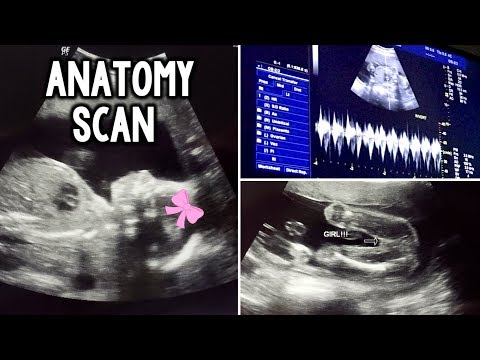
Nuchal scan 12 weeks
12 Week Scan | SO + GI Scan
At 12 Weeks: Nuchal Translucency ScanThe nuchal translucency (NT) scan, or “12-week scan,” is an ultrasound performed in the first trimester between 11.5 weeks and 13 weeks, six days. This scan is combined with a blood test that looks at two specific hormones of pregnancy: the free-Beta hCG and PAPP-A (pregnancy associated plasma protein A). This combined test is an extremely accurate non-invasive screening test available to help identify a fetus at risk for Down syndrome as well as other chromosomal abnormalities and some major structural abnormalities. The sensitivity of this only recently eclipsed by NIPT. An ultrasound screening test is non-invasive and does not have any side effects or complications.
However, it will not give a yes/no answer to whether a problem such as Down syndrome is present. The only way to diagnose Down syndrome or other chromosomal abnormalities is by having a diagnostic test — either a CVS or an amniocentesis — and testing the fetal cells. These tests are invasive and require a needle to be passed into the maternal abdomen and uterus and therefore carry a small risk of miscarriage.
Many patients do not wish to have the diagnostic test because of the small risk of miscarriage and prefer to have the ultrasound screening test, the NT scan, to help them decide if they wish to proceed to testing the fetus. Unfortunately, while NT combined with the first trimester biochemical blood test is a very accurate screening test available for chromosomal abnormalities, it will not detect all fetuses affected with Down syndrome or other chromosomal abnormalities.
Chromosomal abnormalities occur when there is a change in the number or structure of the chromosomes. Normally we have 46 chromosomes, 23 pairs numbered 1-22 and a pair of sex chromosomes.
Boys have XY and girls have XX. The most common chromosomal abnormality seen at birth is Down syndrome. In Down syndrome, an extra copy of chromosome 21 is present, giving a total of 47 chromosomes.
Accredited practices:
To be certain your NT scan is performed correctly, it is important that you have your scan performed at an accredited practice. A NT computer package was developed by the London Fetal Medicine Foundation in the 1990s and was based on more than 100.000 pregnancies.
Strict auditing of the NT ultrasound work performed by every accredited practice in the world is undertaken several times a year. This ensures that the NT scan test is being performed correctly. Recently, the Royal Australian College of Obstetricians and Gynaecologists has taken over regular auditing of Australian practices.
Advantages of the 12 week NT scanThere are several advantages to undergoing a 12-week NT scan, including:
- Estimate individual risk for Down syndrome and other chromosomal abnormality
- Screen for spina bifida
- More accurately date the pregnancy
- Diagnose multiple fetuses
- Diagnose early pregnancy failure
- Allow early detection of some major abnormalities
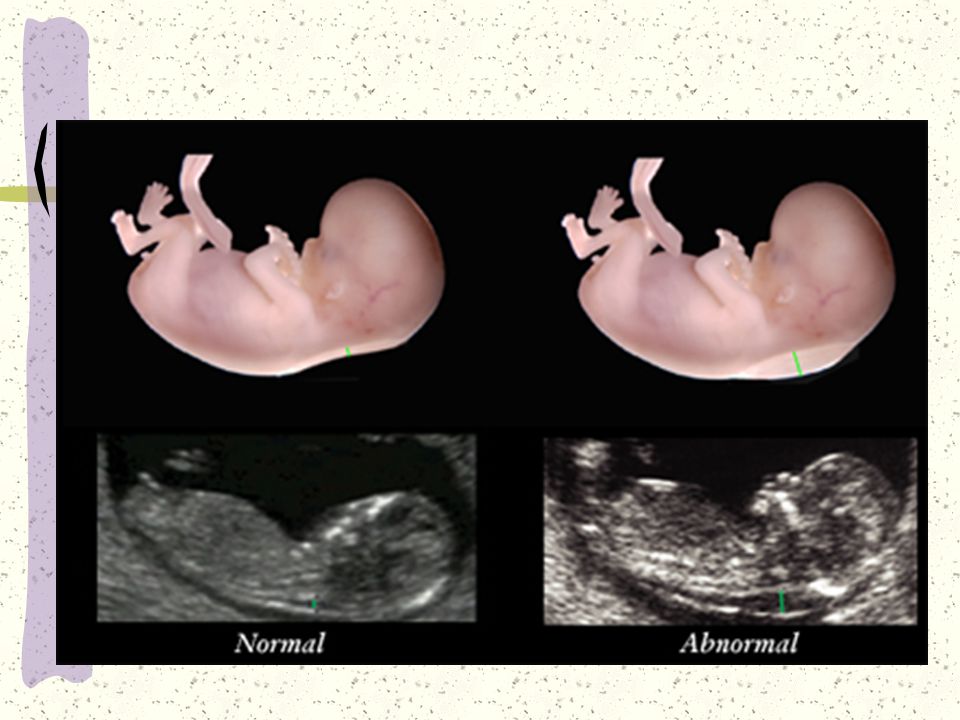
At the end of the first trimester, there is usually a small amount of fluid beneath the skin of the fetus at the back of the head and neck. This fluid is called the nuchal translucency (NT), and can be easily and accurately measured to within a tenth of a millimetre.
