Risk of ntd
Neural tube defects | March of Dimes
Neural tube defects (NTDs) are birth defects of the brain and spinal cord. NTDs can cause serious problems for babies.
To help prevent NTDs, take a vitamin supplement that has 400 micrograms of folic acid in it every day, even if you’re not trying to get pregnant.
If you’re at high risk for NTDs, take 4,000 micrograms of folic acid every day. Talk to your provider about how to get this much safely.
Your risk for having a baby with an NTD is higher if you, your partner or your family members have an NTD, or if you’ve had a baby with an NTD.
Folic acid helps prevent NTDs only if you take it before and in the first weeks of pregnancy.
What are neural tube defects?
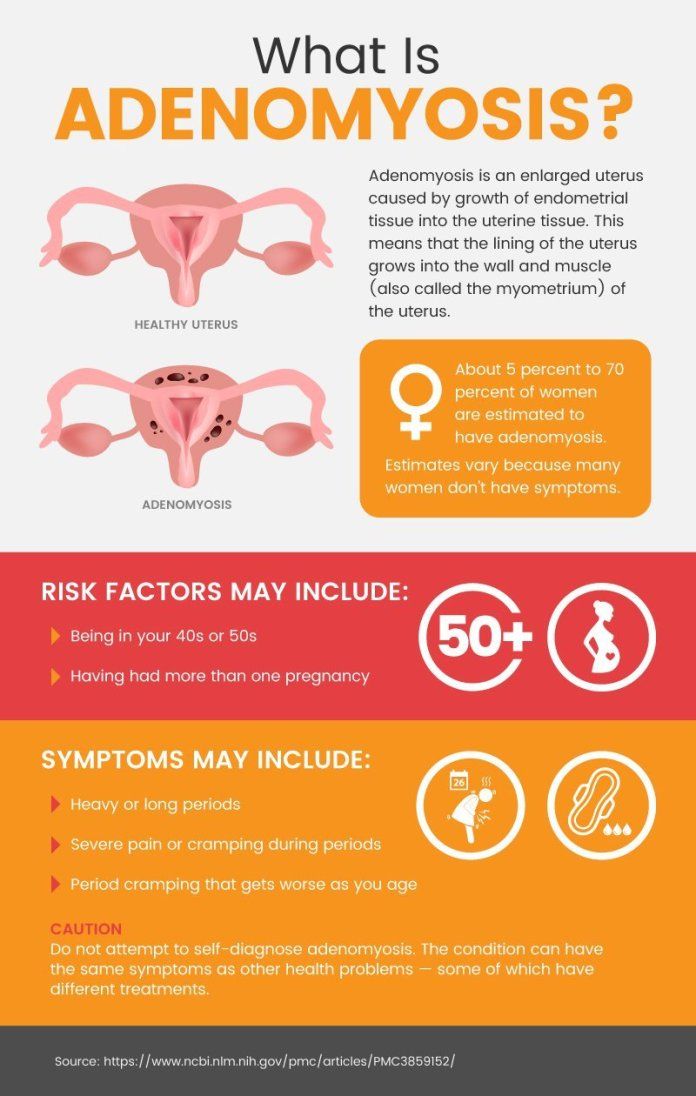
Neural tube defects (also called NTDs) are birth defects of the brain and spinal cord. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works.
A baby’s neural tube normally starts out as a tiny, flat ribbon that turns into a tube by the end of the first month of pregnancy. If the tube doesn’t close completely, an NTD can happen. NTDs can cause serious problems for babies, including death.
NTDs happen in about 3,000 pregnancies each year in the United States. Hispanic women are more likely than non-Hispanic women to have a baby with an NTD.
The two most common NTDs are spina bifida and anencephaly. Spina bifida affects about 1,500 babies a year in the United States. If your baby has spina bifida, the tiny bones of the spine don’t close completely, and part of the spinal cord pokes through the spine. Children with spina bifida may have paralyzed legs (not able to move) and problems controlling their bladder and bowel (going to the bathroom). Milder forms of spina bifida may cause fewer problems for children.
Anencephaly is one of the most severe NTDs. It affects about 1,000 babies each year in the United States. Anencephaly is caused when the upper part of the neural tube that forms the brain doesn’t close completely. Babies with this condition are missing major parts of the brain, skull and scalp. They do not survive long after birth, usually for just a few hours. Girls are 3 times more likely than boys to have anencephaly.
