26 week check up
The Second Trimester of Pregnancy: Checkups and Tests
Just as you’ve had regular visits to your healthcare provider in your first trimester, you’ll continue to do so in your second trimester. These checkups help monitor the development and health of your baby — and your health as well.
Most pregnant people see their doctors every month for a prenatal checkup. You may see your doctor more often if you have a preexisting health condition or high-risk pregnancy.
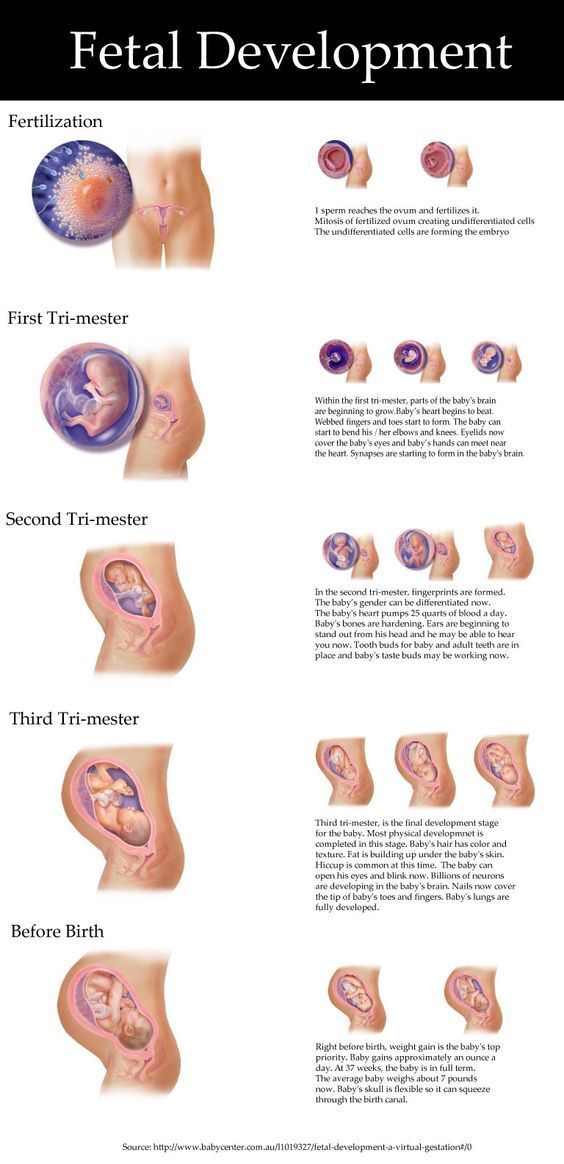
During the second trimester, you’ll likely have an exciting 20-week ultrasound (actually, it’s often anywhere between 18 and 22 weeks). With this scan, you’ll get a good look at your developing baby — even their cute little fingers and toes!
You’ll likely have blood work, urine tests, and a glucose tolerance test, too (maybe not the most fun test, but certainly important to screen you for gestational diabetes).
You may also choose to get testing for complications in the development of the baby. Other tests may be recommended depending on individual health and medical history.
Be sure to tell your healthcare provider if there have been any changes in your diet, lifestyle, or health since your last visit. Don’t hesitate to call your OB-GYN or midwife with questions or concerns in between visits.
During your checkup your doctor will do a brief physical exam. A nurse or assistant will check your weight and take your blood pressure.
Your doctor may recommend additional tests after getting your health history and performing a physical exam.
They may also want to know your family medical history and any medications or supplements you’re taking. Your doctor will also ask you about:
- fetal movement
- sleep patterns
- diet and prenatal vitamin use
- symptoms of preterm labor
- symptoms of preeclampsia, such as swelling
Physical assessments during the second trimester usually include the following checks:
- fundal height, or belly size, and fetal growth
- fetal heartbeat
- edema, or swelling
- weight gain
- blood pressure
- urine protein levels
- urine glucose levels
It can help to come prepared with a list of questions to ask your doctor during the visit.
Also, be sure to see your doctor immediately if you experience symptoms that include:
- vaginal bleeding
- severe or continuous headache
- dimness or blurring of vision
- abdominal pain
- persistent vomiting
- chills or fever
- pain or burning during urination
- leaking of fluid from vagina
- swelling or pain in one lower extremity
Fundal height
Your doctor will measure the height of your uterus, also called the fundal height, measuring from the top of your pelvic bone to the top of your uterus.
There’s usually a relationship between the fundal height and the length of your pregnancy. For example, at 20 weeks, your fundal height should be 20 centimeters (cm), plus or minus 2 cm. At 30 weeks, 30 cm, plus or minus 2 cm, and so on.
This measurement isn’t always accurate as fundal height may be unreliable in people with larger bodies, those who have fibroids, are carrying twins or multiples, or who have excess amniotic fluid.
Your doctor will use the increase in your uterine size as a marker for fetal growth. Measurements can vary. A 2- or 3-cm difference is generally not a cause for concern.