This fluid is called the nuchal translucency (NT), and can be easily and accurately measured to within a tenth of a millimetre.
When there is extra fluid and the NT measurement is thicker than normal, there is an association with chromosomal anomalies such as Down syndrome and some structural abnormalities in the fetus. Not all babies with an increased NT measurement have Down syndrome or any structural abnormality.
The extra fluid at the back of the head and neck usually disappears by 18 weeks. The fluid in itself is not an abnormality and does not harm the baby but may simply be the sign of a potential problem. The baby is measured from head to bottom to determine the crown-rump length and the nuchal translucency is measured. These measurements are entered into the computer program with the patient’s date of birth and the first trimester biochemistry blood test. The computer then calculates the patient’s age-related risk for Down syndrome and the new individual risk for this pregnancy.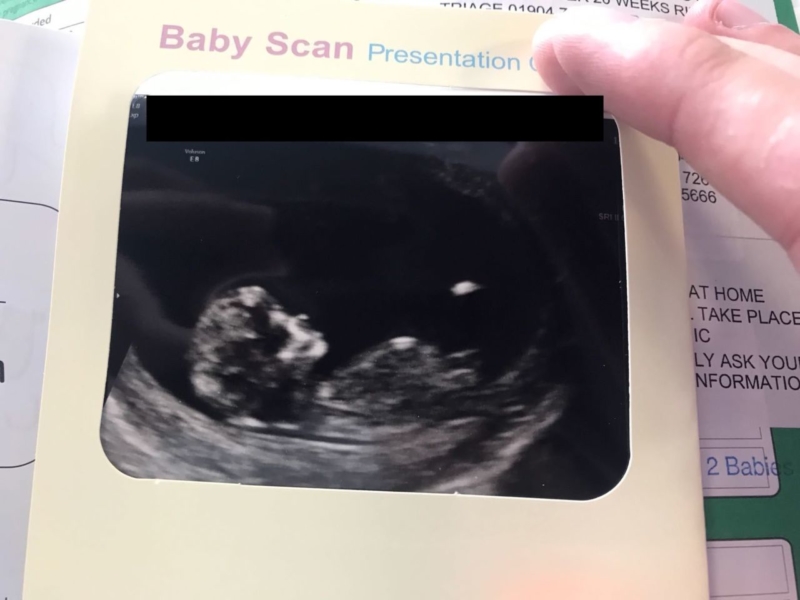 The findings are then discussed with the patient. The combined NT result will provide the patient with a risk assessment. This will either be a high risk (risk is greater than 1 in 300) or a low risk (risk less than 1 in 300). As this is a screening test and not a diagnostic test, even with a low calculated risk, Down syndrome is not completely excluded and can still occur occasionally.
The findings are then discussed with the patient. The combined NT result will provide the patient with a risk assessment. This will either be a high risk (risk is greater than 1 in 300) or a low risk (risk less than 1 in 300). As this is a screening test and not a diagnostic test, even with a low calculated risk, Down syndrome is not completely excluded and can still occur occasionally.
Free- BhCG (Beta human chorionic gonadotrophin) and PAPP-A (Pregnancy associated plasma protein-A) levels can be assessed from a blood test. This is best done at 10 weeks, some two weeks prior to the NT scan but it can also be done just before or on the same day as the NT scan. The PAPP-A level tends to be lower and the BhCG level tends to be higher in pregnancies affected by Down syndrome.
Accuracy of Nuchal TranslucencyWhen the ultrasound is combined with the first trimester blood test (BhCG and PAPPA) and nasal bone, the detection rate increases to 95%. None of these screening tests can give 100% detection. If a pregnant woman wants to completely exclude a chromosome abnormality, then she should consider having prenatal testing with either a CVS or an amniocentesis. Genetic counselling is also recommended. The results of the examination will be available to you shortly after the examination. One of our genetic counsellors or doctors will be available to discuss the result and the options for further testing.
None of these screening tests can give 100% detection. If a pregnant woman wants to completely exclude a chromosome abnormality, then she should consider having prenatal testing with either a CVS or an amniocentesis. Genetic counselling is also recommended. The results of the examination will be available to you shortly after the examination. One of our genetic counsellors or doctors will be available to discuss the result and the options for further testing.
Nuchal translucency scan - 12 week scan, down's syndrome screening.
This is often parents’ favourite scan – you will be amazed at just how much detail you can see and if everything looks normal, the risk of miscarriage and major abnormality becomes very small. If you haven’t had a scan yet, this scan will:
- Make sure that the pregnancy is in the right place
- Count how many babies there are!
- Accurately date your pregnancy and decide on a definite due date for you
- Look at the basic structure of the baby
But the main purpose of this particular scan is to screen for chromosomal abnormalities such as Down’s syndrome.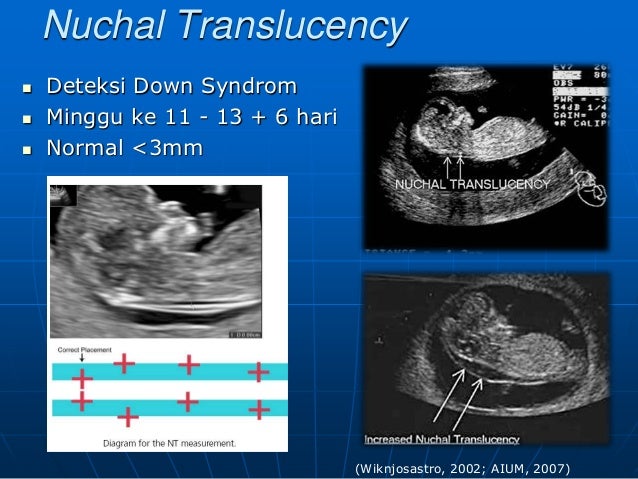 Down’s syndrome is something that affects about 1 in 700 pregnancies overall, but it becomes more common as a mother gets older. It happens because the egg that is released at conception has an extra copy of chromosome 21 and this in turn leads to every cell in the baby having an extra copy of chromosome 21.
