Treatment for flu in pregnancy
Assessment and Treatment of Pregnant Women With Suspected or Confirmed Influenza
By reading this page you agree to ACOG's Terms and Conditions. Read terms
Number 753 (October 2018. Reaffirmed 2021)
Immunization, Infectious Disease, and Public Health Preparedness Expert Work Group
The Society for Maternal-Fetal Medicine endorses this document. This Committee Opinion was developed by the American College of Obstetricians and Gynecologists’ Immunization, Infectious Disease, and Public Health Preparedness Expert Work Group, in collaboration with members Geeta K. Swamy, MD and Laura E. Riley, MD.
ABSTRACT: Pregnant and postpartum women are at high risk of serious complications of seasonal and pandemic influenza infection. Pregnancy itself is a high-risk condition, making the potential adverse effects of influenza particularly serious in pregnant women. If a pregnant woman has other underlying health conditions, the risk of adverse effects from influenza is even greater. Antiviral treatment is necessary for all pregnant women with suspected or confirmed influenza, regardless of vaccination status. Obstetrician–gynecologists and other obstetric care providers should promptly recognize the symptoms of influenza, adequately assess severity, and readily prescribe safe and effective antiviral therapy for pregnant women with suspected or confirmed influenza. Over-the-phone treatment for low-risk patients is preferred to help reduce the spread of disease among other pregnant patients in the office. Obstetrician–gynecologists and other obstetric care providers should treat pregnant women with suspected or confirmed influenza with antiviral medications presumptively based on clinical evaluation, regardless of vaccination status or laboratory test results. Pregnant women with suspected or confirmed influenza infection should receive antiviral treatment with oseltamivir or zanamivir based on the current resistance patterns. Treatment within 48 hours of the onset of symptoms is ideal but treatment should not be withheld if the ideal window is missed.
 Because of the high potential for morbidity and mortality for pregnant and postpartum patients, the Centers for Disease Control and Prevention advises that postexposure antiviral chemoprophylaxis can be considered for pregnant women and women who are up to 2 weeks postpartum (including after pregnancy loss) who have had close contact with infectious individuals.
Because of the high potential for morbidity and mortality for pregnant and postpartum patients, the Centers for Disease Control and Prevention advises that postexposure antiviral chemoprophylaxis can be considered for pregnant women and women who are up to 2 weeks postpartum (including after pregnancy loss) who have had close contact with infectious individuals.
Recommendations
Obstetrician–gynecologists and other obstetric care providers should promptly recognize the symptoms of influenza, adequately assess severity, and readily prescribe safe and effective antiviral therapy for pregnant women with suspected or confirmed influenza.
Obstetrician–gynecologists and other obstetric care providers should treat pregnant women with suspected or confirmed influenza with antiviral medications presumptively based on clinical evaluation, regardless of vaccination status or laboratory test results.
Pregnant women with suspected or confirmed influenza infection should receive antiviral treatment with oseltamivir or zanamivir based on the current resistance patterns.

Based on previous influenza seasons, oseltamivir is the preferred treatment for pregnant women (75 mg orally twice daily for 5 days) assuming there is sufficient supply and the prevalence of resistant circulating viruses is low. Zanamivir also may be prescribed (two 5-mg inhalations [10 mg total] twice daily for 5 days), or alternatively peramivir may be administered (one 600-mg dose by intravenous infusion for 15–30 minutes).
Pregnant women who are not identified as high or moderate risk of complications but have symptoms suggestive of influenza infection can be prescribed antiviral treatment over the phone or in person in accordance with Centers for Disease Control and Prevention (CDC) guidelines.
Pregnant women without high-risk symptoms but with comorbidities (eg, asthma), obstetric issues (eg, preterm labor), or who are unable to care for themselves (eg, obtain prescription medications or unable to tolerate oral intake) should be seen as soon as possible in an ambulatory setting with resources to determine the severity of illness.

Because of the high potential for morbidity and mortality for pregnant and postpartum patients, the CDC advises that postexposure antiviral chemoprophylaxis can be considered for pregnant women and women who are up to 2 weeks postpartum (including after pregnancy loss) who have had close contact with infectious individuals.
Background
Pregnant and postpartum women are at high risk of serious complications of seasonal and pandemic influenza (flu) infection. Pregnancy itself is a high-risk condition, making the potential adverse effects of influenza particularly serious in pregnant women. If a pregnant woman has other underlying health conditions, the risk of adverse effects from influenza is even greater. Complications of flu include preterm delivery, pneumonia, hospital or intensive care unit admission, and maternal and fetal death 1 2. Influenza vaccination, which is an essential element of prenatal and postpartum care, is the most effective and safe way to prevent influenza infection and reduce the related maternal morbidity and mortality 3 4 5. Influenza vaccination rates during pregnancy have plateaued, with only approximately 50% of pregnant women receiving influenza vaccine and, to date, efforts to increase rates of vaccination have not been successful 6. Seasonal influenza vaccination effectiveness in pregnant women is similar to its efficacy among the general adult population and varies from season to season, depending on host characteristics (such as age and presence of comorbidities) and how well circulating influenza viruses match the viruses contained in the vaccine 4. Thus, although vaccination is an essential component of influenza prevention and can mitigate the severity of illness, no vaccine is 100% effective. Antiviral treatment is necessary for all pregnant women with suspected or confirmed influenza, regardless of vaccination status. For pregnant women who are already infected, treatment can reduce the severity of the flu. Obstetrician–gynecologists and other obstetric care providers should promptly recognize the symptoms of influenza (particularly once influenza virus circulation has been identified in the community), adequately assess severity, and readily prescribe safe and effective antiviral therapy for pregnant women with suspected or confirmed influenza 2.
Influenza vaccination rates during pregnancy have plateaued, with only approximately 50% of pregnant women receiving influenza vaccine and, to date, efforts to increase rates of vaccination have not been successful 6. Seasonal influenza vaccination effectiveness in pregnant women is similar to its efficacy among the general adult population and varies from season to season, depending on host characteristics (such as age and presence of comorbidities) and how well circulating influenza viruses match the viruses contained in the vaccine 4. Thus, although vaccination is an essential component of influenza prevention and can mitigate the severity of illness, no vaccine is 100% effective. Antiviral treatment is necessary for all pregnant women with suspected or confirmed influenza, regardless of vaccination status. For pregnant women who are already infected, treatment can reduce the severity of the flu. Obstetrician–gynecologists and other obstetric care providers should promptly recognize the symptoms of influenza (particularly once influenza virus circulation has been identified in the community), adequately assess severity, and readily prescribe safe and effective antiviral therapy for pregnant women with suspected or confirmed influenza 2.
Assessment of Pregnant Women With Influenza
Pregnant women with suspected influenza should be assessed based on a variety of symptoms, including but not limited to fever of 100.0°F or higher, cough, fatigue, headache, and body aches. It is important to note that not all people infected with influenza will develop a fever; therefore, the absence of fever should not rule out an influenza diagnosis Figure 1. Initial triage and treatment by telephone is acceptable to help reduce the spread of disease among other pregnant patients in the office.
Following symptom assessment, obstetrician–gynecologists and other obstetric care providers should ask patients questions to help determine the severity of the illness. Pregnant women who cannot maintain oral fluid intake, show signs of dehydration, are experiencing difficulty breathing or pain in the chest, or exhibit any signs of obstetric complications are considered moderate or high risk and should be referred immediately to an emergency department or equivalent setting. Pregnant women who are not identified as high or moderate risk of complications but have symptoms suggestive of influenza infection can be prescribed antiviral treatment over the phone or in person in accordance with CDC guidelines Figure 1. Over-the-phone treatment for low-risk patients is preferred to help reduce the spread of disease among other pregnant patients in the office. Pregnant women without high-risk symptoms but with comorbidities (eg, asthma), obstetric issues (eg, preterm labor), or who are unable to care for themselves (eg, obtain prescription medications or unable to tolerate oral intake) should be seen as soon as possible in an ambulatory setting with resources to determine the severity of illness.
Pregnant women who are not identified as high or moderate risk of complications but have symptoms suggestive of influenza infection can be prescribed antiviral treatment over the phone or in person in accordance with CDC guidelines Figure 1. Over-the-phone treatment for low-risk patients is preferred to help reduce the spread of disease among other pregnant patients in the office. Pregnant women without high-risk symptoms but with comorbidities (eg, asthma), obstetric issues (eg, preterm labor), or who are unable to care for themselves (eg, obtain prescription medications or unable to tolerate oral intake) should be seen as soon as possible in an ambulatory setting with resources to determine the severity of illness.
Treatment of Pregnant Women With Influenza
It is important to note that receipt of an annual influenza vaccine does not eliminate the possibility of acquiring influenza infection. Pregnant women with suspected or confirmed influenza infection should receive antiviral treatment with oseltamivir and acetaminophen for treatment of fever.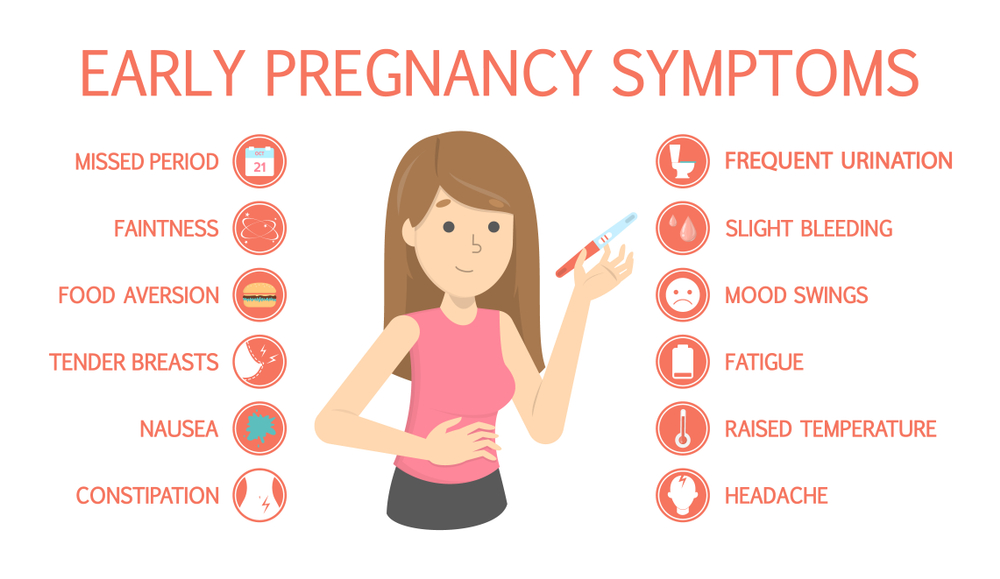 Zanamivir and peramivir are alternative approved influenza antiviral options for treatment. Pregnancy is not a contraindication to these antivirals 7. Based on previous influenza seasons, oseltamivir is the preferred treatment for pregnant women (75 mg orally twice daily for 5 days) assuming there is sufficient supply and the prevalence of resistant circulating viruses is low. Zanamivir also may be prescribed (two 5-mg inhalations [10 mg total] twice daily for 5 days), or alternatively peramivir may be administered (one 600-mg dose by intravenous infusion for 15–30 minutes) 7. Obstetrician–gynecologists and other obstetric care providers should check with their laboratory regarding requirements for testing and turnaround time. However, obstetrician–gynecologists and other obstetric care providers should not rely on test results to initiate treatment. Obstetrician–gynecologists and other obstetric care providers should treat pregnant women with suspected or confirmed influenza with antiviral medications presumptively based on clinical evaluation, regardless of vaccination status or laboratory test results.
Zanamivir and peramivir are alternative approved influenza antiviral options for treatment. Pregnancy is not a contraindication to these antivirals 7. Based on previous influenza seasons, oseltamivir is the preferred treatment for pregnant women (75 mg orally twice daily for 5 days) assuming there is sufficient supply and the prevalence of resistant circulating viruses is low. Zanamivir also may be prescribed (two 5-mg inhalations [10 mg total] twice daily for 5 days), or alternatively peramivir may be administered (one 600-mg dose by intravenous infusion for 15–30 minutes) 7. Obstetrician–gynecologists and other obstetric care providers should check with their laboratory regarding requirements for testing and turnaround time. However, obstetrician–gynecologists and other obstetric care providers should not rely on test results to initiate treatment. Obstetrician–gynecologists and other obstetric care providers should treat pregnant women with suspected or confirmed influenza with antiviral medications presumptively based on clinical evaluation, regardless of vaccination status or laboratory test results. Treatment within 48 hours of the onset of symptoms is ideal but treatment should not be withheld if the ideal window is missed 2 8. Recommendations for treatment with antivirals are based on information from previous influenza seasons. Obstetrician–gynecologists and other obstetric care providers should refer to CDC recommendations for treatment updates 9.
Treatment within 48 hours of the onset of symptoms is ideal but treatment should not be withheld if the ideal window is missed 2 8. Recommendations for treatment with antivirals are based on information from previous influenza seasons. Obstetrician–gynecologists and other obstetric care providers should refer to CDC recommendations for treatment updates 9.
Postexposure Chemoprophylaxis
Because of the high potential for morbidity and mortality for pregnant and postpartum patients, the CDC advises that postexposure antiviral chemoprophylaxis can be considered for pregnant women and women who are up to 2 weeks postpartum (including after pregnancy loss) who have had close contact with infectious individuals. The chemoprophylaxis recommendation is oseltamivir 75 mg once daily for 7–10 days depending on the source of exposure 9. Once signs or symptoms of influenza are present, early treatment is an alternative to prophylaxis. In addition, in women with frequent exposures, early treatment as opposed to prophylaxis may be considered 9.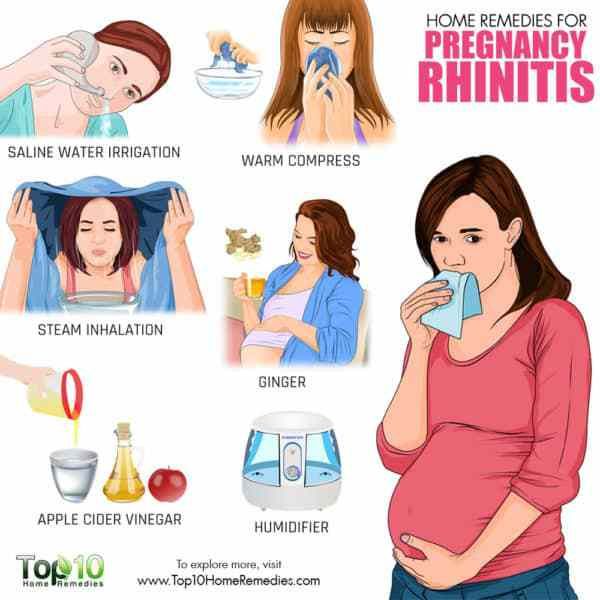 Finally, at-risk family members of patients with an influenza diagnosis should be referred to their health care providers for consideration of antiviral chemoprophylaxis.
Finally, at-risk family members of patients with an influenza diagnosis should be referred to their health care providers for consideration of antiviral chemoprophylaxis.
Conclusion
Pregnant women are disproportionately affected by influenza compared with the general population. It is critical for obstetrician–gynecologists and other obstetric care providers to be able to identify influenza in pregnant women and to understand the treatment protocol. Following this guidance can reduce morbidity and mortality related to influenza in pregnant women.
For More Information
The American College of Obstetricians and Gynecologists has identified additional resources on topics related to this document that may be helpful for obstetrician–gynecologists, other health care providers, and patients. You may view these resources at: www.acog.org/More-Info/Influenza-Assessment-and-Treatment.
These resources are for information only and are not meant to be comprehensive. Referral to these resources does not imply the American College of Obstetricians and Gynecologists' endorsement of the organization, the organization's website, or the content of the resource. The resources may change without notice.
Referral to these resources does not imply the American College of Obstetricians and Gynecologists' endorsement of the organization, the organization's website, or the content of the resource. The resources may change without notice.
References
- Callaghan WM, Creanga AA, Jamieson DJ. Pregnancy-related mortality resulting from influenza in the United States during the 2009–2010 pandemic. Obstet Gynecol 2015;126:486–90.
Article Locations:Article Location
- Oboho IK, Reed C, Gargiullo P, Leon M, Aragon D, Meek J, et al. Benefit of early initiation of influenza antiviral treatment to pregnant women hospitalized with laboratory-confirmed influenza. J Infect Dis 2016;214:507–15.
Article Locations:Article LocationArticle LocationArticle Location
- Influenza vaccination during pregnancy. ACOG Committee Opinion No. 732. American College of Obstetricians and Gynecologists. Obstet Gynecol 2018;131:e109–14.
Article Locations:Article Location
- Thompson MG, Li D, Shifflett P, Sokolow LZ, Ferber JR, Kurosky S, et al.
 Effectiveness of seasonal trivalent influenza vaccine for preventing influenza virus illness among pregnant women: a population-based case-control study during the 2010–2011 and 2011–2012 influenza seasons. Pregnancy and Influenza Project Workgroup. Clin Infect Dis 2014;58:449–57.
Effectiveness of seasonal trivalent influenza vaccine for preventing influenza virus illness among pregnant women: a population-based case-control study during the 2010–2011 and 2011–2012 influenza seasons. Pregnancy and Influenza Project Workgroup. Clin Infect Dis 2014;58:449–57.
Article Locations:Article LocationArticle Location
- Regan AK, Klerk Nd, Moore HC, Omer SB, Shellam G, Effler PV. Effectiveness of seasonal trivalent influenza vaccination against hospital-attended acute respiratory infections in pregnant women: a retrospective cohort study. Vaccine 2016;34:3649–56.
Article Locations:Article Location
- Ding H, Black CL, Ball S, Fink RV, Williams WW, Fiebelkorn AP, et al. Influenza vaccination coverage among pregnant women—United States, 2016–17 influenza season. MMWR Morb Mortal Wkly Rep 2017;66:1016–22.
Article Locations:Article Location
- Centers for Disease Control and Prevention. Influenza antiviral medications: summary for clinicians .
 Atlanta (GA): CDC; 2018. Available at: https://www.cdc.gov/flu/pdf/professionals/antivirals/antiviral-summary-clinician.pdf. Retrieved June 12, 2018.
Atlanta (GA): CDC; 2018. Available at: https://www.cdc.gov/flu/pdf/professionals/antivirals/antiviral-summary-clinician.pdf. Retrieved June 12, 2018.
Article Locations:Article LocationArticle Location
- Muthuri SG, Venkatesan S, Myles PR, Leonardi-Bee J, Al Khuwaitir TS, Al Mamun A, et al. Effectiveness of neuraminidase inhibitors in reducing mortality in patients admitted to hospital with influenza A h2N1pdm09 virus infection: a meta-analysis of individual participant data. PRIDE Consortium Investigators. Lancet Respir Med 2014;2:395–404.
Article Locations:Article Location
- Fiore AE, Fry A, Shay D, Gubareva L, Bresee JS, Uyeki TM. Antiviral agents for the treatment and chemoprophylaxis of influenza—recommendations of the advisory committee on immunization practices (ACIP). Centers for Disease Control and Prevention (CDC). MMWR Recomm Rep 2011;60:1–24.
Article Locations:Article LocationArticle LocationArticle Location
Published online on September 24, 2018.
Copyright 2018 by the American College of Obstetricians and Gynecologists. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, posted on the Internet, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without prior written permission from the publisher.
Requests for authorization to make photocopies should be directed to Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923, (978) 750-8400.
American College of Obstetricians and Gynecologists 409 12th Street, SW, PO Box 96920, Washington, DC 20090-6920
Assessment and treatment of pregnant women with suspected or confirmed influenza. ACOG Committee Opinion No. 753. American College of Obstetricians and Gynecologists. Obstet Gynecol 2018;132:e169–73.
This information is designed as an educational resource to aid clinicians in providing obstetric and gynecologic care, and use of this information is voluntary. This information should not be considered as inclusive of all proper treatments or methods of care or as a statement of the standard of care. It is not intended to substitute for the independent professional judgment of the treating clinician. Variations in practice may be warranted when, in the reasonable judgment of the treating clinician, such course of action is indicated by the condition of the patient, limitations of available resources, or advances in knowledge or technology. The American College of Obstetricians and Gynecologists reviews its publications regularly; however, its publications may not reflect the most recent evidence. Any updates to this document can be found on www.acog.org or by calling the ACOG Resource Center.
This information should not be considered as inclusive of all proper treatments or methods of care or as a statement of the standard of care. It is not intended to substitute for the independent professional judgment of the treating clinician. Variations in practice may be warranted when, in the reasonable judgment of the treating clinician, such course of action is indicated by the condition of the patient, limitations of available resources, or advances in knowledge or technology. The American College of Obstetricians and Gynecologists reviews its publications regularly; however, its publications may not reflect the most recent evidence. Any updates to this document can be found on www.acog.org or by calling the ACOG Resource Center.
While ACOG makes every effort to present accurate and reliable information, this publication is provided “as is” without any warranty of accuracy, reliability, or otherwise, either express or implied. ACOG does not guarantee, warrant, or endorse the products or services of any firm, organization, or person. Neither ACOG nor its officers, directors, members, employees, or agents will be liable for any loss, damage, or claim with respect to any liabilities, including direct, special, indirect, or consequential damages, incurred in connection with this publication or reliance on the information presented.
Neither ACOG nor its officers, directors, members, employees, or agents will be liable for any loss, damage, or claim with respect to any liabilities, including direct, special, indirect, or consequential damages, incurred in connection with this publication or reliance on the information presented.
All ACOG committee members and authors have submitted a conflict of interest disclosure statement related to this published product. Any potential conflicts have been considered and managed in accordance with ACOG's Conflict of Interest Disclosure Policy. The ACOG policies can be found on acog.org. For products jointly developed with other organizations, conflict of interest disclosures by representatives of the other organizations are addressed by those organizations. The American College of Obstetricians and Gynecologists has neither solicited nor accepted any commercial involvement in the development of the content of this published product.
Topics
Anti-infective agents Antiviral agents Human influenza Infectious diseases Infectious disease transmission Pregnancy Pregnancy complications Public health Therapeutics Therapeutic uses Treatment outcome
Influenza (flu) and pregnancy | March of Dimes
It’s safe to get the flu shot.
 It protects you and your baby from serious health problems during and after pregnancy.
It protects you and your baby from serious health problems during and after pregnancy.Pregnant women who get the flu are more likely than women who don’t get it to have problems, like preterm labor and premature birth.
If you think you have the flu, call your health care provider right away. Quick treatment can help prevent serious flu complications.
What is the flu?
Influenza (also called flu) is a virus that can cause serious illness. It’s more than just a runny nose and sore throat. The flu can make you very sick, and it can be especially harmful if you get it during or right after pregnancy.
How does the flu spread?
The flu spreads easily from person to person. When someone with the flu coughs, sneezes or speaks, the virus spreads through the air. You can get infected with the flu if you breathe it in or if you touch something (like a door handle or a phone) that has the flu virus on it and then touch your nose, eyes or mouth.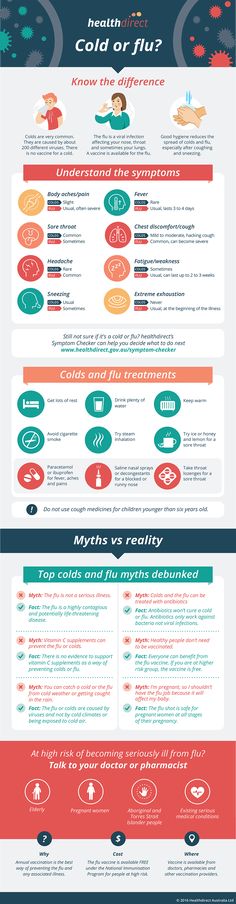
People with the flu may be able to infect others from 1 day before they get sick up to 5 to 7 days after. People who are very sick with the flu or young children may be able to spread the flu longer, especially if they still have symptoms.
How can the flu harm your pregnancy?
Health complications from the flu, like a lung infection called pneumonia, can be serious and even deadly, especially if you’re pregnant. If you get the flu during pregnancy, you’re more likely than other adults to have serious complications. It’s best to get a flu shot before you get pregnant. Getting a flu shot can help reduce your risk of getting the flu, having serious flu complications and needing treatment in a hospital.
Pregnant women who get the flu are more likely than women who don’t get it to have preterm labor (labor that happens before 37 weeks of pregnancy) and preterm birth (birth that happens before 37 weeks of pregnancy. Fever from the flu may be linked to birth defects, like neural tube defects, and other problems in your baby. A birth defect is a health condition that is present at birth. Birth defects change the shape or function of one or more parts of the body. They can cause problems in overall health, how the body develops, or in how the body works. Neural tube defects are birth defects of the brain and spinal cord.
A birth defect is a health condition that is present at birth. Birth defects change the shape or function of one or more parts of the body. They can cause problems in overall health, how the body develops, or in how the body works. Neural tube defects are birth defects of the brain and spinal cord.
How does the flu shot help protect you from flu?
The flu shot contains a vaccine that helps prevent you from getting the flu. The flu shot can’t cause the flu. It’s safe to get a flu shot any time during pregnancy, but it’s best to get it before flu season (October through May). Even though you’re more likely to get the flu during flu season, you can get it any time of year.
There are many different flu viruses, and they’re always changing. Each year a new flu vaccine is made to protect against three or four flu viruses that are likely to make people sick during the upcoming flu season. Protection from a flu shot only lasts about a year, so it’s important to get a flu shot every year. You can get the shot from your health care provider, and many pharmacies and work places offer it each fall. Use the HealthMap Vaccine Finder to find out where you can get the flu vaccine.
You can get the shot from your health care provider, and many pharmacies and work places offer it each fall. Use the HealthMap Vaccine Finder to find out where you can get the flu vaccine.
Is it safe to get a flu shot during pregnancy?
It’s safe for most pregnant women to get the flu shot. Tell your health care provider if you have any severe allergies or if you’ve ever had a severe allergic reaction to a flu shot. Severe allergic reactions to flu shots are rare. If you’re worried about being allergic to the flu shot, talk to your provider to make sure it’s safe for you.
Some flu vaccines are made with eggs. Most women with egg allergies can get the flu shot. But if you have severe egg allergies, get the shot in a medical setting (like a doctor’s office, hospital or clinic) from a provider who knows how to treat severe allergies and allergic reactions.
Pregnant women should not get the flu nasal spray. This is a spray that’s put in your nose.
What are signs and symptoms of the flu?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Common signs and symptoms of the flu include:
Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Common signs and symptoms of the flu include:
- Being very tired or sleepy (also called fatigue)
- Cough
- Fever (100 F or above), chills or body shakes. Not everyone who has the flu has a fever.
- Headache, or muscle or body aches
- Runny or stuffy nose
- Sore throat
- Vomiting (throwing up) or diarrhea (more common in children)
The flu often comes on quickly. Fever and most other symptoms can last a week or longer. But some people can be sick from the flu for a long time, including children, people older than 65, pregnant women and women who have recently had a baby.
Call 911 and get medical care right away if you have any of these signs or symptoms:
- Feeling your baby move less or not at all
- High fever that doesn’t go down after taking acetaminophen (Tylenol®). Don’t take any medicine without checking with your provider first.

- Pain or pressure in the chest or belly
- Sudden dizziness or confusion
- Trouble breathing or shortness of breath
- Vomiting that’s severe or doesn’t stop
- Flu signs or symptoms that get better but then come back with fever and a worse cough
How is the flu treated during pregnancy?
If you think you have the flu even if you’ve been vaccinated, call your health care provider right away. Your provider may prescribe an antiviral medicine to help prevent or treat the flu. Antivirals kill infections caused by viruses. They can make your flu milder and help you feel better faster. Antivirals also can help prevent serious flu complications, like pneumonia. For flu, antivirals work best if you take them within 2 days of having symptoms. Quick treatment with antiviral medicine can help prevent serious flu complications.
If you’ve had close contact with someone who has the flu during your pregnancy or in the 2 weeks after giving birth, tell your health care provider. Even if you don’t have signs or symptoms of flu, your provider may want to treat you with an antiviral medicine to help prevent you from getting the flu and having serious complications.
Even if you don’t have signs or symptoms of flu, your provider may want to treat you with an antiviral medicine to help prevent you from getting the flu and having serious complications.
Three medicines are approved in the United States to prevent or treat the flu in pregnant women and women who recently had a baby. Talk to your provider about which one is right for you:
- Oseltamivir (brand name Tamiflu®).This medicine comes as a capsule or liquid.
- Zanamivir (brand name Relenza®). This medicine is a powder that you breathe in by mouth. It isn’t recommended for people with breathing problems, like asthma.
- Peramivir (Rapivab®). This medicine is given through a needle into a vein (also called IV) by a health care provider.
If you have a fever, call your provider as soon as possible. Before taking any over-the-counter medication, be sure to check with your provider first. Not all medication is safe to take during pregnancy. If you have the flu, get lots of rest and drink plenty of fluids. You may not want to eat much. Try eating small meals to help your body get better.
You may not want to eat much. Try eating small meals to help your body get better.
How can you stop the flu from spreading?
When you have the flu, you can spread it to others. Here’s what you can do to help prevent it from spreading:
- Stay home when you’re sick and limit contact with others.
- Cough or sneeze into a tissue or into your arm. Throw used tissues in the trash.
- Try not to touch your eyes, nose or mouth.
- Wash your hands with soap and water before touching anyone. You also can use alcohol-based hand sanitizers. Use enough hand sanitizer so that it takes at least 15 seconds for your hands to dry.
- Wash your dishes and utensils well with hot soapy water, or in a dishwasher if you have one.
- Don’t share your dishes, glasses, utensils or toothbrush.
Why is the flu so harmful during pregnancy?
The flu can be dangerous during pregnancy because pregnancy affects your immune system, heart and lungs. Your immune system is your body’s way of protecting itself from illnesses and diseases. When your body senses something like a virus that can harm your health, your immune system works hard to fight the virus.
Your immune system is your body’s way of protecting itself from illnesses and diseases. When your body senses something like a virus that can harm your health, your immune system works hard to fight the virus.
When you’re pregnant, your immune system isn’t as quick to respond to illnesses as it was before pregnancy. A lowered immune system means you’re more likely get sick with viruses like the flu.
During pregnancy, your lungs need more oxygen, especially in the second and third trimesters. Your growing belly puts pressure on your lungs, making them work harder in a smaller space. You may even find yourself feeling shortness of breath at times. Your heart is working hard, too. It’s busy supplying blood to you and your baby. All of this means your body is stressed during pregnancy. This stress on your body can make you more likely to get the flu. If you’re pregnant or had a baby within the last 2 weeks, you’re more likely than other women to have serious health problems from the flu.
More information
Centers for Disease Control and Prevention Flu & Pregnancy
Flu.gov
What is the Flu? Common Influenza Questions (familiesfightingflu.org)
Last reviewed: November, 2022
Colds during pregnancy: how to treat?
Any cold or respiratory disease in early pregnancy, during the primary formation of the fetus, can lead to unpredictable consequences and complications. The matter is complicated by the fact that most medications are absolutely contraindicated for use during gestation.
In this regard, the treatment and prevention of colds in pregnant women is an important issue, which should be approached especially responsibly! The main thesis is: be careful with medicines and apply mild preventive measures based on alternative medicine methods to avoid respiratory diseases and flu.
"One for two - immunity"
This is a very fragile system, it is not necessary to interfere in its work, but it is necessary to support and strengthen it. Pregnancy belongs to the category of special, albeit temporary, conditions during which a woman needs additional protection.
Pregnancy belongs to the category of special, albeit temporary, conditions during which a woman needs additional protection.
This issue will help simple recommendations that are available to everyone:
• During the period of frequent weather changes, it is necessary to dress warmer, paying special attention to footwear.
• During an epidemic, it is better for a pregnant woman to refrain from being in crowded places - transport, metro, shops and hospitals. If there is an urgent need, to prevent possible infection, a protective respiratory mask should be worn before leaving the house.
• Be especially careful about hygiene after visiting the street and public places. Upon returning home, the first thing to do is wash your hands thoroughly.
Interesting: More than 90% of all acute respiratory infections are caused by viruses, about 10% are bacteria and other pathogens. Accordingly, any soap can be used, not necessarily antibacterial.
• Before going outside, you can lubricate the nasal mucosa with oxolin ointment. Upon returning home, flush the upper respiratory tract with soda solution.
• Rationalization of nutrition and intake of vitamins will strengthen the immune defense. It is especially useful to eat fruits and vegetables that are enriched with vitamins and have not undergone heat treatment.
Interesting: our grandmothers used to say: in order not to get sick, you need to drink chicken broth! Strange, but until recently, scientists did not attach much importance to this prophylactic. Pulmonologist Stefan Rennard decided to find out if this was true or not. The professor conducted a study and proved that the use of chicken broth affects the mobility of neutrophils, white blood cells that protect the body from infections and activate the immune system.
- Vitamins can be taken using ready-made pharmaceutical multivitamin complexes.
 Before choosing a drug, you should consult your doctor.
Before choosing a drug, you should consult your doctor. - Compliance with the regimen and duration of sleep - at least 9 hours a day. The possibility of psychotraumatic situations should be minimized.
- Maintaining cleanliness in the living quarters (ventilation, wet cleaning).
- Air humidification is an important aspect in the prevention of influenza and respiratory diseases. If air conditioners or heaters are used in the house of a pregnant woman, it would be best to purchase a mechanical humidifier.
Medications for prevention
- Grippferon - a drug in the form of drops for the nose, which provides prevention and treatment of influenza, is not contraindicated for pregnant and lactating women. The medicine stimulates an increase in immunity, has a pronounced antiviral effect that can protect against colds, infections and influenza varieties.
- Ascorbic acid - can be used as a separate source of vitamin C in a synthetic version, with a reduced daily intake from food.
 Ascorbic acid not only prevents infection, but also fights viruses that have already entered the body of a woman.
Ascorbic acid not only prevents infection, but also fights viruses that have already entered the body of a woman. - Viferon - nasal ointment, which is prescribed for the prevention of influenza and respiratory infections during an epidemic. The ointment has protective and immunomodulatory effects, and also allows you to deal with disorders that are already occurring in the body at the time of use. Viferon in the form of a nasal ointment has no contraindications for use in pregnant women at any time, including the first trimester.
- Aquamaris is a natural drug in the form of a nasal spray that allows you to moisturize the nasal mucosa, thereby reducing the risk of influenza viruses entering the nasal cavity.
I would like to say a few words about such a method of prevention as vaccination. Most often, the expectant mother may be at risk of infection due to the annual influenza epidemic. This disease is dangerous for a pregnant woman precisely because of its complications: pneumonia, bronchitis, otitis media.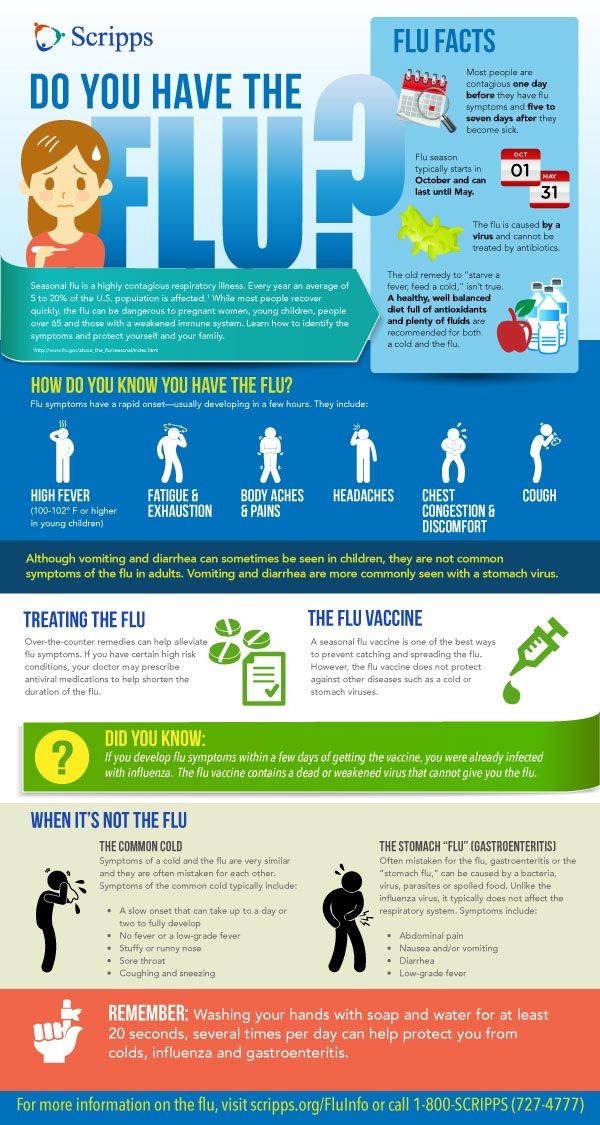 Influenza in a pregnant woman can also affect the health of the fetus. Most of all, it is dangerous in the early stages of pregnancy, when the tissues and organs of the human embryo are laid and formed. Viral intoxication or drug exposure can lead to pathology of the child's organs. In later pregnancy, there is a risk of infection of the fetus.
Influenza in a pregnant woman can also affect the health of the fetus. Most of all, it is dangerous in the early stages of pregnancy, when the tissues and organs of the human embryo are laid and formed. Viral intoxication or drug exposure can lead to pathology of the child's organs. In later pregnancy, there is a risk of infection of the fetus.
The most dangerous consequence of influenza in a pregnant woman is threatened miscarriage or premature birth!
It is quite natural that expectant mothers often wonder whether or not to vaccinate.
Studies have concluded that the use of inactivated ("killed") influenza vaccines does not have a teratogenic effect on the fetus and does not harm the health of a pregnant woman. After consulting with your doctor about such an inoculation, you can come to an optimal solution. If an influenza epidemic is inevitable, and the pregnant woman has no contraindications, then the vaccine should be given. If a pregnant woman has a negligible risk of infection, she does not come into contact with a large number of people, or is opposed to vaccination, then you can not do it. According to research, it is known that vaccination of mothers reduces the risk of influenza infection of a born child by 63%. Seasonal influenza prevention is carried out in September, October. Vaccinations for pregnant women are recommended from the second trimester of pregnancy.
According to research, it is known that vaccination of mothers reduces the risk of influenza infection of a born child by 63%. Seasonal influenza prevention is carried out in September, October. Vaccinations for pregnant women are recommended from the second trimester of pregnancy.
In the period of a planned pregnancy, a flu shot is given 1 month before it: the formation of immunity occurs 2-4 weeks. Protection after vaccination lasts about a year.
If infection does occur, action should be taken immediately if at least one symptom of the disease is detected. The health of a pregnant woman and her unborn child depends entirely on her responsibility and respect for her own body.
Proven folk remedies will be used first. Since pregnant women cannot steam their legs, steam their hands, and this will facilitate nasal breathing. Bundle up, put on woolen socks and crawl under the covers: warmth, peace and sleep are good for colds. Do not forget to drink plenty of water - hot green tea with lemon and honey, lime blossom tea, cranberry juice, rosehip broth, dried fruit compote. Ginger in the form of tea also helps, not only with catarrhal symptoms, but with nausea in the morning.
Ginger in the form of tea also helps, not only with catarrhal symptoms, but with nausea in the morning.
Various hot milk drinks are also suitable. Honey can be added to milk, and it is best to boil it on onions. It must be emphasized right away that not all herbs for colds during pregnancy can be used. Here is a list of medicinal plants that are contraindicated: aloe, anise, barberry, elecampane (grass and root), sweet clover, oregano, St. John's wort, strawberries (leaves), viburnum (berries), raspberries (leaves), lemon balm, lovage, wormwood, licorice ( root), celandine, sage. Accordingly, preparations containing these plants should not be taken.
The use of medicines for colds during pregnancy must be treated with great care!
It is contraindicated to use the following drugs : Pertussin, Tussin plus, Joset, Glycodin, Ascoril, Travisil, Broncholitin, ACC, Grippeks, Codelac, Terpinkod. Do not use lozenges and lozenges for sore throat or cough are also undesirable due to the likelihood of allergic reactions.
Spray Pinosol, judging by the components indicated in the instructions, is not dangerous during pregnancy. However, the essential oils contained in the preparation - pine, peppermint, eucalyptus, thymol, guaiazulene (wormwood oil) - can lead to an allergic reaction with swelling of the nasal mucosa.
Viferon suppositories are allowed to be used only after 14 weeks from the start of conception. This drug contains recombinant human interferon alpha-2, ascorbic acid and alpha-tocopherol acetate and has antiviral, immunomodulatory and antiproliferative effects. It is used in the treatment of various infectious and inflammatory diseases in adults and children (including newborns). In the form of an ointment, Viferon is used to treat herpetic lesions of the skin and mucous membranes. The ointment is applied in a thin layer to the affected areas of the skin 3-4 times a day for 5-7 days.
The homeopathic preparation Stodal, which includes predominantly herbal ingredients, acts on various types of cough and has an expectorant and bronchodilator effect.
Viburkol - homeopathic suppositories - have analgesic, anti-inflammatory, sedative, antispasmodic action. They are prescribed in the complex therapy of acute respiratory viral infections and other uncomplicated infections (including in newborns), as well as in inflammatory processes of the upper respiratory tract and inflammatory diseases of the genitourinary system.
So, you can try to eliminate a slight ailment on your own, but there are conditions under which you need to call a doctor at home:
- Prolonged fever;
- Myalgia, fatigue, fatigue, general malaise;
- Difficulty breathing, nasopharyngeal lumps and dry or wet barking cough;
- A pregnant woman is troubled by severe pressing headache.
In conclusion, I would like to emphasize the importance of treating chronic diseases before pregnancy, a healthy lifestyle during childbearing and following all doctor's orders.
I wish expectant mothers and their loved ones to try to maintain a good mood: optimists live longer and happier, they are more productive.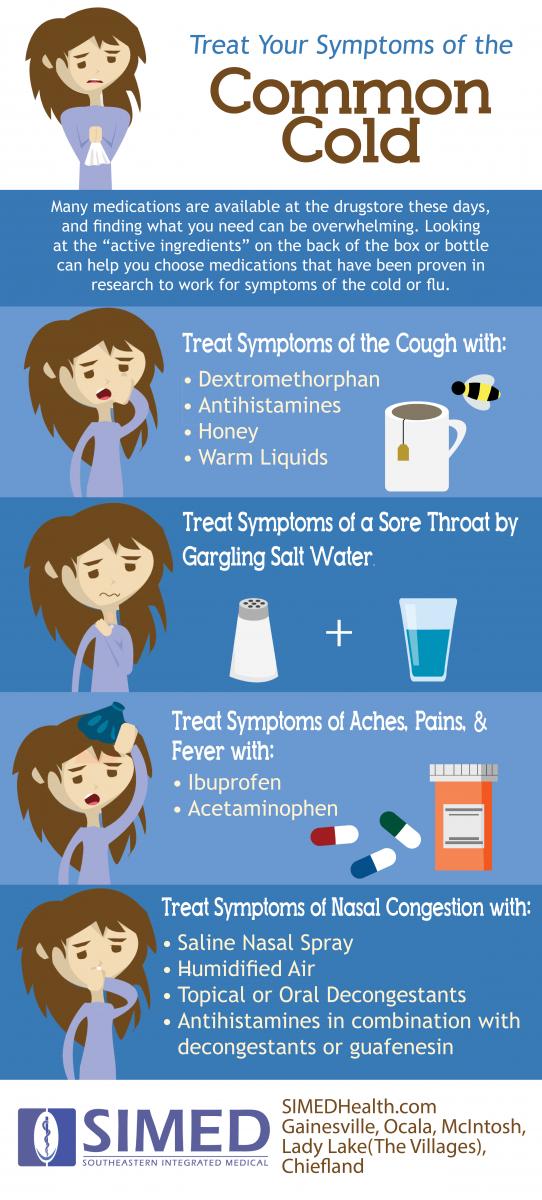 Remember your victories and pleasant moments more often and everything will be fine!
Remember your victories and pleasant moments more often and everything will be fine!
Cold during pregnancy, what can pregnant women with a cold, how to treat if the temperature, what you can drink.
Cold treatment during pregnancy
Acute respiratory diseases, also called colds, can also occur in pregnant women. Over the entire period of bearing a child, approximately 2/3 of expectant mothers suffer one or more episodes of a cold, which can have a course of varying severity. In most cases, colds are caused by viruses. 1
A cold while carrying a child can adversely affect its development. Oxygen deficiency due to a runny nose negatively affects the baby. At the same time, the treatment of a cold is fraught with difficulties - pregnant women should not take many medicines, as they can also affect the development of the fetus.
Causes and risk factors
Most often, pregnant women get sick with a cold in the autumn-winter-spring periods. It is during these seasons that flu and SARS epidemics are observed. The main cause of the development of a cold are pathogens from the group of rhinoviruses, adenoviruses, enteroviruses, as well as influenza and parainfluenza viruses. Bacteria usually lead to the development of lower respiratory tract infections - tracheitis, bronchitis, etc.
It is during these seasons that flu and SARS epidemics are observed. The main cause of the development of a cold are pathogens from the group of rhinoviruses, adenoviruses, enteroviruses, as well as influenza and parainfluenza viruses. Bacteria usually lead to the development of lower respiratory tract infections - tracheitis, bronchitis, etc.
Risk factors include various concomitant diseases in pregnant women. These can be diseases of the cardiovascular, digestive, immune, endocrine and other systems. Respiratory diseases are considered the most dangerous risk factor, especially if they occur in a chronic form. Pregnancy itself is also a risk factor, since in this natural state for a woman, immunity decreases and protective mechanisms weaken. 1
Cold risk for pregnant women
Cold pathogens initially enter the upper respiratory tract (usually the nasal cavity) and begin to actively multiply in the epithelium of the mucous membrane. As a result, an inflammatory reaction develops, which leads to the appearance of characteristic symptoms - a runny nose, nasal congestion and difficulty in nasal breathing.
In case of a severe course of a cold (flu), other parts of the respiratory system may also be affected with the development of more serious complications that affect the health of the mother. These complications can also affect the course of pregnancy, leading to conditions such as:
- Fetal malformations.
- Miscarriages.
- Intrauterine infections.
- Intrauterine growth retardation.
- Placental abruption.
- Fetal hypoxia.
The effect of a cold on pregnancy can occur in a variety of ways. First of all, any infection leads to a change in the functioning of the immune system, namely, to the development of immunodeficiency. Against the background of an already existing immunodeficiency during pregnancy, such changes can lead to the activation of diseases that have been in a “dormant” state for a long time (allergies, bronchial asthma, etc.). In addition, ARI pathogens have a toxic effect on the body of the expectant mother, which manifests itself in a change in the circulatory system.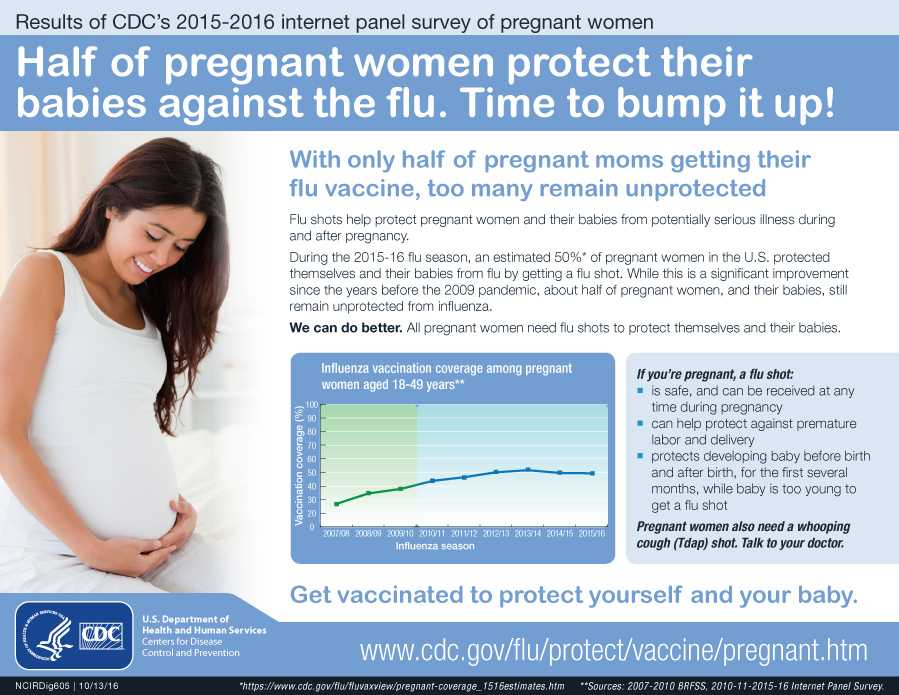 As a result, the risk of developing thrombosis or bleeding increases. Toxic effects can lead to oxygen starvation of the mother and fetus, which is also accompanied by an increased risk of complications.
As a result, the risk of developing thrombosis or bleeding increases. Toxic effects can lead to oxygen starvation of the mother and fetus, which is also accompanied by an increased risk of complications.
Fortunately, acute respiratory infections in pregnant women usually occur in a mild form, like a cold. 1 Therefore, when prescribing timely treatment for colds during pregnancy, health risks can be reduced to a minimum.
Pregnancy 1st trimester
The most dangerous period. At this time, the organs of the fetus are just being formed, so the risk of pathology is high. In addition, the onset of gestation is accompanied by a decrease in the mother's immunity. At this stage, prevention is very important.
Complications that may require antibiotics are no less dangerous. It is advisable to treat a cold during pregnancy using rinsing the nose and throat with solutions of sea water, bed rest and drinking plenty of water.
Pregnancy 2nd trimester
In this period, the placenta is formed, as well as the main organs of the child, so the risks of the disease are less. The therapy is predominantly symptomatic: washing the nose and throat with solutions of sea water, antipyretic at high temperatures.
The therapy is predominantly symptomatic: washing the nose and throat with solutions of sea water, antipyretic at high temperatures.
Pregnancy 3rd trimester
It is characterized by more severe symptoms, because the woman's body at this stage has to work for two. The disease can provoke premature birth, so bed rest is recommended. For the treatment of colds, seawater solutions are also used to wash the nose and throat. Additionally, you can use other drugs that are allowed during pregnancy, which are prescribed by a doctor.
Features of the course of a cold during pregnancy
In pregnant women, acute respiratory infections can have a long course. The causative agents of infections from the upper respiratory tract, together with the blood, enter the placenta, where they begin to multiply actively. This is associated with a high risk of fetal complications. 2
The symptoms of a cold during pregnancy are the same as those of other people. These include cough, runny nose, sore throat, nasal congestion. Also, a cold during pregnancy can be manifested by an increase in body temperature. Along with this symptom, there are complaints of weakness, fatigue, poor appetite.
These include cough, runny nose, sore throat, nasal congestion. Also, a cold during pregnancy can be manifested by an increase in body temperature. Along with this symptom, there are complaints of weakness, fatigue, poor appetite.
Prevention
Difficulties in treatment make prevention especially relevant. A product such as Aqualor can be used as a prophylaxis for washing the nasal cavity and removing pathogens of respiratory infections from it in the autumn-winter-spring period. It helps not only to prevent, but also to help treat the disease at the first symptoms.
Danger
Some viruses pose a threat to the fetus, they can cause changes in its development. Also, the disease is dangerous for its complications, so the treatment of a cold at home should be carried out only after consulting a doctor. A timely diagnosed cold in the nose allows you to stop the spread of infection, prevents the development of bronchitis, otitis media and other complications.
What to do at the first symptoms of a cold
Like the treatment of a cold in children, a disease in pregnant women requires medical supervision. You can help your body with a light plant-based diet, plenty of fluids, and regular nose and throat rinsing.
Aqualor sprays can help treat colds and runny nose: they remove pathogens from the surface of the mucous membrane of the nose and throat, cleanse the nose of crusts and excess mucus, moisturize the mucous membrane and create all the conditions for recovery.
How to treat a pregnant woman for a cold
The first question that worries expectant mothers is how to treat a cold during pregnancy so as not to harm the baby? "Classic" drugs in this case are not always used due to the lack of information about their safety. In some cases, women themselves refuse any drugs for fear of affecting the course of pregnancy. Therefore, the treatment of a cold in such cases begins with general recommendations. The main requirements are plenty of fluids, rest, light meals and cleansing of the nasopharynx. Treatment during illness with fever includes the use of antipyretics prescribed by a doctor. It is important to provide assistance as soon as possible and prevent the development of complications.
The main requirements are plenty of fluids, rest, light meals and cleansing of the nasopharynx. Treatment during illness with fever includes the use of antipyretics prescribed by a doctor. It is important to provide assistance as soon as possible and prevent the development of complications.
Exact treatment regimens are selected based on the causes and characteristics of the course of a cold in a particular patient. The disease can be caused by both viruses and bacteria, and it can occur in acute and chronic forms. Also, do not forget about possible complications that may require more complex and lengthy treatment.
In almost all cases, the treatment of a cold at home can be started with a universal method - irrigation of the mucous membrane with a solution of sea water. The unique mineral composition activates natural defenses, the optimal water-salt balance creates conditions for the normal functioning of tissues.
Aqualor refers to those drugs that are allowed and recommended for pregnant women for treatment. The product is based on sea water, improves nasal breathing, prevents maternal and fetal hypoxia.
The product is based on sea water, improves nasal breathing, prevents maternal and fetal hypoxia.
The drug is available both in 150 ml bottles, suitable for long-term use at home, and in 50 ml mini-formats, which are convenient to take with you. All Aqualor products are suitable for pregnant women, with the exception of Aqualor Protect. The choice is made depending on the causes and characteristics of the course of a cold. Aqualor Soft spray is suitable for regular nasal rinsing, Aqualor Forte can be used to relieve congestion. With a severe runny nose, you can use the Aqualor Active Forte spray, with a prolonged runny nose - Aqualor Active Soft. The products of the Aqualor Active line are enriched with CO 9 bubbles0206 2 that contribute to the destruction of bacterial biofilms, which can cause prolonged and severe rhinitis.
What not to do
It is important to understand that therapy in pregnant women is very different from usual. It is strictly forbidden to take medicines without the consent of the doctor. Many drugs are contraindicated during pregnancy, others are prescribed only if the potential benefit outweighs the harm.
Many drugs are contraindicated during pregnancy, others are prescribed only if the potential benefit outweighs the harm.
Symptomatic relief requires a cold without fever. Her treatment excludes drugs that include alcohol, antibiotics, sulfonamides. Their appointment should be supervised by a doctor.
Flushing and drinking plenty of water are good if the first signs of a cold are observed. Treatment of complications is always carried out by a specialist. Help is urgently needed if:
- high temperature (above 39 degrees) or it does not go astray;
- there is persistent vomiting;
- uterine tone or contractions are observed;
- there is bloody discharge from the vagina;
- on the fifth day there is no improvement, the general condition worsens;
- has rashes.
Terminals
Therapy of acute respiratory infections in pregnant women, as well as the treatment of a cold during breastfeeding, requires caution in prescribing medications.