Recommended dosage of folic acid during pregnancy
Folic Acid | CDC
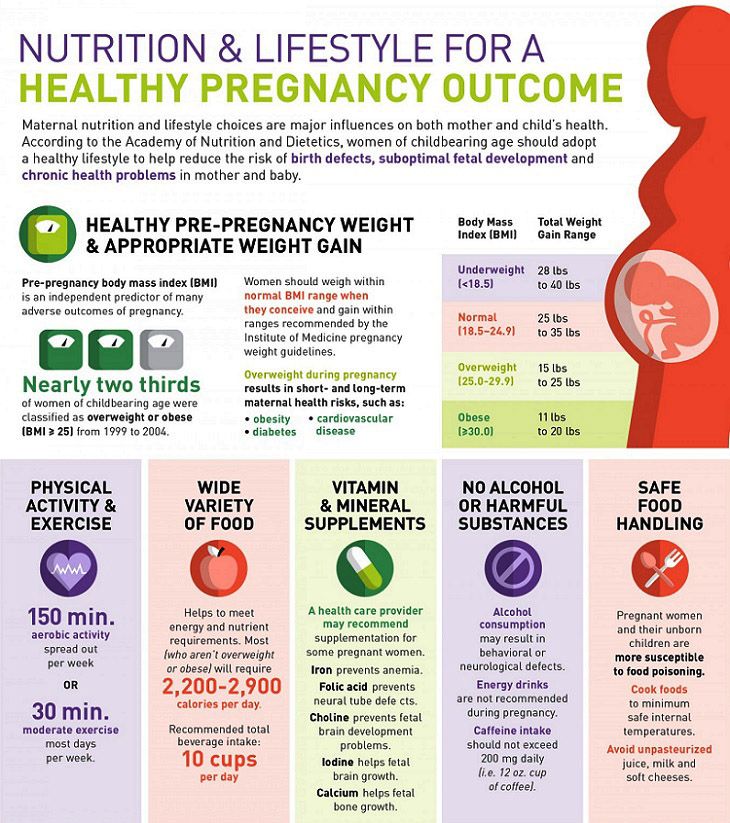
CDC urges all women of reproductive age to take 400 micrograms (mcg) of folic acid each day, in addition to consuming food with folate from a varied diet, to help prevent some major birth defects of the baby’s brain (anencephaly) and spine (spina bifida).
About folic acid
Folic acid is a B vitamin. Our bodies use it to make new cells. Think about the skin, hair, and nails. These–and other parts of the body – make new cells each day. Folic acid is the synthetic (that is, not generally occurring naturally) form of folate used in supplements and in fortified foods such as rice, pasta, bread, and some breakfast cereals
Why folic acid is important before and during pregnancy
When the baby is developing early during pregnancy, folic acid helps form the neural tube. Folic acid is very important because it can help prevent some major birth defects of the baby’s brain (anencephaly) and spine (spina bifida). The neural tube forms the early brain and spine.
Women of reproductive age need 400 mcg of folic acid every day
- All women of reproductive age should get 400 mcg of folic acid every day to get enough folic acid to help prevent some birth defects because
- About half of U.S. pregnancies are unplanned, and
- Major birth defects of the baby’s brain or spine occur very early in pregnancy (3-4 weeks after conception), before most women know they are pregnant.
- When taking folic acid, a higher dose than 400 mcg of folic acid each day is not necessarily better to prevent neural tube defects, unless a doctor recommends taking more due to other health conditions.
- When planning to become pregnant, women who have already had a pregnancy affected by a neural tube defect should consult with their healthcare provider. CDC recommends that these women consume 4,000 mcg of folic acid each day one month before becoming pregnant and through the first 3 months of pregnancy.

- When planning to become pregnant, women who have already had a pregnancy affected by a neural tube defect should consult with their healthcare provider. CDC recommends that these women consume 4,000 mcg of folic acid each day one month before becoming pregnant and through the first 3 months of pregnancy.
Learn more about CDC’s folic acid recommendations here.
Learn more about the recommended intake level of folic acid here.
When to start taking folic acid
Every woman of reproductive age needs to get folic acid every day, whether she is planning to get pregnant or not, to help make new cells.
Are folate and folic acid the same thing?
The terms “folate” and “folic acid” are often used interchangeably, even though they are different. Folate is a general term to describe many different types of vitamin B9.
Types of folate can include
- Dihydrofolate (DHF)
- Tetrahydrofolate (THF)
- 5, 10-methylenetetrahydrofolate (5, 10-Methylene-THF)
- 5-methyltetrahydrofolate (5-Methyl-THF or 5-MTHF)
Food fortification is a way to add vitamins or minerals, or both, to foods. Some rice, pasta, bread, and breakfast cereals are fortified with folic acid. These foods are labeled “enriched.” Folic acid is a specific type of folate that does not generally occur naturally.
Folic acid is the ideal form of folate to use for food fortification. It is more stable than types of natural food folate, which can easily be broken down by heat and light. Folic acid is better suited for food fortification because many fortified products, such as bread and pasta, are cooked.6
CDC recommends that women of reproductive age who could become pregnant consume at least 400 micrograms (mcg) of folic acid every day. However, it’s difficult to get 400 mcg of folic acid through diet alone. You can get 400 mcg of folic acid each day by taking a vitamin with folic acid in it, eating fortified foods, or a combination of the two, in addition to consuming a balanced diet rich in natural food folate.
How to get enough folic acid to prevent neural tube defects
In addition to eating foods with folate from a varied diet, women can get folic acid from
- Taking a vitamin that has folic acid in it:
- Most vitamins sold in the United States have the recommended daily amount of folic acid (400 mcg) that women need for the prevention of neural tube defects.
 Vitamins can be found at most local pharmacy, grocery, or discount stores.