Down’s syndrome is something that affects about 1 in 700 pregnancies overall, but it becomes more common as a mother gets older. It happens because the egg that is released at conception has an extra copy of chromosome 21 and this in turn leads to every cell in the baby having an extra copy of chromosome 21.
This causes a wide range of both physical disability and learning difficulties. At the moment there still isn’t a completely safe test that will tell you that your baby definitely does or doesn’t have Down’s syndrome, but the NHS offers everyone combined first trimester screening, which is a test performed at around 12 weeks using a combination of ultrasound scan findings and a basic blood test to assess the likelihood of whether your baby is or isn’t affected. The key ultrasound marker at this stage is the nuchal translucency measurement, or the space at the back of the baby’s neck. At this stage in the baby’s development it is normal for some fluid to build up in this space at the back of the baby’s neck – it happens to every baby so a little bit of fluid is entirely normal, but a baby with problems will often retain more fluid and the nuchal translucency measurement is increased. As well as being a good marker for babies with Down’s syndrome, an increased nuchal translucency measurement can also pick up other genetic conditions, such as Edwards’ syndrome (where the baby has an extra copy of chromosome 18) and Patau’s syndrome (an extra copy of chromosome 13), and some other structural problems, including heart abnormalities.
As well as being a good marker for babies with Down’s syndrome, an increased nuchal translucency measurement can also pick up other genetic conditions, such as Edwards’ syndrome (where the baby has an extra copy of chromosome 18) and Patau’s syndrome (an extra copy of chromosome 13), and some other structural problems, including heart abnormalities.
The nuchal translucency scan is best done during the 12th week, but it can be done from 11 weeks and 3 days up until 14 weeks and your local NHS hospital will offer you an appointment to have this done at around this time. Nevertheless, some parents may opt to have this done privately instead.
Reasons why patients choose to have it done at Beard Mill Clinic include:
Plenty Of Time
Each appointment at Beard Mill Clinic is allocated one hour to make sure that there is plenty of time to do the scan and discuss the results with you.
Wealth Of Experience
Victoria has spent over 20 years working with Professor Kypros Nicolaides who has been the leading pioneer in developing the nuchal translucency scan and screening for abnormalities at this stage of pregnancy.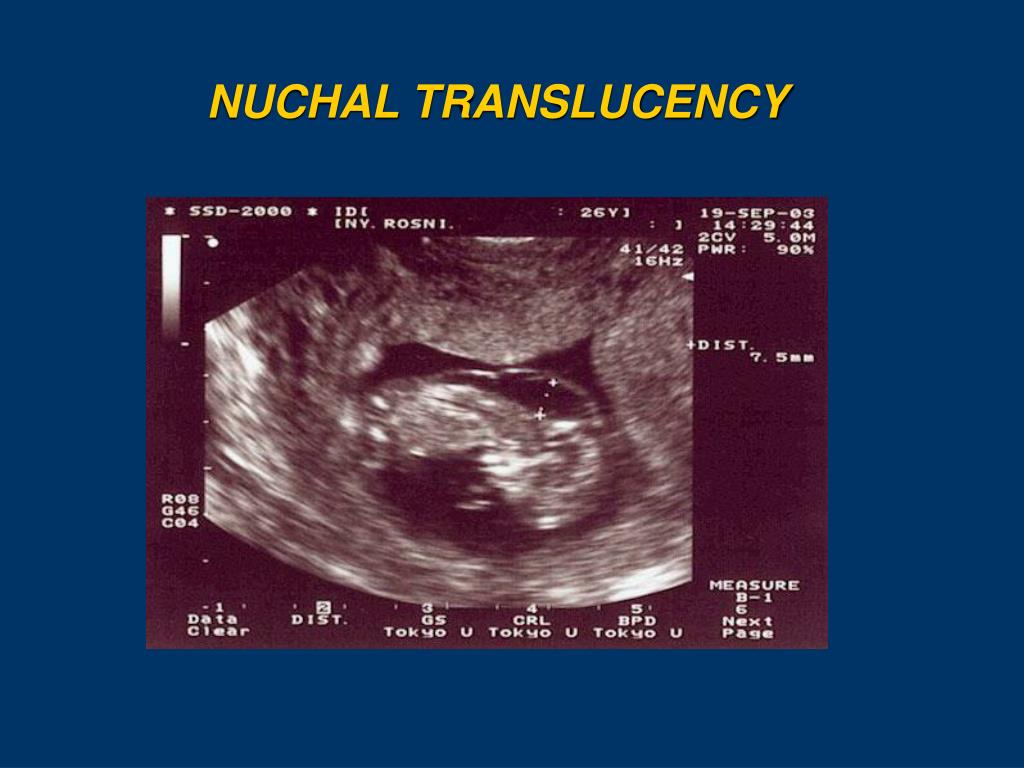 During this time, she has been directly involved in developing the risk calculation software and in teaching other people how to perform the nuchal scan. In doing this, she has come to understand the screening process inside out and can use her expertise to give you the best possible advice.
During this time, she has been directly involved in developing the risk calculation software and in teaching other people how to perform the nuchal scan. In doing this, she has come to understand the screening process inside out and can use her expertise to give you the best possible advice.
