40 weeks pregnant inducing labor
Labor induction - Mayo Clinic
Overview
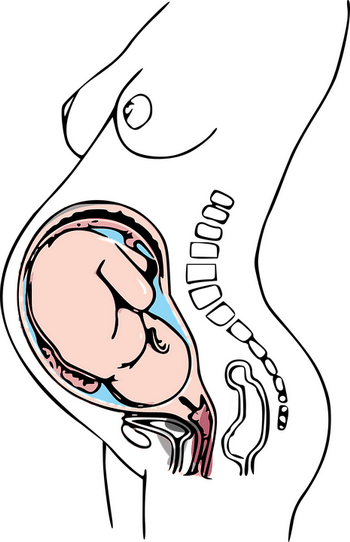
Labor induction — also known as inducing labor — is prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
A health care provider might recommend inducing labor for various reasons, primarily when there's concern for the mother's or baby's health. An important factor in predicting whether an induction will succeed is how soft and expanded the cervix is (cervical ripening). The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
If a health care provider recommends labor induction, it's typically because the benefits outweigh the risks. If you're pregnant, understanding why and how labor induction is done can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
To determine if labor induction is necessary, a health care provider will likely evaluate several factors. These include the mother's health and the status of the cervix. They also include the baby's health, gestational age, weight, size and position in the uterus. Reasons to induce labor include:
- Nearing 1 to 2 weeks beyond the due date without labor starting (postterm pregnancy).
- When labor doesn't begin after the water breaks (prelabor rupture of membranes).
- An infection in the uterus (chorioamnionitis).
- When the baby's estimated weight is less than the 10th percentile for gestational age (fetal growth restriction).
- When there's not enough amniotic fluid surrounding the baby (oligohydramnios).
- Possibly when diabetes develops during pregnancy (gestational diabetes), or diabetes exists before pregnancy.
- Developing high blood pressure in combination with signs of damage to another organ system (preeclampsia) during pregnancy. Or having high blood pressure before pregnancy, developing it before 20 weeks of pregnancy (chronic high blood pressure) or developing the condition after 20 weeks of pregnancy (gestational hypertension).

- When the placenta peels away from the inner wall of the uterus before delivery — either partially or completely (placental abruption).
- Having certain medical conditions. These include heart, lung or kidney disease and obesity.
Elective labor induction is the starting of labor for convenience when there's no medical need. It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
A scheduled induction might help avoid delivery without help. In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
As a result of recent studies, women with low-risk pregnancies are being offered labor induction at 39 to 40 weeks. Research shows that inducing labor at this time reduces several risks, including having a stillbirth, having a large baby and developing high blood pressure as the pregnancy goes on. It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Risks
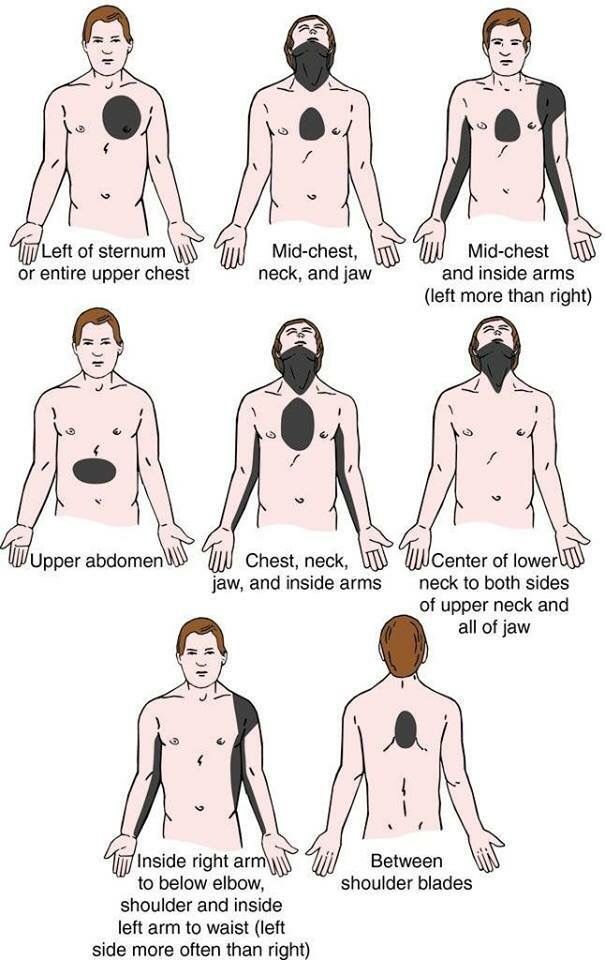
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
Labor induction carries various risks, including:
- Failed induction. An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary.