If your fundal height doesn’t grow or is growing slower or faster than expected, your doctor may recommend an ultrasound to check the baby and amniotic fluid.
Fetal heartbeat
Your doctor will check whether your baby’s heart rate is too fast or too slow using Doppler ultrasound.
Doppler technology uses sound waves to measure the heartbeat. It’s safe for you and your baby. Fetal heart rate is usually faster in early pregnancy. It can range from 120 to 160 beats per minute.
Edema (swelling)
Your doctor will also check your legs, ankles, and feet for swelling, or edema. Swelling in your legs is common in pregnancy and generally increases in the third trimester.
Abnormal swelling might indicate a problem like preeclampsia, gestational diabetes, or a blood clot. Though, more than likely, it’s just one of those fun side effects of pregnancy that will go away after giving birth.
Weight gain
Your doctor will note how much weight you’ve gained compared with your weight before pregnancy. They’ll also note how much weight you’ve gained since your last visit.
The amount of weight gain recommended during the second trimester will depend on your pre-pregnancy weight, number of babies you are carrying, and how much weight you have already gained.
If you’re gaining more weight than expected, you may consider making some changes to your diet. A nutritionist or dietitian can help you come up with an eating plan that includes the nutrients you need.
Some people who gain more weight than expected may not be overeating but gaining water weight, which is lost after delivery.
If you aren’t gaining enough weight, you’ll need to supplement your diet. Your doctor may recommend eating two or three healthy snacks each day in addition to what you’ve been eating.
Writing down what and how much you eat will help your doctor come up with a plan to keep you and your baby nourished. If you still aren’t gaining enough weight you may want to consult a dietitian.
If you still aren’t gaining enough weight you may want to consult a dietitian.
Blood pressure
Blood pressure typically decreases during pregnancy due to new hormones in pregnancy and changes in your blood volume. It will usually reach its lowest at 24 to 26 weeks of pregnancy.
Some people will have low blood pressure in their second trimester, for example, 80/40. As long as you feel well, it’s not a cause for concern.
High blood pressure can be dangerous during pregnancy, but is generally okay when it’s well managed.
If blood pressure is high or increasing, your doctor may check you for other symptoms of gestational hypertension or preeclampsia.
Many people have healthy babies despite high blood pressure during pregnancy. It’s important to get monitored regularly, so you can manage high blood pressure if you have it.
Urinalysis
Each time you go in for a checkup, your doctor will check your urine for the presence of protein and sugars. The greatest concern with protein in your urine is development of preeclampsia, which is high blood pressure with swelling and possibly excessive protein in your urine.
The greatest concern with protein in your urine is development of preeclampsia, which is high blood pressure with swelling and possibly excessive protein in your urine.
If you have high glucose levels, your doctor may perform other tests. These may include a test for gestational diabetes, a condition that causes you to develop high blood sugar levels.
If you have symptoms, like painful urination, your doctor may check your urine for bacteria. Urinary tract, bladder, and kidney infections can cause bacteria to appear in your urine.
If this happens, you may be prescribed antibiotics that are safe to take during pregnancy.
In addition to your regular checkups, you might have additional tests during your second trimester, depending on any health risks or complications that develop. Some tests include:
Ultrasound
Ultrasound has become an essential tool for the evaluation of your baby during pregnancy. They’re completely safe for you and your baby, and they’re typically a much-anticipated opportunity to get a sneak peek of your sweet babe.
Many have an ultrasound in the first trimester to confirm pregnancy. Some will wait until the second trimester if they have a low risk for complications.
Also, if the first trimester pelvic exam agreed with menstrual dating, the time of your last menstrual period, the ultrasound may wait until the second trimester.
A second trimester ultrasound can confirm or change the menstrual dating and the stage of your pregnancy to within 10 to 14 days. A second trimester ultrasound will also be able to check fetal anatomy, the placenta, and the amniotic fluid.
While an ultrasound in the second trimester can provide lots of information, it does have limitations. Some anatomical problems are easier to see than others, and some can’t be diagnosed before birth.
For example, excessive fluid buildup in the brain (hydrocephalus), can usually be diagnosed with ultrasound, but small defects in the heart often go undetected before birth.
Triple screen test
In the second trimester, most people under the age of 35 are offered a triple screen test.![]() This is also sometimes called “multiple marker screening” or “AFP plus.” During the test, the mother’s blood is tested for three substances.
This is also sometimes called “multiple marker screening” or “AFP plus.” During the test, the mother’s blood is tested for three substances.
These are:
- AFP, which is a protein produced by your baby
- hCG, which is a hormone that’s produced in the placenta
- estriol, which is a type of estrogen produced by both placenta and baby
Screening tests look for abnormal levels of these substances. The test is typically given between 15 and 22 weeks of pregnancy. The best time for the test is between 16 and 18 weeks.
The triple screen tests can detect fetal abnormalities like Down syndrome, trisomy 18 syndrome, and spina bifida.
Abnormal triple screen test results don’t always mean there is something wrong. Instead, it could indicate risk of a complication, and further testing should be done.
For high-risk pregnancies, if a triple screen test comes back with abnormal results, your doctor may recommend further testing. In some cases, amniocentesis or chorionic villus sampling might be done.
These tests are more precise than the triple screen test, but have an increased risk of complications. Ultrasounds are also sometimes used to look for conditions that could cause abnormal results.
Cell-free fetal DNA test
A cell-free fetal DNA (cffDNA) test may be used to assess your baby’s risk of having a chromosomal disorder. This is a newer test, typically offered to people with pregnancies at increased risk for trisomy 13, 18, or 21.
The American College of Gynecologists (ACOG) notes that this test, like the triple screen test, is used as a screening and not as a diagnostic tool. In other words, if you have a positive cffDNA test, you’ll need a follow-up diagnostic test to confirm a chromosomal abnormality in your baby.
Cell-free fetal DNA is a genetic material released by the placenta. It can be detected in your blood. It shows the genetic makeup of your baby and can detect chromosomal disorders.
While the cffDNA test is more precise in testing for chromosomal abnormalities, it’s still recommended that pregnant people get the triple screen test. The triple screen test checks the blood for both chromosomal abnormalities and neural tube defects.
The triple screen test checks the blood for both chromosomal abnormalities and neural tube defects.
Amniocentesis
Unlike the triple screen tests, amniocentesis can provide a definite diagnosis.
During this procedure, your doctor will take a sample of your amniotic fluid by inserting a needle through your skin and into your amniotic sac. They’ll check your amniotic fluid for any chromosomal and genetic abnormalities in your baby.
Amniocentesis is considered an invasive procedure. It carries a small risk of losing the pregnancy. The decision to get one is a personal choice. It’s only used when the benefits of the test results outweigh the risks of performing the test.
Amniocentesis can provide you with information that only you may use to make decisions, or to alter the course of your pregnancy. For example, if knowing that your baby has Down syndrome would not alter the course of the pregnancy, amniocentesis may not benefit you.
Also, if your doctor finds that an ultrasound already indicates a disorder, you may decide against amniocentesis. However, ultrasound results will not always be accurate because they don’t analyze the fetal chromosome. Amniocentesis provides a more definite diagnosis.
However, ultrasound results will not always be accurate because they don’t analyze the fetal chromosome. Amniocentesis provides a more definite diagnosis.
One-hour glucose tolerance test
ACOG recommends that all pregnant people be screened for gestational diabetes using a 1-hour oral glucose tolerance test.
For this test, you’ll have to drink a sugar solution, generally containing 50 grams of sugar. After one hour, you’ll have your blood drawn to check your sugar level.
If your glucose test is abnormal, your doctor will recommend a 3-hour glucose tolerance test. This is similar to the 1-hour test. Your blood will be drawn after waiting 3 hours.
Gestational diabetes causes your body to have trouble controlling the amount of sugar in your blood. Controlling your blood sugar level is important for a healthy delivery.
If you have gestational diabetes, you may need to make changes in your diet and exercise habits, or take medication. Gestational diabetes normally goes away after you have your baby.
Other tests
Depending on your obstetrical history and your current health, your doctor may perform additional tests for:
- blood count
- platelet count
- RPR, a rapid plasma reagin test for syphilis
- sexually transmitted infections (STIs)
- bacterial vaginosis
Some of these tests require a blood draw, and others require a urine sample. Your doctor may also need to swab your cheek, vagina, or cervix to test for infections.
Blood and platelet tests can identify a weak immune system or problems with blood clotting, which can complicate pregnancy and childbirth.
STIs and other bacterial infections can also cause issues for you and your baby. If they’re detected early you can treat them before your baby is born.
If your healthcare provider detects an abnormality in your baby, you’ll have plenty of opportunity to learn more about the condition from either your doctor or specialists. Your doctor may suggest you speak with a genetic counselor to learn about the problem’s cause, treatment, risk of recurrence, outlook, and prevention.
Your doctor will discuss options for managing your pregnancy. If pregnancy termination is an option, your doctor won’t tell you what decision to make.
If termination is not an option due to your personal beliefs, the information your doctor shares with you may help you manage your pregnancy. In some cases, such as with neural tube defects, the outcome may improve with a cesarean delivery.
Your doctor can also connect you with community resources to help you prepare for a baby with special needs.
If a maternal health problem is diagnosed, you and your healthcare provider can work closely together to treat or monitor the problem.
Infections can usually be treated with antibiotics or proper rest and diet. More serious complications like hypertension or gestational diabetes, require frequent visits to the doctor.
You may need to make changes to your diet or lifestyle. In some cases, your doctor may recommend bed rest or emergency medication.