Extra Markers
Victoria is trained and certified to look at the additional markers for Down’s syndrome that are not routinely offered at most other scanning clinics. These additional markers include:
- Looking at the baby’s nose bone and its profile
- Listening to the flow of blood across a valve in the baby’s heart (the tricuspid valve)
- Measuring the resistance in the vessel that takes blood into the baby’s heart (the ductus venosus)
Babies with Down’s syndrome are more likely to have a small or absent nose bone, with a flat profile. They often have leakage across the tricuspid valve and reverse flow in the ductus venosus. So adding in these additional markers will take the average detection rate of the standard technique of 80% up to 95%.
Same Day Results
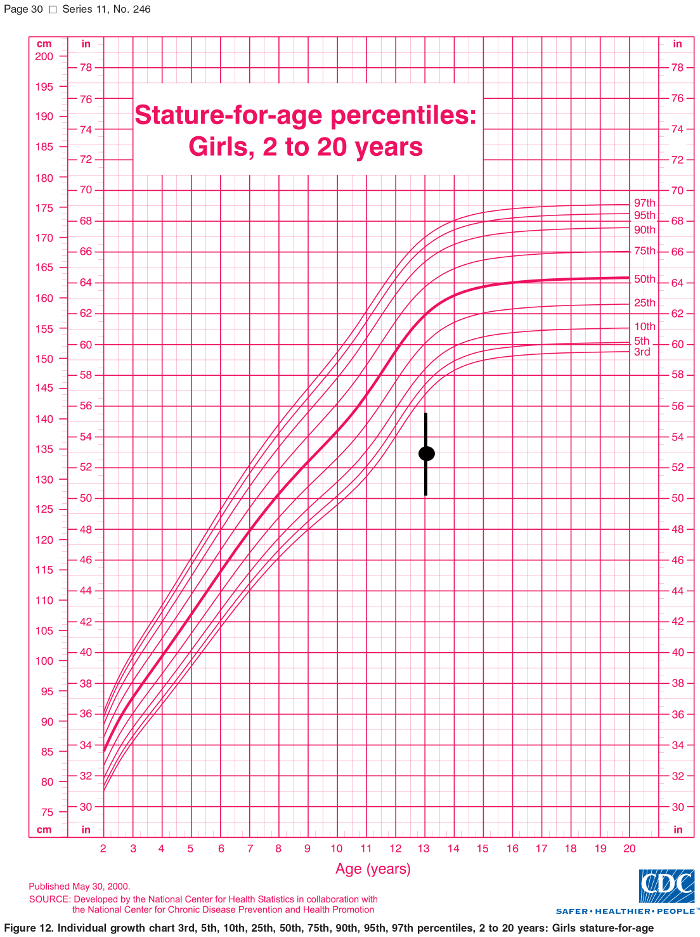
When the blood has been taken in advance of the scan, Victoria is able to process all the results straight away and explain both the scan findings and blood results to you, showing you how your measurements fall within the context of the “normal” range and how this then affects your own specific risk for Down’s syndrome.
The risk calculation software used at Beard Mill Clinic displays simple graphs which really help you understand what the risk means and Victoria gives you plenty of time to ask questions and clarify anything you are not sure about. You then take away a comprehensive report with all the results clearly documented.
Even if the blood results are not available, Victoria will give you as much explanation as she can based on the scan findings and help you to understand how the blood results fit into the risk assessment. She is able to process blood samples within 24 hours, so will ring you the following day with the final result and then e-mail you your report.
Early Blood Tests
The blood test that is used to screen for Down’s syndrome is usually taken at the time of the nuchal translucency scan, but the research data suggests that the results are actually more accurate if the blood is taken at 9 weeks, rather than 12 weeks. So wherever possible, Victoria will try to arrange for you to have your blood test before your scan. This has the double advantage of giving you the best possible result and ensuring that the blood results are ready when you come for your scan, so that your risk can be discussed with you face-to-face, rather than given to you by letter a week or two later, or over the phone.
Of course this isn’t always possible to arrange, in which case, it can be done at the same time as the scan. But as an added incentive, Victoria will offer to do a quick scan if you come to Beard Mill Clinic early to have the bloods taken, allowing you to hear the heart beat and to check your dates. There is no additional charge for this.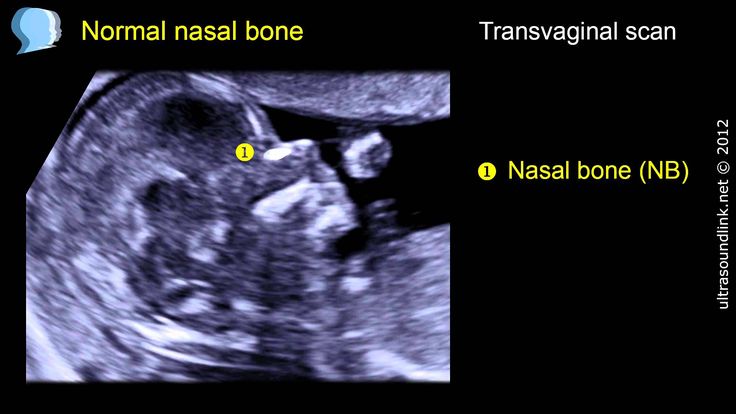
Awkward Babies
Some of the patients who contact Beard Mill Clinic about the nuchal translucency scan do so because it hasn’t been possible to measure the nuchal when they went for their routine NHS appointment. This is often because the baby wasn’t in the right position, but Victoria has the luxury of much more time and has not yet failed to get a nuchal measurement. So if you find yourself in this position, do ring to make an appointment.
Referral For Further Tests
In most cases, patients will be reassured by their result, but if your risk of Down’s syndrome is high, or a problem is suspected, Victoria will arrange a direct referral to your own NHS consultant and ensure you receive the right follow-up.
Full Explanation
Taking the measurements is the easy bit, interpreting the results and communicating these to the parents can sometimes be the more challenging part of screening. And this is where Victoria’s expertise comes into its own.
Through her training, she has acquired a deep understanding of how the individual components of the screening tests work and endeavours to explain this as fully as she can.
She is passionate about providing each and every patient with the best possible standard of screening and then equipping them with the knowledge and understanding to use this information appropriately.
Importance of ultrasound at 12 weeks of gestation
Ultrasound at 12 weeks of gestation
Nowadays, monitoring the course of pregnancy is difficult to imagine without ultrasound. This method is safe, painless and universal in terms of the fact that the doctor has the opportunity to evaluate various parameters of fetal development, and the functional features of the placenta, uterus, and umbilical cord.
According to the norms established by the Ministry of Health of the Russian Federation, the first screening ultrasound is done to women at the 12th week of pregnancy. nine0005
Why is ultrasound done at 12 weeks pregnant?
At the end of the first trimester, namely at 12 weeks (perhaps a little earlier or a little later), every pregnant woman should undergo an ultrasound screening. This procedure is carried out in order to:
This procedure is carried out in order to:
- Confirm pregnancy (after all, sometimes tests or blood tests for hCG can give ambiguous results).
- Confirm the correct position and attachment of the gestational sac with the embryo. Pregnancy must be uterine. The ectopic location of the fetal egg is a serious pathology that requires immediate medical intervention. nine0017
- Detection of pathologies of the female reproductive system that may adversely affect the process of bearing a fetus. For example, at the first ultrasound, the length of the cervix is estimated. If it has an insufficient value (1-1.5 mm), this indicates the presence of isthmic-cervical insufficiency, which can lead to miscarriage.
- Specify the gestational age, that is, the gestational age.
- Assess the level of development of the fetus and the preliminary result of the process of laying its main internal organs. nine0017
- Assess how correctly and fully formed the fetal heart muscle.

- Detect primary markers of chromosomal or genetic disorders. Not all such pathologies can be detected at a period of 12 weeks, but, for example, it is possible to suspect Down syndrome in an unborn child after the first screening.
Ultrasound at the 12th week of pregnancy (screening of the research norms will be described below) is also the first opportunity for a future mother to see her baby, which, of course, causes a lot of positive, useful emotions. nine0005
How to prepare for screening?
Ultrasound during pregnancy is a procedure that does not require special preparation. Women are only recommended 2-3 days before the study to refrain from food that provokes excessive gas formation in the intestines. Otherwise, you just need to come to the doctor’s appointment calm and in a good mood.
How is the first ultrasound at 12 weeks?
There are two options for doing an ultrasound at 12 weeks of gestation:
- Transvaginally - using a special vaginal probe inserted into the pregnant woman's vagina.
- Transabdominal - examination is carried out through the skin of the abdomen of a pregnant woman using a special gel.
What does ultrasound show at 12 weeks pregnant?
An ultrasound at week 12 shows the size of the fetus, the location of the fetal egg, the place of attachment of the chorion (future placenta), the level of the fetal heartbeat, and the amount of amniotic fluid. nine0005
If an ultrasound scan at 12 weeks of gestation shows that the fetus is developing abnormally, the attending physician should assess how critical this deviation is and how it may affect the health of the unborn child. Perhaps a slight discrepancy in the size of the fetus is due to its anatomical or physiological features and it is impossible to speak of the presence of a gross pathology. To clarify the diagnosis, an additional ultrasound is usually prescribed a few weeks after the first one. nine0005
If ultrasound, as well as the results of other tests, indicate that the fetus has a certain chromosomal disorder, then the question of terminating the pregnancy may be raised. The decision in this case should be made by the woman, and the doctor is obliged to give her his recommendations.
The decision in this case should be made by the woman, and the doctor is obliged to give her his recommendations.
Child gender
The gender of the child is a criterion that is not included in the mandatory protocol for ultrasound examination. Gender does not affect the normal development of the fetus, but almost every expectant mother wants to know as soon as possible who will be born to her, a daughter or a son. nine0005
At 12 weeks it is difficult to determine the sex of the unborn child. Some ultrasound specialists, by measuring the angle of the genital tubercle, may suggest whether it will be a boy or a girl. The error rate is 50%, so you need to be patient and wait at least until 16-20 weeks, when the sex can be seen more clearly.
Heart rate limits
The study of the heart of the unborn child is one of the main aspects of ultrasound at 12 weeks of pregnancy, the norms for it are as follows:
- From 0 to 5 weeks, when the embryo is just born and its size is from 2 to 15 mm, the heart rate can be 80-130 bpm.

- From 5 to 8 weeks, the fetal heart may beat at a rate of 120-170 bpm.
- By week 12, heart rate may be 170-190 bpm.
KTR
KTR, that is, the size of the fetus from the coccyx to the crown, is an important criterion for assessing development in the first trimester of pregnancy. For a period of 12 weeks, it can be 42-59mm. This parameter is included in the mandatory ultrasound protocol of the first trimester.
Child head BPR norms
After ultrasound of 12 weeks of pregnancy , the decoding of its results and their comparison with the norm are carried out immediately. First of all, the doctor evaluates the biparietal size of the fetal head. At 12 weeks, it should be approximately 21 mm.
