Acid reflux or pregnancy
Indigestion and heartburn in pregnancy
Indigestion, also called heartburn or acid reflux, is common in pregnancy. It can be caused by hormonal changes and the growing baby pressing against your stomach.
You can help ease indigestion and heartburn by making changes to your diet and lifestyle, and there are medicines that are safe to take in pregnancy.
Symptoms of indigestion and heartburn
Symptoms of indigestion and heartburn include:
- a burning sensation or pain in the chest
- feeling full, heavy or bloated
- burping or belching
- feeling or being sick
- bringing up food
Symptoms usually come on soon after eating or drinking, but there can sometimes be a delay between eating and developing indigestion.
You can get symptoms at any point during your pregnancy, but they are more common from 27 weeks onwards.
Things you can do to help with indigestion and heartburn
Changes to your diet and lifestyle may be enough to control your symptoms, particularly if they are mild.
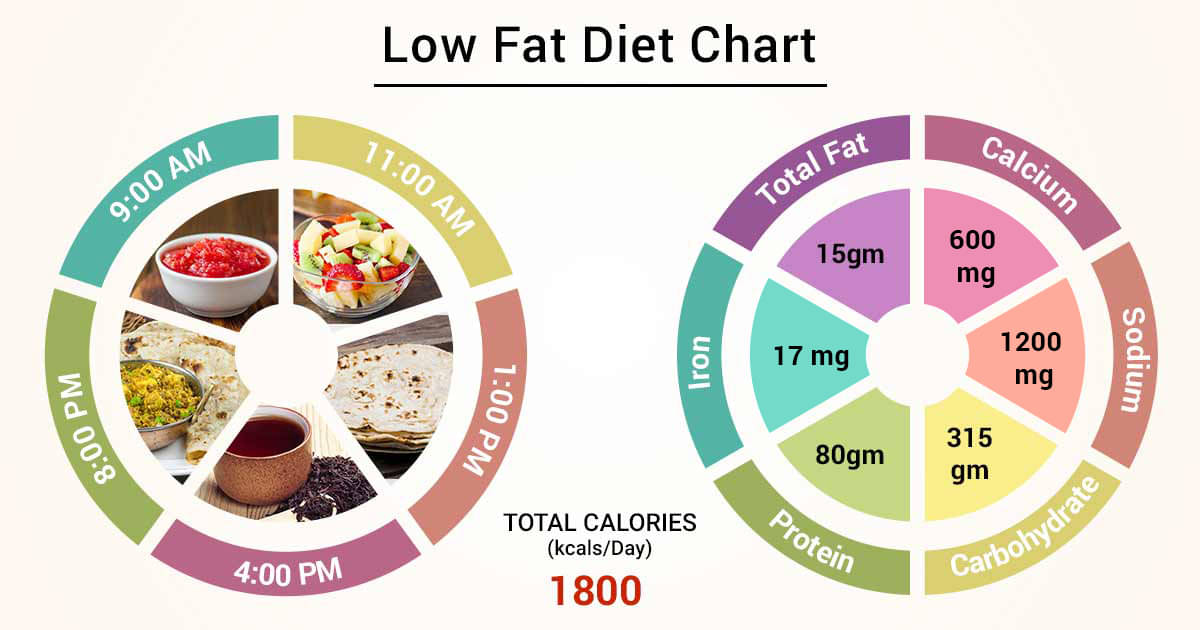
Eat healthily
You're more likely to get indigestion if you're very full.
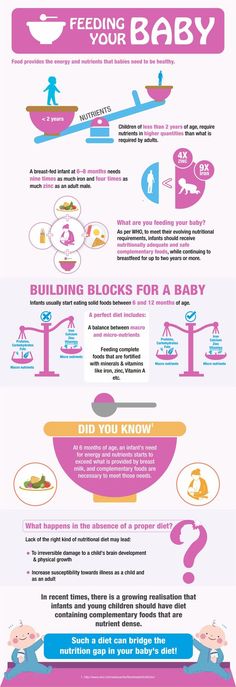
If you're pregnant, it may be tempting to eat more than you would normally, but this may not be good for you or your baby.
Find out more about a healthy diet in pregnancy and foods to avoid.
Change your eating and drinking habits
You may be able to control your indigestion with changes to your eating habits.
It can help to eat small meals often, rather than larger meals 3 times a day, and to not eat within 3 hours of going to bed at night.
Cutting down on drinks containing caffeine, and foods that are rich, spicy or fatty, can also ease symptoms.
Keep upright
Sit up straight when you eat. This will take the pressure off your stomach. Propping your head and shoulders up when you go to bed can stop stomach acid coming up while you sleep.
Stop smoking
Smoking when pregnant can cause indigestion, and can seriously affect the health of you and your unborn baby.
When you smoke, the chemicals you inhale can contribute to your indigestion. These chemicals can cause the ring of muscle at the lower end of your gullet to relax, which allows stomach acid to come back up more easily. This is known as acid reflux.
Smoking also increases the risk of:
- your baby being born prematurely (before week 37 of your pregnancy)
- your baby being born with a low birthweight
- sudden infant death syndrome (SIDS), or "cot death"
There's lots of help available to stop smoking. Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Avoid alcohol
Drinking alcohol can cause indigestion. During pregnancy, it can also lead to long-term harm to the baby. It's safest to not drink alcohol at all in pregnancy.
Find out more about alcohol and pregnancy
When to get medical help
See your midwife or GP if you need help managing your symptoms or if changes to your diet and lifestyle do not work. They may recommend medicine to ease your symptoms.
You should also see your midwife or GP if you have any of the following:
- difficulty eating or keeping food down
- weight loss
- stomach pains
Your midwife or GP may ask about your symptoms and examine you by pressing gently on different areas of your chest and stomach to see whether it's painful.
If you're taking prescription medicines
Speak to your GP if you're taking medicine for another condition, such as antidepressants, and you think it may be making your indigestion worse. They may be able to prescribe an alternative medicine.
Never stop taking a prescribed medicine unless you're advised to do so by your GP or another qualified healthcare professional who's responsible for your care.
Medicines for indigestion and heartburn
Medicines for indigestion and heartburn during pregnancy include:
- antacids – to neutralise the acid in your stomach (some are available over the counter from a pharmacist)
- alginates – to relieve indigestion caused by acid reflux by stopping the acid in your stomach coming back up your gullet
You may only need to take antacids and alginates when you start getting symptoms. However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
If you're taking iron supplements as well as antacids, do not take them at the same time. Antacids can stop iron from being absorbed by your body.
If antacids and alginates do not improve your symptoms, your GP may prescribe a medicine to reduce the amount of acid in your stomach. 2 that are widely used in pregnancy and not known to be harmful to an unborn baby are:
- ranitidine – a tablet you take twice a day
- omeprazole – a tablet you take once a day
Causes of indigestion in pregnancy
Symptoms of indigestion come when the acid in your stomach irritates your stomach lining or your gullet. This causes pain and a burning feeling.
When you're pregnant, you're more likely to have indigestion because of:
- hormonal changes
- the growing baby pressing on your stomach
- the muscles between your stomach and gullet relaxing, allowing stomach acid to come back up
You may be more likely to get indigestion in pregnancy if:
- you had indigestion before you were pregnant
- you've been pregnant before
- you're in the later stages of pregnancy
Video: Eating well on a budget
In this video, a dietitian gives advice on how to eat healthily on a budget.
Media last reviewed: 13 January 2021
Media review due: 13 January 2024
Gastroesophageal Reflux Disease (GERD) and Heartburn During Pregnancy
Written by WebMD Editorial Contributors
Medically Reviewed by Nivin Todd, MD on August 26, 2022
In this Article
- Symptoms of Heartburn During Pregnancy
- Causes of Heartburn During Pregnancy
- Prevention of Heartburn During Pregnancy
- Treatment of Heartburn During Pregnancy
- Heartburn Medication to Avoid During Pregnancy
More than half of pregnant women get serious heartburn, particularly during their second and third trimesters. Heartburn, also called acid indigestion, is an irritation or burning sensation of the esophagus (the tube that carries food and liquid to your stomach when you swallow). It’s caused by stomach contents that reflux (come back up).
Symptoms of Heartburn During Pregnancy
If you have heartburn while you’re pregnant, you may:
- Feel burning or pain in your chest or throat, especially after you eat
- Have sensations of fullness, heaviness, or bloating
- Burp or belch
- Have a sour or bitter taste in your mouth
- Cough or have sore throat
Causes of Heartburn During Pregnancy
Heartburn in pregnancy may happen because of changing hormone levels, which can affect the muscles of the digestive tract.
Pregnancy hormones can cause your lower esophageal sphincter (the muscular valve between the stomach and esophagus) to relax, allowing stomach acids to flow back up into your esophagus. Also, as your baby grows, your enlarged uterus can crowd the abdomen, pushing stomach acids upward. Although it's rare, gallstones can also cause heartburn during pregnancy.
Prevention of Heartburn During Pregnancy
Some tips that may help you cut down on heartburn during your pregnancy include:
- Eat several small meals each day instead of three large ones.
- Eat slowly.
- Avoid fried, spicy, or rich (fatty) foods or any foods that seem to cause relaxation of the lower esophageal sphincter and increase the risk of heartburn.
- Don’t smoke tobacco or drink alcohol, which can make heartburn symptoms worse.
- Drink less while eating. Drinking large amounts while eating may increase the risk of acid reflux and heartburn.
- Don't lie down directly after eating.

- Keep the head of your bed higher than the foot of your bed. Or place pillows under your shoulders to help prevent stomach acids from rising into your esophagus.
- Wear loose-fitting clothing. Tight-fitting clothes can increase the pressure on your stomach and abdomen.
- Try to avoid constipation.
Treatment of Heartburn During Pregnancy
If your heartburn won’t go away, see your doctor. They may prescribe or recommend OTC medications that are safe to take during pregnancy. Heartburn usually disappears following childbirth.
Medications may include:
Over-the-counter antacids such as calcium carbonate or magnesium hydroxide. These are generally safe to use during pregnancy. You may find that liquid heartburn relievers are more effective in treating heartburn, because they coat the esophagus.
h3 blockers. These medications block chemical signals that produce stomach acid. They include cimetidine (Tagamet) and famotidine (Pepcid, Zantac 360), and they’re available in over the counter and prescription strengths.
Proton pump inhibitors (PPIs). Like h3 blockers, these drugs help cut down on stomach acid. PPIs, which include lansoprazole (Prevacid) and omeprazole (Prilosec), are available over the counter and by prescription.
If you take iron supplements, talk to your doctor before you take a PPI or h3 blocker. These medications can make the supplements less effective.
Heartburn Medication to Avoid During Pregnancy
Talk to your doctor before taking any antacids. Some contain ingredients that may harm you or your baby. Be sure to not to take these medications:
Ranitidine. In 2020, the FDA stopped sales of an h3 blocker called ranitidine (the ingredient in older Zantac products) because it was contaminated with a cancer-causing agent. If you take OTC ranitidine, stop your use. If you have a prescription for ranitidine, talk to your doctor about other options before you stop your medication.
Heartburn / GERD Guide
- Overview & Facts
- Symptoms & Complications
- Diagnosis & Tests
- Treatment & Care
- Living & Managing
Acid related diseases in pregnancy | Rassvet Clinic
Heartburn during pregnancy is a very common complaint. It is known that up to 80% of pregnant women experience symptoms characteristic of gastroesophageal reflux disease (GERD) (heartburn, dysphagia, belching, and others), and the frequency of heartburn in the first trimester is 7.2%, in the second - 18.2%, in the third - 40%.
It is known that up to 80% of pregnant women experience symptoms characteristic of gastroesophageal reflux disease (GERD) (heartburn, dysphagia, belching, and others), and the frequency of heartburn in the first trimester is 7.2%, in the second - 18.2%, in the third - 40%.
The main factors behind this high prevalence of GERD in pregnancy include hormonal changes such as hyperprogesteronemia (increased levels of the hormone progesterone) and hyperestrogenemia (increased levels of estrogen hormones), as well as increased intra-abdominal pressure due to uterine and fetal growth.
The action of gestational hormones in the first trimester of pregnancy is due to the fact that they, without affecting the basal tone of the lower esophageal sphincter (LES), reduce the increase in pressure of this sphincter in response to a variety of physiological stimuli, including food intake. In the second and third trimesters of pregnancy, progesterone and estrogen reduce the basal tone of the LES to 50% of the initial level, the maximum decrease occurs at 36 weeks of gestation. After a successful delivery, the tone of the LES in women who did not suffer from GERD before pregnancy, as a rule, returns to normal - in connection with this, this condition is called "pregnancy heartburn."
After a successful delivery, the tone of the LES in women who did not suffer from GERD before pregnancy, as a rule, returns to normal - in connection with this, this condition is called "pregnancy heartburn."
Pregnancy heartburn usually does not lead to the development of esophagitis, complications of GERD (strictures, ulcers, bleeding) and does not require serious medical treatment.
If a woman had GERD before pregnancy, the complaints may worsen during pregnancy and require examination and medication.
The diagnosis of GERD during pregnancy is established primarily on the basis of complaints, anamnesis data and objective examination. X-ray examination in pregnant women - due to possible damaging effects on the fetus - is not used, pH-metry and manometry can be used, but the need for its use is doubtful.
Esophagogastroduodenoscopy (EGD) is the method of choice for diagnosing GERD in pregnant women, but it should only be used for strict indications, such as a history of complications of GERD and the ineffectiveness of ongoing drug therapy.
Treatment of GERD in pregnant women should be based on changes in lifestyle and nutrition: exclusion of a horizontal position of the body immediately after meals, sleeping with the head end of the bed elevated (by 15 cm), exclusion of physical activity that increases intra-abdominal pressure (including wearing corsets, tight belts, bandages). The last meal should take place no later than 3 hours before bedtime, you need to eat in small portions, pay special attention to the normalization of the stool.
First-line drugs for the treatment of GERD in pregnant women include antacids and alginates. With the ineffectiveness of these drugs, it is permissible to prescribe prokinetics (metoclopramide), blockers of histamine h3 receptors and (according to strict indications) proton pump inhibitors (PPIs).
H2-histamine blockers are the most commonly prescribed group of drugs for pregnant women. They are classified as risk category B by the US Food and Drug Administration (FDA) ( "drugs taken by a limited number of pregnant women without evidence of their effect on the incidence of congenital anomalies or damaging effects on the fetus") . In Russian instructions, only cimetidine and ranitidine are allowed with a caveat: use during pregnancy is possible only if the expected effect of therapy outweighs the potential risk to the fetus. Famotidine and nizatidine in the Russian Federation are contraindicated for pregnant women.
In Russian instructions, only cimetidine and ranitidine are allowed with a caveat: use during pregnancy is possible only if the expected effect of therapy outweighs the potential risk to the fetus. Famotidine and nizatidine in the Russian Federation are contraindicated for pregnant women.
Although most PPIs are also classified by the FDA as risk category B, in Russia there are more stringent restrictions on the use of this group of drugs in pregnant women. So, lansoprazole is contraindicated in the first trimester, in the second and third trimesters it can be used only if the expected benefit of therapy outweighs the potential risk to the fetus. The use of pantoprazole and esomeprazole is possible only under strict indications, when the benefit to the mother outweighs the potential risk to the fetus. Rabeprazole during pregnancy is contraindicated.
Pregnancy has a beneficial effect on the course of peptic ulcer disease: 75-80% of women experience remission of the disease, and it does not have a noticeable effect on its outcome. However, some patients may experience an exacerbation. This is most often observed in the first trimester of pregnancy (14.8%) and the third trimester (10.2%), as well as 2-4 weeks before the due date or in the early postpartum period. Uncomplicated peptic ulcer does not adversely affect the development of the fetus.
However, some patients may experience an exacerbation. This is most often observed in the first trimester of pregnancy (14.8%) and the third trimester (10.2%), as well as 2-4 weeks before the due date or in the early postpartum period. Uncomplicated peptic ulcer does not adversely affect the development of the fetus.
Treatment of peptic ulcer in pregnant women includes adherence to generally accepted "regime" measures and diet; taking in the usual therapeutic doses of non-absorbable antacids (1 sachet 3 times a day 1 hour after meals and adsorbents 1 sachet 3 times a day 1 hour after meals). If there is no effect, h3-blockers are prescribed (ranitidine 150/300 mg once a night), in case of their insufficient effectiveness, as well as with the development of complications, we can take PPIs (omeprazole 20-40 mg, lansoprazole 30-60 mg, pantoprazole 40 mg). mg in the morning before the first meal). Bismuth preparations are contraindicated for pregnant women. Eradication therapy for H. pylori infection in pregnant women is not carried out.
pylori infection in pregnant women is not carried out.
Author:
Kaibysheva Valeria Olegovna
Gastroenterologist Ph.D.
GERD during pregnancy - causes, symptoms, diagnosis and treatment
GERD during pregnancy is an acid-dependent disease of the esophagus caused by damage to the mucosa during reflux of stomach contents, which has arisen or aggravated under the influence of gestational factors. Manifested by heartburn, sour eructation, odynophagia, less often - nausea, vomiting, dysphagia, epigastric pain, cough, dysphonia, hypersalivation in sleep, taste perversions, depressed mood. It is diagnosed using alkaline and omeprazole tests, esophagoscopy, pH-metry, manometry. For treatment, alginates, antacids, selective histamine blockers, drugs that inhibit the proton pump, prokinetics are used.
General information
GERD (gastroesophageal reflux disease, gastroesophageal reflux) is one of the most common diseases of the gastrointestinal tract, contributing to such a common symptom as pregnancy heartburn. According to the observations of specialists in the field of obstetrics and gynecology, from 30 to 95% of patients during the period of bearing a child experience heartburn, which some experts even consider a natural manifestation of pregnancy. In 21-80% of patients suffering from GERD, the disease debuted precisely in connection with gestation.
According to the observations of specialists in the field of obstetrics and gynecology, from 30 to 95% of patients during the period of bearing a child experience heartburn, which some experts even consider a natural manifestation of pregnancy. In 21-80% of patients suffering from GERD, the disease debuted precisely in connection with gestation.
Women who have given birth more than once are more susceptible to the disease. The relevance of timely detection of gastroesophageal reflux is due to a significant deterioration in the quality of life of a pregnant woman and the need to prescribe pharmacotherapy to almost half of the patients.
GERD during pregnancy
Causes
Gastroesophageal reflux of acidic gastric contents develops when the cardiac sphincter is weakened, the motility of the esophagus and stomach is impaired, gastric secretion is increased, and the protective properties of the esophageal mucosa are reduced. The occurrence of GERD is promoted by congenital and acquired hernia of the esophageal opening of the diaphragm with displacement into the posterior mediastinum of the abdominal esophagus, part or all of the stomach, smoking, dietary errors, and obesity.
Nitrates, antidepressants, progestins, anticholinergics, calcium channel blockers, and other medications that cause transient relaxation of the esophageal sphincter play a role. Specialists in the field of modern gastroenterology consider pregnancy as a separate prerequisite for the development of gastroesophageal reflux disease. The high incidence of GERD during gestation is associated with the action of factors such as:
- Progesterone increase . Under the action of progestins, the lower esophageal sphincter relaxes, the tone of which is restored only in the postpartum period. By reducing the tone of smooth muscle fibers and reducing the sensitivity of intestinal receptors to histamine and serotonin, physiological hyperprogesteronemia slows down gastrointestinal motility and impairs gastric emptying. As a result, reflux occurs more frequently.
- Increased intra-abdominal pressure . During pregnancy, the relative position of the internal organs of the abdominal cavity is disturbed, which is associated with the development of the fetus and the growth of the uterus.
 When the stomach is displaced towards the diaphragm, evacuation stagnation of its contents is formed faster and the risk of diaphragmatic hernia formation increases. The factor of increasing intra-abdominal pressure is most significant in carrying multiple pregnancies and large fetuses.
When the stomach is displaced towards the diaphragm, evacuation stagnation of its contents is formed faster and the risk of diaphragmatic hernia formation increases. The factor of increasing intra-abdominal pressure is most significant in carrying multiple pregnancies and large fetuses.
Pathogenesis
The mechanism of GERD development during pregnancy is based on the reflux of aggressive stomach contents into the lower esophagus. Gastroesophageal reflux usually occurs when the pressure of the cardiac sphincter is less than 2 mm Hg. Art. or an increase in intragastric pressure of more than 5 mm Hg. Art. Both of these factors are found in pregnant women. Refluxate containing hydrochloric acid, pepsin, and in some cases bile acids, has an irritating effect on the epithelium of the esophagus, causes a local inflammatory reaction, and in some patients provokes the onset of erosive processes.
Classification
When systematizing the forms of GERD in pregnant women, the same criteria are taken into account as outside the gestational period - the nature of the course of the disease and the condition of the esophageal mucosa.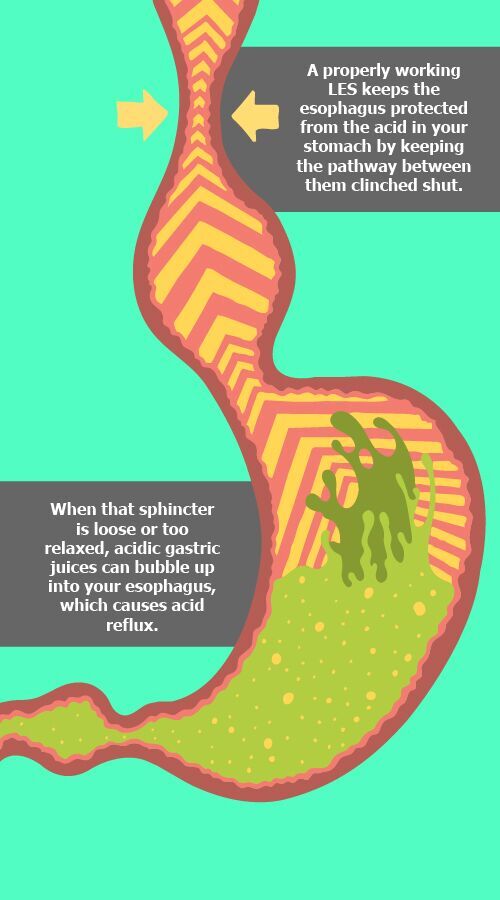 This approach makes it possible to develop optimal medical tactics aimed at eliminating clinical symptoms and the morphological basis of their occurrence without the risk of negative effects on the fetus. Depending on the time of existence of the disorder, acute gastroesophageal reflux disease is distinguished, lasting up to 3 months, and a chronic process that exists for 3 months or more. Taking into account the characteristics of damage to the mucosa of the esophagus, such forms of GERD are distinguished as:
This approach makes it possible to develop optimal medical tactics aimed at eliminating clinical symptoms and the morphological basis of their occurrence without the risk of negative effects on the fetus. Depending on the time of existence of the disorder, acute gastroesophageal reflux disease is distinguished, lasting up to 3 months, and a chronic process that exists for 3 months or more. Taking into account the characteristics of damage to the mucosa of the esophagus, such forms of GERD are distinguished as:
- Gastroesophageal reflux without esophagitis . With a non-erosive variant of the disorder, detected in 55-70% of patients, there are no endoscopic signs of damage to the epithelium. Although the likelihood of complications in this case is lower, the patient's quality of life deteriorates in the same way as in the presence of erosions.
- Reflux esophagitis . In 30-45% of pregnant women with GERD during endoscopy, visible signs of esophagitis caused by the aggressive action of the contents of the stomach are determined.
 In the erosive form of gastroesophageal reflux, acute and long-term consequences of the disease are more often observed.
In the erosive form of gastroesophageal reflux, acute and long-term consequences of the disease are more often observed.
When predicting the outcome of GERD in a pregnant woman, the severity of the endoscopically positive variant of the disease according to the Los Angeles classification is also taken into account. The most favorable during pregnancy is reflux esophagitis A and B degrees, in which the defects extend to 1-2 folds of the mucosa, and their sizes, respectively, are up to or more than 5 mm. With C degree of GERD, less than 75% of the esophageal circumference is affected, and with D - 75% or more, which significantly increases the likelihood of a complicated course.
Symptoms of GERD during pregnancy
75% of patients with gastroesophageal reflux complain of heartburn, which gradually increases as labor approaches. Discomfort and burning behind the sternum often occur after eating spicy, fatty, fried foods, overeating, exercise, lying down and bending over. Heartburn attacks can recur several times a day and last from minutes to several hours. Pregnant women suffering from GERD may experience sour or bitter belching, sensation of a lump in the throat, retrosternal pain when swallowing with irradiation to the precordial region, neck, lower jaw, interscapular space.
Heartburn attacks can recur several times a day and last from minutes to several hours. Pregnant women suffering from GERD may experience sour or bitter belching, sensation of a lump in the throat, retrosternal pain when swallowing with irradiation to the precordial region, neck, lower jaw, interscapular space.
Sometimes in the II-III trimesters, nausea and vomiting are noted, it is extremely rare to swallow solid and then liquid food. Extra-esophageal manifestations of reflux disease during pregnancy are a feeling of fullness in the epigastrium, rapid satiety, repeated attacks of coughing and suffocation, a hoarse voice, sore throat, increased salivation during sleep, burning cheeks and tongue, taste perversion, bad breath. Often, pregnant women experience a sad, depressed mood. Rarely, GERD is asymptomatic.
Complications
Usually, gastroesophageal reflux does not cause any obstetric complications, however, with extensive erosive damage to the esophagus, more severe anemia in pregnant women may develop.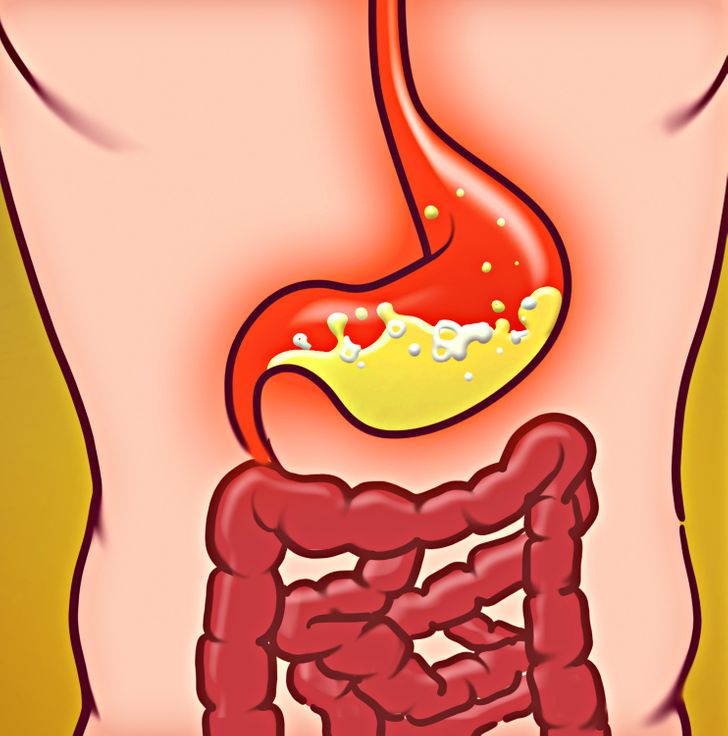 In two thirds of patients, GERD worsens during pregnancy: in 10-11% of cases, a relapse occurs in the 1st trimester, aggravated by early toxicosis, in 33-34% - in the 2nd trimester, and in more than half of pregnant women - in the 3rd.
In two thirds of patients, GERD worsens during pregnancy: in 10-11% of cases, a relapse occurs in the 1st trimester, aggravated by early toxicosis, in 33-34% - in the 2nd trimester, and in more than half of pregnant women - in the 3rd.
Rare specific complications that occur against the background of physiological immunodeficiency during pregnancy are acute esophagitis caused by candidal and herpes infections. There is a risk of ulceration of the mucosa with the development of esophageal bleeding. Long-term consequences of reflux disease are narrowing (strictures) of the esophagus, dysplasia and metaplasia of the epithelium (Barrett's esophagus) and esophageal adenocarcinoma.
Diagnosis
During pregnancy, the diagnosis of GERD is usually made on the basis of typical clinical symptoms with daily occurrence of heartburn. An obstetrician-gynecologist and a gastroenterologist are involved in the diagnosis. Instrumental methods traditionally used in the diagnosis of the disease are used to a limited extent in pregnant women due to the possible provocation of preterm labor and the aggravation of other complications (nephropathy, early toxicosis, preeclampsia, eclampsia).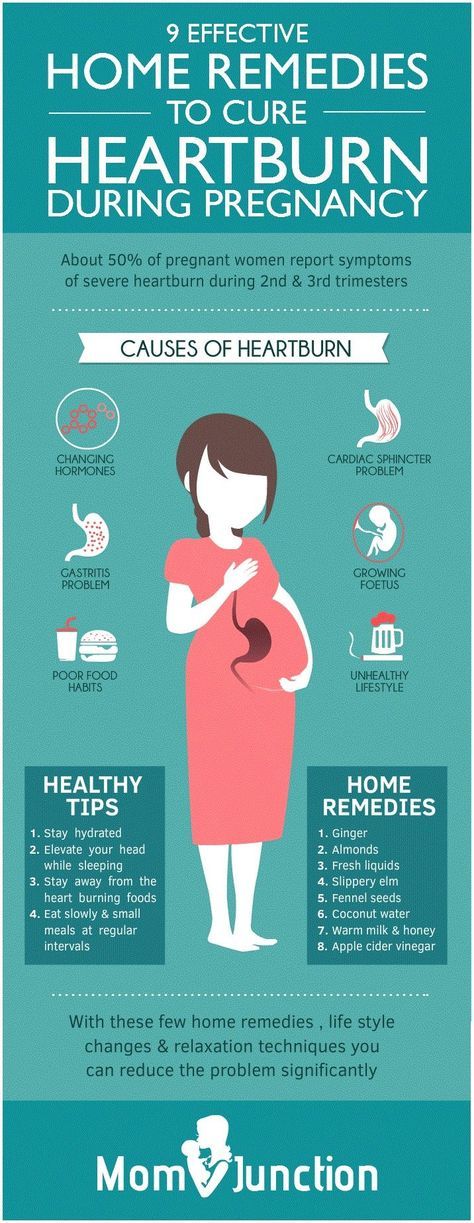 Recommended for diagnostic purposes:
Recommended for diagnostic purposes:
- Alkaline test . Reception of absorbable antacids quickly stops an attack of heartburn. The positive effect of alkaline preparations is associated with the neutralization of hydrochloric acid coming from the stomach into the esophagus. In the presence of extraesophageal manifestations, the study is supplemented with an omeprazole test aimed at eliminating symptoms by inhibiting gastric secretion.
- Esophageal Endoscopy . Esophagoscopy is performed if extensive erosion, ulceration, esophageal bleeding, strictures are suspected, and neoplasia can be ruled out. In endoscopic examination, GERD is manifested by swelling and slight vulnerability of the esophageal mucosa, it is possible to identify areas of damaged epithelium. In some cases, it is possible to visualize the reflux of gastric juice.
- Intraesophageal pH-metry. The method is effective in non-erosive forms of gastroesophageal reflux.
 Electrometric determination of the acidity of the contents of the esophagus is carried out using a flexible intraesophageal probe attached to an acidogastrometer. pH-metry allows you to identify episodes of reflux of gastric juice and determine the conditions for their occurrence.
Electrometric determination of the acidity of the contents of the esophagus is carried out using a flexible intraesophageal probe attached to an acidogastrometer. pH-metry allows you to identify episodes of reflux of gastric juice and determine the conditions for their occurrence. - Manometry . Registration of pressure in different parts of the gastrointestinal tract using special catheters with strain gauges verifies the weakening of the cardiac sphincter and dysmotility. A manometric study also provides an objective assessment of elasticity, tone, contractile activity of the esophageal wall, and pressure profiling in the esophagus.
If necessary, the examination is supplemented with gastrocardiomonitoring, gastrointestinal impedancemetry, bilemetry. X-ray studies of the esophagus during pregnancy are not performed. GERD is differentiated from functional dyspepsia, gastric and duodenal ulcers, acute infectious esophagitis, benign tumors and esophageal cancer. If extraesophageal symptoms are detected, differential diagnosis with angina pectoris, bronchial asthma may be required.
If extraesophageal symptoms are detected, differential diagnosis with angina pectoris, bronchial asthma may be required.
Treatment of GERD during pregnancy
Therapeutic tactics are aimed at the rapid elimination of clinical symptoms, restoration of the esophageal mucosa, prevention of complications and relapses. In 25% of cases, the condition can be improved by non-drug methods. Pregnant women with mild GERD are recommended to stop smoking, correct diet and diet with frequent small meals, reduce the amount of high-protein and low-lipid foods, and exclude citrus juices, chocolate, caffeine-containing drinks, spices, mint, and alcohol.
Caution is required when using drugs that transiently reduce cardiac tone. Efficient sleep with a raised headboard, chewing chewing gum with calcium carbonate. Identification of severe clinical symptoms requires the appointment of special drug therapy. During pregnancy, some of the drugs used in standard treatment regimens for gastroesophageal reflux are used with caution due to possible effects on the fetus or the occurrence of obstetric complications. Patients with severe GERD are shown:
Patients with severe GERD are shown:
- Nonabsorbable antacids and alginates . Considered 1st line drugs for the treatment of gastroesophageal reflux disease in pregnant women. By neutralizing hydrochloric acid, reducing the digestive capacity of pepsin, adsorbing lysolecithin, bile acids, improving the evacuation of stomach contents, stimulating the secretion of prostaglandins, antacids reduce the damaging effect of refluxate. Alginates have a protective effect on the esophageal mucosa.
- Histamine 2-receptor blockers H . They are used when antacid therapy for GERD is ineffective. The antisecretory activity of selective histamine blockers is due to the action on the receptors of the parietal cells of the stomach. Due to inhibition of secretion, the acidity and volume of gastric contents decrease, which helps to reduce its aggressiveness and pressure on the cardiac sphincter. The effect of h3-histamine blockers on the fetus is not well understood, which limits their use.

- Proton pump inhibitors . High efficiency and rapid achievement of therapeutic results in the appointment of PPIs are based on blocking the secretion of hydrochloric acid at the level of the secretory tubules of parietal cells. The limited use of pump inhibitors is due to a decrease in the bactericidal properties of gastric juice, which, against the background of natural suppression of immunity, contributes to the development of food infections and impaired calcium absorption, which is necessary for the normal course of gestation.
Gastrointestinal motility prokinetics and herbal coating preparations can be used as adjunctive agents. During gestation, surgical treatment of severe and complicated forms of GERD is not performed. Pregnancy is recommended to be completed by natural childbirth at a physiological time. Caesarean section is performed when obstetric indications are identified.
Prognosis and prevention
When adequate treatment is prescribed, the damaged esophageal mucosa usually fully recovers in 4-12 weeks, with non-erosive variants of the disease, improvement occurs within 4-10 days.