Remember that your doctor is an important ally. Use your checkups as opportunities to gather information. No question is off the table! Your healthcare providers have heard it all, and they are on hand to help address your concerns and make you feel comfortable throughout your pregnancy.
Use your checkups as opportunities to gather information. No question is off the table! Your healthcare providers have heard it all, and they are on hand to help address your concerns and make you feel comfortable throughout your pregnancy.
It’s important to get routine checkups during pregnancy, especially during your second trimester. Many tests can help you identify and diagnose potential health problems for you and your developing baby.
Diagnosis of certain conditions can help you manage complications and health issues during your pregnancy.
Be sure to bring up any questions or concerns with your doctor, and don’t hesitate to contact them outside of an office visit.
Check-ups, tests and scans available during your pregnancy
Check-ups, tests and scans available during your pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
As part of your antenatal care you will be offered a number of check-ups, tests and scans. Some tests are offered to every woman as part of normal antenatal care in Australia. Other tests will be suggested if you or your baby have a higher risk of problems or are experiencing any concerns during the pregnancy. You don’t have to do any recommended tests if you don’t want to — it’s your choice.
Some tests are offered to every woman as part of normal antenatal care in Australia. Other tests will be suggested if you or your baby have a higher risk of problems or are experiencing any concerns during the pregnancy. You don’t have to do any recommended tests if you don’t want to — it’s your choice.
Checkup, tests and scans infographic
Check out our handy guide for antenatal visits.
Many problems can be detected before your baby is born, but not all of them. There are 2 main types of test offered during antenatal care:
- screening tests, which will let you know if your baby has a higher risk of having a problem, but can’t confirm the problem for sure
- diagnostic tests, which show whether your baby has a problem, with a much greater level of certainty
Your check-ups and tests may be done at a hospital, doctor’s clinic or somewhere else in your community, depending on whether you’re having your baby in a public or private hospital, a birthing centre or at home. This may also determine whether your check-ups are done by your doctor, midwife or obstetrician.
This may also determine whether your check-ups are done by your doctor, midwife or obstetrician.
The timing and number of some of the visits and tests listed below may change slightly depending on the antenatal care you choose, if you’ve had a prior pregnancy and if you are having any problems.
Here are the check-ups, tests and scans you would usually be offered if you have an uncomplicated pregnancy:
First visit
- confirmation that you are pregnant
- calculating how many weeks your pregnancy is and when your due date will be. You may be offered an ultrasound scan if the date is not clear.
- blood pressure, height and weight
- medical and family history
- a blood test, including checking your blood group and test for anaemia, rubella immunity, hepatitis B, hepatitis C, syphilis, chlamydia and HIV
- urine test, to see if you have a bladder or urinary tract infection
- screening for Down syndrome
- cervical screening to check for human papillomavirus (HPV) and/or any signs of cervical cancer
- if at risk of vitamin D deficiency, a test for this may be offered
As part of your check-up, you will usually also discuss with your doctor or midwife:
- which medications you are taking
- whether you smoke or drink alcohol
- whether you would like an influenza (flu) vaccination
- which vitamin and mineral supplements you can take or should avoid
- antenatal care options available to you
- where you can get further information and antenatal classes
Read more here about your first antenatal visit.
19-20 weeks
- blood pressure
- measuring your tummy (abdominal palpation) to check your baby's growth
- checking how your health is and if there are any problems
- ultrasound scan to check your baby's physical development, growth and any complications with your pregnancy. If you want to, during the ultrasound, you can find out whether the baby is a boy or girl.
22 weeks
- blood pressure
- measuring your tummy (abdominal palpation) to check your baby's growth
- checking how your health is and if you have any problems
26-27 weeks
- blood pressure
- measuring your tummy (abdominal palpation) to check your baby's growth
- checking how your health is and if you have any problems
- blood glucose tolerance test for diabetes
28 weeks
- blood pressure
- measuring your tummy (abdominal palpation) to check baby's growth
- checking how your health is and if you have any problems
- checking your baby's heartbeat and movements
- discussing your birth plan and going home with your baby
- blood test to check for anaemia and blood platelet levels
- if your blood type is Rh negative, an anti-D immunoglobulin injection may be given
- pertussis (whooping cough) vaccination
- urine test, if you have signs of a urinary tract infection or raised blood pressure
32 weeks
- blood pressure
- measuring your tummy (abdominal palpation) to check your baby's growth
- checking how your health is and if you have any problems
- checking your baby's heartbeat and movements
- urine test, if you have signs of a urinary tract infection or raised blood pressure
34-36 weeks
- blood pressure
- measuring your tummy (abdominal palpation) to check your baby's growth
- checking how your health is and if you have any problems
- checking your baby's heartbeat and movements
- urine test, if you have signs of a urinary tract infection or raised blood pressure
- vaginal swab for Group B streptococcus (GBS)
- if your blood type is Rh negative, a second anti-D immunoglobulin injection may be given
- assessing presentation (which way up your baby is) and station (how far down the baby's head has moved into your pelvis)
38-39 weeks
- blood pressure
- measuring your tummy (abdominal palpation) to check your baby's growth
- checking how your health is and if you have any problems
- checking your baby's heartbeat and movements
- urine test, if you have signs of a urinary tract infection or raised blood pressure
- assessing presentation and station
40-41 weeks
- blood pressure
- measuring your tummy (abdominal palpation) to check your baby's growth
- checking how your health is and if you have any problems
- checking your baby's heartbeat and movements
- urine test, if you have signs of a urinary tract infection or raised blood pressure
- assessing presentation and station
- if you haven’t had your baby yet, checking your baby’s heartbeat and the amount of fluid around them
As well as the tests, scans and check-ups listed above, your GP, midwife or obstetrician may offer further tests, depending on your risk factors and circumstances. These can include:
These can include:
- Chorionic villus sampling (CVS), where a small amount of the baby’s placenta is collected to test for chromosome problems such as Down syndrome or other abnormality. This is usually done between 11 and 13 weeks of pregnancy, or at another time if a problem is suspected.
- Non-invasive pre-natal testing (NIPT), which is a very accurate test to detect Down syndrome and certain other abnormalities. It can be performed from 10 weeks into the pregnancy.
- A nuchal translucency scan, which looks at the back of your baby’s neck to assess the risk of your baby having Down syndrome. This test is done between 11 and 14 weeks of pregnancy, and may be conducted at the same time as the dating ultrasound.
- Amniocentesis, where a small amount of amniotic fluid (fluid around the baby) is collected to test if the baby has a chromosome problem or other abnormality. This is usually done at 15 to 20 weeks, or at another time if a problem is detected.

Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2020
Back To Top
Related pages
- Blood tests during pregnancy
- Your first antenatal visit
- Checkups, scans and tests during pregnancy
- Antenatal care during your pregnancy
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Citizens | Ministry of Health of the Kaliningrad Region
| Gestational age | Analyzes | Events (registration, medical examinations, doctor visit schedule) |
| Up to 12 weeks | Early registration in the antenatal clinic Taking medications: folic acid throughout the first trimester, no more than 400 mcg / day; potassium iodide 200-250 mcg/day (in the absence of thyroid disease) | |
| At first appearance | An obstetrician-gynecologist collects anamnesis, conducts a general physical examination of the respiratory, circulatory, digestive, urinary system, mammary glands, anthropometry (measuring height, body weight, determining body mass index), measuring the size of the pelvis, examining the cervix in the mirrors, bimanual vaginal study | |
| Not later than 7-10 days after the initial visit to the antenatal clinic | Inspections and consultations: - general practitioner; - a dentist; - an otolaryngologist; - an ophthalmologist; - other medical specialists - according to indications, taking into account concomitant pathology | |
| First trimester (up to 13 weeks) (and at first visit) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol. 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, to the herpes simplex virus (HSV), to cytomegalovirus (CMV), determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of the main blood groups (A, B, 0) and Rh-affiliation. In Rh-negative women: a) examination of the father of the child for group and Rh-affiliation. 7. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 8. Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida. 9. PCR chlamydial infection, PCR gonococcal infection, PCR mycoplasma infection, PCR trichomoniasis. | Visiting an obstetrician-gynecologist every 3-4 weeks (with the physiological course of pregnancy). Electrocardiography (hereinafter - ECG) as prescribed by a general practitioner (cardiologist). Up to 13 weeks of pregnancy are accepted: - folic acid no more than 400 mcg / day; - potassium iodide 200-250 mcg / day (in the absence of thyroid disease) |
| 1 time per month (up to 28 weeks) | Blood test for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 11-14 weeks | Biochemical screening for serum marker levels: - pregnancy-associated plasma protein A (PAPP-A), - free beta subunit of human chorionic gonadotropin (hereinafter - beta-CG) | In the office of prenatal diagnostics, an ultrasound examination (hereinafter referred to as ultrasound) of the pelvic organs is performed. According to the results of complex prenatal diagnostics, a conclusion of a geneticist is issued. |
| After 14 weeks - once | Culture of midstream urine | To exclude asymptomatic bacteriuria (the presence of bacterial colonies more than 105 in 1 ml of an average portion of urine, determined by a culture method without clinical symptoms) to all pregnant women. |
| In the second trimester (14-26 weeks) | General (clinical) analysis of blood and urine. | Visiting an obstetrician-gynecologist every 2-3 weeks (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), uterine tone, palpation of the fetus, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 1 time per month (up to 28 weeks) | Blood for Rh antibodies (in Rh-negative women with Rh-positive affiliation of the father of the child) | |
| 16-18 weeks | Blood test for estriol, alpha-fetoprotein, beta-hCG | Only at late turnout unless biochemical screening for serum marker levels at 11-14 weeks |
| 18-21 weeks | The second screening ultrasound of the fetus is performed in the antenatal clinic | |
| In the third trimester (27-40 weeks) | 1. 2. Biochemical blood test (total protein, urea, creatinine, total bilirubin, direct bilirubin, alanine transaminase (hereinafter - ALT), aspartate transaminase (hereinafter - AST), glucose, total cholesterol). 3. Coagulogram - platelet count, clotting time, bleeding time, platelet aggregation, activated partial thromboplastin time (hereinafter referred to as APTT), fibrinogen, determination of prothrombin (thromboplastin) time. 4. Determination of antibodies of classes M, G (IgM, IgG) to the rubella virus in the blood, determination of antibodies to toxoplasma in the blood. 5. General analysis of urine. 6. Determination of antibodies to pale treponema (Treponema pallidum) in the blood, determination of antibodies of classes M, G to the human immunodeficiency virus HIV-1 and HIV-2 in the blood, determination of antibodies of classes M, G to the antigen of viral hepatitis B and viral hepatitis C in blood. 7. | A visit to an obstetrician-gynecologist every 2 weeks, after 36 weeks - weekly (with the physiological course of pregnancy). At each visit to the doctor of the antenatal clinic - determination of the circumference of the abdomen, VDM, uterine tone, fetal palpation, auscultation of the fetus with a stethoscope. Potassium iodide 200-250 mcg/day |
| 24-28 weeks | Oral glucose tolerance test (OGTT) | |
| 28-30weeks | In Rh-negative women with Rh-positive blood of the child's father and the absence of Rh antibodies in the mother's blood | Administration of human immunoglobulin antirhesus RHO[D] |
| 30 weeks | A certificate of incapacity for work is issued for maternity leave | |
| 30-34 weeks | The third screening ultrasound of the fetus with dopplerometry in the antenatal clinic. - general practitioner; - a dentist. | |
| After 32 weeks | At each visit to the doctor of the antenatal clinic, in addition to determining the circumference of the abdomen, the height of the fundus of the uterus (hereinafter referred to as VDM), the tone of the uterus, determine the position of the fetus, the presenting part, the doctor auscultates the fetus with a stethoscope. | |
| After 33 weeks | Cardiotocography (hereinafter referred to as CTG) of the fetus is performed | |
| Throughout pregnancy | In antenatal clinics there are schools for pregnant women, which are attended by expectant mothers along with fathers. In the process of learning, there is an acquaintance with the changes in the body of a woman during physiological pregnancy, acquaintance with the process of childbirth, the correct behavior in childbirth, the basics of breastfeeding. | |
| Over 37 weeks | Hospitalization with the onset of labor. According to indications - planned antenatal hospitalization. | |
| 41 weeks | Planned hospitalization for delivery | |
| No later than 72 hours after delivery | All women with an Rh-negative blood group who gave birth to a child with a positive Rh-belonging, or a child whose Rh-belonging is not possible to determine, regardless of their compatibility according to the AB0 system | Re-introduction of human immunoglobulin anti-rhesus RHO[D] |
| postpartum period | 1. Early breastfeeding 2. Recommendations for breastfeeding. 3. Consultation of medical specialists on concomitant extragenital disease (if indicated). 4. Toilet of the external genital organs. 5. Dry processing of seams (if any). 6. Removal of external non-absorbable sutures (if any) on the 5th day. 7. Early discharge. | |
| Daily postpartum | 1. Examination by an obstetrician-gynecologist; 2. Inspection and palpation of the mammary glands. | |
| 3 days after birth | Ultrasound of the pelvic organs | |
| After delivery by caesarean section | 1. Complete blood count, general urinalysis. 2. Biochemistry of blood (according to indications). | Ultrasound of the pelvic organs |
Study plan during pregnancy
What tests should be done when you are expecting a baby? Ultrasound, screenings, tests and other studies - hand over on time.
Any expectant mother wants her baby to be born on time and be healthy. Previously, one had to rely only on the wisdom of nature and anxiously await the birth of a child. But now, almost all the changes that occur with the baby in the womb can be tracked with the help of mandatory tests and studies that are prescribed in the antenatal clinic.
Previously, one had to rely only on the wisdom of nature and anxiously await the birth of a child. But now, almost all the changes that occur with the baby in the womb can be tracked with the help of mandatory tests and studies that are prescribed in the antenatal clinic.
Why is this necessary?
The right way
How to eat properly for a future mother, what myths about pregnancy should not be believed, and how to quickly get ready for the hospital, experts say.
Getting up early and taking tests on an empty stomach, sitting in queues, ultrasounds, examinations and measurements seem to many women to be useless procedures that take too much time and effort. If the state of health is normal, some expectant mothers try to avoid even scheduled studies . But all the data that is collected during pregnancy is needed by the doctor for only one purpose - so that your pregnancy goes well and you give birth to a healthy baby. Including without genetic anomalies. Take your trips to the antenatal clinic not as a severe necessity, but as a manifestation of your care about the unborn baby, which begins even before his birth. After all, many hidden problems with your or his health can only be detected by the results of the tests.