If BDP turns out to be more than normal, but at the same time all other fetal parameters (KTR, femur length, and so on) exceed it, we can say that this is just a large fetus. nine0005
nine0005
If BDP exceeds the norm, and all other indicators fit into it, fetal hydrocephalus is most often suspected.
Nose length standards
When deciphering an ultrasound at 12 weeks of gestation, such an indicator as the length of the fetal nose (the length of the nasal bone) is necessarily taken into account. More precisely, first of all, the doctor evaluates whether the nasal bone is visualized in principle. Its size (length) for a period of 12 weeks should be approximately 3 mm.
In cases where the nasal bone of the fetus is not visualized, there is a risk that the child will be born with Down syndrome. For a more accurate determination of this chromosomal pathology, another indicator is analyzed - the thickness of the collar space (NTP). This is a space of accumulation of fluid between the neck of the fetus and the upper shell of its skin. If TVP is greater than normal, and the nasal bone is not visualized, the likelihood of the fetus having chromosomal abnormalities is assessed as high. nine0005
nine0005
Is it necessary to have an ultrasound at 12 weeks?
If a woman wants to endure and give birth to a healthy child, reduce the risk of miscarriage or pregnancy fading, then she definitely needs to undergo an ultrasound scan in the first trimester of pregnancy. No hard deadlines have been set. Ultrasound can be done both at 12 and, for example, at 11 or 13 weeks (but no later than 14 weeks). It all depends on the course of pregnancy, the woman's well-being, the results of a blood test. The best advice on when to have an ultrasound can only be given by your doctor. nine0005
12 week fetal ultrasound
- First trimester prenatal screening
- Ultrasound at 12 weeks for Down syndrome
- Ultrasound at 12 weeks for Edwards syndrome
- Ultrasound at 12 weeks for Patau syndrome
- Ultrasound at 12 weeks for Turner syndrome
- Ultrasound at 12 weeks for Triploid Syndrome
- Biochemical prenatal screening
- Fetal development by week
- Our apparatus
- other types.
 ..
.. - Pregnancy management
- Fetometry data at various times
The cost of ultrasound in the first trimester up to 10 weeks is 450 UAH. The price includes biometrics according to protocols, 3D/4D visualization.
The cost of ultrasound in the first trimester for a period of 10 weeks 6 days is 550 hryvnia. The price includes prenatal screening, biometric protocols, 3D/4D visualization.
The cost of a comprehensive prenatal screening by PRISCA (ultrasound + beta hCG + PAPP with the calculation of the individual risk of chromosomal pathologies (for example, Down syndrome or Edwards syndrome) - 1005 hryvnia.
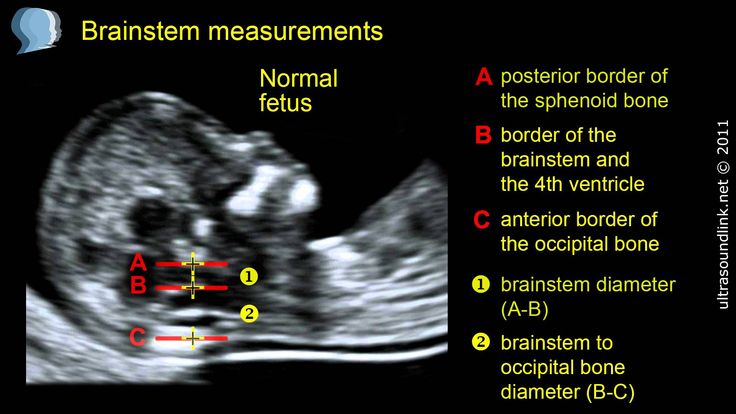
Fetal ultrasound at 12 weeks of gestation takes a number of very important measurements to identify the risk group for fetal chromosomal abnormalities. It has been established that the most optimal time for screening the first trimester of pregnancy is 12 weeks of pregnancy (from 11 to 13 weeks and 6 days). With ultrasound of the fetus at 12 weeks of gestation, is measured in addition to the length of the embryo (coccygeal-parietal size - KTR), the size of the fetal head (head circumference, biparietal size, fronto-occipital size). Mandatory ultrasound of the fetus at 12 weeks of gestation is an assessment of the structures of the fetal brain, the symmetry of the hemispheres. Normally, the fetal brain on ultrasound looks like a butterfly. The long bones of the fetus (shoulder, ulna, radius, femur, tibia, fibula) are measured, the symmetry of the limbs and their motor activity are assessed. With ultrasound of the fetus at 12 weeks of gestation, the transverse size of the abdomen of the fetus, the circumference of the abdomen are measured, the presence of the stomach, heart in typical places is noted. When conducting an ultrasound of the fetus at 12 weeks of gestation, the presence of heart defects can be suspected with sufficient resolution of the ultrasound scanner and the proper experience and education of the ultrasound operator. There are published data on the diagnosis of transposition of the great vessels, the common atrioventricular canal, cardiac ectopia, etc., registered during fetal ultrasound at 12 weeks of gestation.