- Low fetal heart rate. The medications used to induce labor — oxytocin or a prostaglandin — might cause the uterus to contract too much, which can lessen the baby's oxygen supply and lower the baby's heart rate.

- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both mother and baby. The longer the time between membrane rupture and labor, the higher the risk of an infection.
-
Uterine rupture. This is a rare but serious complication in which the uterus tears along the scar line from a prior C-section or major uterine surgery. Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.
An emergency C-section is needed to prevent life-threatening complications. The uterus might need to be removed.
- Bleeding after delivery. Labor induction increases the risk that the uterine muscles won't properly contract after giving birth, which can lead to serious bleeding after delivery.
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a classical incision or major uterine surgery
- The placenta is blocking the cervix (placenta previa)
- Your baby is lying buttocks first (breech) or sideways (transverse lie)
- You have an active genital herpes infection
- The umbilical cord slips into the vagina before delivery (umbilical cord prolapse)
If you have had a C-section and have labor induced, your health care provider is likely to avoid certain medications to reduce the risk of uterine rupture.
How you prepare
Labor induction is typically done in a hospital or birthing center. That's because mother and baby can be monitored there, and labor and delivery services are readily available.
What you can expect
During the procedure
There are various ways of inducing labor. Depending on the circumstances, the health care provider might use one of the following ways or a combination of them. The provider might:
-
Ripen the cervix. Sometimes prostaglandins, versions of chemicals the body naturally produces, are placed inside the vagina or taken by mouth to thin or soften (ripen) the cervix. After prostaglandin use, the contractions and the baby's heart rate are monitored.
In other cases, a small tube (catheter) with an inflatable balloon on the end is inserted into the cervix. Filling the balloon with saline and resting it against the inside of the cervix helps ripen the cervix.
- Sweep the membranes of the amniotic sac.
 With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor.
With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor. -
Rupture the amniotic sac. With this technique, also known as an amniotomy, the health care provider makes a small opening in the amniotic sac. The hole causes the water to break, which might help labor go forward.
An amniotomy is done only if the cervix is partially dilated and thinned, and the baby's head is deep in the pelvis. The baby's heart rate is monitored before and after the procedure.
- Inject a medication into a vein. In the hospital, a health care provider might inject a version of oxytocin (Pitocin) — a hormone that causes the uterus to contract — into a vein. Oxytocin is more effective at speeding up labor that has already begun than it is as at cervical ripening.
 The provider monitors contractions and the baby's heart rate.
The provider monitors contractions and the baby's heart rate.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, the induction techniques used and how the body responds to them. It can take minutes to hours.
After the procedure
In most cases, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might require another induction or a C-section.
By Mayo Clinic Staff
Related
Products & Services
Exploring induced labor for full-term pregnancy
You are here
Home » News & Events » NIH Research Matters
August 28, 2018
At a Glance
- A large study found that, for healthy women, inducing labor at full term rather than waiting for natural labor doesn’t increase the risk of major complications for newborns.
- The findings also reverse the notion that inducing labor at full term increases the risk of needing surgical delivery.

