscarriage can also have symptoms such as nausea, vomiting, frequent urination, dizziness, weakness, Why does it happen that a miscarriage occurs? Here you can name many reasons, but in each case, studies are carried out, the patient takes tests. The causes of spontaneous abortion may be as follows in the first trimester: But besides this, there may be many other specific reasons that are individual for each woman. For example, hard physical work, activities in hazardous enterprises, severe stress and anxiety can also cause spontaneous abortion. The threat of spontaneous miscarriage occurs in many women, but not everyone can have an abortion. Much depends on the state of health, immunity, even emotional state. There are several types of spontaneous abortions: Some other types can also be distinguished: Also, such miscarriages can be divided into several types: Spontaneous abortion can happen to every woman. But there are certain risk factors that by themselves cannot cause a miscarriage, but can be provocateurs: In order to accurately understand that a spontaneous abortion has occurred, it is necessary to correctly diagnose it. If such miscarriages occur frequently, the cause must be investigated. To do this, conduct a variety of studies, consultations with geneticists, endocrinologists and other specialists. How to treat spontaneous miscarriage depends on the type of miscarriage. If it is threatening and has begun, then the following should be done: In any case, abortion should not be left to chance, it is necessary to consult a doctor who will choose the treatment tactics. Spontaneous miscarriage in early pregnancy usually carries certain risks. The consequences of spontaneous miscarriage can be different: Usually, if the patient has received quality medical care, there are practically no complications. After about 10 days, the bleeding stops, and after 4 weeks, the woman begins her regular menstruation. Pregnancy after spontaneous miscarriage can occur and be quite successful. But first you need to establish the cause of the abortion. If these are genetic problems, endocrine pathologies, troubles with the blood or uterus, then special treatment is necessary. Spontaneous abortion is an unpleasant phenomenon that can happen to every woman. But it is necessary to carry out the treatment correctly and consult a doctor in time. In addition, preventive measures should be taken.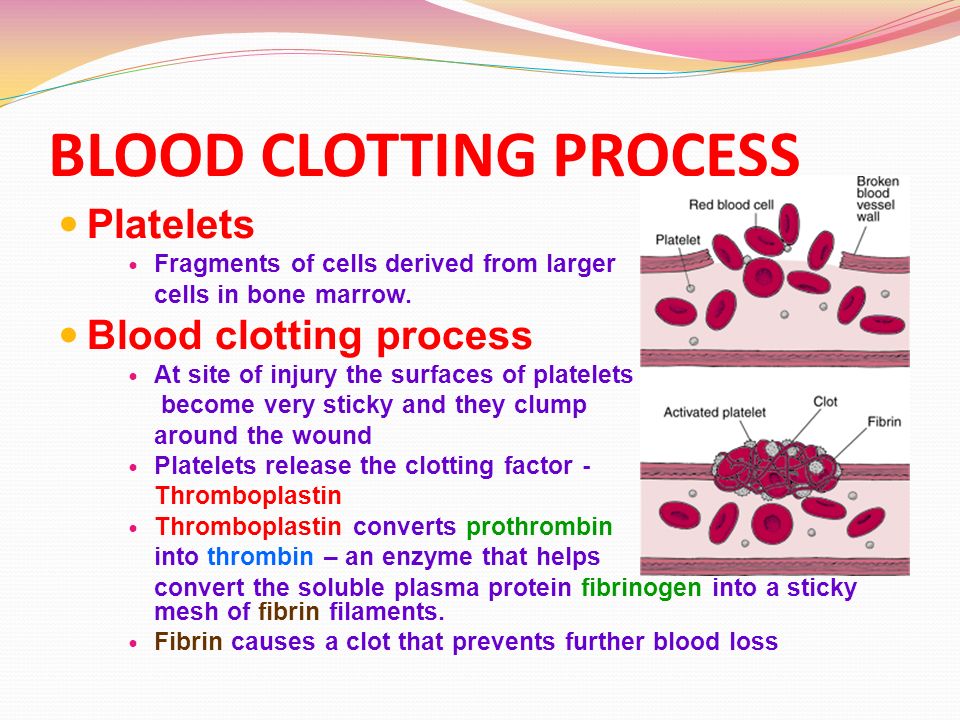 It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
 This infection, also called septic miscarriage, can cause:
This infection, also called septic miscarriage, can cause:
Prices
What is a spontaneous miscarriage and how it happens
What is it?
What are the signs of a miscarriage?
 You should monitor your condition and if at least a slight bleeding has begun, you should immediately consult a doctor. nine0003
You should monitor your condition and if at least a slight bleeding has begun, you should immediately consult a doctor. nine0003 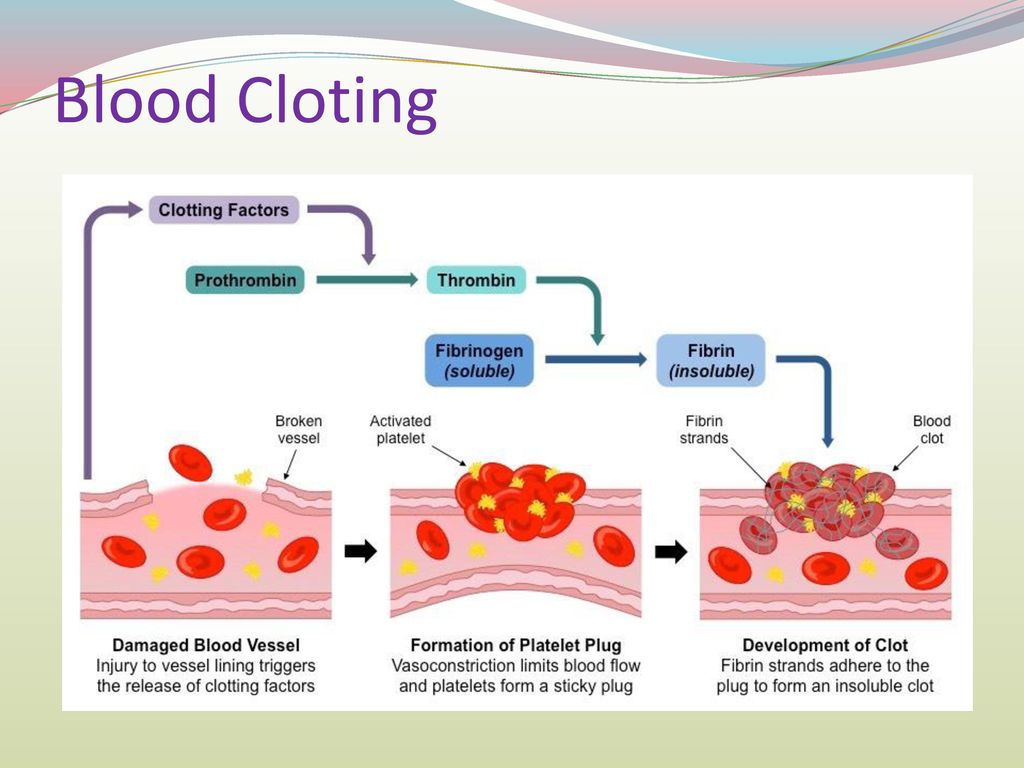 nine0003
nine0003 What can cause an early miscarriage?
What types of miscarriage can there be? nine0077
What cannot cause a miscarriage
Diagnosing a miscarriage
 To do this, you should:
To do this, you should:
How to treat? nine0077
What are the consequences?
Is there any prevention?
 But there are general recommendations that will help reduce the risk of miscarriages:
But there are general recommendations that will help reduce the risk of miscarriages: