Anti itch cream pregnancy
How to Treat Itchy Skin Naturally During Pregnancy
During pregnancy, as the blood supply to the skin increases, it is very common to experience mild itching. You may also experience itching as the skin on your abdomen stretches. If you experience mild itching during pregnancy, there are several natural steps you can take to alleviate your symptoms.
- Regularly apply an unscented lotion or moisturizer.
- Wear clothing that is loose so it is less likely to irritate the skin.
- Try to wear clothing made of natural fibers, such as cotton, which are more breathable than synthetic materials.
How to Treat Itchy Skin During Pregnancy When Naturally Doesn’t Work
If natural options do not work, you may consider taking medication. You may also find calamine lotion beneficial in alleviating the itching. Keep in mind, however, that the safety of using calamine lotion during pregnancy and breastfeeding is unknown, so make sure to talk with your doctor before using it.
When Itching is Severe Contact Your Healthcare Provider
More severe itching may indicate an underlying liver condition known as Intrahepatic Cholestasis of Pregnancy (ICP) or Obstetric Cholestasis (OC). Your doctor may perform a set of liver function tests (LFTs) to determine if you have obstetric cholestasis. If you are diagnosed with OC, your doctor will need to regularly perform LFTS for the duration of your pregnancy to monitor the health of both you and the baby.
While there is currently no cure for OC, some options for easing symptoms include taking a warm bath or applying ice to an itchy area of skin. As OC can interfere with the absorption of vitamin K, which is necessary for proper blood clotting, your doctor may also recommend that you take a vitamin K supplement.
OC is a liver condition that disrupts the flow of bile in the body during pregnancy. Bile salts generally flow from the liver to the digestive tract to aid in digestion. With OC, the flow of bile is disrupted causing a buildup of bile in the body. This can cause severe itching all over the body, although for some women, itching occurs primarily on the hands and feet.
This can cause severe itching all over the body, although for some women, itching occurs primarily on the hands and feet.
Such itching may worsen at night but is not typically accompanied by a rash. Other symptoms may include dark urine, gray bowel movements, and Jaundice (yellowing of the skin and whites of the eyes).
OC occurs most commonly during the third trimester, although it can develop earlier. The good news is that it generally subsides within a few days after delivery.
While OC affects less than 1% of pregnant women, it is a potentially serious condition that needs to be monitored by your doctor, particularly as it increases the risk for pregnancy complications such as preterm birth and stillbirth.
An additional condition that may cause itchiness is prurigo of pregnancy
This condition is characterized by small, itchy bumps on the skin which may be mistaken for insect bites. Prurigo can occur at any point during pregnancy and may continue post-delivery. Many believe it is caused by changes in immune function during pregnancy. Fortunately, prurigo poses no risk to your baby.
Many believe it is caused by changes in immune function during pregnancy. Fortunately, prurigo poses no risk to your baby.
To treat prurigo, your doctor may prescribe topical emollients or steroids combined with oral antihistamines.
For OC, it is not recommended to use antihistamines or corticosteroid creams during pregnancy as they may be harmful to your baby. However, medications, such as Urso, can help reduce bile in the mother’s blood.
These medications also alleviate itchiness and reduce the risk of complications for the fetus. Urso is safe to take during pregnancy, although caution is advised when using it while breastfeeding.
While such medication may help treat OC, your doctor may also want to induce labor early to prevent complications such as stillbirth. If you have OC, make sure to talk with your doctor or midwife about your options.
Want to Know More?
- Skin Changes During Pregnancy
- How Your Body Changes During Pregnancy
- Treating Mosquito Bites Naturally During Pregnancy
Compiled using information from the following sources:
1. ICP Care. (n.d.). What is ICP? Overview.
ICP Care. (n.d.). What is ICP? Overview.
2. Mayo Clinic Staff. (2014, August 16). Cholestasis of pregnancy.
https://www.mayoclinic.org/diseases-conditions/cholestasis-of-pregnancy/basics/definition/con-20032985
3. National Health Service. (2014). Itching and obstetric cholestasis in pregnancy.
https://www.nhs.uk/conditions/pregnancy-and-baby/pages/itching-obstetric-cholestasis-pregnant.aspx#close
4. PDR Network. (n.d.). Drug summary: Urso 250/Urso Forte.
https://www.pdr.net/drug-summary/urso-250-urso-forte?druglabelid=2807
5. PDR Network. (n.d.). Drug summary: Calamine.
https://www.pdr.net/drug-summary/calamine?druglabelid=2638
6. Sachdeva, S. (2008). The dermatoses of pregnancy. Indian Journal of Dermatology, 53, 103-105. doi: 10.4103/0019-5154.43203
7. The American College of Obstetrics and Gynecologists. (2014). Skin conditions during pregnancy.
https://www.acog.org/Patients/FAQs/Skin-Conditions-During-Pregnancy
The Safety Of Anti-Itch Creams During Pregnancy
Pregnancy
What medications can be used to reduce itching in pregnancy
Megha Trivedi, MD
AUTHOR
Raja Sivamani, MD MS AP
EDITOR
Some of us have dealt with itchiness our entire lives and have become masters at deciding which medications we can use to control those itching urges. However, whether or not you’ve had experience with itchiness, pregnancy can be a challenging time and many women have questions about medication safety when trying to control their symptoms. This article aims to give you the information you need about systemic (medications that get into the bloodstream) therapies for itch and their safety for a developing baby. Antihistamines are the major category of drugs which will be discussed.
However, whether or not you’ve had experience with itchiness, pregnancy can be a challenging time and many women have questions about medication safety when trying to control their symptoms. This article aims to give you the information you need about systemic (medications that get into the bloodstream) therapies for itch and their safety for a developing baby. Antihistamines are the major category of drugs which will be discussed.
Antihistamines can be divided into two major categories: first-generation and second-generation. The major difference is that the first-generation drugs have been around longer and have greater penetration into the circulation of the central nervous system. This means that they have greater sedative effects compared to second-generation agents (why many people feel sleepy after taking a medication with diphenhydramine). For the same reason, the first generation drugs are also used to control nausea and vomiting during pregnancy.[1] Some common first-generation agents include Diphenhydramine (ingredient in Benadryl), hydroxyzine (ingredient in Vistaril and Atarax), and chlorpheniramine (ingredient in Aller-Chlor, and Teldrin). Common second-generation agents include Loratadine (ingredient in Claritin), cetirizine (ingredient in Zyrtec), and fexofenadine (ingredient in Allegra).[2]
Common second-generation agents include Loratadine (ingredient in Claritin), cetirizine (ingredient in Zyrtec), and fexofenadine (ingredient in Allegra).[2]
Pregnancy Category B Antihistamines
Pregnancy category B indicates that there are very few human studies, if any, but animal studies do not show an increased risk of adverse effects on the fetus with use of the medication.
The first generation antihistamines - diphenhydramine and chlorpheniramine - and the second-generation antihistamines - loratadine and cetirizine - are considered pregnancy category B medications. The “Allergic Rhinitis and its Impact on Asthma” guidelines recommend using second-generation antihistamines over first-generations because of fewer sedative and other side effects in the general population.[3] However, it can be argued that first-generation agents are preferred during pregnancy since there is a greater amount of safety data published for these medications in pregnant women. [2]
[2]
Several large meta-analyses (combines the results of many reports/studies on one topic and presents the major conclusion) on safety data of antihistamine use in pregnancy have concluded there is no definitive risk of an increased rate of birth defects or other adverse fetal outcomes compared to the general population. Overall, these reports have indicated the relative safety of these medications in pregnancy. One recent large report that included 32 individual studies stated no significant correlation between antihistamine use and fetal malformations, prematurity, spontaneous abortions, low birth weight, or stillbirths. This report went on to further state that 3 cases in which expectant mothers were accidentally exposed to overdoses of medication did not result in any adverse fetal outcomes.[4]
Current recommendations are that first-generation antihistamines are preferred over second-generation agents in pregnant women. However, care should be used with all antihistamines in the third trimester close to the time of birth. IV antihistamines and high doses should be avoided especially during this time, as they are known to stimulate uterine contractions which can result in lack of oxygen to the baby (especially diphenhydramine). Of the second-generation medications, loratadine should be used before trying cetirizine.[2]
IV antihistamines and high doses should be avoided especially during this time, as they are known to stimulate uterine contractions which can result in lack of oxygen to the baby (especially diphenhydramine). Of the second-generation medications, loratadine should be used before trying cetirizine.[2]
In terms of lactation safety, diphenhydramine and cetirizine are considered L2 (safer), but the baby should be monitored for effects of sedation. Chlorpheniramine is L3 (moderately safe), and again the baby should be monitored for excessive sedation. Loratadine is considered L1 (safest), but the baby should be monitored for effects of sedation, fast heart rate, and dry mouth.[2]
Pregnancy Category C Antihistamines
Pregnancy category C includes medications for which there is no human data, and animal studies do not exist or show adverse effects to the fetus.
This category includes the first-generation antihistamine, hydroxyzine, and the second-generation antihistamine, fexofenadine.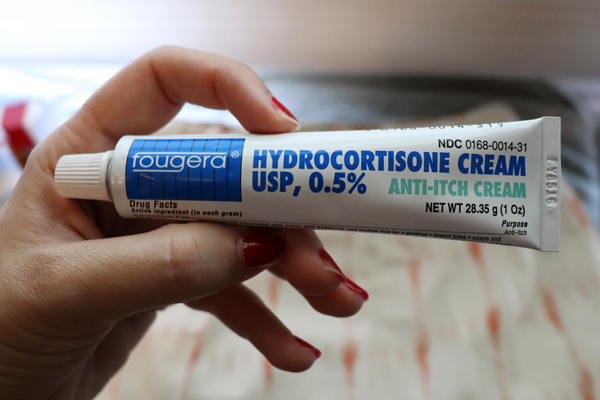
Care should be used when using these agents during pregnancy, as there have been reports of adverse fetal outcomes in human reports and/or animal studies with both medications. High doses of hydroxyzine use in pregnant mothers have been associated with withdrawal symptoms in newborns, including tonic-clonic seizures in one report. Currently, hydroxyzine is not prescribed to pregnant women by allergists.[5] There is limited data on the use of fexofenadine in pregnant women, but a few reports have correlated its use with low birth weight in animal studies. Since there is very little known about this drug, it is not recommended as a first-line agent in pregnant women with an itch.[5]
Hydroxyzine is L1 in lactation safety (safest), but the baby should be monitored for sedation, dry mouth, and high heart rate. Fexofenadine is L2 (safer), and the baby should be monitored for sedation.[2]
A Word About Oral Doxepin
This drug is known as tricyclic antidepressant, and its original use was to treat depression and sleep disorders. However, it has also been found to be useful in the treatment of itch. No animal studies have demonstrated fetal malformations or adverse fetal side effects with the use of this drug. This being said, there are very few, if any, human studies evaluating this drug during pregnancy. There has been one report of polydactyly, heart defects, and oral cleft abnormalities correlated with maternal exposures to the medication in the first trimester. It is recommended to use antihistamines before attempting to use this medication to control the itch. This drug should especially be avoided in the third trimester due to the risk of reduced muscle tone, vomiting, and weak suck in the newborn.[2]
However, it has also been found to be useful in the treatment of itch. No animal studies have demonstrated fetal malformations or adverse fetal side effects with the use of this drug. This being said, there are very few, if any, human studies evaluating this drug during pregnancy. There has been one report of polydactyly, heart defects, and oral cleft abnormalities correlated with maternal exposures to the medication in the first trimester. It is recommended to use antihistamines before attempting to use this medication to control the itch. This drug should especially be avoided in the third trimester due to the risk of reduced muscle tone, vomiting, and weak suck in the newborn.[2]
In terms of lactation safety, it is considered L5 (contraindicated), as this drug is thought to be secreted in breast milk and can cause an infant to experience breathing difficulties, loss of muscle tone, decreased suckling and vomiting.[6]
* This Website is for general skin beauty, wellness, and health information only. This Website is not to be used as a substitute for medical advice, diagnosis or treatment of any health condition or problem. The information provided on this Website should never be used to disregard, delay, or refuse treatment or advice from a physician or a qualified health provider.
This Website is not to be used as a substitute for medical advice, diagnosis or treatment of any health condition or problem. The information provided on this Website should never be used to disregard, delay, or refuse treatment or advice from a physician or a qualified health provider.