Mandatory ultrasound of the fetus at 12 weeks of gestation is an assessment of the structures of the fetal brain, the symmetry of the hemispheres. Normally, the fetal brain on ultrasound looks like a butterfly. The long bones of the fetus (shoulder, ulna, radius, femur, tibia, fibula) are measured, the symmetry of the limbs and their motor activity are assessed. With ultrasound of the fetus at 12 weeks of gestation, the transverse size of the abdomen of the fetus, the circumference of the abdomen are measured, the presence of the stomach, heart in typical places is noted. When conducting an ultrasound of the fetus at 12 weeks of gestation, the presence of heart defects can be suspected with sufficient resolution of the ultrasound scanner and the proper experience and education of the ultrasound operator. There are published data on the diagnosis of transposition of the great vessels, the common atrioventricular canal, cardiac ectopia, etc., registered during fetal ultrasound at 12 weeks of gestation.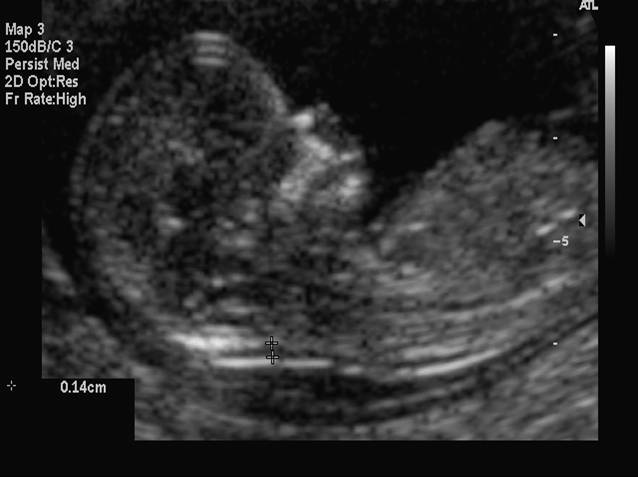 nine0005
nine0005
First trimester prenatal screening
In addition to the above measurements, fetal ultrasound at 12 weeks of gestation screens for fetal chromosomal abnormalities. It has been established that most chromosomal pathologies are accompanied by an increase in the collar space located in the neck of the fetus. This feature is due to the fact that with chromosomal abnormalities of the fetus, in particular with Down syndrome, the skin has increased folding, i.e., roughly speaking, there is more skin. Fluid accumulates under such skin, which contributes to the visualization of a thickening of the collar zone during ultrasound of the fetus at 12 weeks of gestation. In fetuses with a karyotype disorder (with chromosomal diseases), the thickness of the collar zone is 2.5 mm (or more) greater than the average value for a given gestational age in fetuses with a normal karyotype. nine0005
Fetal ultrasound at 12 weeks of gestation in Down's syndrome
In addition to the enlargement of the nuchal area in trisomy 21 (Down's syndrome), 60–70% of fetuses do not visualize the nasal bones. It is noticed that people with Down syndrome have a short nose. In the process of embryogenesis, the nose with Down syndrome (nasal bones) is formed later than in fetuses with a normal karyotype. Also, from 15 to 21 weeks of gestation, there is an increased frequency of shortening of the nasal bones compared with the average values for this gestational age in fetuses with Down syndrome. nine0005
It is noticed that people with Down syndrome have a short nose. In the process of embryogenesis, the nose with Down syndrome (nasal bones) is formed later than in fetuses with a normal karyotype. Also, from 15 to 21 weeks of gestation, there is an increased frequency of shortening of the nasal bones compared with the average values for this gestational age in fetuses with Down syndrome. nine0005
Fetuses with Down's syndrome have a shortening of the upper jaw, resulting in smooth facial contours.
In fetuses with Down's syndrome, dopplerometry determines the pathological nature of the curves of blood flow velocities in the venous duct. Assessment of the nature of blood flow in the venous duct is one of the mandatory screening parameters when performing ultrasound of the fetus at 12 weeks as part of the prenatal screening of the first trimester. Reverse blood flow in the venous duct is considered pathological. nine0005
Fetal ultrasound at 12 weeks of gestation in Edwards syndrome
Trisomy 18 (Edwards syndrome) is characterized by early manifestations of slow fetal development and a tendency to bradycardia (decrease in fetal heart rate). Moreover, up to a certain period of pregnancy, the fetus develops normally (more often up to 8 weeks of pregnancy).
Moreover, up to a certain period of pregnancy, the fetus develops normally (more often up to 8 weeks of pregnancy).
Fetuses with Edwards syndrome show a lack of visualization of the nasal bones. nine0005
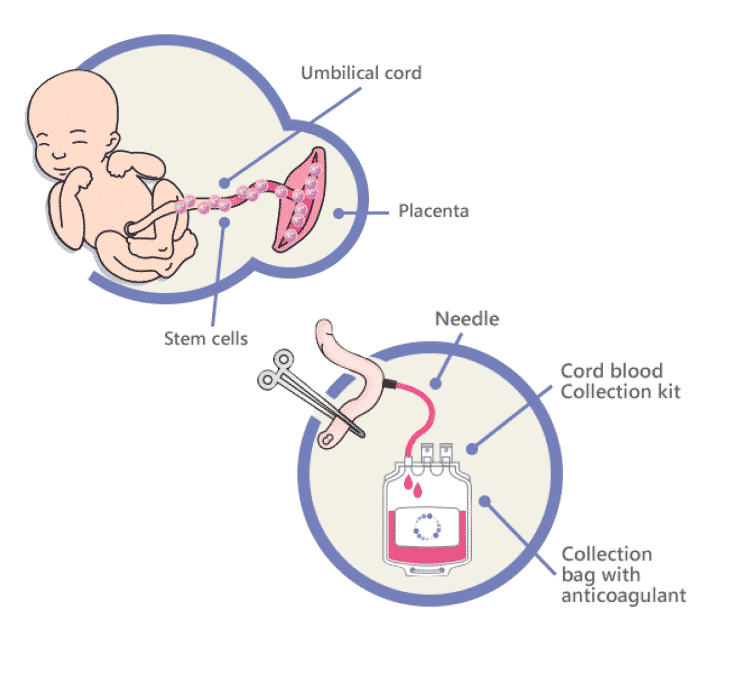
In fetuses with Edwards syndrome, a single umbilical artery is a common finding. Normally, the umbilical cord has two arteries and one vein.