The results can help women and their health care providers make more informed decisions about whether to induce labor.monkeybusinessimages/iStock/Thinkstock
Research shows that babies do best when they are born during weeks 39 and 40. A pregnancy is considered full term at 39 weeks, and the due date is 40 weeks. Sometimes a woman with a healthy pregnancy will ask for labor to be induced at 39 or 40 weeks.
Previous studies suggested that inducing labor may increase the risk of needing a cesarean delivery or C-section, which is major surgery. It takes longer to recover from surgery than a vaginal birth. Also, having surgery may increase a woman’s risk of having a C-section in future pregnancies.
NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) funded a large national study to examine the risks and benefits of a woman choosing labor induction at 39 weeks, rather than waiting for labor to begin naturally. The study was led by Dr. William Grobman of Northwestern University. Results were published on August 9, 2018, in the New England Journal of Medicine.
The study was led by Dr. William Grobman of Northwestern University. Results were published on August 9, 2018, in the New England Journal of Medicine.
More than 6,000 healthy women who were pregnant for the first time were enrolled. The investigators randomly assigned about half of the women to have their labor induced during week 39. The other half waited for labor to begin naturally. For women who waited for natural labor and had problems, the health care team intervened with delivery, either by induction or C-section.
The team compared serious health problems and deaths in the two groups of babies. Serious health problems included needing help with breathing, having a seizure, or getting an infection. There was no significant difference between the groups in serious health problems or deaths (4.3% for induced labor and 5.4% for waiting). This finding suggests that induced labor doesn’t put babies at increased risk of health problems.
The researchers did find a significant difference in the proportions of women needing a cesarean delivery (18. 6% for induced labor and 22.2% for waiting). Also, the proportion of women with blood pressure disorders was significantly lower in those who were induced (9.1%) than those who waited for natural labor (14.1%).
6% for induced labor and 22.2% for waiting). Also, the proportion of women with blood pressure disorders was significantly lower in those who were induced (9.1%) than those who waited for natural labor (14.1%).
“Prior to this study, there was concern that induction of labor would increase the chance of cesarean delivery,” says Dr. Uma M. Reddy, an NICHD medical officer and coauthor of the study. “Our analysis suggests that elective induction at 39 weeks is associated with a lower rate of cesarean delivery and does not increase the risk of major complications for newborns.”
“Induction at 39 weeks should not be routine for every woman, but it’s important to talk with their provider and decide if they want to be induced and when,” Grobman says.
Related Links
- Improving Blood Flow in Preterm Infants
- Prenatal Steroids Reduce Brain Injury in Preemies
- Know Your Terms: Full-Term Pregnancy
- Is It Worth It? Reducing Elective Deliveries Before 39 Weeks
- National Child & Maternal Health Education Program
References: Labor Induction versus Expectant Management in Low-Risk Nulliparous Women. Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM, Mallett G, Hill K, Thom EA, El-Sayed YY, Perez-Delboy A, Rouse DJ, Saade GR, Boggess KA, Chauhan SP, Iams JD, Chien EK, Casey BM, Gibbs RS, Srinivas SK, Swamy GK, Simhan HN, Macones GA; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. N Engl J Med. 2018 Aug 9;379(6):513-523. doi: 10.1056/NEJMoa1800566. PMID: 30089070.
Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM, Mallett G, Hill K, Thom EA, El-Sayed YY, Perez-Delboy A, Rouse DJ, Saade GR, Boggess KA, Chauhan SP, Iams JD, Chien EK, Casey BM, Gibbs RS, Srinivas SK, Swamy GK, Simhan HN, Macones GA; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. N Engl J Med. 2018 Aug 9;379(6):513-523. doi: 10.1056/NEJMoa1800566. PMID: 30089070.
Funding: NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
Connect with Us
- Contact Us
- YouTube
- Flickr
40th week of pregnancy - what happens at the fortieth week of pregnancy: nausea, discharge, signs of labor
WHAT HAPPENS
There is very little space in the uterus now, so do not be surprised if the number of movements is reduced. Be sure to listen to every movement of the baby: both excessive activity and complete cessation are not very good signs. Normally, at 40 weeks of pregnancy, in 12 hours you should feel about 10 movements.