References
- Gilboa SM, Ailes EC, Rai RP, et al.: (2014). Antihistamines and birth defects: A systematic review of the literature. Expert Opinion on Drug Safety, 13(12):1667–98. PMID: 25307228
- Murase JE, Heller MM, Butler DC. (2014). Safety of dermatologic medications in pregnancy and lactation: Part I. Pregnancy. Journal of the American Academy of Dermatology, 70(3):401-e1. PMID: 24528911
- Ridolo E, Caminati M, Martignago I, et al.: (2016). Allergic rhinitis: pharmacotherapy in pregnancy and old age. Expert Review in Clinical Pharmacology, 9(8):1081–9. PMID: 27177184
- Etwel F, Faught LH, Rieder MJ, et al.: (2016). The Risk of Adverse Pregnancy Outcome After First Trimester Exposure to h2 Antihistamines: A Systematic Review and Meta-Analysis.
 Drug Safety, 22:1-2. PMID: 27878468
Drug Safety, 22:1-2. PMID: 27878468 - Gonzalez-Estrada A, Geraci SA. (2016). Allergy Medications During Pregnancy. American Journal of the Medical Sciences, 352(3):326-3. PMID: 27650241
- Frey OR, Scheidt P, von Brenndorff AI. (1999). Adverse effects in a newborn infant breast-fed by a mother treated with doxepin. Annals of Pharmacotherapy, 33(6):690-3. PMID: 10410181
Share
Why does the skin itch during pregnancy?
Skin itching during pregnancy is not a very common phenomenon. Most often, the skin begins to itch unbearably (as after mosquito bites) in the evening, closer to night, which can provoke insomnia and generally worsen a woman’s mood. Usually itching does not harm the baby and goes away after childbirth. However, it is still worth consulting with a gynecologist and dermatologist.
What does it come from?
The cause of itching during pregnancy in most cases is a violation of the liver: the production and outflow of bile, a general increase in the level of bilirubin in the blood.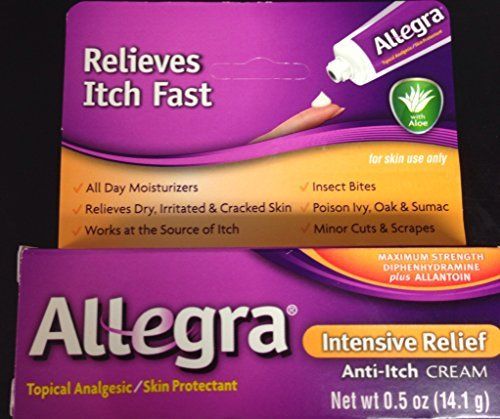 This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
Who is predisposed?
Itching during pregnancy is usually observed in women with chronic diseases of the biliary tract and with high levels of cholesterol in the blood. Such future mothers need to regularly (at least once a month) do a biochemical blood test to exclude toxic effects on liver cells.
How to fight?
A pregnant woman should tell her gynecologist about the discomfort associated with skin itching. In some cases, itching can be a sign of the development of such a dangerous disease as hepatitis. The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
It is important to find the cause of the bothersome itching, eliminating a whole group of skin diseases that can occur during pregnancy.
Itching in the abdomen and chest
This itch is worth mentioning separately. As a rule, the skin on the abdomen or chest itches in the second and third trimesters due to its stretching, because it is these parts of the body that increase in volume during pregnancy. In this case, it is very important not to scratch the skin - this will lead to the appearance of stretch marks, which, unlike itching, will not go away after childbirth. Regularly use moisturizing creams, special products for stretch marks, do a light massage of the chest and abdomen with circular movements of your fingers and do not take hot showers.
Regularly use moisturizing creams, special products for stretch marks, do a light massage of the chest and abdomen with circular movements of your fingers and do not take hot showers.
You can get answers to any questions about pregnancy and childbirth from leading EMC experts in the classes of the School of Moms.
Subscribe to our Instagram. You will find useful information about pregnancy and childbirth from leading EMC obstetricians and gynecologists.
Ecofucin for the treatment of thrush during pregnancy.
Thrush is a disease of the vaginal and vulvar mucosa caused by yeast-like fungi of the genus Candida, which affects 35% of women during pregnancy 1 .