It affects about 1,000 babies each year in the United States. Anencephaly is caused when the upper part of the neural tube that forms the brain doesn’t close completely. Babies with this condition are missing major parts of the brain, skull and scalp. They do not survive long after birth, usually for just a few hours. Girls are 3 times more likely than boys to have anencephaly.
Taking folic acid before and during early pregnancy can help prevent NTDs in your baby. Folic acid is a B vitamin that every cell in your body needs for normal growth and development.
What causes NTDs?
We’re not exactly sure what causes NTDs. Experts think some may be caused by genetics. This means an NTD can be passed from parents to children through genes. Genes are part of your body’s cells that stores instructions for the way your body grows, looks and works.
NTDs also may be caused by things in your environment, which includes where you live, where you work, the kinds of foods you eat or have access to and how you like to spend your time. Some things in your environment can be harmful to a pregnancy, like certain drugs, cigarette smoke, air pollution and lead.
Some things in your environment can be harmful to a pregnancy, like certain drugs, cigarette smoke, air pollution and lead.
Are you at risk for having a baby with an NTD?
Any woman can have a baby with an NTD. But there are things that may make you more likely than other women to have a baby with an NTD. These are called risk factors.
Your risk for having a baby with an NTD is higher if:
- You’ve had a baby with an NTD. If you’ve had a baby with an NTD, there’s a 2- to 3-percent chance of having a baby with an NTD in another pregnancy. A genetic counselor can help you understand your risk for having a baby with an NTD. This is someone who is trained to help you understand medical conditions that run in families, and how they can affect your health and your baby’s health.
- You or your partner has an NTD, your partner has a child with an NTD or someone in either of your families has an NTD. This means you have a family history of NTDs.
 Use the March of Dimes Family Health History Form to keep track of health conditions, including NTDs,that may run in your family. Fill it out and share it with your health care provider or genetic counselor.
Use the March of Dimes Family Health History Form to keep track of health conditions, including NTDs,that may run in your family. Fill it out and share it with your health care provider or genetic counselor.
Other risk factors for NTDs include:
- Taking certain anti-seizure medicines. Talk to your health care provider before you get pregnant about how the medicine may affect your pregnancy.
- Obesity. Some studies show that being obese increases your risk for having a baby with an NTD. If you’re obese, you have an excess amount of body fat and your body mass index (BMI) is 30 or higher. To find out your BMI, go to cdc.gov/bmi. Talk to your provider about getting to a healthy weight before pregnancy.
- Diabetes. If your diabetes is uncontrolled, you may be at increased risk for having a baby with an NTD. Eating healthy foods and being active every day can help you keep your diabetes under control.

- Using opioids in the first 2 months of pregnancy. Opioids are highly addictive drugs. Your provider may prescribe an opioid to you as a painkiller if you’ve been injured or had surgery. Common prescription opioids include codeine, hydrocodone and oxycodone. These often are sold and used illegally. If you take any opioid during pregnancy, it can cause serious problems for your baby, like premature birth and drug withdrawal called neonatal abstinence syndrome (also called NAS). If you’re pregnant and taking any drug or medicine that may be an opioid, tell your health care provider right away.
- A high body temperature early in pregnancy. This may be caused by a fever or by spending a lot of time in a hot tub or sauna. If you’re pregnant, stay out of hot tubs and saunas. If you do use them, limit the time to less than 10 minutes.
How can you help prevent NTDs in your baby?
Taking folic acid before and during early pregnancy can help prevent NTDs in your baby. NTDs happen in the first month of pregnancy, before you may know you’re pregnant. This is why it’s important to have enough folic acid in your body before you get pregnant.
NTDs happen in the first month of pregnancy, before you may know you’re pregnant. This is why it’s important to have enough folic acid in your body before you get pregnant.
Most women
To help prevent NTDs in your baby, take a vitamin supplement with 400 mcg of folic acid every day before getting pregnant. A supplement is a product you take to make up for certain nutrients that you don’t get enough of in the foods you eat. Start taking this amount of folic acid each day at least 1 month before pregnancy and through the first 12 weeks of pregnancy. Your folic acid supplement can be:
- A multivitamin. This is a pill that contains many vitamins and other nutrients that help your body stay healthy.