Be sure to listen to every movement of the baby: both excessive activity and complete cessation are not very good signs. Normally, at 40 weeks of pregnancy, in 12 hours you should feel about 10 movements.
Like the mother, the baby is preparing for the birth. In order for the process of childbirth to go smoothly, the hormones adrenaline and norepinephrine are produced in the tiny body, which should reduce pain during the passage of the fetus through the birth canal.
By the 39th - 40th week of pregnancy, the baby's blood circulation is established, the digestive system is actively functioning, processing the amniotic fluid and dead skin cells. The meconium formed from them will leave the intestines of the child only after birth. The bones of the skull are still flexible, so that the fetus can pass through the birth canal unhindered.
The 40th week of pregnancy should be the final one, but in practice, only a few women give birth at the expected time. So be patient and wait, continuing to lead a normal life. In any case, very soon you will hug your baby.
In any case, very soon you will hug your baby.
YOUR WELL FEELING
If you have not yet had signs of childbirth, they may appear at the 40th week of pregnancy.
- Lowering of the abdomen. The baby in the uterus moves down and presses the head against the pelvic floor. Due to this, heartburn disappears in the expectant mother and it becomes much easier for her to breathe. But due to the strong pressure on the bladder, pregnant women at this time are forced to go to the toilet more often;
- Disorders of the food system. Approximately 24 to 48 hours before the onset of labor, stool liquefaction may occur;
- Loss of appetite;
- Weight loss. Before childbirth, body weight may decrease by 1 - 2 kg;
- Mucus plug outlet. During 40 weeks of pregnancy, the cork closed the entrance to the cervix, protecting the baby from infections. Her separation (you will learn about this from lumps of mucus on panties) frees the birth canal for the child;
- Amniotic fluid discharge.
 Amniotic fluid is poured out immediately before childbirth. Most often it is transparent, but if meconium particles have got into it, the color may be yellowish or greenish;
Amniotic fluid is poured out immediately before childbirth. Most often it is transparent, but if meconium particles have got into it, the color may be yellowish or greenish; - Painful and false contractions at 40 weeks. Primiparous women can confuse training contractions with real ones, especially since by the time of 39-40 weeks of pregnancy, false uterine contractions are also accompanied by pain and are repeated more often than in previous periods. To understand exactly what kind of contractions you have, change the position of the body during muscle contractions. Lie down or, conversely, stand up, walk around the room, then sit on a chair. If the contractions have stopped, then this is not childbirth.
RISK FACTORS
The main danger of 40 weeks of pregnancy is rapid delivery. A baby can be born very quickly, especially in multiparous women. Therefore, it is better to go to the hospital in advance, about a week before the expected date of birth. And if you live near a hospital, avoid long trips and tiring shopping trips.
At the 40th week of pregnancy, it is necessary to monitor the nature of the discharge. If they have changed their smell, color and texture (for example, they have become purulent or curdled), this indicates an infectious disease that requires immediate treatment. The presence of pathogenic microbes in the vagina creates a risk of infection of the child.
As at any time, anemia is dangerous at 39-40 weeks of gestation, due to which the level of oxygen in the tissues decreases. Low hemoglobin provokes fetal hypoxia, and the expectant mother faces an increased risk of developing late toxicosis and complications in childbirth.
Possible signs of anemia during pregnancy:
- Dry skin;
- Brittle nails and hair;
- Feeling weak and easily fatigued;
- Paleness of skin and mucous membranes;
- Insomnia;
- Headaches;
- Feeling of impending fainting;
- Arrhythmia and bradycardia;
- Constipation;
- Presence of taste perversions.

Anemia is treated with iron supplements and a special diet.
MEDICAL SUPERVISION
At the 40th week of pregnancy, you will have another trip to the doctor, where the usual procedures will be carried out: measuring blood pressure, weighing, determining the height of the fundus of the uterus and, of course, listening to the baby's heartbeat.
And in order to monitor the work of the kidneys, you will need to pass urine for analysis. If the date of delivery, which was set by the doctor, has passed, you may be prescribed a Doppler ultrasound. This study makes it possible to assess the blood flow of the fetus, blood circulation in the placenta and uterine vessels, and also to determine whether the baby receives enough oxygen and necessary substances. Another study, sometimes prescribed at 40 weeks of gestation, is cardiotocography, thanks to which the specialist will be able to exclude intrauterine hypoxia.
RECOMMENDATIONS
In the time remaining before the birth, try to relax properly, because after the birth of the child this is unlikely to work. It is very important to remain calm now, because your emotional state greatly affects the baby. Tune in to the upcoming birth and think only about the good.
It is very important to remain calm now, because your emotional state greatly affects the baby. Tune in to the upcoming birth and think only about the good.
At the 39th - 40th week of pregnancy, you should not experiment with nutrition. Eat foods high in protein and carbohydrates. They will help to accumulate strength and stock up on energy that you will need during childbirth. Don't forget about vitamins. Now the body needs vitamin K (it is found in spinach, in all types of cabbage, in asparagus, herbs, plums and prunes). This element improves blood clotting, which is very important for childbirth. You also need vitamin A, which is found in yellow, red and orange vegetables and fruits, beef liver, egg yolks and full-fat dairy products. Its lack can lead to a lack of baby weight. And at 39– At 40 weeks pregnant, you need B vitamins: they ensure not only the proper development of the fetus, but also the well-being of the mother. Their most valuable source is dry brewer's yeast, but they can be used only after consulting a doctor. Also, B vitamins are present in oatmeal, millet, meat, fish, eggs, legumes and dairy products.
Also, B vitamins are present in oatmeal, millet, meat, fish, eggs, legumes and dairy products.
If at 40 weeks of pregnancy you feel the onset of contractions, do not rush to go to the hospital. Before childbirth, you should replenish energy reserves, and for this you can drink sweet tea, jelly or compote, eat a little low-fat cottage cheese or yogurt. As soon as the duration of the contractions reaches 1 minute, and the interval between them is 5-7 minutes, go to the hospital.
Many future parents are interested in the question of whether it is harmful to have sex at the 39th - 40th week of pregnancy. In the absence of contraindications, this is not prohibited. And in some cases, sexual intercourse is even recommended as a means of preparing for childbirth. The semen contains the hormone prostaglandin, which softens the cervix, and the orgasm experienced by a woman stimulates the onset of contractions.
Pregnancy and childbirthNinth month of pregnancy: changes in the female body and fetal development by week
Newborn careDowry for a newborn
What do you need to have at home for discharge, what stroller and crib to choose, and what equipment to buy?
Pregnancy and childbirthWhat to take with you to the hospital
Pregnancy and childbirthPsychology of pregnancy and motherhood
Positive attitude and overcoming fears during pregnancy, psychological hygiene and well-being of a woman.
How to Prepare for Pregnancy
How to properly organize your life before childbirth and how to choose a maternity hospital.
Communication with a childHow to prepare for the birth of a baby?
How to build a relationship between an older and younger child and what you need to be prepared for.
Breast-feedingAll About Breastfeeding
Let's dispel the most popular misconceptions about breastfeeding.
37-40 weeks of pregnancy
37th week of pregnancy for a baby
At 37 weeks of gestation, the baby is approximately 48 cm tall and weighs 2,600 g. facial features, pronounced cartilage tissue. The accumulation of subcutaneous fat at this stage of pregnancy makes the outline of the body softer and more rounded. The skin of the child is gradually smoothed out, it is no longer as pink as in the previous weeks of intrauterine development, the integument gradually brightens. The body of the baby is still abundantly covered with grease, but the amount of fluff is noticeably reduced, fluff hair remains only on the shoulders and back, in some babies they disappear almost completely.
facial features, pronounced cartilage tissue. The accumulation of subcutaneous fat at this stage of pregnancy makes the outline of the body softer and more rounded. The skin of the child is gradually smoothed out, it is no longer as pink as in the previous weeks of intrauterine development, the integument gradually brightens. The body of the baby is still abundantly covered with grease, but the amount of fluff is noticeably reduced, fluff hair remains only on the shoulders and back, in some babies they disappear almost completely.
Fat accumulation continues this week. It reaches a maximum of 15% of the total body weight of the child. It is difficult to overestimate the importance of adipose tissue for newborns, it is it that protects the child from overheating or hypothermia, since the baby's thermoregulation system after childbirth is still not sufficiently formed and continues to develop in the first months of a small person's life.
At this time, not only the volume of subcutaneous fat increases, but muscles and skeleton also develop intensively. The child constantly moves arms and legs. These unique workouts help increase muscle mass. Also, the baby makes rhythmic respiratory movements that strengthen the intercostal muscles and the diaphragm, and prepare the respiratory organs for childbirth.
The child constantly moves arms and legs. These unique workouts help increase muscle mass. Also, the baby makes rhythmic respiratory movements that strengthen the intercostal muscles and the diaphragm, and prepare the respiratory organs for childbirth.
Pregnant woman at 37 weeks
As the due date approaches, pregnant women begin to notice the appearance of their precursors, that is, certain signs, changes that occur under the influence of hormones. The body of a woman is preparing to give birth to a child, progesterone gives way to the dominant role of the birth hormone estrogen, the state of health of a pregnant woman changes.
From the 37th week, expectant mothers can observe the following changes:
- slight weight loss;
- abdominal shrinkage;
- the appearance of training or "false" contractions and the increase in their intensity;
- discharge of mucus from the cervix.
The nature of the stool changes, it becomes looser, aching pains in the lower back of varying intensity may appear, the fundus of the uterus descends. A woman notes some signs on her own, others are observed by a gynecologist during a routine examination.
Harbingers do not appear in all women. Some expectant mothers notice only some of the above symptoms, while others observe signs of an impending birth not two or three weeks before their date, but just a few hours. Both the appearance of precursors at the 37th week and their absence are a variant of the norm and depend on the individual characteristics of the woman's body.
This week the woman's body is intensified preparation for the birth of a child. If the fetus is located correctly, head down, it gradually descends, goes to the lower part of the uterus, presses to the body and bends the limbs, intuitively taking the most comfortable position for passing the birth canal. The consequence of the movement of the fetus is the omission of the bottom of the uterus. The abdomen drops, the pressure on the diaphragm significantly decreases, the pregnant woman can breathe easily, the shortness of breath that haunted her in previous weeks disappears. The pressure on the stomach also decreases, heartburn disappears, a feeling of heaviness after eating and other unpleasant sensations. Moving the baby can put pressure on the bowels and bladder. A pregnant woman at this time often experiences the urge to urinate, may suffer from frequent loose stools. The reason for frequent bowel movements is not only the mechanical effect of the uterus on it, but also an increase in the content of estrogens in the body, hormones that contribute to the excretion of fluid. At the 37th week, the expectant mother can empty her intestines up to 3-4 times a day and at the same time observe a significant liquefaction of feces.
The pressure on the stomach also decreases, heartburn disappears, a feeling of heaviness after eating and other unpleasant sensations. Moving the baby can put pressure on the bowels and bladder. A pregnant woman at this time often experiences the urge to urinate, may suffer from frequent loose stools. The reason for frequent bowel movements is not only the mechanical effect of the uterus on it, but also an increase in the content of estrogens in the body, hormones that contribute to the excretion of fluid. At the 37th week, the expectant mother can empty her intestines up to 3-4 times a day and at the same time observe a significant liquefaction of feces.
38th week of pregnancy: the development of the future baby
At the 38th week, the fetus is fully formed, so childbirth at this time is no longer dangerous for both the mother and the baby. The weight of the fetus is about 3 kg, but this indicator can vary significantly for different babies, the weight depends on the individual characteristics of the mother and child, the structural features of the body and other factors. The body length of a newborn is approximately 50 cm.
The body length of a newborn is approximately 50 cm.
All organs and systems at 38 weeks of age are characterized by physiological and morphological maturity, they are fully ready for work. At this time, the child prepares for childbirth, makes respiratory movements and prepares the intercostal muscles for breathing. The tissues of the lungs are bathed in amniotic fluid, which helps maintain the right level of surfactant that coats the baby's lungs from the inside. All elements of the respiratory system are ready for use. With the first breath after birth, the alveoli begin to transfer oxygen from the air to the blood, gas exchange occurs, the respiratory and circulatory systems begin to work intensively.
Pregnant woman
The body of a pregnant woman continues to actively prepare for the birth of a baby, the estrogen content rapidly increases, and the progesterone level decreases significantly. A change in the hormonal background contributes to the softening of the tissues of the birth canal and cervix. Throughout pregnancy, the lumen of the cervical canal is closed by a plug of thick mucus, which protects the baby from infection, and the uterine cavity protects against the penetration of microorganisms dangerous to health. In the last weeks of pregnancy, the consistency of the mucus changes, it becomes more liquid and begins to gradually flow out. In some women, mucus leaves gradually, while in other women in labor at the same time. The discharge resembles colorless egg white in its consistency and appearance. Sometimes the mucus is colored pinkish, brown or yellow. The discharge of the cork is painless, a woman may experience a slight feeling of discomfort in the lower abdomen. More abundant vaginal discharge than during the entire pregnancy can signal the passage of the cork.
Throughout pregnancy, the lumen of the cervical canal is closed by a plug of thick mucus, which protects the baby from infection, and the uterine cavity protects against the penetration of microorganisms dangerous to health. In the last weeks of pregnancy, the consistency of the mucus changes, it becomes more liquid and begins to gradually flow out. In some women, mucus leaves gradually, while in other women in labor at the same time. The discharge resembles colorless egg white in its consistency and appearance. Sometimes the mucus is colored pinkish, brown or yellow. The discharge of the cork is painless, a woman may experience a slight feeling of discomfort in the lower abdomen. More abundant vaginal discharge than during the entire pregnancy can signal the passage of the cork.
A woman should carefully monitor the color and volume of discharge, since too much colorless discharge may indicate not only the cork has come off, but also be one of the symptoms of amniotic fluid leakage.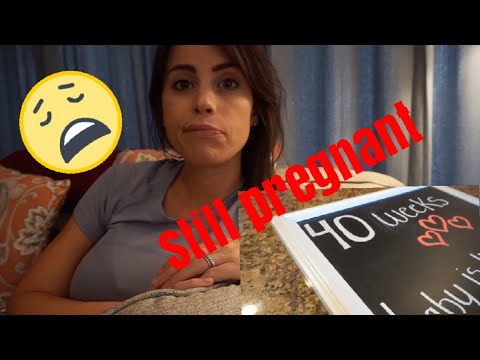 Indicator pads and amnio tests or test strips will help determine the cause of the discharge. Pads are sold in many pharmacies and can be easily used at home. If amniotic fluid leakage is confirmed, you should immediately consult a doctor.
Indicator pads and amnio tests or test strips will help determine the cause of the discharge. Pads are sold in many pharmacies and can be easily used at home. If amniotic fluid leakage is confirmed, you should immediately consult a doctor.
After the mucus plug has passed, you should stop visiting the pool and swimming in open water, as the risk of infection of the child increases significantly. It is also necessary to exclude sexual contact.
39th week of pregnancy: what happens to the fetus?
