Vaginal infection and pregnancy
Bacterial vaginosis and pregnancy | March of Dimes
Bacterial vaginosis (BV) is a common infection that’s easily treated, but it can cause problems for your baby during pregnancy.
Having BV during pregnancy can increase your baby’s risk for premature birth and low birthweight.
BV can increase your risk for pelvic inflammatory disease, which can cause problems if you’re trying to get pregnant.
BV isn’t a sexually transmitted infection, but it is common in sexually active women.
Getting treated for BV during pregnancy can help protect your baby.
What is bacterial vaginosis?
Bacterial vaginosis (also called BV or vaginitis) is an infection caused when there’s too much of certain bacteria in the vagina. It’s the most common vaginal infection in women ages 15 to 44.
BV is not a sexually transmitted infection (also called STI or sexually transmitted disease or STD), but it is common in sexually active women and it rarely happens to women who haven’t had sex. An STI is an infection you can get by have unprotected sex with an infected person. If you have BV that’s not treated, it can increase your risk of getting an STD. It’s important to have any infection treated during pregnancy to help protect you and your baby.
What causes BV?
We don’t know for sure what causes BV. Any woman can get it, but you’re at increased risk for BV if you:
- Have new sex partners
- Have more than one sex partner
- Douche (use water or other liquid to clean inside the vagina)
- Are pregnant
- Are African-American. BV is twice as common in African-American women than in white women.
- Have an intrauterine device (also called IUD), especially if you have irregular bleeding. An IUD is a kind of birth control. It's a t-shaped piece of plastic that's placed in your uterus that helps prevents prevent pregnancy.
How can BV affect pregnancy?
The Centers for Disease Control and Prevention (also called CDC) estimates that 1 million pregnant women get BV each year. Pregnant women are at increased risk for BV because of hormone changes that happen during pregnancy. Hormones are chemicals made by the body.
Pregnant women are at increased risk for BV because of hormone changes that happen during pregnancy. Hormones are chemicals made by the body.
If you have BV during pregnancy, your baby is at increased risk for premature birth and low birthweight. Premature birth is birth before 37 weeks of pregnancy. Low birthweight is when your baby is born weighing less than 5 pounds, 8 ounces. Being born too early or too small can cause health problems for your baby.
BV also can cause pelvic inflammatory diseases (also called PID). PID is an infection in the uterus that can increase your risk for infertility (not being able to get pregnant).
How can you reduce your risk for BV?
Here are some things you can do to help protect yourself from BV:
- Don’t have sex. BV isn’t an STI, but you’re more likely to get it if you have sex than if you don’t.
- Limit the number of sex partners you have. Have sex with only one person who doesn’t have other sex partners.

- Use a condom every time you have sex. Condoms are barrier methods of birth control. Barrier methods help prevent pregnancy (and STIs) by blocking or killing your partner’s sperm. Other kinds of birth control, like the pill and implants, don’t protect you from STIs.
- Don’t douche. Douching can remove normal bacteria in your vagina that can help protect you from infection.
- Use warm water only and no soap to clean the outside of your vagina. Always wipe front to back.
What are the signs and symptoms of BV?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Many women with BV have no signs or symptoms, but you may have:
- Thin white or grey vaginal discharge
- Strong, fishy odor, especially after having sex
- Pain, itching or burning in the vagina
- Itching around the outside of the vagina
- Burning feeling when you urinate
If you think you may have BV, tell your health care provider right away. Your provider can check your vagina for signs of vaginal discharge and test a sample of vaginal fluid for bacteria associated with BV.
Your provider can check your vagina for signs of vaginal discharge and test a sample of vaginal fluid for bacteria associated with BV.
BV is treated with antibiotics. Antibiotics are medicines that kill infections caused by bacteria. The antibiotic may be oral (taken by mouth) or a cream or gel that you put into your vagina. Treatment with antibiotics for BV is safe for your baby during pregnancy, and it may help reduce your risk for STDs.
If you have BV:
- Take all your medicine exactly as your provider tells you to. Take all of it even if you have no signs or symptoms.
- If you have female sex partners, tell them you have BV so they can get tested and treated.
- Don’t have sex until you finish your treatment.
- Tell your provider if you have signs or symptoms after you finish your treatment.
More information
Bacterial vaginosis—CDC fact sheet
Bacterial vaginosis fact sheet from womenshealth.gov
Vaginitis FAQ from the American College of Obstetricians and Gynecologists
Last reviewed: February, 2018
Infections in Pregnancy: Bacterial Vaginosis
What Is Bacterial Vaginosis?
Bacterial vaginosis (BV) is an infection in the vagina caused by bacteria. The vagina naturally has “good” bacteria called lactobacilli and a few “bad” bacteria called anaerobes. Normally, there’s a careful balance between lactobacilli and anaerobes. When that balance is disrupted, however, anaerobes can increase in number and cause BV.
The vagina naturally has “good” bacteria called lactobacilli and a few “bad” bacteria called anaerobes. Normally, there’s a careful balance between lactobacilli and anaerobes. When that balance is disrupted, however, anaerobes can increase in number and cause BV.
BV is the most common vaginal infection in women between ages 15 and 44. It’s also one of the most common infections in women who are pregnant, affecting approximately 1 million pregnant women each year. BV is typically a mild infection and is easily treatable with medication. When left untreated, however, the infection can increase your risk for sexually transmitted infections and complications during pregnancy.
What Are the Symptoms of Bacterial Vaginosis?
Approximately 50 to 75 percent of women with BV don’t experience any symptoms. When symptoms do occur, you may have abnormal and foul-smelling vaginal discharge. The discharge is usually thin and dull gray or white. In some cases, it may also be foamy. The fish-like odor that’s often associated with the discharge is a result of the chemicals that are produced by the bacteria that cause BV. Menstruation and sexual intercourse usually make the odor worse, as blood and semen react with the bacteria to release odorous chemicals. Itching or irritation around the outside of the vagina can also occur in women with BV.
The fish-like odor that’s often associated with the discharge is a result of the chemicals that are produced by the bacteria that cause BV. Menstruation and sexual intercourse usually make the odor worse, as blood and semen react with the bacteria to release odorous chemicals. Itching or irritation around the outside of the vagina can also occur in women with BV.
What Causes Bacterial Vaginosis?
BV is the result of an overgrowth of certain bacteria in the vagina. Like in other parts of the body, including the mouth and intestines, there are various bacteria that live in the vagina. Many of these bacteria actually protect the body from other bacteria that can cause disease. In the vagina, lactobacilli are the naturally occurring bacteria that fight off infectious bacteria. The infectious bacteria are known as anaerobes.
There’s normally a natural balance between lactobacilli and anaerobes. Lactobacilli typically account for the majority of bacteria in the vagina and control the growth of anaerobes. However, if the lactobacilli are reduced in number, anaerobes have the opportunity to grow. When an overgrowth of anaerobes takes place in the vagina, BV can occur.
However, if the lactobacilli are reduced in number, anaerobes have the opportunity to grow. When an overgrowth of anaerobes takes place in the vagina, BV can occur.
Doctors don’t know the exact cause of the bacterial imbalance that triggers BV. However, certain factors can increase your risk of developing the infection. These include:
- douching
- having unprotected sexual intercourse
- having multiple sex partners
- using antibiotics
- using vaginal medications
How Is Bacterial Vaginosis Diagnosed?
To diagnose BV, your doctor will ask you about your medical history and perform a pelvic exam. During the exam, your doctor will examine your vagina and check for signs of an infection. Your doctor will also take a sample of your vaginal discharge so it can be analyzed under a microscope.
How Is Bacterial Vaginosis Treated?
BV is often treated with antibiotics. These may come as pills you swallow or as a cream that you insert into your vagina. Regardless of the type of treatment used, it’s important to follow your doctor’s instructions and to complete the full round of medication.
Regardless of the type of treatment used, it’s important to follow your doctor’s instructions and to complete the full round of medication.
Your doctor may prescribe the following antibiotics:
- metronidazole, such as Flagyl and Metrogel-Vaginal, which can be taken orally
- tinidazole, such as Tindamax, which is another type of oral medication
- clindamycin, such as Cleocin and Clindesse, which is a topical medication that can be inserted into the vagina
These medications are usually effective in treating BV. They all have similar side effects, with the exception of metronidazole. This particular medication may cause severe nausea, vomiting, and headaches when taken with alcohol. Make sure to speak with your doctor if you have concerns about any of the possible side effects.
Once treatment is received, BV usually clears up within two to three days. However, treatment usually continues for at least one week. Don’t stop taking your medications until your doctor tells you to do so. It’s important to take the full course of antibiotics to prevent the infection from coming back. You may need long-term treatment if your symptoms persist or continue to come back.
It’s important to take the full course of antibiotics to prevent the infection from coming back. You may need long-term treatment if your symptoms persist or continue to come back.
What Are the Possible Complications of Bacterial Vaginosis?
When left untreated, BV can cause serious complications and health risks. These include:
- Pregnancy complications: Pregnant women with BV are more likely to have an early delivery or low birth weight baby. They also have a greater chance of developing another type of infection after delivery.
- Sexually transmitted infections: BV increases your risk of getting sexually transmitted infections, including the herpes simplex virus, chlamydia, and HIV.
- Pelvic inflammatory disease: In some cases, BV may lead to pelvic inflammatory disease, an infection of the reproductive organs in women. This condition can increase the risk of infertility.
- Infections after surgery: BV puts you at a higher risk for infections after surgeries affecting the reproductive system.
 These include hysterectomies, abortions, and cesarean deliveries.
These include hysterectomies, abortions, and cesarean deliveries.
How Can Bacterial Vaginosis Be Prevented?
You can take the following steps to lower your risk of developing BV:
- Minimize irritation. You can minimize vaginal irritation by not using soap to clean the outside of your vagina. Even mild and unscented soap can irritate the vagina. It’s also helpful to stay out of hot tubs and whirlpool spas. Wearing cotton underpants can help keep the area cool and prevent irritation.
- Don’t douche. Douching removes some of the bacteria that protect your vagina from infection, which increases your risk of getting BV.
- Use protection. Always practice safe sex by using a condom with all of your sexual partners. This is the best way to prevent the spread of BV. It’s also important to limit your number of sex partners and to get tested for sexually transmitted infections every six months.
BV is a common infection, but taking these preventive measures can reduce your risk of getting it. It’s crucial to call your doctor right away if you believe you have BV, especially if you’re pregnant. Getting prompt treatment will help prevent complications from occurring.
It’s crucial to call your doctor right away if you believe you have BV, especially if you’re pregnant. Getting prompt treatment will help prevent complications from occurring.
Vaginal infections during pregnancy: what expectant mothers need to know condition of the vagina.
Like all open cavities of the body, it is inhabited by a variety of microbes. Some of them, falling on the mucous membranes, fail to stay there for a long time - they are expelled by the flow of mucus or urine, and those microorganisms that are able to resist and multiply under these conditions constitute the normal microflora of the vagina. If the process of attachment and formation of new microbes is not accompanied by inflammation, it is called colonization, but if the tissue is damaged at the time of the appearance of bacteria, then we are talking about the development of an infection.
The normal microflora protects the vagina from harmful microorganisms. It contains many bacteria (108–1010 microbial bodies/1 g of secretions). First of all, the composition of the microflora depends on whether the woman has problems with the monthly cycle and hormone production. If everything is in order with both, lactobacilli will settle in the vagina, which form hydrogen peroxide and protect their “home” from harmful bacteria. In addition, they produce lactic acid, lactocidin, acidophilus and lactocin B - these substances also help fight "uninvited guests.
First of all, the composition of the microflora depends on whether the woman has problems with the monthly cycle and hormone production. If everything is in order with both, lactobacilli will settle in the vagina, which form hydrogen peroxide and protect their “home” from harmful bacteria. In addition, they produce lactic acid, lactocidin, acidophilus and lactocin B - these substances also help fight "uninvited guests.
Bacterial vaginosis and most vaginal infections are not considered sexually transmitted diseases. This is why the partner is usually not given any treatment. However, if a man has unpleasant sensations (itching, burning, a small rash), he will also have to see a doctor.
- Photo
- Monkey Business Images/Getty Images
Other bacteria live in the vagina: staphylococci, streptococci, intestinal or anaerobic bacteria. And sometimes they are accompanied by mycoplasmas, ureaplasmas, gardnerella. However, having learned about this, you should not worry: the main thing is that these microorganisms are in the right ratio with each other. As long as the balance between them is not disturbed, they will not create problems. If, for some reason, the living conditions in the vagina change, for example, during pregnancy, this may result in the appearance of a disease.
And sometimes they are accompanied by mycoplasmas, ureaplasmas, gardnerella. However, having learned about this, you should not worry: the main thing is that these microorganisms are in the right ratio with each other. As long as the balance between them is not disturbed, they will not create problems. If, for some reason, the living conditions in the vagina change, for example, during pregnancy, this may result in the appearance of a disease.
In an evolutionary way
The composition of the microflora of our secluded places changes depending on age and hormonal changes in a woman's body. During the monthly cycle, young women ready to conceive a child change both the quantity and quality of microbes living in the vagina. So, at the time of menstruation and after love contacts, the number of lactobacilli decreases, and there are more intestinal bacteria, enterococci and streptococci.
The right balance
Due to disturbances in the microflora of the vagina, such a nuisance as bacterial vaginosis may appear. This disease does not apply to sexually transmitted infections. It usually begins when the normal microflora of the vagina, which consists mainly of lactobacilli, is displaced by those types of bacteria that should be present here in small quantities.
This disease does not apply to sexually transmitted infections. It usually begins when the normal microflora of the vagina, which consists mainly of lactobacilli, is displaced by those types of bacteria that should be present here in small quantities.
How does bacterial vaginosis manifest itself? As a rule, it manifests itself in copious liquid secretions with an unpleasant odor, reminiscent of spoiled fish. To cure the disease, the doctor will need to find and eliminate the cause of its occurrence; in addition, the doctor will prescribe to the patient drugs to combat harmful bacteria and agents that will help restore the normal microflora of the vagina. With regard to preventing bacterial vaginosis, experts advise women to be less nervous, not to wear too tight clothes that press between the legs (for example, jeans), synthetic underwear and tights without a cotton gusset. In addition, you should not get carried away with a thorough and deep toilet of the vagina, since attempts to flush it from the inside, for example, with a syringe, can lead to the fact that normal bacteria will simply be washed out of their shelter. We should not forget that antibiotic treatment can lead to an imbalance in the vagina.
We should not forget that antibiotic treatment can lead to an imbalance in the vagina.
The appearance of most vaginal infections is not a reason to suspect a partner of infidelity. Ordinary fatigue or stress can cause trouble.
- Photo
- Getty Images/iStockphoto
To know in person
What happens if the normal microflora of the vagina fails to cope with the appearance of harmful bacteria? In this case, a woman may start to have trouble: thrush (another name is vulvovaginal candidiasis, candidiasis, mycosis), trichomonas or nonspecific colpitis. Let's talk about each of them in more detail.
1) According to statistics, about 70% of women have been treated for thrush at least once in their lives . At the same time, 40–50% of the fair sex experienced repeated outbreaks of the disease, and 5% developed an unpleasant chronic form of candidiasis.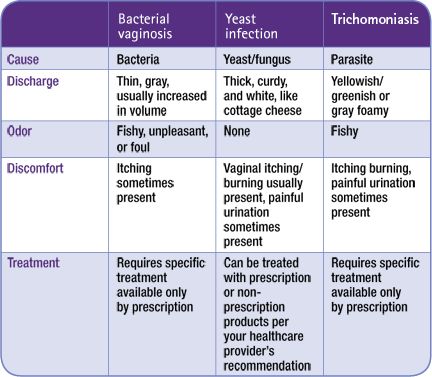 The disease occurs due to hormonal disruptions in the body, as a result of a weakened immune system, after treatment with antibiotics. Usually, fungi that live in the body itself, for example, in the intestines, act as the causative agent of thrush. However, sometimes candida is passed from partner to partner. As long as there are few yeast-like fungi in the vagina, they do not cause problems. If for some reason they begin to multiply, a woman develops “curdled” (thick and flaky) white discharge, severe itching in the genital area, and sometimes even a burning sensation at the time of going to the toilet “in a small way”. In men, candida causes inflammation of the glans penis, foreskin, and urinary organs.
The disease occurs due to hormonal disruptions in the body, as a result of a weakened immune system, after treatment with antibiotics. Usually, fungi that live in the body itself, for example, in the intestines, act as the causative agent of thrush. However, sometimes candida is passed from partner to partner. As long as there are few yeast-like fungi in the vagina, they do not cause problems. If for some reason they begin to multiply, a woman develops “curdled” (thick and flaky) white discharge, severe itching in the genital area, and sometimes even a burning sensation at the time of going to the toilet “in a small way”. In men, candida causes inflammation of the glans penis, foreskin, and urinary organs.
It happens that thrush haunts the expectant mother throughout pregnancy and is difficult to treat. Despite the seeming harmlessness, it should always be treated. In addition to discomfort, it causes inflammation of the mucosa of the labia and vagina. As a result, the mucosa becomes more vulnerable and can be easily injured during childbirth. In addition, there is a risk that the causative agent of infection from the genitals of the expectant mother will reach the child during childbirth. Therefore, at the 36th week of pregnancy, all women take a swab from the vagina for flora and, if necessary, prescribe treatment. Sometimes it is possible to cope with the situation with local means (candles), but it is also often necessary to prescribe tablets.
In addition, there is a risk that the causative agent of infection from the genitals of the expectant mother will reach the child during childbirth. Therefore, at the 36th week of pregnancy, all women take a swab from the vagina for flora and, if necessary, prescribe treatment. Sometimes it is possible to cope with the situation with local means (candles), but it is also often necessary to prescribe tablets.
2) Nonspecific (bacterial) vaginitis, or colpitis , begins due to the multiplication of harmful microorganisms - staphylococci, streptococci, intestinal bacteria, mycoplasmas. As a result, a woman has unusual vaginal discharge: yellow, with pus. In addition, the patient may complain that she often has to run to the toilet "in a small way", and pain appears during sexual intercourse. With the detection of bacterial vaginosis, even if the expectant mother does not have any complaints and the diagnosis is based on the results of a smear, she is prescribed treatment.
3) Trichomoniasis (specialists also call it trichomonas vaginitis, or colpitis) refers to diseases that are just sexually transmitted. It is caused by the protozoan parasite Trichomonas, which can be found on wet towels, swimwear or toilet bowls in public places. The onset of the disease is characterized by itching, burning in the vaginal area, pain at the time of going to the toilet "in a small way". Plus, a woman has abundant white, sometimes frothy discharge with an unpleasant odor. Since in some cases the problem may not bother the expectant mother in any way, the diagnostic test, on the basis of which the decision is made on the need for treatment, will be the method of seeding microorganisms with the determination of their sensitivity to antibiotics.
Nonspecific vaginitis, like all the problems listed above, must be treated at any stage of pregnancy , and here's why. During pregnancy, a smear for the vaginal flora is taken three times - in the I, II and III trimesters. Its results closer to the term of childbirth will be very important. The fact is that this process provokes the spread of the infection in the body, because childbirth is accompanied by blood loss, leaving behind wound surfaces; plus, the normally sterile uterine cavity communicates with the non-sterile vagina during the movement of the child through the birth canal, and all this creates conditions for the spread of dangerous microbes from the vagina upwards - into the uterus and to the child.
Its results closer to the term of childbirth will be very important. The fact is that this process provokes the spread of the infection in the body, because childbirth is accompanied by blood loss, leaving behind wound surfaces; plus, the normally sterile uterine cavity communicates with the non-sterile vagina during the movement of the child through the birth canal, and all this creates conditions for the spread of dangerous microbes from the vagina upwards - into the uterus and to the child.
That is why the infection must be dealt with before the start of labor, and if the doctor prescribes antibiotics to the expectant mother, do not be afraid to take them, because the presence of disease-causing agents can cause much more harm than a properly selected drug.
During pregnancy, the microflora of the expectant mother's vagina becomes more homogeneous, it is represented mainly by lactobacilli (their number increases 10 times). It would seem that with the increase in the number of microbes-defenders, nothing should threaten a woman and her child.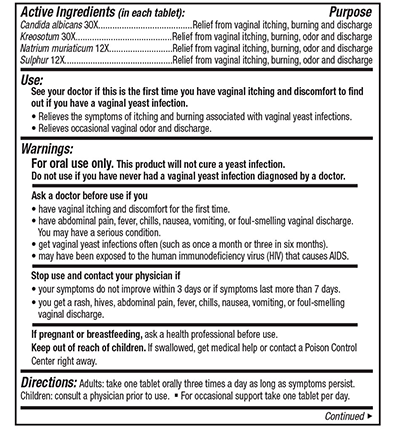 But, alas, along with the predominance of lactobacilli, the acidic environment of the vagina changes, which, coupled with the suppression of the immune system during pregnancy, creates conditions for the growth and reproduction of other microorganisms from among its inhabitants.
But, alas, along with the predominance of lactobacilli, the acidic environment of the vagina changes, which, coupled with the suppression of the immune system during pregnancy, creates conditions for the growth and reproduction of other microorganisms from among its inhabitants.
More useful materials about women's health - in our channel on Yandex.Zen.
Lyubov Prishlya
possible risks – Dobrobut Clinic
Main
Dobrobut Medical Library
Publication date: 2020-03-18
Bacterial vaginosis: symptoms, causes, transmission routes, treatment
Bacterial vaginosis (BV) is a disease caused by excessive growth of opportunistic and pathogenic (in particular, facultative anaerobic) microorganisms in the vagina against the background of a decrease in the number of lactic acid bacteria. Bacterial vaginosis in women of reproductive age is quite common. It accounts for 30 to 50% of all vulvovaginal infections.
It accounts for 30 to 50% of all vulvovaginal infections.
Bacterial vaginosis: causes
Bacterial vaginosis develops when the normal microflora of the vagina is replaced by opportunistic microorganisms (mycoplasmas, fusobacteria, gardnerella, vilonella, peptococci and others).
The causes of bacterial vaginosis are as follows:
- frequent douching;
- use of intrauterine devices;
- excessive sexual activity;
- uncontrolled use of antibiotics;
- psychosocial stress.
How is bacterial vaginosis transmitted? BV is not considered a sexually transmitted disease for the following reasons:
- the condition occurs in women who are not sexually active;
- men do not have an equivalent disease;
- prescribing antibiotics to a male partner does not affect the incidence of exacerbations in women;
- The prevalence of BV differs markedly in ethnic groups, which cannot be explained only by different degrees of sexual activity.

The main signs of bacterial vaginosis
The disease can occur both asymptomatically and with clinical manifestations. The diagnosis is confirmed after receiving the results of the analysis of vaginal discharge: pH above 4.5 and a large number of opportunistic bacteria indicate the presence of BV.
The symptoms of bacterial vaginosis are as follows:
- Vaginal discharge with an unpleasant fishy odor. At the beginning of the disease, they are white or gray in color, with a progressive process they become yellowish-greenish.
- Burning when urinating.
- Dysuria (impaired urination).
- Vaginal pruritus.
- Hyperemia of the mucous membrane of the vagina and cervix.
It should be noted that half of the patients with BV are asymptomatic.
How to treat bacterial vaginosis
The drugs of choice are metronidazole and clindamycin. Assign them orally and / or in the form of vaginal suppositories.![]() It should be noted that after a course of antibiotic therapy, the symptoms in 10-15% of patients remain the same. The recurrence rate reaches 80% and increases with increasing sexual activity. The use of estrogen-containing contraceptives reduces the number of repeated exacerbations.
It should be noted that after a course of antibiotic therapy, the symptoms in 10-15% of patients remain the same. The recurrence rate reaches 80% and increases with increasing sexual activity. The use of estrogen-containing contraceptives reduces the number of repeated exacerbations.
How else to treat bacterial vaginosis? Macrolides, lincosamides, penicillins, nitroimidazoles are reserved drugs. Due to the likelihood of activation of the candidal flora, antimycotics are prescribed in parallel with antibacterial drugs. You can use combined forms, for example, Terzhinan, Klion-D. Also, gynecologists recommend taking probiotics, which help restore the vaginal microflora - this reduces the likelihood of recurrence of the disease.
Bacterial vaginosis is not considered a sexually transmitted infection, so the sexual partner is not treated.
Complications of bacterial vaginosis, disease prevention
BV can lead to pregnancy complications and the development of pelvic inflammatory disease. There is a link between a decrease in the number of lactobacilli in the vagina and the frequency of infection with gonococci and chlamydia. BV increases the chance of infection or reactivation of the human papillomavirus.
There is a link between a decrease in the number of lactobacilli in the vagina and the frequency of infection with gonococci and chlamydia. BV increases the chance of infection or reactivation of the human papillomavirus.
Bacterial vaginosis during pregnancy can complicate the course of the underlying disease, which increases the risk of miscarriage or premature birth. Pregnant women diagnosed with bacterial vaginosis are more likely to develop chorioamnionitis (inflammation of the membranes and infection of the amniotic fluid), postpartum endometritis. BV can also cause subclinical iron deficiency. Read more about iron deficiency in early pregnancy on our website https://www.dobrobut.com. Studies have confirmed the relationship between bacterial vaginosis and tubal infertility.
Prevention of bacterial vaginosis consists in avoiding douching, limiting the number of sexual partners, and a healthy lifestyle.
Do you want to get an online explanation from the doctor of the Dobrobut MS?
Download our Google Play and App Store app
Our doctors
See all doctors 636
Our certificates
Certificate no. QIZ 804 468 C1
QIZ 804 468 C1
Certificate no. QIZ 804 469 C1
Certificate No. QIZ 804 470 C1
Certificate no. QIZ 804 471 C1
View all certificates
Request a call back
Enter your phone number
Other articles
Removal of scars and scars with laser and ointments
What kind of scars can be removed with a laser. Removal of postoperative scars with a fractional laser. Recovery rules. Ointments for resorption of scars, recommendations for their use
Breast cancer - stages of development, symptoms, treatment, prognosis
The first signs of breast cancer. Stages of development and characteristics of breast cancer. General principles of treatment, postoperative therapy, prognosis.