- A prenatal vitamin. This is a multivitamin that has nutrients you need during pregnancy. Your health care provider may give you a prescription for prenatal vitamins, or you can get them over the counter without a prescription.
- A supplement that contains just folic acid
Take a vitamin supplement with 400 mcg of folic acid each day, even if you’re not trying to get pregnant.
Women at high risk for NTDs
If you’re at high risk for having a baby with an NTD, it’s recommended you take 4,000 mcg of folic acid each day to help prevent an NTD. Start taking 4,000 mcg 3 months before you get pregnant through 12 weeks of pregnancy. You’re at high risk if:
- You’ve had a pregnancy with an NTD in the past.
- You or your partner has an NTD.
- Your partner has a child with an NTD.
Studies show that taking 4,000 mcg of folic acid before and during early pregnancy can help reduce your risk of having another baby with an NTD by about 70 percent. Ask your provider how to safely get this much folic acid. It’s not safe to take several multivitamins or prenatal vitamins because you can get too much of other nutrients, which may be harmful to your health. Your provider can help you figure out the best and safest way for you to get the right amount of folic acid.
Can you get folic acid from food?
Yes! You can get folic acid from foods that are fortified with folic acid. Fortified means a food has folic acid added to it. Check the product label to see how much folic acid you get in each serving. Look for the word “fortified” or “enriched” on labels on foods like:
- Bread
- Breakfast cereal
- Cornmeal
- Flour
- Pasta
- Products made from a kind of flour called corn masa, like tortillas, tortilla chips, taco shells, tamales and pupusas
- White rice
Some fruits and vegetables are good sources of folic acid. When folic acid is naturally in a food, it’s called folate. Foods that are good sources of folate are:
- Beans, like lentils, pinto beans and black beans
- Leafy green vegetables, like spinach and Romaine lettuce
- Asparagus
- Broccoli
- Peanuts (But don’t eat them if you have a peanut allergy.
 )
) - Citrus fruits, like oranges and grapefruit
- Orange juice (100 percent juice is best. This means one serving of juice is equal to one serving of fruit.)
It’s hard to get all the folic acid you need from food. Even if you eat foods that have folic acid in them, take your vitamin supplement each day, too.
Can you find out if your baby has an NTD before birth?
Yes. You can get prenatal tests (medical tests you get during pregnancy) called screening tests to find out if your baby is at increased risk of having an NTD. Screening tests for NTDs include:
- Maternal blood screening (also called a quad screen). It’s called a quad screen because it measures four substances in your blood. The test is done between 15 to 22 weeks of pregnancy.
- Ultrasound. This test uses sound waves and a computer screen to show a picture of your baby inside the womb. You usually get an ultrasound at 16 to 20 weeks of pregnancy.
If a screening test shows an increased risk of NTDs, your provider may recommend a diagnostic test to find out for sure if your baby has an NTD. Diagnostic tests for NTDs include:
Diagnostic tests for NTDs include:
- Amniocentesis. In this test, your provider takes some amniotic fluid from around your baby in the uterus (womb) to check for birth defects, like NTDs, in your baby. You can get this test at 15 to 20 weeks of pregnancy.
- Detailed ultrasound of your baby’s skull and spine
If you find out that your baby has an NTD, talk to your health care provider to learn more about your baby’s condition and options for birth and treatment. For example:
- You can plan to have your baby in a hospital that specializes in caring for babies with NTDs. This way your baby can have any necessary surgery or treatment soon after birth.
- You can decide whether to have a vaginal or cesarean birth (also called c-section). During vaginal birth, the uterus contracts to help push the baby out through the vagina. A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. In some cases, a c-section may be safer for you and your baby than vaginal birth.

- If your baby has spina bifida, you can find out about surgery for your baby in the womb before birth. Surgery to repair spina bifida in the womb before birth is more effective than surgery after birth.
For more information
American Academy of Pediatrics
Spina Bifida Association
Centers for Disease Control and Prevention
Last reviewed: February, 2022
Risk factors associated with neural tube defects in infants referred to western Iranian obstetrical centers; 2013–2014
1. Onrat ST, Seyman H, Konuk M. Incidence of neural tube defects in Afyonkarahisar, Western Turkey. Genet Mol Res. 2009;8(1):154–61. [PubMed] [Google Scholar]
2. Seidahmed MZ, Abdelbasit OB, Shaheed MM, Alhussein KA, Miqdad AM, Khalil MI, et al. Epidemiology of neural tube defects. Saudi Med J. 2014;35( Suppl 1):S29–35. [PMC free article] [PubMed] [Google Scholar]
3. Flores A, Vellozzi C, Valencia D, Sniezek J. Global burden of neural tube defects, risk factors, and prevention. Indian J Community Health. 2014;26(Suppl 1):3–5. [PMC free article] [PubMed] [Google Scholar]
Indian J Community Health. 2014;26(Suppl 1):3–5. [PMC free article] [PubMed] [Google Scholar]
4. Wilde JJ, Petersen JR, Niswander L. Genetic, epigenetic, and environmental contributions to neural tube closure. Annu Rev Genet. 2014;48:583–611. doi: 10.1146/annurev-genet-120213-092208. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. Mandıracıoğlu A, Ulman I, Lüleci E, Ulman C. The incidence and risk factors of neural tube defects in Izmir, Turkey: a nested case-control study. Turk J Pediatr. 2004;46(3):214–20. [PubMed] [Google Scholar]
6. Loo KW, Gan SH. Folic acid supplementation is not the sole factor in determining neural tube defects: The possible role of autoantibodies. African Journal of Biotechnology. 2012;11(55):11767–71. doi: 10.5897/AJB12.065. [CrossRef] [Google Scholar]
7. Copp AJ, Stanier P, Greene ND. Neural tube defects: recent advances, unsolved questions, and controversies. The Lancet Neurology. 2013;12(8):799–810. doi: 10.1016/S1474-4422(13)70110-8. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
[PMC free article] [PubMed] [CrossRef] [Google Scholar]
8. Rai SK, Singh R, Pandey S, Singh K, Shinde N, Rai S, et al. High incidence of neural tube defects in Northern part of India. Asian J Neurosurg. 2016;11(4):352–5. [PMC free article] [PubMed] [Google Scholar]
9. De Marco P, Merello E, Cama A, Kibar Z, Capra V. Human neural tube defects: Genetic causes and prevention. Biofactors. 2011;37(4):261–8. doi: 10.1002/biof.170. [PubMed] [CrossRef] [Google Scholar]
10. Carmichael SL, Yang W, Feldkamp ML, Munger RG, Siega-Riz AM, Botto LD, et al. Reduced risks of neural tube defects and orofacial clefts with higher diet quality. Arch Pediatr Adolesc Med. 2012;166(2):121–6. doi: 10.1001/archpediatrics.2011.185. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Yang J, Carmichael SL, Canfield M, Song J, Shaw GM. Socioeconomic status in relation to selected birth defects in a large multicentered US case-control study. Am J Epidemiol. 2008;167(2):145–54. doi: 10. 1093/aje/kwm283. [PubMed] [CrossRef] [Google Scholar]
1093/aje/kwm283. [PubMed] [CrossRef] [Google Scholar]
12. Salih MA, Murshid WR, Seidahmed MZ. Classification, clinical features, and genetics of neural tube defects. Saudi Med J. 2014;35( Suppl 1):S5–S14. [PMC free article] [PubMed] [Google Scholar]
13. Yerby MS. Clinical care of pregnant women with epilepsy: neural tube defects and folic acid supplementation. Epilepsia. 2003;44( Suppl 3):33–40. doi: 10.1046/j.1528-1157.2003.t01-1-44703.x-i1. [PubMed] [CrossRef] [Google Scholar]
14. Nauman N, Jalali SS, AslamShami S, Akhtar N. Consanguinity and Neural Tube Defects. Journal of Rawalpindi Medical College. 2016;20(2):120–3. [Google Scholar]
15. Golalipour MJ, Qorbani M, Mirfazeli A, Mobasheri E. Risk factors of neural tube defects in northern iran. Iran Red Crescent Med J. 2014;16(6):e7940. doi: 10.5812/ircmj.7940. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Suarez L, Felkner M, Brender JD, Canfield M, Hendricks K. Maternal exposures to cigarette smoke, alcohol, and street drugs and neural tube defect occurrence in offspring. Matern Child Health J. 2008;12(3):394–401. doi: 10.1007/s10995-007-0251-y. [PubMed] [CrossRef] [Google Scholar]
Matern Child Health J. 2008;12(3):394–401. doi: 10.1007/s10995-007-0251-y. [PubMed] [CrossRef] [Google Scholar]
17. Salmasi G, Grady R, Jones J, McDonald SD. Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89(4):423–41. doi: 10.3109/00016340903505748. [PubMed] [CrossRef] [Google Scholar]
18. Talebian A, Soltani B, Sehat M, Zahedi A, Noorian A, Talebian M. Incidence and Risk Factors of Neural Tube Defects in Kashan, Central Iran. Iran J Child Neurol. 2015;9(3):50–6. [PMC free article] [PubMed] [Google Scholar]
19. Al Rakaf MS, Kurdi AM, Ammari AN, Al Hashem AM, Shoukri MM, Garne E, et al. Patterns of folic acid use in pregnant Saudi women and prevalence of neural tube defects - Results from a nested case-control study. Prev Med Rep. 2015;2:572–6. doi: 10.1016/j.pmedr.2015.06.016. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
20. Safi J, Joyeux L, Chalouhi G. Periconceptional folate deficiency and implications in neural tube defects. J Pregnancy. 2012;2012:295083. doi: 10.1155/2012/295083. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
J Pregnancy. 2012;2012:295083. doi: 10.1155/2012/295083. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
21. Golalipour M, Vakili M, Arya B. Neural tube defects in newborns in the south-east of the Caspian sea border (Gorgan, Iran 1998–2000) Med J Islam Repub Iran. 2003;16(4):199–203. [Google Scholar]
22. Mobasheri E, Keshtkar A, Golalipour MJ. Maternal folate and vitamin B12 status and neural tube defects in Northern Iran: a case control study. Iran J Pediatr. 2010;20(2):167–73. [PMC free article] [PubMed] [Google Scholar]
23. Nili F, Jahangiri M. Risk factors for neural tube defects: a study at university-affiliated hospitals in Tehran. Arch Iran Med. 2006;9(1):20–5. [PubMed] [Google Scholar]
24. Shahnazi M, Azeri S. Contributing Factors in Major Malformations in Neonatals Born in Alzahra Medical-Educational Hospital, Tabriz. Journal of Nursing and Midwifery, Tabriz. 2010;18:49–56. [Google Scholar]
25. Tong VT, Dietz PM, Rolle IV, Kennedy SM, Thomas W, England LJ. Clinical interventions to reduce secondhand smoke exposure among pregnant women: a systematic review. Tob Control. 2015;24(3):217–23. doi: 10.1136/tobaccocontrol-2013-051200. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Clinical interventions to reduce secondhand smoke exposure among pregnant women: a systematic review. Tob Control. 2015;24(3):217–23. doi: 10.1136/tobaccocontrol-2013-051200. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
26. Wang M, Wang ZP, Gao LJ, Yang H, Zhao ZT. Maternal consumption of non-staple food in the first trimester and risk of neural tube defects in offspring. Nutrients. 2015;7(5):3067–77. doi: 10.3390/nu7053067. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
27. Molloy AM, Kirke PN, Troendle JF, Burke H, Sutton M, Brody LC, et al. Maternal vitamin B12 status and risk of neural tube defects in a population with high neural tube defect prevalence and no folic acid fortification. Pediatrics. 2009;123(3):917–23. doi: 10.1542/peds.2008-1173. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
28. Thompson MD, Cole DE, Ray JG. Vitamin B-12 and neural tube defects: the Canadian experience. Am J Clin Nutr. 2009;89(2):697S–701S. doi: 10.3945/ajcn. 2008.26947B. [PubMed] [CrossRef] [Google Scholar]
2008.26947B. [PubMed] [CrossRef] [Google Scholar]
29. Zhang T, Xin R, Gu X, Wang F, Pei L, Lin L, et al. Maternal serum vitamin B12, folate and homocysteine and the risk of neural tube defects in the offspring in a high-risk area of China. Public Health Nutr. 2009;12(05):680–6. doi: 10.1017/S1368980008002735. [PubMed] [CrossRef] [Google Scholar]
30. Chandler AL, Hobbs CA, Mosley BS, Berry RJ, Canfield MA, Qi YP, et al. Neural tube defects and maternal intake of micronutrients related to one - carbon metabolism or antioxidant activity. Birth Defects Res A Clin Mol Teratol. 2012;94(11):864–74. doi: 10.1002/bdra.23068. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
31. Afshar M, Kiyanfar S. The incidence of NTD in newborns and related risk factors in Birjand, 1996–2000. Journal of Gorgan University of Medical Sciences. J Gorgan Uni Med Sci. 2004;6(2):45–51. [Google Scholar]
32. Gu X, Lin L, Zheng X, Zhang T, Song X, Wang J, et al. High prevalence of NTDs in Shanxi Province: a combined epidemiological approach. Birth Defects Res A Clin Mol Teratol. 2007;79(10):702–7. doi: 10.1002/bdra.20397. [PubMed] [CrossRef] [Google Scholar]
Birth Defects Res A Clin Mol Teratol. 2007;79(10):702–7. doi: 10.1002/bdra.20397. [PubMed] [CrossRef] [Google Scholar]
33. Deak KL, Siegel DG, George TM, Gregory S, Ashley - Koch A, Speer MC. Further evidence for a maternal genetic effect and a sex - influenced effect contributing to risk for human neural tube defects. Birth Defects Res A Clin Mol Teratol. 2008;82(10):662–9. doi: 10.1002/bdra.20511. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
34. Grewal J, Carmichael SL, Ma C, Lammer EJ, Shaw GM. Maternal periconceptional smoking and alcohol consumption and risk for select congenital anomalies. Birth Defects Res A Clin Mol Teratol. 2008;82(7):519–26. doi: 10.1002/bdra.20461. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
35. Bannigan J, Burke P. Ethanol teratogenicity in mice: a light microscopic study. Teratology. 1982;26(3):247–54. doi: 10.1002/tera.1420260305. [PubMed] [CrossRef] [Google Scholar]
36. Li ZW, Liu JM, Ren AG, Zhang L, Guo ZY, Li Z. [Maternal passive smoking and the risk of neural tube defects: a case-control study in Shanxi province, China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2008;29(5):417–20. [PubMed] [Google Scholar]
[Maternal passive smoking and the risk of neural tube defects: a case-control study in Shanxi province, China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2008;29(5):417–20. [PubMed] [Google Scholar]
37. Suarez L, Ramadhani T, Felkner M, Canfield MA, Brender JD, Romitti PA, et al. Maternal smoking, passive tobacco smoke, and neural tube defects. Birth Defects Res A Clin Mol Teratol. 2011;91(1):29–33. doi: 10.1002/bdra.20743. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
38. Wang M, Wang ZP, Zhang M, Zhao ZT. Maternal passive smoking during pregnancy and neural tube defects in offspring: a meta-analysis. Arch Gynecol Obstet. 2014;289(3):513–21. doi: 10.1007/s00404-013-2997-3. [PubMed] [CrossRef] [Google Scholar]
39. Benedum CM, Yazdy MM, Mitchell AA, Werler MM. Risk of spina bifida and maternal cigarette, alcohol, and coffee use during the first month of pregnancy. Int J Environ Res Public Health. 2013;10(8):3263–81. doi: 10.3390/ijerph20083263. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
40. Viljoen E. Harmful effects of smoking in pregnancy. S Afr Med J. 2008;95(5):329–30. [PubMed] [Google Scholar]
Viljoen E. Harmful effects of smoking in pregnancy. S Afr Med J. 2008;95(5):329–30. [PubMed] [Google Scholar]
41. Dolk H, Committee EPM. What is the “primary” prevention of congenital anomalies? The Lancet. 2009;374(9687):378. doi: 10.1016/S0140-6736(09)61411-2. [PubMed] [CrossRef] [Google Scholar]
| Basic documents | |||||
| 1 | RD 34.21.122-87 | "Instructions for the device of lightning protection of buildings and structures" | download | ||
| 2 | since 153-34.21.122-2003 | "Instruction for lightning protection of buildings, structures and industrial communications" | Download | ||
| 3 | Explanation of Rostekhnadzor’s Office for Supervision in the Electric Power Industry on the procedure for using the “Instructions for Lightning Protection of Buildings, Structures and Industrial Communications” | Download | |||
| 4 | 9004 | 900 9001 Electrical Installation Rules.Download | |||
| State standards of the Russian Federation | |||||
| 1 | GOST R IEC 62561.1-2014 | "Components of lightning protection systems. Part 1. Requirements for the connecting components" | download | ||
| 2 | GOST REC 62561.2-2014 | "Components of lightning protection systems. Part 2. Requirements for conductors and grounding electrodes" | 11111111111111111111111111111111111111111111111111111111111111111111111IONA Download | ||
| 3 | GOST R IEC 62561.3-2014 | "Lightning protection system components. Part 3. Requirements for isolating spark gaps" | Download | ||
| 4 | GOST R IEC 62561.4-2014 | "Components of lightning protection systems. Part 4. Requirements for guidelines of conductors" | download | ||
| 5 | GOST REC 62561. 5-2014 5-2014 | "Components lightning protection - Part 5: Requirements for manholes and seals for grounding electrodes0008 | download | ||
| 7 | GOST REC 62305-2-2010 | "Risk Protection. Part 2. Risk assessment" | Download | ||
| 8 | GOST R 50571.5.54-54- 2013 (IEC 60364-5-54:2011) | "Low-voltage electrical installations. Part 5-54. Selection and installation of electrical equipment. Earthing devices, protective conductors and protective potential equalization conductors" | Download | ||
| 9 | GOST R 50571.22-2000 (IEC 60364-7-707-84) | "Requirements for special electrical installations. Section 707. grounding of information processing equipment" | download | ||
| 10 | GOST 12.1.030-81 | "Electrical safety. Protective grounding, zeroing." | Download | ||
| 11 | GOST 12.1.038-82 | "Electrical safety. Maximum allowable values of contact voltage and current." Maximum allowable values of contact voltage and current." | Download | ||
| 12 | GOST R IEC 60050-195-2005 | "Earthing and protection against electric shock. Terms and definitions." | Download | ||
| 13 | GOST 464-79 | "Interstate standard. Grounding for fixed installations of wired communication, radio relay stations, radio broadcasting nodes of wire broadcasting and antennas of collective television reception systems. Resistance standards" | 0011 Download|||
| 14 | GOST R IEC 61643-12-2011 | "National standard of the Russian Federation. Low-voltage surge protection devices. Part 12. Surge protection devices in low-voltage power distribution systems. Principles of selection and application " | Download | ||
| 15 | GOST R 54986-2012 (IEC 61643-21:2009) | "National standard of the Russian Federation. Low-voltage surge protection devices. Part 21. Protection devices against surge surges in telecommunication systems. and signaling (information systems). Performance requirements and test methods " Part 21. Protection devices against surge surges in telecommunication systems. and signaling (information systems). Performance requirements and test methods " | download | ||
| 16 | GOST R 55630-2013 | "Impulsive overstrain and protection against overstrain in low-voltage systems of alternating current. General provisions" | download | ||
| GOST 28298-89 | " Grounding of mine electrical equipment. Technical requirements and methods of control" | Download | |||
| 0011 Technical circular No. 11/2006 | "Technical circular about grounding electrodes and grounding conductors" | download | |||
| 2 | Technical circular No. 26/2010 | "On protective and equalization of potentials in explosive zones" | Download | ||
| 3 | Technical circular No. 30/2012 | "On the implementation of lightning protection and grounding of overhead lines and overhead lines up to 1 kV" | Download | ||
| Documents | |||||
| 1 | RD 78. 145-93 145-93 | Manual to the leading document "Systems and complexes of security, fireproof signaling. Rules for the production and acceptance of work. Chapter 14" | Download | ||
| 2 | RD 153-34.3-35.125-99 | "Guidelines for the protection of electrical networks 6 - 1150 kV from lightning and internal surges." | Download | ||
| 3 | RD 45.091.195-90 | "Instructions for the design of electric communication complexes. General requirements and norms for grounding equipment, cables and metal structures" | download | 4 9000 | RD 45.155-2000 | "Article" Article and potential equalization of FOCL equipment at wired communication facilities" | Download |
| Organizational standards | |||||
| 1 | VSP 22-02-07 MO RF | "Standards for the design, installation and operation of lightning protection of military infrastructure" | Download | Download | |
| 3 | STO 70238424. 29.240.99.005-2011 29.240.99.005-2011 | "Surge protection devices for power plants and networks. Delivery conditions. Norms and requirements" | Download | ||
| 4 | STO 70238424.29.240.99.006-2011 | "Defense and maintenance and maintenance organization devices. Organization of operation and maintenance. Norms and requirements" | Download | STO 56947007-29.130.15.114-2012 | "Guidelines for the design of grounding devices for 6-750 kV substations" | Download |
| 6 | STO 56947007-29.240.02.001-2008 | "Methodological instructions for the protection of distribution electric networks with a voltage of 0.4-10 kV from thunderous overvoltages" | Download | 7 | N CE-191 RID "Railways" | "Instructions for grounding power supply devices on electrified railways" | Download |
| 8 | N 2871r JSC "Russian Railways" | "The concept of integrated protection of technical equipment and objects of railway infrastructure from the effects of atmospheric and switching overvoltage effects " | download | ||
| other documents | |||||
| 1 | Order of Rostekhnadzor dated 06. 11.2012 N 625 11.2012 N 625 | "On approval of federal norms and rules in the field of industrial safety" Instructions for the device, inspection and measurement of resistance of mine grounds " | Download | ||
| 2 | SO 153-34.20.501-2003 | "Rules for the technical operation of power plants and networks of the Russian Federation" | Download | ||
| 3 | Order of the Ministry of Energy of the Russian Federation of 13.01.2003 N 6 | "On approval of the Rules for the technical operation of consumer electrical installations" | download | 4 | SNiP 3.05.06-85 | "Electrotechnical devices" | Download |
| 5 | RM 14-11-95 | "Grounding electrical control and automation networks. A practical guide" | Download | ||
| 6 | PM4-249-91 | Process Automation Grounding Guide | Download | ||
Risk Management in an Organization's Quality Management System use this04 identifier 90 to this item:
http://earchive. tpu.ru/handle/11683/49113
tpu.ru/handle/11683/49113 | Title: | Risk management in the organization's quality management system |
| Authors: | Nepoyaranov, Artyom Sergeevich |
| Metadata.dc.contributor.advisor: | Redko, Lyudmila Anatolyevna |
| Keywords: | process; risk - management; risk analysis; Quality Management System; risk level; process; risk management; risk analysis; Quality Management System; level of risk |
| Issue Date: | 2018 |
| Citation: | Nepoiranov AS Risk management in the organization's quality management system: Bachelor's thesis / AS Nepoiranov; National Research Tomsk Polytechnic University (TPU), Engineering School of Non-Destructive Testing and Safety (ISNKB), Department of Control and Diagnostics (OKD); scientific hands L. A. Redko. - Tomsk, 2018. |
| Abstract: | The object of the study is the enterprise quality management system. The subject of the study is the process of design and survey work. The initial information for the performance of the work is interstate standards on the quality management system, risk management, scientific publications and methodological literature, statistical data and internal documentation of the enterprise, reference data from the Internet. The purpose of the work: to conduct a risk analysis of the process of design and survey work. Tasks performed to achieve the goal: 1. Analytical review of literary sources and regulatory and technical documentation in the field of risk management. 2. Approbation of the methodology for analyzing the types and consequences of failures on the process of design and survey work. The subject of the study is the process of design and survey work. The initial information for the performance of the work is interstate standards on the quality management system, risk management, scientific publications and methodological literature, statistical data and internal documentation of the enterprise, reference data from the Internet. The purpose of the work: to conduct a risk analysis of the process of design and survey work. Tasks performed to achieve the goal: 1. Analytical review of literary sources and regulatory and technical documentation in the field of risk management. 2. Approbation of the methodology for analyzing the types and consequences of failures on the process of design and survey work. The object of research is the company's quality management system. The subject of the study is the process of design and survey work. The initial information for the work is interstate standards for the quality management system, risk management, scientific publications and methodological literature, statistics and internal documentation of the enterprise, reference data of the Internet.  |
 Seventh edition.
Seventh edition.