At risk for the occurrence of a recurrent form of thrush are those pregnant women who have already had episodes of thrush in their anamnesis the level of estrogens rises, and therefore glycogen accumulates in the vaginal mucosa - a nutrient medium for yeast-like fungi of the genus Candida.
Lactobacillus is the predominant microorganism in the vaginal microflora of a healthy woman. A normal concentration of lactobacilli provides the necessary acidity in the vagina, which inhibits the growth of fungi. Lactobacilli also participate in the formation of local immunity
In addition, during thrush, the vaginal microflora is disturbed - the number of lactobacilli decreases sharply. These changes lead to the growth and reproduction of pathogenic fungi of the genus Candida, which leads to an increase in the number of manifestations of acute and recurrent forms of thrush.
Symptoms of thrush in a pregnant woman:
- itching and burning in the vulva and/or vagina, swelling and irritation in the vulva
- vaginal discharge of a "cheesy character", sometimes with an unpleasant odor
- pain during and after intercourse
- urination disorder and pain
The appearance of at least one of the symptoms is a reason for an unscheduled visit to the doctor.
Why is it important to diagnose and treat thrush in a pregnant woman in time?
Some women are asymptomatic carriers of yeast-like fungi of the genus Candida and experience neither discomfort nor manifestations of the disease throughout the entire period of pregnancy 2
A pregnant woman with thrush (including an asymptomatic carrier) is a source of infection for her unborn child. Infection from mother to child occurs in 75-80% of cases 3 . Infection of a newborn occurs when passing through the birth canal (the skin of the child comes into contact with the infected mucous membranes of the mother's birth canal). In newborns, candidiasis is manifested by lesions of the mucous membranes and skin 2 , which can lead to negative consequences. For premature babies, infection with fungi of the genus Candida is especially dangerous 2 .
Timely and effective treatment of thrush in a pregnant woman is an important task
Treatment of thrush
Safety and efficacy are the main criteria for choosing a drug in the treatment of thrush in pregnant women
The earlier a pregnant woman is diagnosed and treated for thrush, the less the risk of negative consequences and complications for the course of pregnancy and for the health of the mother and her unborn child. In the treatment of thrush, experts recommend an integrated approach to therapy.
In the treatment of thrush, experts recommend an integrated approach to therapy.
It is important to follow the recommendations of a specialist, following the prescribed dosages and regimen.
Comprehensive treatment should be aimed at solving two problems: eliminating the cause of thrush (fungi of the genus Candida) and restoring the vaginal microflora. It is important to know that not all drugs are approved for use during pregnancy. For example, most oral (systemic) drugs and some topical drugs for treating thrush are contraindicated during pregnancy.
Ecofucin
® in the treatment of thrush in pregnancyEcofucin
® is allowed at all stages of pregnancy and lactation 4
Natamycin
- practically not absorbed into the blood and has no systemic effect
- has fungicidal action - causes fungal cell death
- resistance to it does not develop
- does not inhibit the growth of natural microflora
+
Prebiotic 5
- actively fermented by the normal microflora of the vagina, stimulating the growth of lactobacilli 6
- causes restoration of the vaginal microflora, stimulates local immunity 6
The active substance 7 of the drug Ecofucin ® eliminates the cause of thrush, and the prebiotic 5 in the composition of the drug Ecofucin ® helps to restore the vaginal microflora and strengthen local immunity 6 .
Efficacy and safety of the drug Ecofucin proven by clinical studies
Ecofucin promotes faster recovery of patients with thrush.
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Ecofucin increases the number of own lactobacilli in the vagina and reduces the risk of recurrence of thrush.
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Dosage and Administration
The regimen for the use of Ecofucin ® in a pregnant woman is prescribed by the attending physician individually.
Additional conditions for effective treatment of thrush are: giving up bad habits, a carbohydrate-restricted diet, wearing underwear made from natural fabrics, etc.
It is important to consult a gynecologist in a timely manner and exclude self-treatment.
1. Tikhomirov A.L., Sarsania S.I. Features of candidal vulvovaginitis in pregnant women at the present stage. // Farmateka No. 9, 2009, p. 64-70.
2. Prilepskaya V.N., Mirzabalaeva A.K., Kira E.F., Gomberg M.A., Apolikhina I.A., Bairamova G.R. Federal clinical guidelines "Urogenital candidiasis". // 2013.