Ultrasound of the fetus at 12 weeks of pregnancy with Patau syndrome
With trisomy 13, 70% of fetuses have tachycardia (increased heart rate).
Also in fetuses with Patau syndrome, early detection of fetal growth retardation may occur.
Fetuses with Patau syndrome have megacystis (bladder enlargement). nine0005
Fetal holoprosencephaly in Patau's syndrome (impaired brain formation) and omphalocele are more often combined signs detected by ultrasound of the fetus at 12 weeks of gestation.
Ultrasound of the fetus at 12 weeks of gestation with Turner syndrome
In Turner syndrome, 50% of fetuses have tachycardia (rapid heart rate over 160 beats per minute) and early signs of fetal growth retardation (the size of the fetus ceases to correspond to the gestational age, usually from 8 weeks of gestation. nine0005
nine0005
Ultrasound of the fetus at 12 weeks of gestation with Triploid syndrome
Triploidy is characterized by early signs of slowing down the development of an asymmetric type.
Bradycardia (heart rate below 120 beats per minute), holoprosencephaly (violation of the division of the brain into sections, and, accordingly, the impossibility of normal mental development of the child), omphalocele (eversion of the abdominal organs into the hernial sac in the umbilical cord) are also characteristic of triploidy. nine0005
Posterior fossa cysts, choroid plexus cysts. Cysts are represented by the accumulation of fluid in the brain. The presence of bilateral cysts is considered an unfavorable sign, while the isolated presence of one small cyst in the brain (in particular, choroid plexus cysts), the absence of other markers of chromosomal diseases are not regarded as a pathology and require dynamic monitoring.
Early pyelectasis (dilation of the renal pelvis) is also a marker of fetal chromosomal abnormalities. nine0005
nine0005
All of these data can be recorded with a fetal ultrasound at 12 weeks of gestation. It is important to note that the presence of these markers is not a diagnosis that reliably confirms the presence of a chromosomal pathology in the fetus. If several markers of fetal chromosomal pathologies listed above are detected during ultrasound, invasive prenatal diagnosis is recommended to obtain material of fetal origin. These procedures include amniocentesis and chorionbiopsy. After receiving a section of the chorion (placenta) or amniotic fluid, the chromosome set of the child is determined (karyotyping). Only karyotyping is the reason for the diagnosis of a chromosomal abnormality in the fetus. nine0005
Biochemical prenatal screening
Ultrasound data are supplemented with biochemical markers of chromosomal pathologies. The "double test" includes the determination of beta-hCG and pregnancy-associated protein A (PAPP-A) in the mother's fasting blood. Normative values are calculated according to the average values for a given gestational age and are defined as MoM. MoM indicators from 0.5 to 2 are considered normal. Moreover, the changes should deviate from unity in one direction. That is, if beta hCG is 1.3 MoM, and PAPP-A is 1.4 MoM, this is normal, while the PAPP-A indicator of 0.6 MoM with hCG 1.3 MoM may indicate the implementation of an unfavorable development of pregnancy on later terms, for example, the development of late preeclampsia. Deviations in the "Double test" from normal (beyond 0.5-2 MoM) may be alarming due to the presence of a chromosomal abnormality in the fetus. But the "Double test" is evaluated only in combination with screening Fetal ultrasound at 12 weeks gestation . Down syndrome is characterized by an increase in beta hCG by several times (2.5-3 MoM and above) with normal or reduced PAPP-A. An important condition for conducting the "Double Test" and assessing its reliability are the timing - exclusively from 11 weeks to 13 weeks and 6 days of pregnancy (obstetric period).
MoM indicators from 0.5 to 2 are considered normal. Moreover, the changes should deviate from unity in one direction. That is, if beta hCG is 1.3 MoM, and PAPP-A is 1.4 MoM, this is normal, while the PAPP-A indicator of 0.6 MoM with hCG 1.3 MoM may indicate the implementation of an unfavorable development of pregnancy on later terms, for example, the development of late preeclampsia. Deviations in the "Double test" from normal (beyond 0.5-2 MoM) may be alarming due to the presence of a chromosomal abnormality in the fetus. But the "Double test" is evaluated only in combination with screening Fetal ultrasound at 12 weeks gestation . Down syndrome is characterized by an increase in beta hCG by several times (2.5-3 MoM and above) with normal or reduced PAPP-A. An important condition for conducting the "Double Test" and assessing its reliability are the timing - exclusively from 11 weeks to 13 weeks and 6 days of pregnancy (obstetric period).
Thus, prenatal screening of the first trimester of pregnancy takes into account the age of the pregnant woman (after 35 years, the risk of fetal chromosomal abnormality in this woman is higher), ultrasound data, biochemical marker data (“Double test” and “Triple test”). nine0005
nine0005
Of course, the most important of the three indicators (ultrasound, biochemical screening, woman's age) is still ultrasound in prenatal screening.
For high-quality ultrasound screening, it is important to exclude the presence of the listed markers of chromosomal pathologies. Indispensable assistance in prenatal ultrasound screening of the first trimester is the use of 3d 4d ultrasound during pregnancy. With the help of 3d 4d ultrasound during pregnancy, volumetric reconstruction of parts of the body of the fetus and the fetus as a whole is performed. With the help of 3d 4d ultrasound during pregnancy, unilateral aplasia (absence) of the nasal bone is excluded. The unilateral absence of the nasal bone is also a marker of chromosomal pathology, and during a conventional ultrasound, depending on the side of the scan, you can see one nasal bone and not notice the absence of the second bone on the other side. 3d 4d Ultrasound during pregnancy allows you to prevent such a mistake, the price of which is not measurable.