Vitamins can be found at most local pharmacy, grocery, or discount stores.
- Most vitamins sold in the United States have the recommended daily amount of folic acid (400 mcg) that women need for the prevention of neural tube defects.
- Eating fortified foods:
- You can find folic acid in some breads, breakfast cereals, and corn masa flour.
- Getting a combination of the two: taking a vitamin that has folic acid in it and eating fortified foods.
If taking folic acid for reasons other than neural tube defect prevention, talk to your healthcare provider.
Learn more about where to find folic acid in the United States here.
More Information
For more information, visit the Frequently Asked Questions page.
You can also contact CDC-INFO in English or Spanish:
- 1-800-CDC-INFO (800-232-4636)
- TTY: 1-888-232-6348
- In English
- en español
Folic Acid and Pregnancy: How Much You’ll Need
Folic acid is a B vitamin found in many supplements and fortified foods. It’s the synthetic form of folate. Folic acid is used by your body to make new cells and produce DNA. It’s required for normal growth and development throughout your life.
It’s required for normal growth and development throughout your life.
Taking folic acid is particularly vital before and during pregnancy. It’s important for the proper organ development of a developing baby.
Research shows that taking folic acid before you get pregnant may help prevent birth defects including serious neural tube defects such as spina bifida, encephalocele (rarely), and anencephaly.
Approximately 3,000 babies are born with neural tube defects in the United States each year. Normally, the neural tube develops into the spinal cord and brain by 28 days after conception.
If the neural tube doesn’t close properly, neural tube defects occur. Anencephaly is a condition in which the brain doesn’t develop properly. Babies born with anencephaly cannot survive.
Babies born with spina bifida or encephalocele may face multiple surgeries, paralysis, and long-term disability.
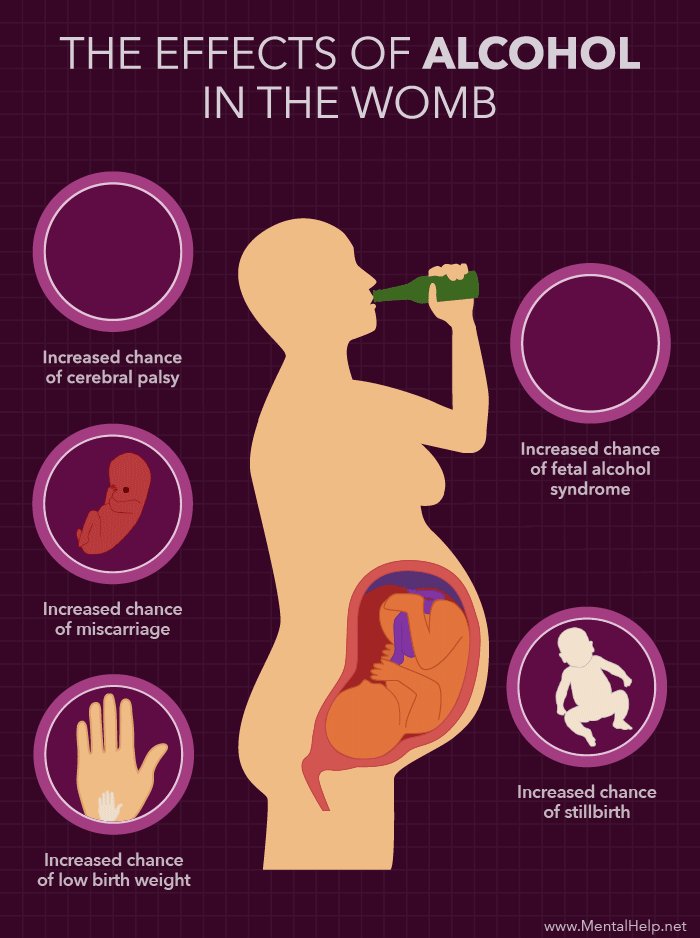
According to a 2015 review of studies, maternal folic acid supplementation significantly decreases the risk of congenital heart defects. These defects occur in 8 out of every 1,000 births in the United States.
These defects occur in 8 out of every 1,000 births in the United States.
According to the American Heart Association, congenital heart defects happen when the heart or blood vessels don’t grow normally before birth. They may impact the interior walls of the heart, the heart valves, or the arteries and veins of the heart.
Research also shows folic acid supplementation in early pregnancy may help prevent cleft lip and cleft palate.
These birth defects occur if parts of the mouth and lip do not merge together properly during the first 6 to 10 weeks of pregnancy. One or more surgeries are usually needed to correct the condition.
All pregnant women should take get at least 600 micrograms (mcg) of folic acid daily, according to The American College of Obstetricians and Gynecologists. Most prenatal vitamins contain this amount of folic acid.
Taking folic acid after you discover you’re pregnant may not be soon enough. Many women don’t realize they’re pregnant until 6 weeks or more after conception. Neural tube defects occur during the first month of pregnancy, often before you realize you’re pregnant.
Neural tube defects occur during the first month of pregnancy, often before you realize you’re pregnant.
To make sure you have enough folic acid in your body to prevent neural tube defects, the CDC recommends women who plan to become pregnant or who are of childbearing age take 400 mcg of folic acid daily.
If you’ve already given birth to a child with a neural tube defect, you may need higher doses of folic acid in the months leading up to your next pregnancy and during the first few months of pregnancy. Your doctor can advise you on the right dose.
You may also need higher doses of folic acid if you:
- have kidney disease and are on dialysis
- have sickle cell disease
- have liver disease
- drink more than one alcoholic beverage daily
- take medications to treat epilepsy, type 2 diabetes, lupus, psoriasis, rheumatoid arthritis, asthma, or inflammatory bowel disease
Natural folate is found in many foods including leafy greens, beets, and broccoli. Some foods in the United States are fortified with folic acid. These include:
Some foods in the United States are fortified with folic acid. These include:
- cereals
- rice
- orange juice
- pasta
Many servings of fortified breakfast cereals contain 100 percent of the folic acid you need. Even so, it may be hard to know exactly how much you’re getting unless you track the amounts of folate and folic acid in everything you eat.
There’s no guarantee that you will get enough folic acid from food alone, so a supplement is important.
If you have morning sickness in early pregnancy, it may be difficult to eat enough fortified foods to get the folic acid you need.
To make sure you get enough folic acid, doctors will usually recommend taking a folic acid supplement or a prenatal vitamin that contains folic acid before and during pregnancy.
You can’t get too much natural folate from foods. However, you should not consume more than 1,000 mcg (1 mg) of folic acid (from vitamins, fortified foods, or a combination of both) daily.
There’s no way to prevent all birth defects with 100 percent certainty. Taking adequate amounts of folic acid before and during pregnancy may help decrease your risk of:
- neural tube defects
- congenital heart defects
- cleft palate
- cleft lip
If pregnancy is in your future, consider adding a prenatal vitamin to your daily routine. Prenatal vitamins are available in capsule, tablet, and chewable forms. To avoid stomach upset, take prenatal vitamins with food.
Always talk to your doctor about taking the correct dose of prenatal vitamin because taking too many supplements can be toxic for your baby-to-be.
You should also add foods fortified with folic acid to your diet. Don’t wait until you find out you’re pregnant to get serious about folic acid. By then, it may be too late. Talk to your doctor to determine the right amount of folic acid you’ll need.
Folic acid for pregnancy planning
Our services
Surrogate mothers are urgently needed.
Requirements: physical and mental health, presence of own children is obligatory, age up to 35 years. For all questions, please contact:
8(495)2235324, 8(926)0423057
home » About clinic » Folic acid when planning pregnancy
Any woman who plans to soon become pregnant and become a mother should consciously and carefully prepare for this new status. And if everyone knows about a healthy lifestyle, parting with bad habits and walking in the fresh air, then expectant mothers often ignore the intake of certain vitamins and medicines before pregnancy. One such remedy is folic acid.
What is folic acid?
Folic acid is vitamin B9. Often you can hear the generalized name - folates, they are derivatives of this vitamin. We must understand that we get them from food, and folic acid tablets are a synthetic agent that is already converted into folates inside the body. nine0003
nine0003
All derivatives of vitamin B9 play an important role in hematopoiesis, that is, the formation of new blood cells. Therefore, the lack of these substances leads to anemia - a condition in which there are not enough red blood cells, or they are irregular in shape and do not perform their functions. Folates have another very important feature: they stimulate the formation of nucleic acids (DNA and RNA), which are the basis of all body cells. Therefore, it is folic acid that is necessary for all rapidly dividing human tissues, including embryonic tissues. nine0003
The role of folic acid:
- participates in the formation of DNA in all cells, that is, the source of hereditary information;
- stimulates hematopoiesis;
- indirectly blocks the formation of cancer cells;
- restores muscle tissue;
- during pregnancy: plays a role in the laying and development of the nervous tissue of the embryo, participates in the formation of placental vessels.

Why do you need folate during pregnancy? nine0017
During pregnancy, especially in the early stages, the consumption of folate increases dramatically. All cells of the embryo are intensively dividing in order to eventually form full-fledged tissues. The nervous tissue of the future man is transformed especially quickly and difficultly. And it is she who requires a large amount of folic acid.
Folic acid deficiency during pregnancy can occur due to the following reasons:
- Insufficient intake of folate from food. nine0027 Folate malabsorption (in chronic inflammatory diseases of the stomach and intestines).
- Genetic disorders of the folate cycle. In rare cases, a woman's body lacks the necessary enzymes (MTHFR). As a result, folic acid is not converted to folates, and they do not perform the necessary functions. Intermediate metabolic products accumulate in the body, which can lead to cardiovascular diseases, tumor processes, infertility and miscarriage.
 In the presence of such a mutation, it is recommended to take folic acid derivatives, for example, Metafolin. It is absorbed faster and in greater volume. nine0028
In the presence of such a mutation, it is recommended to take folic acid derivatives, for example, Metafolin. It is absorbed faster and in greater volume. nine0028 - Taking certain anti-epilepsy drugs and hormonal drugs dramatically reduces blood folate levels:
- oral contraceptives;
- barbiturates, diphenylhydantoin;
- sulfa drugs (for example, biseptol), which inhibit the synthesis of vitamin B9 by the intestinal microflora;
- drinking alcohol also lowers their levels.
At what stage of pregnancy should I take folic acid supplements? nine0017
Folic acid intake to prevent fetal malformations should be started already at the stage of preparation for pregnancy, at least three months before the intended conception. That is why pregnancy should be planned. If conception occurred unexpectedly, then you need to start taking the drug as soon as it became known.
Reasons for taking folates at the stage of pregnancy planning:
- If a woman has an unbalanced diet, her folic acid level can be low, so it takes time to replenish her reserves.
 It usually takes three to four months. nine0028
It usually takes three to four months. nine0028 - The neural tube of the fetus is laid at such an early stage that a woman may not even be aware of the pregnancy, especially with a long menstrual cycle.
- Folate deficiency can make pregnancy difficult.
Doctors of the Intime Family Planning Clinic give the following recommendations for taking folic acid: in most cases, three months before conception and throughout pregnancy, you need to take 400 micrograms of folic acid per day. In some cases, the dosage is advised to increase: up to 1 mg per day for epilepsy and diabetes; up to 4 mg per day if there have been children with neural tube defects in the past Increased doses of folates can only be prescribed by a doctor after a thorough examination. The dose of folic acid during pregnancy remains the same. nine0003
We wish you an easy pregnancy and healthy babies!
×
Send a request for a free consultation
We provide the first free consultation for new patients. Just leave your contact details and we will contact you within a business day.
Just leave your contact details and we will contact you within a business day.
Your name
Your Phone
Choose a service Family PlanningIn vitro fertilizationMen's healthWomen's healthTests
By clicking on the button, you consent to the processing of personal data and agree to the privacy policy.
Pregnancy and nutrients: when, what and how much?
Summary. It's no secret that during pregnancy a woman's body should receive a sufficient amount of vitamins, micro- and macroelements necessary for the normal course of pregnancy and fetal development. Is it possible to fill the deficiency of vitamins with the help of food? What micronutrients should a pregnant woman take? What is the optimal dose of folic acid during pregnancy? These questions were answered during the training workshop for gynecologists "Actual GuideLines of Gynecology, Reproductology, Obstetrics", which took place on 29March 2019 in Kharkov, answered Tamara Romanenko , Doctor of Medical Sciences, Professor of the Department of Obstetrics and Gynecology No.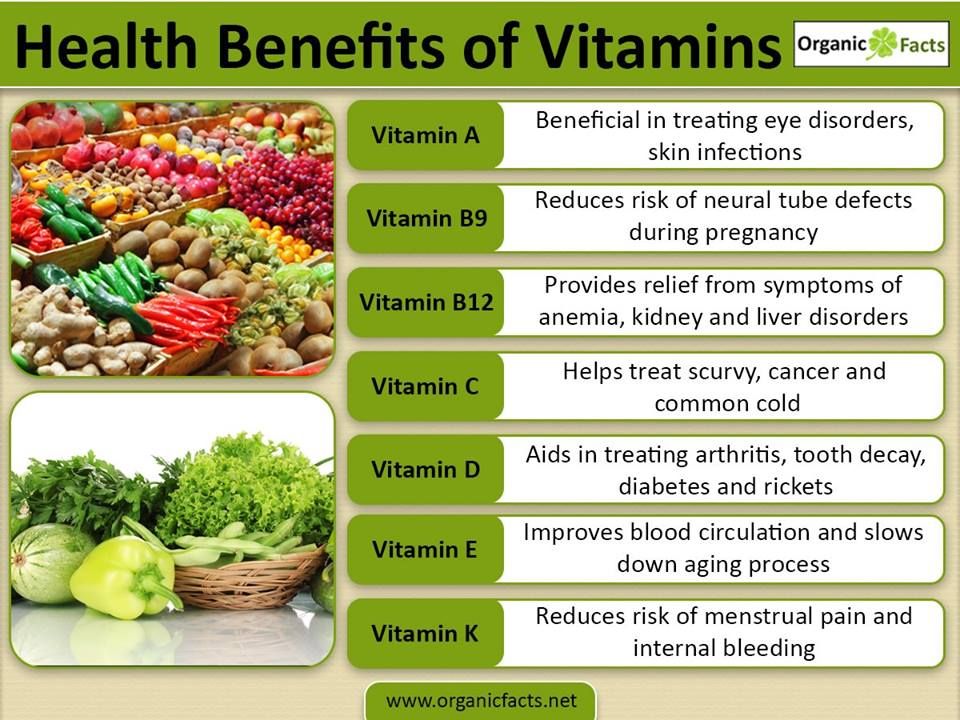 1 of the National Medical Academy of Postgraduate Education named after P.L. Shupyk. The event was organized by the MedExpert Group of Companies, National Medical University named after A.A. Bogomolets and the National Medical Academy of Postgraduate Education named after P.L. Shupyk.
1 of the National Medical Academy of Postgraduate Education named after P.L. Shupyk. The event was organized by the MedExpert Group of Companies, National Medical University named after A.A. Bogomolets and the National Medical Academy of Postgraduate Education named after P.L. Shupyk.
Micronutrients and women's reproductive health
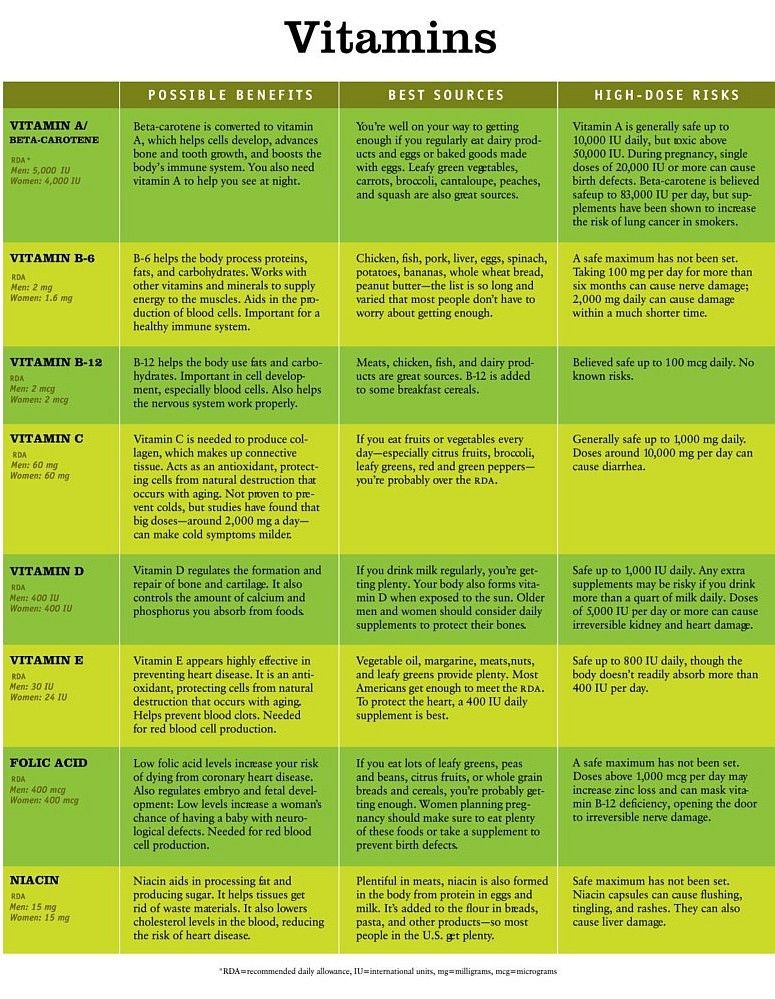
Micronutrients (vitamins, macro- and microelements) are sources of energy, participate in the assimilation of food, regulate functions that carry out the processes of growth, adaptation and development of the whole organism. It has been proven that the amount of vitamins and minerals in women of reproductive age is significantly reduced. Most often, they are deficient in folate, iron, vitamins D, A and B 6 zinc.
In modern conditions, when a person is not engaged in physical labor, his need for energy and nutrients is lower, but this does not apply to vitamins and minerals. The high intensity of metabolic processes in modern people is associated with the pressure of an aggressive environment, intellectual stress, stress, and various situations in family life. At the same time, the need for vitamins and minerals increases to the greatest extent during periods when a woman is preparing to become a mother, pregnancy and breastfeeding. To ensure the required amount of vitamins, a woman should consume a large number of quality foods. At the same time, it should be remembered that the amount of vitamins in food decreases during heat treatment, long-term and improper storage, canning, and intensive processing of food. The degree of digestibility of vitamins with food can vary between 5–80%. nine0003
At the same time, the need for vitamins and minerals increases to the greatest extent during periods when a woman is preparing to become a mother, pregnancy and breastfeeding. To ensure the required amount of vitamins, a woman should consume a large number of quality foods. At the same time, it should be remembered that the amount of vitamins in food decreases during heat treatment, long-term and improper storage, canning, and intensive processing of food. The degree of digestibility of vitamins with food can vary between 5–80%. nine0003
The speaker emphasized that a diet composed exclusively of natural products cannot fully meet a person's need for essential micronutrients. Possible risk factors for vitamin and mineral deficiency can be inadequate nutrition in quantity and quality, somatic diseases, genetically determined anomalies of vitamin metabolism, the influence of environmental factors, the use of certain drugs, overweight or underweight, young or old age, bad habits. nine0003
Vitamin deficiencies and pregnancy
Women eat a significant amount of food that is low in vitamins and minerals, their diet is often unbalanced. Violation of the rational nutrition of the mother before and during pregnancy is one of the causes of congenital malformations and other pathologies. It is known that congenital malformations can occur due to various endogenous and exogenous processes and causes (genetic defects, exposure to toxic substances, drugs, ionizing radiation, somatic and extragenital pathology in the expectant mother, etc.). However, since ancient times, there has been a clear relationship between maternal nutrition and the birth of children with congenital malformations. A poor-quality and quantitatively depleted diet of a future mother poses a threat to the normal development of the child, as well as to the course of the entire process of pregnancy and the health of a woman in the future. Both insufficient and excessive amounts of vitamins can be one of the causes of congenital malformations. nine0003
Violation of the rational nutrition of the mother before and during pregnancy is one of the causes of congenital malformations and other pathologies. It is known that congenital malformations can occur due to various endogenous and exogenous processes and causes (genetic defects, exposure to toxic substances, drugs, ionizing radiation, somatic and extragenital pathology in the expectant mother, etc.). However, since ancient times, there has been a clear relationship between maternal nutrition and the birth of children with congenital malformations. A poor-quality and quantitatively depleted diet of a future mother poses a threat to the normal development of the child, as well as to the course of the entire process of pregnancy and the health of a woman in the future. Both insufficient and excessive amounts of vitamins can be one of the causes of congenital malformations. nine0003
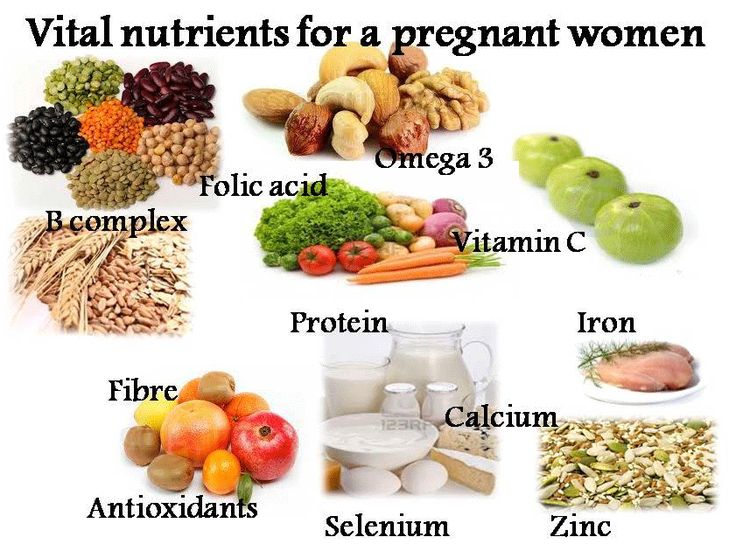
Vitamins and minerals are necessary for the normal development of the child at all stages. So, in the period before conception, it is important for the future mother to receive zinc, folate, iron, vitamins B 6 , B 12 and D, in the first trimester of pregnancy - folate, iron, vitamins B 12 and D, during II-III trimester - iron, calcium, vitamins, in the postpartum period and during breastfeeding - iron, calcium, vitamin D, fats and proteins.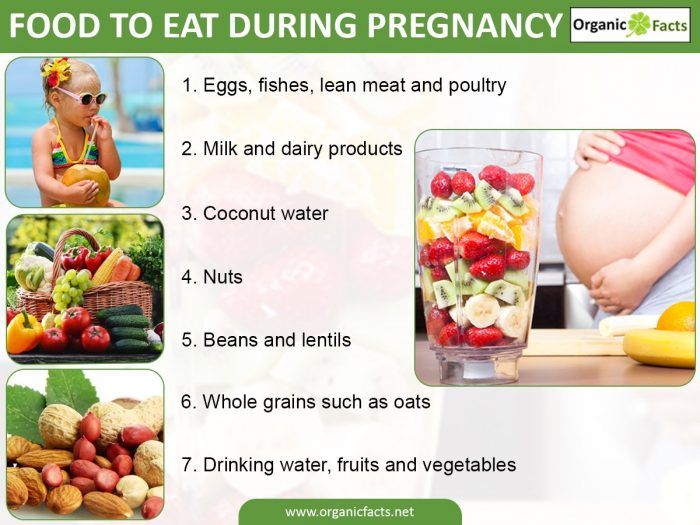
Pregnancy is associated with changes in metabolism, the work of the hormonal system, the blood system, therefore, during this period, the need for vitamins and minerals increases. So, during pregnancy, the body needs 1.5 times more calcium, zinc and iodine, and the need for individual vitamins and trace elements increases to 50-80%. For example, the need for folic acid increases by 50%, vitamin B 12 - by 11%, iron - by 83%.
Folic acid
During pregnancy, the need for folic acid increases by 150%. Folic acid deficiency during pregnancy increases the risk of preeclampsia, development of placental dysfunction with fetal growth retardation syndrome, miscarriage, miscarriage, premature birth. At the same time, not only the insufficiency of the effect of folate matters, but also the toxic effect of homocysteine, which freely penetrates the placenta and can harm the unborn child. nine0003
The role of folates and hyperhomocysteinemia
Recently, special attention has been paid to the study of risk factors for such a severe pregnancy complication as preeclampsia.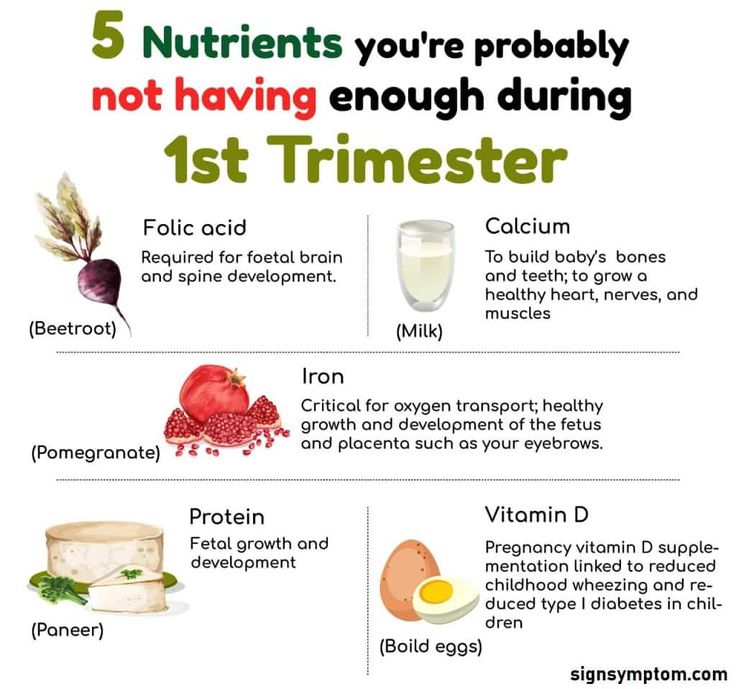 The results of the studies show a 40% reduction in the risk of developing preeclampsia in pregnant women taking folic acid 1 month before the onset of gestation.
The results of the studies show a 40% reduction in the risk of developing preeclampsia in pregnant women taking folic acid 1 month before the onset of gestation.
With a lack of folic acid, hyperhomocysteinemia may occur - a pathological condition of the body, manifested by an increased concentration of homocysteine in the blood (normal concentration in blood plasma is 10 μmol / l). The level of homocysteine may increase in vitamin deficiency states (deficiency of folic acid, vitamin B 6 , B 12 and B 1 ), increased intake of methionine from food, smoking and coffee abuse, sedentary lifestyle, kidney disease, medication, concomitant diseases, genetic inheritance (the most studied is the defect in the enzyme methylenetetrahydrofolate reductase MTH - FR ).
Deficiency of folic acid, vitamins B 12 and B 6 leads to hyperhomocysteinemia, which causes the development of endothelial dysfunction, thrombus formation, immune maladaptation, oxidative stress, which in turn leads to impaired uteroplacental and fetoplacental blood circulation - the risk of miscarriage, premature birth, preeclampsia, nephropathy of pregnant women, placental abruption, intrauterine fetal death increases. nine0003
nine0003
Folic acid is a methyl group donor, which is necessary for the conversion of homocysteine to methionine. In order for homocysteine to be converted into methionine, a woman from the planning period of pregnancy and the first trimester of pregnancy must receive a sufficient amount of folic acid. It has been shown that the number of cases of premature birth in women who took a sufficient amount of folic acid in combination with vitamins during pregnancy is 2 times lower than in pregnant women who did not take multivitamin preparations. nine0003
Folic acid: choosing the optimal dose
What is the optimal dose of folic acid? The data presented by the speaker from a meta-analysis of 25 randomized controlled trials indicate that the more folate, the less homocysteine. 800 mcg of folate has been shown to reduce homocysteine levels by an average of 23%. Increasing the dose of folic acid to non-physiological 2 and 5 mg reduces the level of homocysteine slightly compared with a dose of 800 mcg. Addition of vitamin B 9 to the treatment regimen0109 12 at a dose of 0.4 mg / day, on average, increases the effect by 7%.
Addition of vitamin B 9 to the treatment regimen0109 12 at a dose of 0.4 mg / day, on average, increases the effect by 7%.
906 nmol/l is the concentration of folic acid in erythrocytes at which the risk of congenital malformations, in particular neural tube defects, is the lowest. This is exactly what the concentration of folic acid should be so that the risk of developing defects is minimal. It has been proven that the duration of folic acid intake necessary to achieve its concentration in erythrocytes of 906 nmol/l should be:
- at a dose of 400 mcg/day - 8-12 weeks;
- at a dose of 800 mcg / day - 4.2-3.5 weeks.
When planning pregnancy and pregnancy itself, it is not possible to replenish this amount of folic acid with food. It has been proven that European women with a quality diet with food receive 0.3 mg of folic acid per day (should be 0.8 mg). In order to make up the difference of 0.5 mg/day, you need to eat 15 servings of spinach or broccoli (foods with the maximum content of folates or folic acid).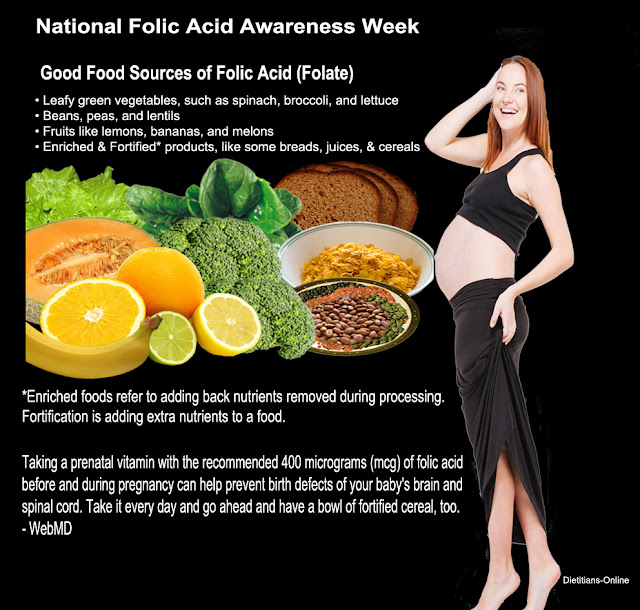 nine0003
nine0003
MTHFR enzyme deficiency
The speaker recalled that MTHFR enzyme deficiency leads to poor absorption of folic acid. According to the Ukrainian Institute of Clinical Genetics of Kharkiv National Medical University, a decrease in the activity of the MTHFR enzyme by 65% is observed in homozygotes (7.04% of Ukrainians) and by 30% in heterozygotes (40.7% of Ukrainians). It has been shown that the absorption of different types of folates in the presence of genetic mutations is different. So, when taking 200 μg of folic acid, patients with a heterozygous carrier type will not receive enough folic acid (48% of patients will not receive an adequate dose). In the presence of genetic mutations, the amount of folic acid that can be absorbed from a dose of 400 mcg is significantly reduced (48% of patients will not receive an adequate dose of folic acid). In the presence of genetic mutations, the amount of folic acid that can be absorbed from a dose of 800 mcg is reduced only in patients with homozygous mutations, this is only 7% of the total. It has been proven that 800 mcg of folic acid provides the body with folates even in the presence of a heterozygous defect in the MTHFR enzyme. nine0003
It has been proven that 800 mcg of folic acid provides the body with folates even in the presence of a heterozygous defect in the MTHFR enzyme. nine0003
Vitamin D (cholecalciferol)
Vitamin D is also important during pregnancy, the need for it increases in the II-III trimester of pregnancy. Vitamin D has a positive effect on the development of the fetus and the course of pregnancy itself. At the same time, a lack of cholecalciferol is associated with an increased risk of intrauterine infections and gestosis and can lead to a delay in the development of the fetal skeleton, a decrease in body weight at birth, and a risk of rickets in children.
According to the Order of the Ministry of Health (MoH) of Ukraine dated July 15, 2011 No. 417 "On the organization of outpatient obstetric and gynecological care in Ukraine", during pregnancy and lactation, the recommended dose of vitamin D is 10 mcg or 400 IU / day . nine0003
The Royal College of Obstetricians & Gynecologists recommend that women at risk of preeclampsia take 800 IU of vitamin D daily as a preventive measure.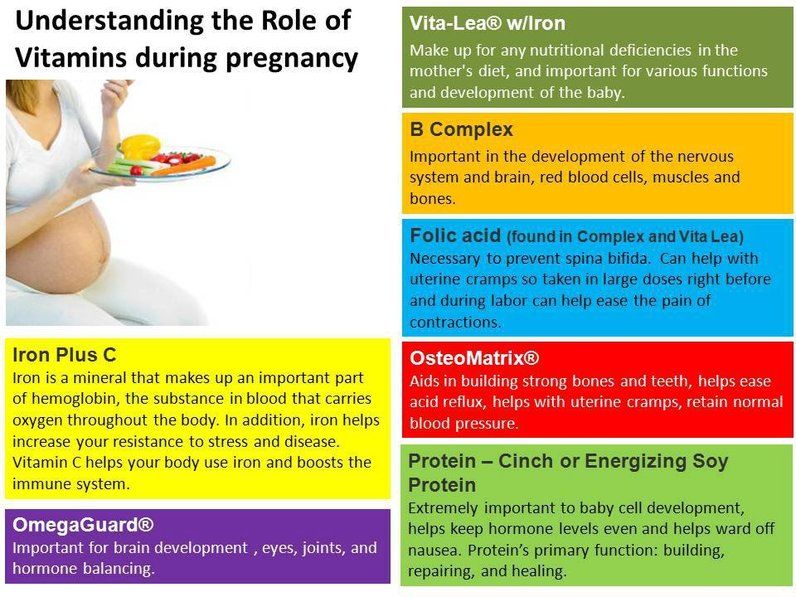
Iron
It has been proven that during pregnancy it is advisable to use ferrous rather than ferric iron preparations, which have fewer side effects. Ferrous iron is absorbed more efficiently, transported faster, and the level of ferritin and hemoglobin increases on the 2nd or 3rd day. nine0003
In accordance with Ukrainian recommendations (Order of the Ministry of Health of Ukraine dated 15.07.2011 No. 417), every woman who comes to register for pregnancy must undergo screening for latent anemia. The National Institute for Health and Care Excellence recommends that pregnant women should be screened for anemia and supplemented with iron if indicated.
Combining iron and folic acid can reduce the risk of neonatal and infant mortality. A decrease in neonatal and infant mortality by 35% and 33%, respectively, was shown among live births whose mothers started taking iron and folic acid supplements in the first 4 months of gestation. nine0003
It should be remembered that iron deficiency anemia is a factor in aggravating the course of pregnancy and the risk of developing major obstetric syndromes, in particular, in the mother it can increase the risk of preeclampsia, mortality, in the fetus - fetal growth retardation syndrome, early development of placental dysfunction, in children born on against the background of anemia during pregnancy, metabolic syndrome, schizophrenia, mental retardation.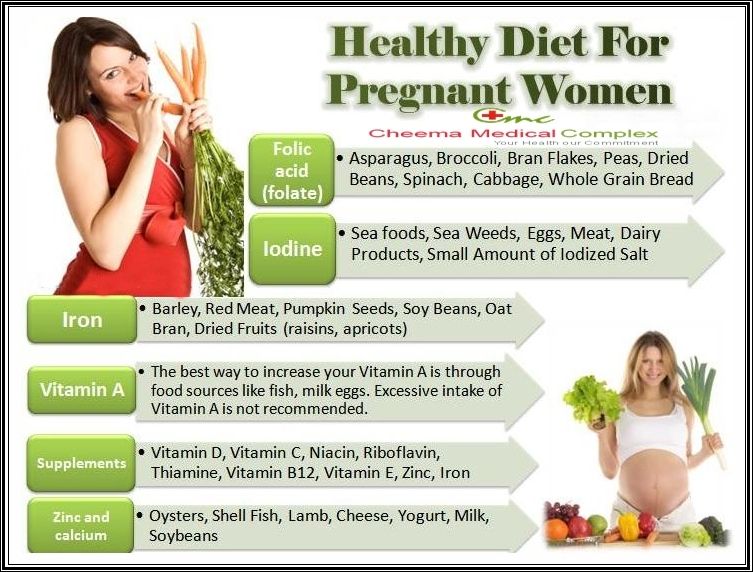
Multivitamin complexes: international recommendations
In accordance with the Canadian principles of preconception prevention of birth defects at low risk, a multivitamin containing 0.4-1.0 mg of folic acid should be taken 2-3 months before conception, throughout pregnancy and 6 weeks after delivery (lactation period) ). At moderate risk, daily multivitamin preparations with 1.0 mg of folic acid are recommended for at least 3 months before conception, for 12 weeks of gestation, then 0.4–1.0 mg of folic acid from the 12th week until the end of pregnancy and 6 weeks postpartum. At high risk, take a multivitamin with 1.0 mg of folic acid and an additional 3.0 mg of folic acid (for a total of 4.0 mg) or a prescription multivitamin containing 5.0 mg of folic acid at least 3 months before conception and 12 weeks of gestation. nine0003
The United States Prevention Task Force (USPSTF) recommends a vitamin supplement containing 400–800 mcg of folic acid for women planning pregnancy.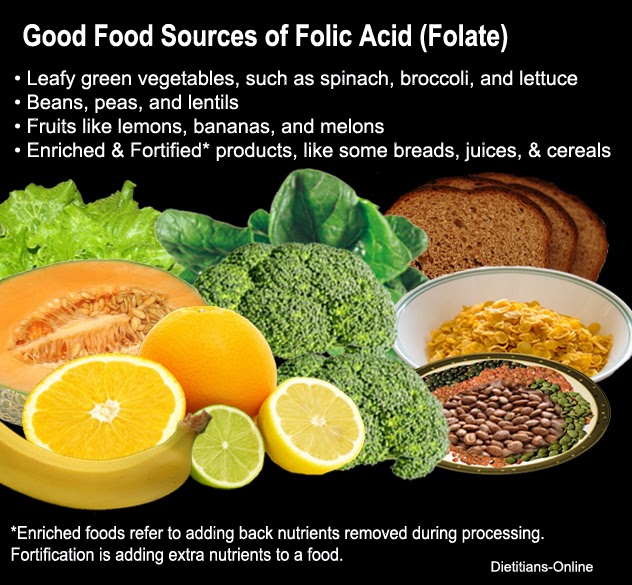
The Italian recommendations for nutrient use during pregnancy and lactation indicate that vitamin complexes should ideally be given 2 months before pregnancy at a dose of 800 mcg.
New Zealand OB/GYNs recommend taking 800 mcg of folic acid daily for at least 4 weeks before pregnancy and for 12 weeks after pregnancy to reduce the risk of developing neural tube defects. nine0003
The experience of the USA and European countries shows that vitamin-mineral complexes are the best choice for women. To ensure a sufficient amount of micronutrients during the periods of preparation for pregnancy, pregnancy itself and breastfeeding, it is advisable to use vitamin-mineral complexes with proven effectiveness. When choosing a multivitamin-mineral complex, preference should be given to preparations containing the full range of essential vitamins and trace elements that provide the daily requirement of a pregnant woman. European and American experts do not recommend the use of dietary supplements during pregnancy, only drugs with proven efficacy and safety.