Including without genetic anomalies. Take your trips to the antenatal clinic not as a severe necessity, but as a manifestation of your care about the unborn baby, which begins even before his birth. After all, many hidden problems with your or his health can only be detected by the results of the tests.
First trimester
The first visit to the antenatal clinic takes place at 7-8 weeks of pregnancy. It is around this time that most expectant mothers find out that they are pregnant. The obstetrician-gynecologist will measure the weight, height, pressure and size of the pelvis. You can also consult with your doctor about taking vitamin and mineral supplements. But you will leave the antenatal clinic for a reason, but with a whole bunch of referrals for analyzes and consultations of specialists. In two weeks you will have to submit: - Urinalysis . The morning portion of urine is collected on an empty stomach. Based on the results of this analysis, the work of the kidneys and the bacterial "population" of the bladder are evaluated. - Vaginal swab for microscopic examination. It will show if there are inflammatory processes in the genitals, obvious and latent infections. - Complete blood count . Rented in the morning and on an empty stomach. It shows the composition of the blood and allows you to track its change in dynamics. For example, such an important factor as the level of hemoglobin in the blood. This substance is the only transporter of oxygen in the blood, and the oxygen supply of the fetus depends on its quantity. - Analysis for blood group and Rh factor . Even if these indicators are tattooed on your forearm, the doctor in charge of your pregnancy is obliged to check them. Moreover, if your Rh factor is negative, the father of the unborn child will also be sent for analysis to find out if you will have a Rh conflict (Rh factor incompatibility). - Blood test for HIV, hepatitis B and C and syphilis .
Based on the results of this analysis, the work of the kidneys and the bacterial "population" of the bladder are evaluated. - Vaginal swab for microscopic examination. It will show if there are inflammatory processes in the genitals, obvious and latent infections. - Complete blood count . Rented in the morning and on an empty stomach. It shows the composition of the blood and allows you to track its change in dynamics. For example, such an important factor as the level of hemoglobin in the blood. This substance is the only transporter of oxygen in the blood, and the oxygen supply of the fetus depends on its quantity. - Analysis for blood group and Rh factor . Even if these indicators are tattooed on your forearm, the doctor in charge of your pregnancy is obliged to check them. Moreover, if your Rh factor is negative, the father of the unborn child will also be sent for analysis to find out if you will have a Rh conflict (Rh factor incompatibility). - Blood test for HIV, hepatitis B and C and syphilis . Even if you are completely confident in yourself and your partner, you should consider the need to check up again as an additional guarantee that everything is in order with you. - Blood test for TORCH infection . These include toxoplasma, mycoplasma, cytomegalovirus and herpes virus. They can stay in a woman's body for years and not cause her any inconvenience, but lead to malformations in the unborn child. If the analysis is positive, the doctor selects a special treatment for the woman. - Blood test for sugar . Pregnancy creates an increased load on all organs of a woman. Including the pancreas. This analysis allows you to determine how effectively it works and foresee all the risks associated with the risk of developing diabetes during pregnancy. - Blood test for clotting , or coagulogram. This study allows you to determine how blood coagulates - whether there is a tendency to clot or bleeding. During the same two weeks, it is necessary to visit a general practitioner, endocrinologist, ophthalmologist and otolaryngologist and make an electrocardiogram.
Even if you are completely confident in yourself and your partner, you should consider the need to check up again as an additional guarantee that everything is in order with you. - Blood test for TORCH infection . These include toxoplasma, mycoplasma, cytomegalovirus and herpes virus. They can stay in a woman's body for years and not cause her any inconvenience, but lead to malformations in the unborn child. If the analysis is positive, the doctor selects a special treatment for the woman. - Blood test for sugar . Pregnancy creates an increased load on all organs of a woman. Including the pancreas. This analysis allows you to determine how effectively it works and foresee all the risks associated with the risk of developing diabetes during pregnancy. - Blood test for clotting , or coagulogram. This study allows you to determine how blood coagulates - whether there is a tendency to clot or bleeding. During the same two weeks, it is necessary to visit a general practitioner, endocrinologist, ophthalmologist and otolaryngologist and make an electrocardiogram. The second visit to the doctor is expected at 10 weeks . You again take a urine test and prepare for the fact that before each visit to the doctor, until the very birth, you will begin to come with a characteristic jar. At this meeting, the doctor will look at the results of your tests and the appointments of other specialists and draw a conclusion about your state of health. On term 12 weeks you must complete the so-called first screening . It consists of a blood test that detects deviations in the development of the child, and an ultrasound examination (ultrasound), which, according to certain parameters, shows the degree of risk of genetic abnormalities in the baby, for example, Down syndrome.