At 39 weeks, the baby weighs 3100-3500 g and is 50-52 cm tall. Height and weight are very relative and can vary significantly. The baby is rapidly preparing for the most important test of his life - birth, which requires endurance and considerable effort. During this period of pregnancy, the size and weight of the child's adrenal glands, that is, the glands of the endocrine system, which are responsible for the reaction of the human body to stress factors, increase. It is the hormones adrenaline and norepinephrine produced by the adrenal glands that help the child quickly adapt to new temperature conditions, tactile, sound and light impulses.
All the senses of the baby are developed at 39 weeks. Within a few moments after birth, the baby can focus his eyes, he reacts to bright light and moving objects, many scientists claim that newborns distinguish colors, see the faces of parents and doctors. The hearing of the baby in the last weeks of fetal life is also fully developed; after birth, he reacts to loud sounds and noise. A newborn baby is able to determine the main shades of taste, recognize sour, bitter, sweet and salty.
In the womb, the baby is in an aquatic environment that minimizes contact. Immediately after birth, the baby experiences many tactile sensations, unlike intrauterine life, he feels the touch of his mother's hands and diapers, towels, dressings and other materials. Babies especially like the touch of skin to skin, so in a modern maternity hospital, newborns must be laid out on their mother's stomach even before cutting the umbilical cord. The child adapts to the new environment more easily, feels protected. Laying out a child has not only a psychological aspect, since it contributes to the colonization of microorganisms from the mother's skin to the skin and mucous membranes of the baby, and increases its immunity.
Laying out a child has not only a psychological aspect, since it contributes to the colonization of microorganisms from the mother's skin to the skin and mucous membranes of the baby, and increases its immunity.
Pregnant woman
In the last weeks of pregnancy, the expectant mother strives to prepare her apartment or house as much as possible for the arrival of a new family member. Scientists call this sign of impending birth the nesting syndrome. Many women observe signs of the syndrome from the thirtieth week of pregnancy, however, nesting reaches its maximum point at the 39-40th week. Pregnant women tend to do general cleaning and repairs, re-paste the wallpaper and purchase a lot of new things that, in their opinion, are simply necessary in the house. After giving birth, many purchases are puzzling. The reason for this behavior is an increase in the level of adrenaline and norepinephrine in the body. These hormones are produced by the adrenal glands, they are necessary not only for the woman, but also for the baby to prepare for the upcoming birth.
40th week of pregnancy: how does the baby develop?
40 weeks - term pregnancy. The weight of a child who was born at such a period ranges from 2,600 g to 4,400 g, and his body length is 48-53 cm. These indicators are very arbitrary, since miniature babies weighing 2,600 g and real heroes are born at 40 weeks, whose body weight approaches 5,000 g. The length of the newborns can also vary from 45 to 55 cm.
Most women give birth exactly at 40 weeks. At this time, the baby is completely ready for birth, it meets all the parameters of a full-term baby. Before childbirth, the child closely presses the arms and legs to the body, bends the head as much as possible and presses against the exit from the uterus. This position allows you to make it possible to pass the birth canal with the narrowest part of the skull. In the course of labor, with each contraction, the child gradually moves down, he does not move in a straight line, but makes helical-translational movements, as if screwing into the mother's birth canal. During the progress of the newborn, the complete descent of his head, the cervix fully opens. This is followed by attempts, that is, contractions of the uterus, which advance the child through the birth canal. Gradually, the head of the baby is shown, and after it - his torso. Childbirth is a complex mechanism that is aimed not only at the safe passage of the birth canal by the child, protecting him from accidental injuries due to increased pressure, but also at preventing ruptures of the woman's soft tissues.
Pregnant woman
The long wait for meeting her unborn child is coming to an end, and the 40th week of pregnancy is the last for most women. Every day, the anxiety of the expectant mother increases, a long wait affects the mood and well-being. Women strive to have a baby as soon as possible so that pregnancy and painful contractions are a thing of the past. Every pregnant woman dreams of meeting a baby, wants to hug him to her chest and stroke the delicate head.
Many women, especially primiparas, are afraid that labor will begin unnoticed, but such cases are extremely rare.