The second visit to the doctor is expected at 10 weeks . You again take a urine test and prepare for the fact that before each visit to the doctor, until the very birth, you will begin to come with a characteristic jar. At this meeting, the doctor will look at the results of your tests and the appointments of other specialists and draw a conclusion about your state of health. On term 12 weeks you must complete the so-called first screening . It consists of a blood test that detects deviations in the development of the child, and an ultrasound examination (ultrasound), which, according to certain parameters, shows the degree of risk of genetic abnormalities in the baby, for example, Down syndrome.
Second trimester
From 16 weeks the doctor can clearly hear the fetal heartbeat with an obstetric stethoscope. At this time, the height of the position of the fundus of the uterus and the volume of the abdomen will be measured to determine whether the development of the child is proceeding correctly. Now these parameters will be measured at each visit. AT 18 weeks is undergoing a second screening , which reveals the risks of chromosomal abnormalities and congenital malformations of the fetus by examining the level of certain blood proteins: alpha-fetoprotein and human chorionic gonadotropin. This study is possible only for a month - from 16 to 20 weeks. In other periods, the level of these proteins is not informative. In addition, at week 18, blood tests for sugar are taken - the work of the pancreas is checked again. The next visit to the doctor is only in a month - at 22 week pregnancy. In addition to the traditional examination, a mandatory ultrasound is waiting for you, which will show how the baby's organs, the placenta, and how much amniotic fluid is contained in the uterus. At this time, it is already possible to determine the sex of the unborn child . In addition to ultrasound, Doppler studies of the blood flow, uterus, placenta and umbilical cord are done to find out how well the baby is supplied with oxygen and nutrients.
Now these parameters will be measured at each visit. AT 18 weeks is undergoing a second screening , which reveals the risks of chromosomal abnormalities and congenital malformations of the fetus by examining the level of certain blood proteins: alpha-fetoprotein and human chorionic gonadotropin. This study is possible only for a month - from 16 to 20 weeks. In other periods, the level of these proteins is not informative. In addition, at week 18, blood tests for sugar are taken - the work of the pancreas is checked again. The next visit to the doctor is only in a month - at 22 week pregnancy. In addition to the traditional examination, a mandatory ultrasound is waiting for you, which will show how the baby's organs, the placenta, and how much amniotic fluid is contained in the uterus. At this time, it is already possible to determine the sex of the unborn child . In addition to ultrasound, Doppler studies of the blood flow, uterus, placenta and umbilical cord are done to find out how well the baby is supplied with oxygen and nutrients. At week 26 , the meeting with the doctor leading the pregnancy will not take much time - only an examination awaits you.
At week 26 , the meeting with the doctor leading the pregnancy will not take much time - only an examination awaits you.
Third trimester
By 30 weeks of pregnancy, a detailed blood test, which you did at the very beginning of pregnancy, must be repeated. Its results are necessary to fill out exchange card - the main document of a pregnant woman, without which she can only go to a specialized maternity hospital in case of sudden birth. At the same time, the position of the child in the uterus is determined, and the long-awaited maternity leave is issued. AT 33 weeks the doctor performs the third screening - using ultrasound, determines the features of the baby's development, reveals some malformations that are visible only in the later stages. The next visit to the doctor is at 35 weeks . At this time, cardiotocography is performed - a study of the child's heart and its motor activity.
 General (clinical) blood test.
General (clinical) blood test. 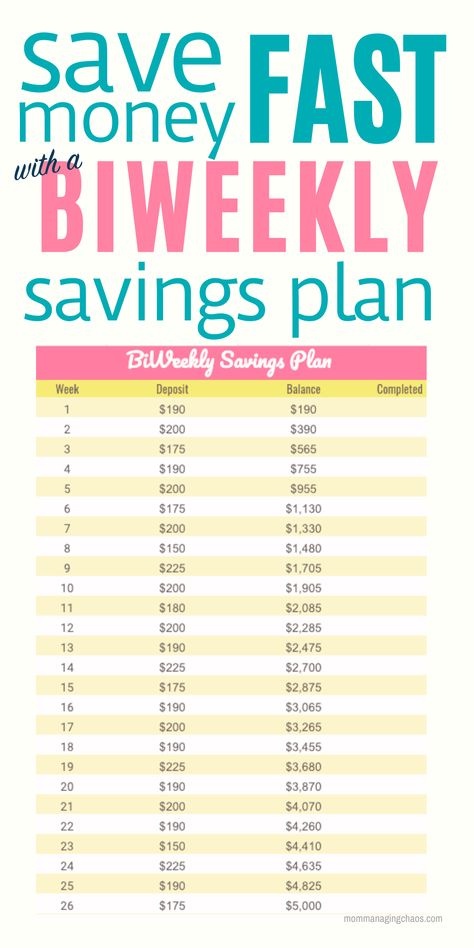
 General (clinical) blood test.
General (clinical) blood test.  Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.
Microscopic examination of the discharge of female genital organs for gonococcus, microscopic examination of the vaginal discharge for fungi of the genus Candida.  Inspections and consultations:
Inspections and consultations: