How does a placenta work
About the placenta – role and complications
About the placenta – role and complications | Pregnancy Birth and Baby beginning of content7-minute read
Listen
What is the placenta?
The placenta is a temporary organ that develops during pregnancy. It attaches to the lining of your uterus and delivers oxygen and nutrients to your growing baby through the umbilical cord.
If something goes wrong with the placenta, it can be serious and even life-threatening to both mum and baby.
What is the role of the placenta during pregnancy?
The placenta passes oxygen, nutrients and antibodies from your blood to your baby. It also carries waste products from your baby back to your blood, so your body can get rid of them.
The placenta also produces some hormones like oestrogen and progesterone that are needed during pregnancy.
What is the normal position of the placenta during pregnancy?
The placenta should attach to the wall of the uterus, usually at the top, side, front or back. The exact location will vary from person to person and in each pregnancy.
The placenta can sometimes develop low in the uterus but will generally move higher as your uterus stretches. The position of the placenta will be checked at your 18-week ultrasound.
This image shows a normal placental location, with the placenta attached at the top of the uterus.How does the placenta work in twin pregnancies?
Fraternal twins come from separate eggs and each have their own placenta. Identical twins come from the same egg that separates, and they may share a placenta or have their own.
Can medicines cross the placenta?
Alcohol, nicotine, medicines and other drugs can cross the placenta and affect your baby’s health.
What should I do to keep my placenta healthy during pregnancy?
It’s important to visit your healthcare provider regularly during pregnancy.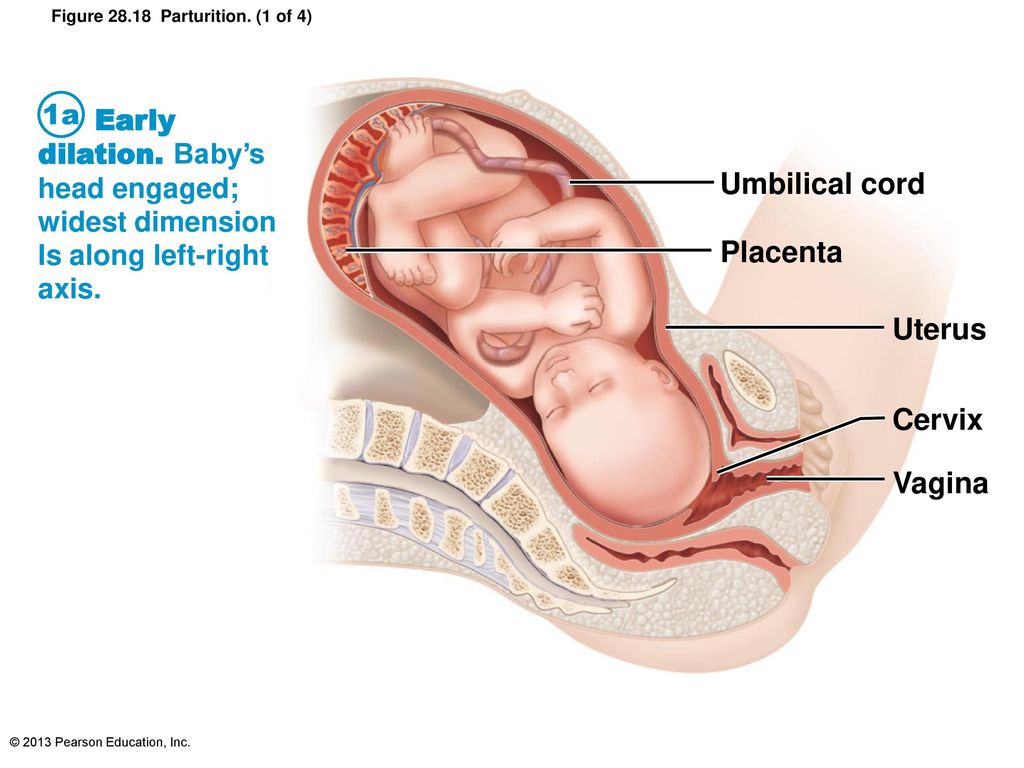 If there are complications, they can be identified during these appointments.
If there are complications, they can be identified during these appointments.
Tell your doctor if you have had problems with the placenta in a previous pregnancy, or if you have had any surgery to your uterus.
If you smoke, drink alcohol or take certain drugs during pregnancy, this increases the likelihood of problems with the placenta.
Always consult your doctor before you take any medicines, including over-the-counter medicines, natural therapies and supplements, while you are pregnant.
Speak with your doctor or midwife if you have any concerns, or if you experience:
- severe abdominal (stomach) pain or back pain
- vaginal bleeding
- contractions
- any trauma to your abdomen, for example from a fall or car accident
What happens to the placenta after my baby is born?
After your baby is born, you will need to birth your placenta. This is called the third stage of labour. This stage of labour can be managed in different ways.
This stage of labour can be managed in different ways.
If you had a vaginal birth, you will usually have some mild contractions and need to give a few pushes to help your placenta to come out.
If you have a caesarean section, your doctor will remove the placenta at the same time your baby is born.
Once you birth your placenta your doctor or midwife will check that it looks complete. If there is any concern that your placenta isn’t complete, they may suggest further investigations. If any bits of placenta are retained (stay inside you), they may have to be surgically removed to prevent infection.
Can I take my placenta home with me?
It is your choice what you do with your placenta. You may choose to discard it; in which case your hospital or birthing centre will take care of this.
If you wish to take your placenta home, you can speak to your doctor or midwife to arrange this.
In some cultures, people bury the placenta in a special place.
‘Placentophagy’ is a practice where people cook and eat their placenta.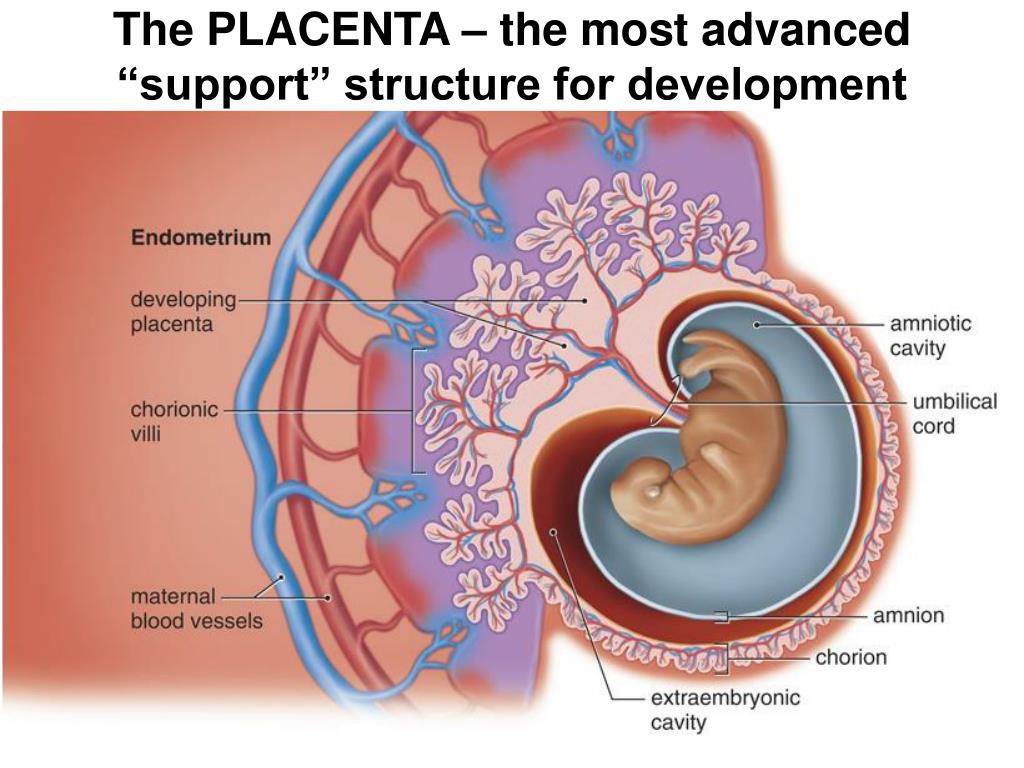 There is no research to support health benefits from this. However, you may choose to do this for cultural, spiritual, or personal reasons.
There is no research to support health benefits from this. However, you may choose to do this for cultural, spiritual, or personal reasons.
Some commercial service providers offer to turn your placenta into capsules for you to swallow. It should be noted that there may be a risk of infection from poor preparation. These practices should be treated with caution.
Can anything go wrong with my placenta?
Problems with your placenta can happen during pregnancy, birth and after birth. These are potentially dangerous for both you and your baby.
If your bleeding is severe and you have significant pain, call triple zero (000) for an ambulance or go to your nearest hospital emergency department.
If you have any vaginal bleeding during pregnancy, it’s important to see your doctor as soon as possible.
Placental abruption is when some or all the placenta comes away from the wall of the uterus before your baby is born.
Placenta praevia is when the placenta partially or totally covers the cervix (the narrow opening in the uterus).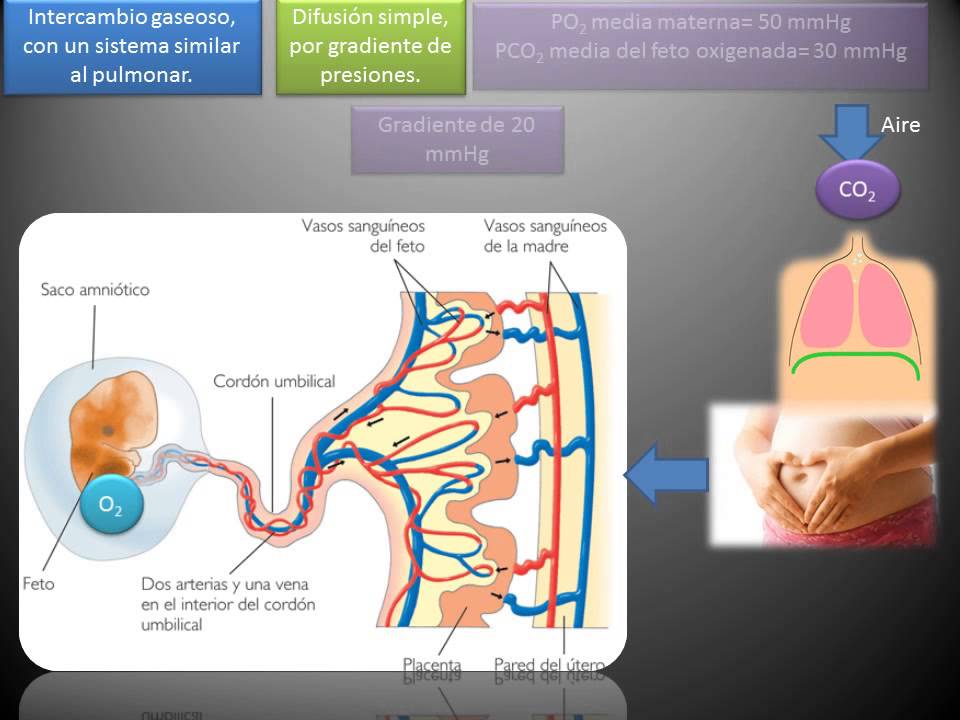
Placental insufficiency is when the placenta doesn’t work properly during pregnancy. It deprives the baby of oxygen and nutrients they need to grow and develop.
Placenta accreta is when the placenta grows too deeply into the wall of the uterus. This can lead to severe bleeding during or after delivery and can be life-threatening.
Retained placenta is when your placenta does not completely come out after the birth. This might be because it is stopped by your cervix or is still attached to your uterus.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
UNSW Embryology (KA02 Fetus or newborn affected by complications of placenta), Royal Women's Hospital (Placenta problems), RANZCOG (Intrauterine Growth Restriction: Screening, Diagnosis, and Management - Placenta accreta), The Royal Women’s Hospital Victoria Australia (Taking Your Placenta Home For Burial Or Consumption), International Journal of Women’s Health (Retained placenta after vaginal delivery: risk factors and management), NHS UK (What complications can affect the placenta?)Learn more here about the development and quality assurance of healthdirect content.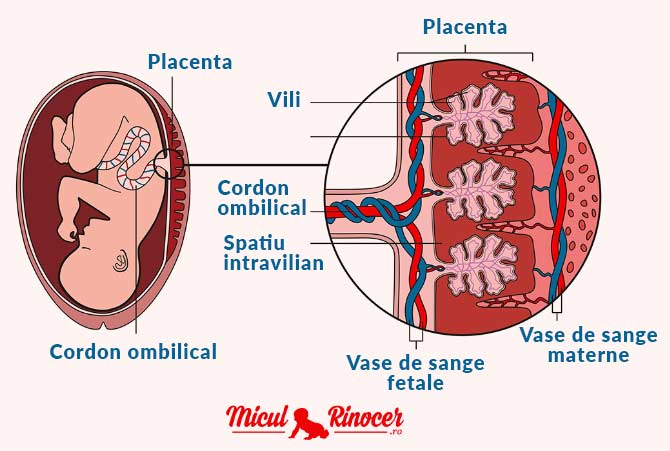
Last reviewed: July 2022
Back To Top
Related pages
- Mum's first 24 hours after birth
- Giving birth - stages of labour
- Placenta complications in pregnancy
Need more information?
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.
Read more on Better Health Channel website
Retained placenta
A retained placenta is when part or all of the placenta is not delivered after your baby is born. It can lead to serious infection or blood loss.
Read more on Pregnancy, Birth & Baby website
Placenta praevia
Placenta praevia is a condition where the placenta lies low and may cover the cervix, blocking the baby's exit during birth.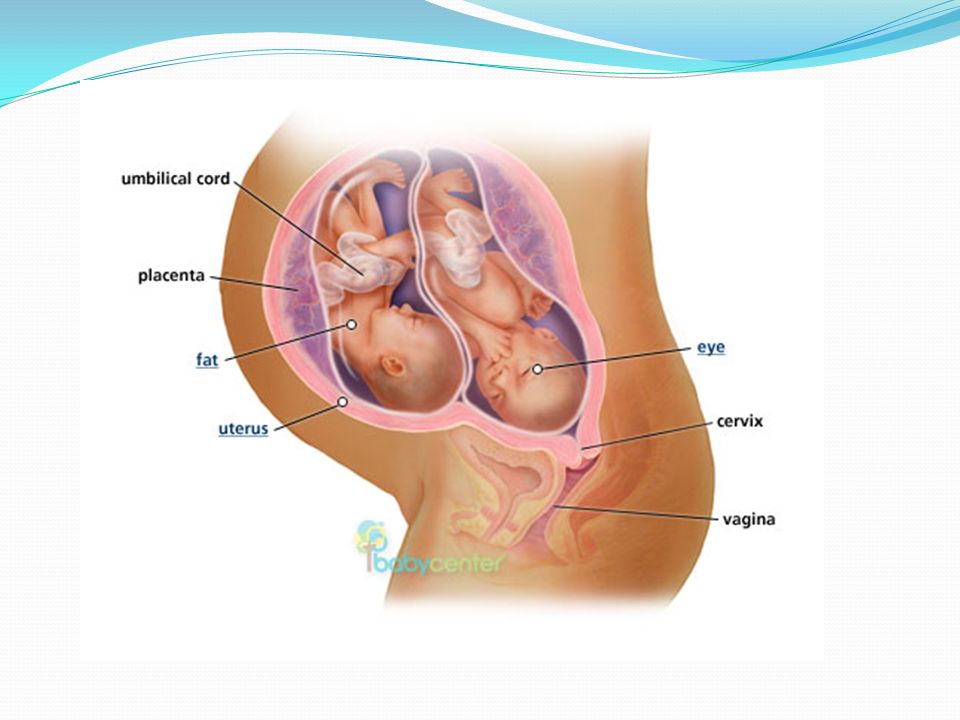
Read more on Pregnancy, Birth & Baby website
Placenta accreta
Placenta accreta is a serious but rare pregnancy complication that causes heavy bleeding. If you have it, you will need special care at the birth.
Read more on Pregnancy, Birth & Baby website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
It is not just a woman’s issue - Alcohol and Drug Foundation
If a woman drinks during pregnancy the alcohol crosses the placenta to the baby.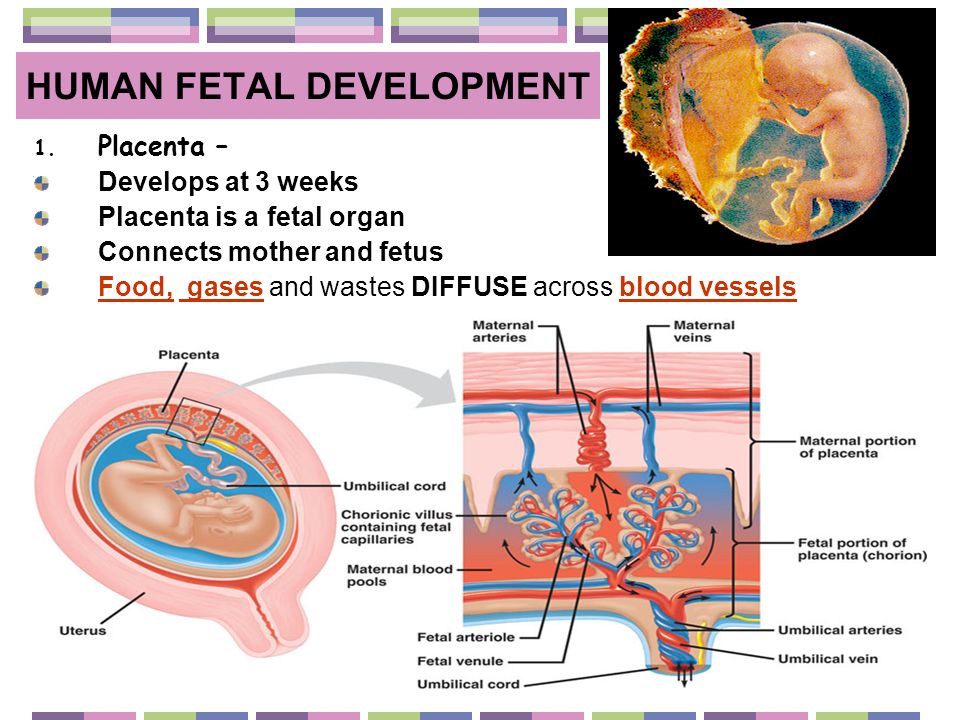 But what about the effect of alcohol on men?
But what about the effect of alcohol on men?
Read more on Alcohol and Drug Foundation website
Placental insufficiency
Find out about placental insufficiency - when the placenta does not work properly, and your baby doesn't get the oxygen and nutrients they need.
Read more on Pregnancy, Birth & Baby website
Placental abruption
Placental abruption is when some or all of the placenta peels away from the uterus wall before birth. It can deprive the baby of oxygen and nutrients.
Read more on Pregnancy, Birth & Baby website
Pregnancy test - Pathology Tests Explained
Starting approximately two weeks after conception, a hormone called human chorionic gonadatropin (hCG) hormone is produced by the developing placenta and can be detected in urine and in blood
Read more on Pathology Tests Explained website
4 weeks pregnant: Key points
When you are 4 weeks pregnant your body and your new baby are undergoing rapid changes.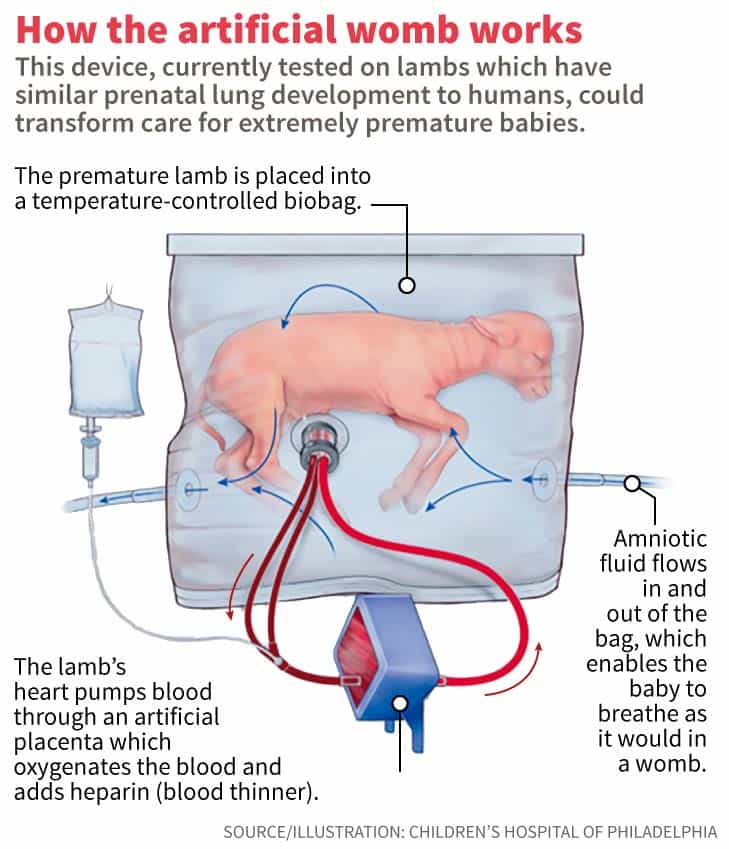 The placenta forms and begins producing a hormone called human chorionic gonadotrophin (hCG), which is the substance a pregnancy test detects to confirm you are pregnant. The cells which are growing into your new baby establish membranes which connect them to the placenta and prepare themselves for differentiation into different types of cells, which will occur next week when you are 5 weeks pregnant. These developments may cause you to experience unusual emotions and also cause changes in your body such as darkening of the areolas of your nipples.
The placenta forms and begins producing a hormone called human chorionic gonadotrophin (hCG), which is the substance a pregnancy test detects to confirm you are pregnant. The cells which are growing into your new baby establish membranes which connect them to the placenta and prepare themselves for differentiation into different types of cells, which will occur next week when you are 5 weeks pregnant. These developments may cause you to experience unusual emotions and also cause changes in your body such as darkening of the areolas of your nipples.
Read more on Parenthub website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.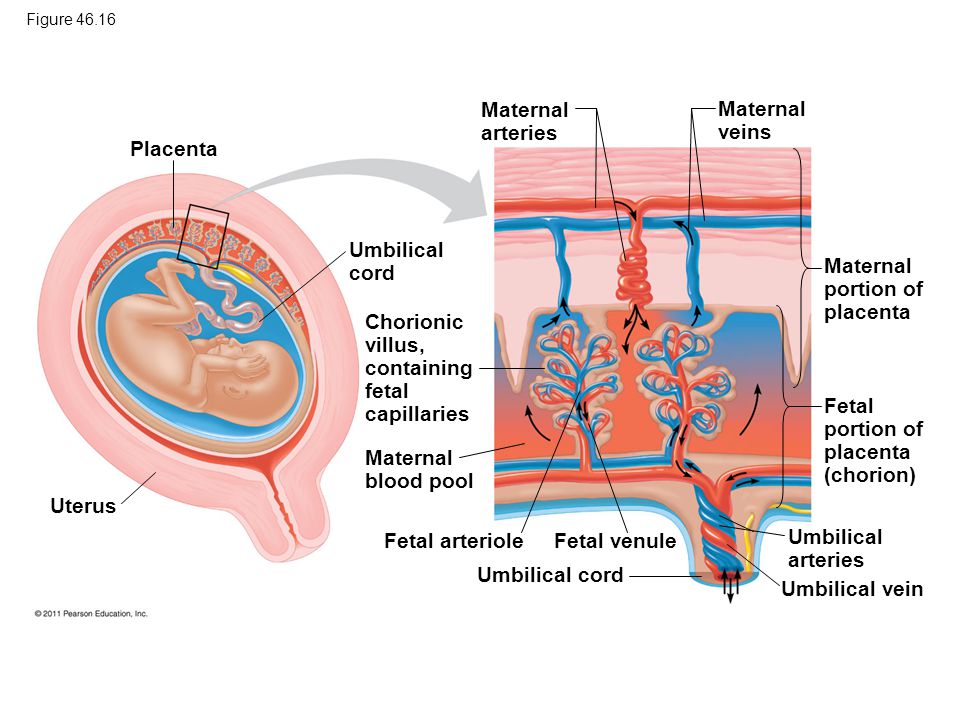
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Placenta - What Is It and How It Works
Placenta Definition
The placenta is an organ which is responsible for nourishing and protecting a fetus during pregnancy. It is unique in that it is a temporary organ; it grows alongside the fetus during pregnancy, and then is expelled along with the fetus at birth. The placenta is also sometimes called “afterbirth,” as it is expelled through the vagina after the fetus has been delivered.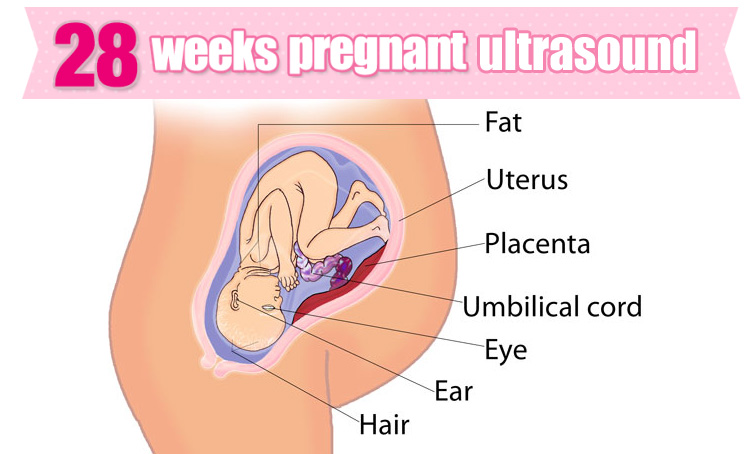
The placenta performs myriad functions to support fetal development, including facilitating blood flow, gas exchange, waste elimination, and serving as a protective barrier for the fetus against any infections the mother experiences during pregnancy.
The placenta is unique in that it is an organ which arises from the tissue of two genetically distinct organisms; part of the placenta develops from the tissue of the mother’s uterine wall, while another part develops from the fetus’ own tissue. After the blastocyst which will develop into the fetus makes contact with the uterine wall, blastocyst and maternal tissue grow together to form a single, cooperating organ that links the two together.
Mammals who give birth to live, fully-developed young, rather than laying eggs or carrying underdeveloped offspring in pouches, are often called “placental mammals.” The evolution of the placenta is one of the primary characteristics shared by all mammals except for marsupials and egg-laying mammals such as the platypus.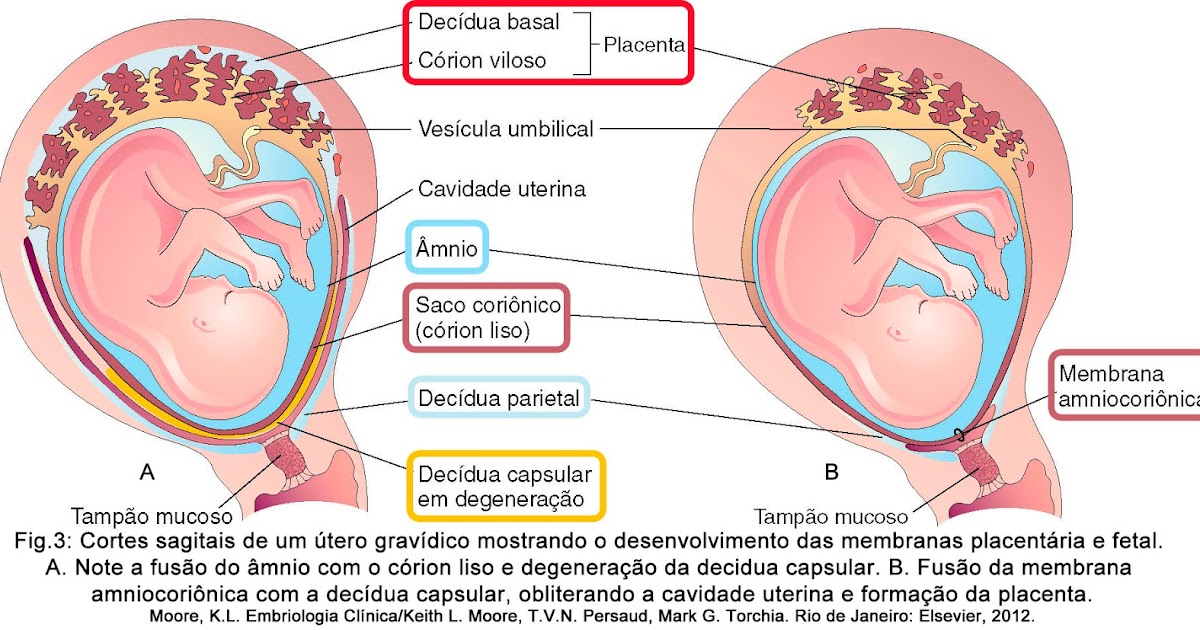
Some marsupials – close cousins to placental mammals like cats, dogs, and humans – have a primitive placenta in which blood vessels grow throughout the protective membranes surrounding the embryo. It is possible that placentas as we know them may have evolved from similar primitive structures in found the common ancestor of marsupials and placental mammals.
Pregnancies in which the placenta does not develop properly typically miscarry. This can occur either because of problems with the development of maternal uterine tissue, or because of problems with development of the fetal placental tissue. Fetuses which suffer from chromosomal problems may not be able to form a proper placenta and may miscarry, most often in the first trimester.
Many animals and some human cultures make a practice of eating the placenta after it is delivered. Scientists are divided on whether this is a good idea for humans. Some say it may contain valuable nutrients and even hormonal components that can be of assistance to the mother after pregnancy; others say that this practice may carry a risk of spreading infectious diseases, and that no benefits to eating the placenta have been proven in humans.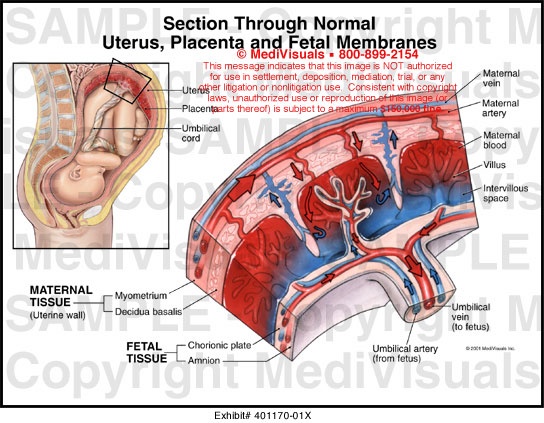
Function of Placenta
The placenta acts as a lifeline between the mother and fetus, ensuring that the fetus gets what it needs from the mother’s body to survive. At the same time, it acts as a protective barrier, shielding the fetus from some maternal infections. The functions of the placenta include:
- Allows gas exchange so the fetus gets enough oxygen
- Helps the fetus get sufficient nutrition
- Helps regulate the fetus’ body temperature
- Removes waste from the fetus for processing by the mother’s body
- Filters out some microbes that could cause infection
- Transfers antibodies from the mother to the fetus, conferring some immune protection
- Produces hormones that keep the mother’s body primed to support pregnancy
The placenta, then, essentially serves the function of several organ systems for the fetus, since the fetus is unable to eat, breathe, or eliminate waste itself while it is inside the womb!
Unfortunately, the placenta is not fool-proof as an infection barrier, and some fetuses do become infected with diseases contracted by their mother. Toxins of sufficiently small molecular size can also pass through.
Toxins of sufficiently small molecular size can also pass through.
That’s one reason why pregnant women are advised to avoid all possible sources of disease and toxins – diseases and toxins which may not be dangerous at all to adult women may be devastating to a developing fetus.
How Does the Placenta Work
When it is delivered, the placenta looks like a flat, round organ that is suffused with thick blood vessels. The fetus’ umbilical cord attaches to one flat surface, while the reverse surface grows out of the mother’s uterus during pregnancy.
The placenta works mainly by allowing substances to be exchanged between maternal and fetal blood. This allows the fetus to obtain nutrients, oxygen, antibodies, and other vital substances without having to share the mother’s blood supply directly.
This is vital because fetuses do not always have the same blood type as their mother, and direct mixing of the bloodstreams could cause the mother’s immune system to attack the fetal blood supply.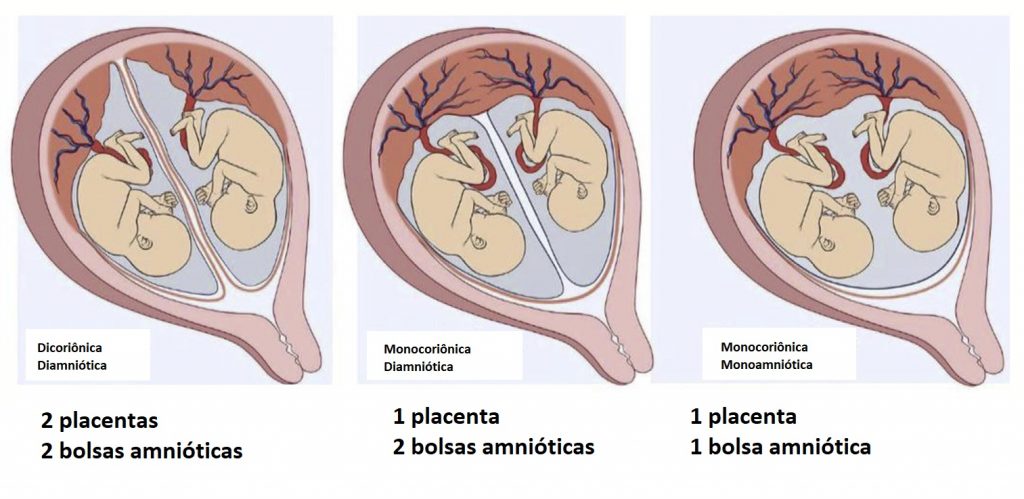 Even with the placenta separating the two, problems are occasionally caused by maternal antibodies attacking fetal blood supplies. Some women receive vaccines or other treatments to stop that form happening.
Even with the placenta separating the two, problems are occasionally caused by maternal antibodies attacking fetal blood supplies. Some women receive vaccines or other treatments to stop that form happening.
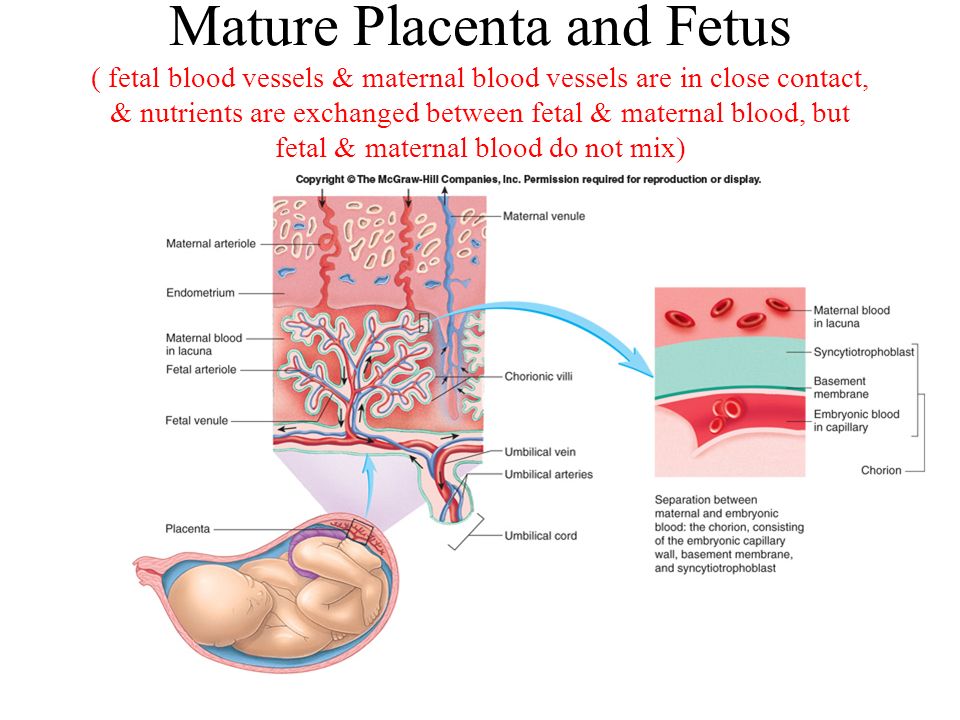
The diagram below shows how the fetal blood vessels infiltrate the placenta. It also shows how the mother’s arteries permeate the placenta. The placental tissue in between the two acts as a sort of filtration system, preventing most cells from passing through the barrier while allowing substances such as nutrients, antibodies, and gases to do so:
Eating the Placenta
In recent years, the topic of placenta-eating has been in the news a great deal. Many celebrities have contracted with companies that promise to turn their placentas into pills or food, and touted it as a move that has great health benefits. But many doctors have cautioned that there’s no evidence that placenta-eating confers real health benefits, and that eating your placenta may actually make your baby’s health worse.
In nature, animals often eat their placentas. There’s good reason for this: in nature food is often scarce, and the placenta is rich in protein, iron, and other nutrients that can be difficult to procure in the wild. That means that placenta-eating is often worth the risk for animal moms who just gave birth, and now need to provide nutritious milk for their young.
However, for humans, the risk of disease may outweigh any benefits of placenta-eating. Because the placenta serves as a filter to prevent harmful bacteria and viruses from reaching the baby, it can contain bacteria from infections the mother had during pregnancy.
Even if these pathogens aren’t harmful to the mother – some viruses and bacteria hardly bother adults – they can still be passed on to the newborn baby through breast milk, if the mother consumes an infected placenta. Cases have been recorded of babies becoming sick with bacterial infections which were later traced to their mother’s placenta supplements.
For that reason, many doctors counsel that the placenta is just like any other human tissue – it should not be eaten by humans, because doing so could spread disease.
Because the placenta does not qualify as a medication, health food and birthing companies that promise a “healthy experience” if you pay them to prepare your placenta are often not subject to the same regulations for safety and effectiveness as medications are.
In conclusion, just because some famous moms have done it doesn’t mean it’s a scientifically supported idea!
Quiz
1. Why are mammals such as dogs, cats, and humans called “placental mammals?”
A. Because the placenta is the evolutionary adaptation we all share, while monotremes, marsupials, and non-mammals do not.
B. Because all placental mammals have placentas, while only some non-mammals have placentas.
C. Both of the above.
Answer to Question #1
A is correct. Only placental mammals have fully developed placentas, while non-mammals and older mammal lineages such as monotremes and marsupials do not.
Only placental mammals have fully developed placentas, while non-mammals and older mammal lineages such as monotremes and marsupials do not.
2. Which of the following is true of the placental filtration system?
A. It is able to filter out all diseases and toxins, protecting the fetus.
B. It allows nutrients and oxygen to pass through, nourishing the fetus.
C. It is able to filter out some diseases and toxins, but not all of them.
D. Both B and C.
Answer to Question #2
D is correct. The placenta allows nutrients, oxygen, and other beneficial substances to pass from the mother to the fetus. It screens out some bacteria and toxins, but is unfortunately not able to screen out all of them. That’s why pregnant women are counseled to avoid potential sources of toxins and disease.
3. Which of the following is NOT true of placental anatomy?
A.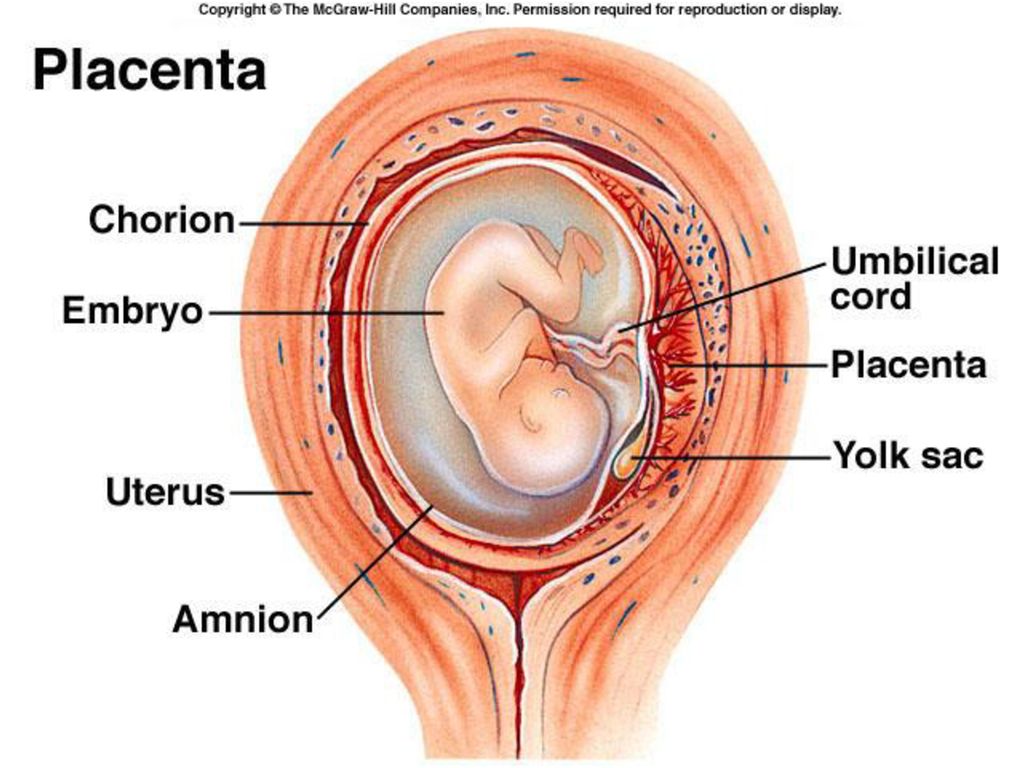 It contains many blood vessels from both the mother and fetus.
It contains many blood vessels from both the mother and fetus.
B. It is composed of both maternal and fetal tissue.
C. It allows the mother’s blood to flow into the fetus, nourishing it.
D. None of the above.
Answer to Question #3
C is correct. The placenta separates the maternal and fetal blood supplies, to prevent the mother’s immune system from attacking fetal blood cells. However, it does allow some substances such as nutrients, gases, and antibodies to be exchanged.
References
- Slater, D. (2017, April 03). The Myth Of The Placental Barrier. Retrieved July 08, 2017, from https://www.fitpregnancy.com/pregnancy/pregnancy-health/myth-placental-barrier
- 10.2 Development of the placental villi. (n.d.). Retrieved July 08, 2017, from http://www.embryology.ch/anglais/fplacenta/villosite01.html
- Should I Eat My Placenta? (n.d.). Retrieved July 08, 2017, from http://www.
webmd.com/baby/should-i-eat-my-placenta
Makarov I.O. • The placenta and its role in the development of pregnancy
HM70A ultrasound machine
Expert class at an affordable price. Single crystal sensors, full screen display, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a trolley.
From the very beginning of pregnancy and up to its end, the mother-placenta-fetus system is formed and functions . The most important component of this system is placenta , which is a complex organ, in the formation of which derivatives of trophoblast and embryoblast take part, as well as decidual tissue . The function of the placenta, first of all, is aimed at providing sufficient conditions for the physiological course of pregnancy and the normal development of the fetus. These functions include: respiratory, nutritional, excretory, protective, endocrine.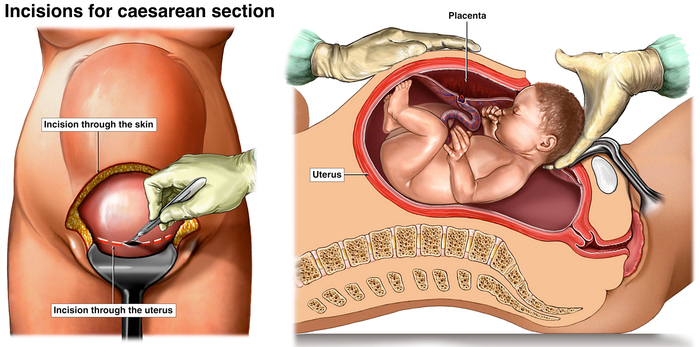 All metabolic, hormonal, immune processes during pregnancy are provided through maternal and fetal vascular system . Despite the fact that the blood of the mother and fetus does not mix, since their is separated by the placental barrier , the fetus receives all the necessary nutrients and oxygen from the mother's blood. The main structural component of the placenta is villous tree .
All metabolic, hormonal, immune processes during pregnancy are provided through maternal and fetal vascular system . Despite the fact that the blood of the mother and fetus does not mix, since their is separated by the placental barrier , the fetus receives all the necessary nutrients and oxygen from the mother's blood. The main structural component of the placenta is villous tree .
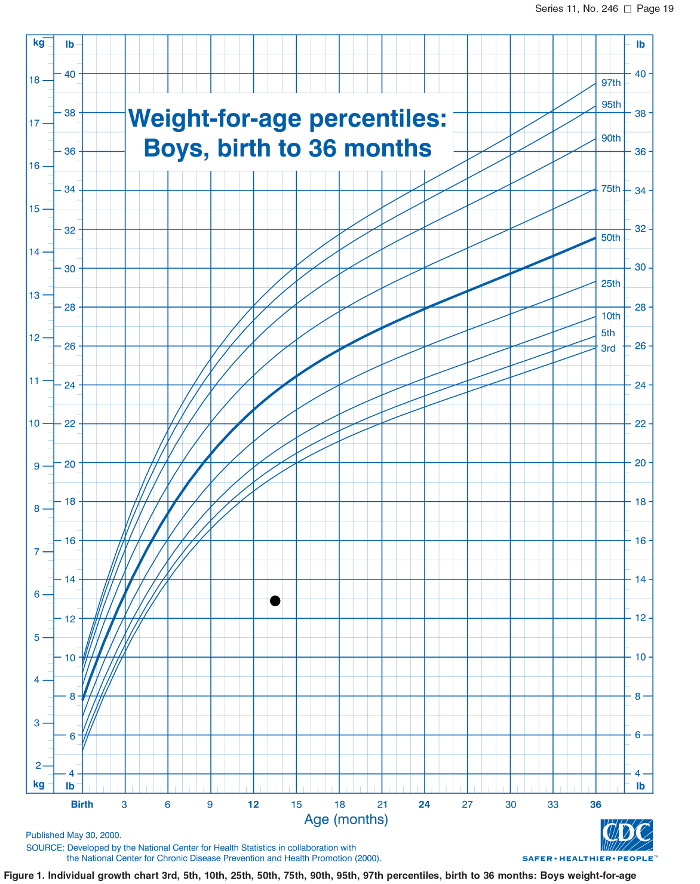
In the normal development of pregnancy, there is a relationship between the growth of the fetus, its body weight and the size, thickness, weight of the placenta. Up to 16 weeks of pregnancy, the development of the placenta outstrips the growth rate of the fetus. In case of death embryo (fetus) inhibition of growth and development of chorionic villi and progression of involution-dystrophic processes in the placenta. Having reached the required maturity at 38-40 weeks of pregnancy, the processes of formation of new vessels and villi in the placenta stop.
Diagram of the structure of the placenta and uteroplacental circulation
1 - umbilical cord arteries
2 - stem villi
3 - decidual septum
4 - decidua
5 - myometrium
6 - veins
7 - spiral arteries
8 - chorion
9 - amnion
10 - intervillous space
11 - vein of the umbilical cord
12 - cotyledon
The mature placenta is a disc-shaped structure 15-20 cm in diameter and 2.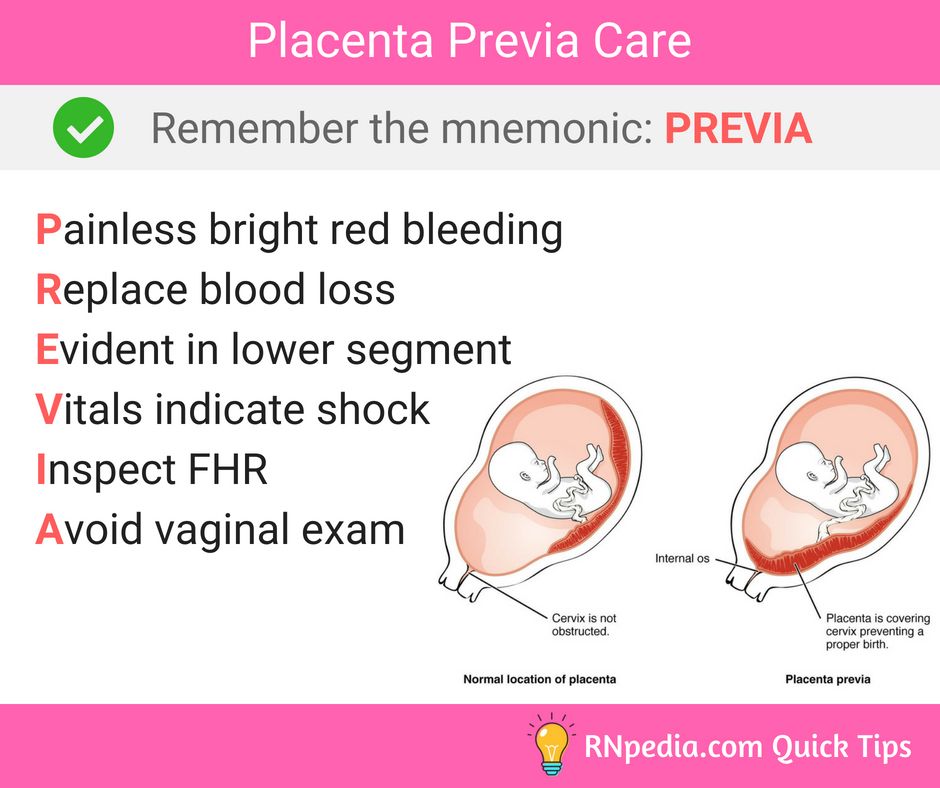 5-3.5 cm thick. Its mass reaches 500-600 g. The maternal surface of the placenta , which faces the uterine wall, has a rough surface formed by the structures of the basal part of the decidua. Fruit surface of placenta , which faces the fetus, is covered by amniotic membrane . Under it are visible vessels that go from the place of attachment of the umbilical cord to the edge of the placenta. The structure of the fruiting part of the placenta is represented by numerous chorionic villi , which are combined into structural formations - cotyledons. Each cotyledon is formed by a stem villus with branches containing fetal vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. In a mature placenta, there are 30 to 50 cotyledons. Cotyledon of the placenta is conditionally comparable to a tree, in which the supporting villi of the 1st order are its trunk, the villi of the 2nd and 3rd orders are large and small branches, the intermediate villi are small branches, and the terminal villi are leaves.
5-3.5 cm thick. Its mass reaches 500-600 g. The maternal surface of the placenta , which faces the uterine wall, has a rough surface formed by the structures of the basal part of the decidua. Fruit surface of placenta , which faces the fetus, is covered by amniotic membrane . Under it are visible vessels that go from the place of attachment of the umbilical cord to the edge of the placenta. The structure of the fruiting part of the placenta is represented by numerous chorionic villi , which are combined into structural formations - cotyledons. Each cotyledon is formed by a stem villus with branches containing fetal vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. In a mature placenta, there are 30 to 50 cotyledons. Cotyledon of the placenta is conditionally comparable to a tree, in which the supporting villi of the 1st order are its trunk, the villi of the 2nd and 3rd orders are large and small branches, the intermediate villi are small branches, and the terminal villi are leaves.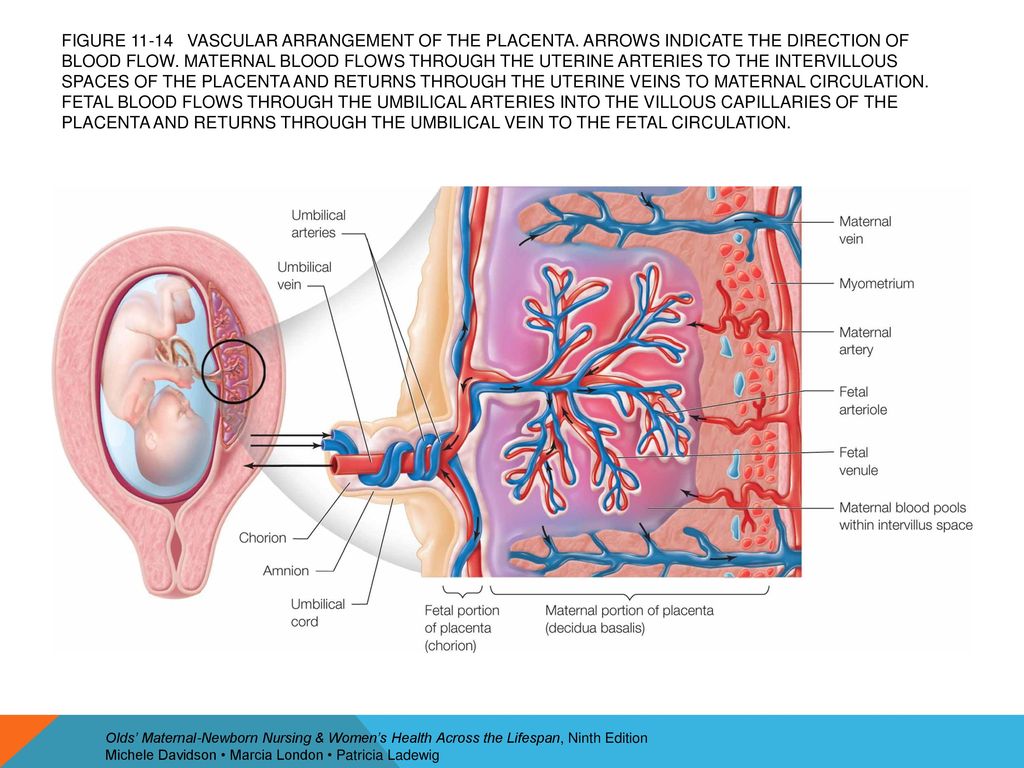 Cotyledons are separated from each other by partitions (septa) emanating from the basal plate. nine0007
Cotyledons are separated from each other by partitions (septa) emanating from the basal plate. nine0007
Intervillous space on the fetal side is formed by the chorionic plate and villi attached to it, and on the maternal side it is limited by the basal plate, decidua and septa extending from it. Most of the placental villi are freely immersed in the intervillous space and are bathed in maternal blood . There are also anchor villi, which are fixed to the basal decidua and provide attachment of the placenta to the wall of the uterus. nine0007
Diagram of blood circulation in the fetus
1 - superior vena cava
2 - oval hole
3 - inferior vena cava
4 - venous duct
5 - portal sinus
6 - portal vein
7 - vein of the umbilical cord
8 - umbilical cord arteries
9 - placenta
10 - epigastric arteries
11 - ductus arteriosus
Spiral arteries , which are the terminal branches of the uterine and ovarian arteries, feeding the pregnant uterus , open into the intervillous space with 120-150 orifices, providing a constant flow of maternal oxygen-rich blood into the intervillous space.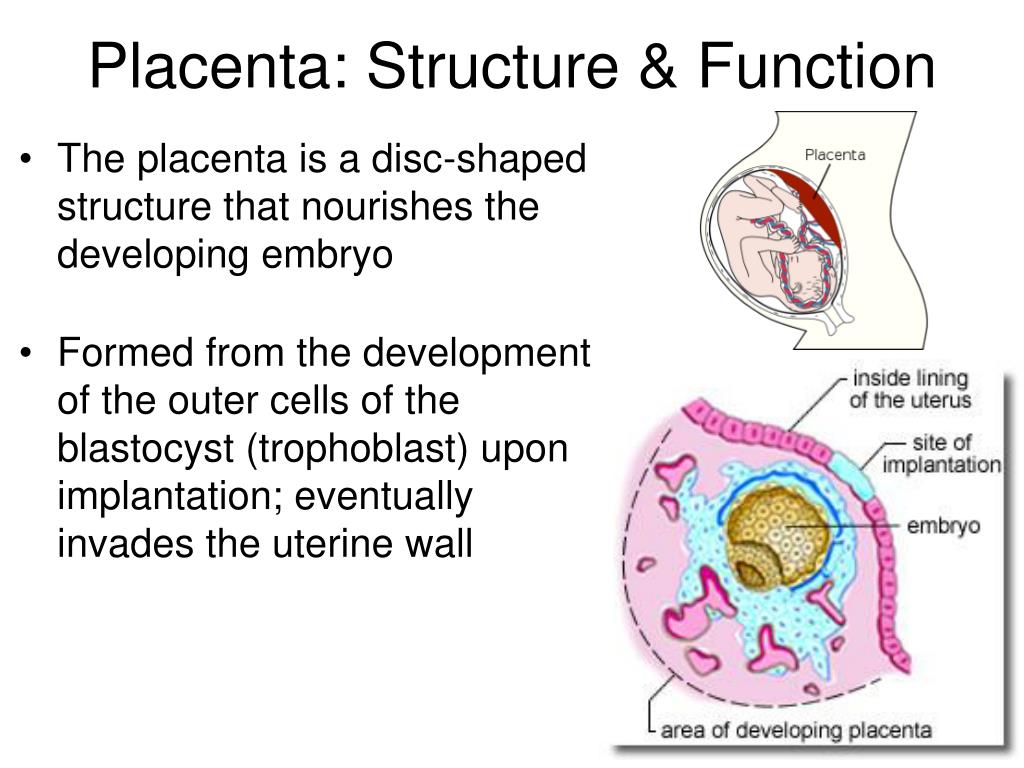 Due to pressure difference , which is higher in the maternal arterial bed compared to the intervillous space, blood saturated with oxygen from the mouths of the spiral arteries is sent through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the dividing septa maternal blood flow through venous orifices. In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix among themselves.
Due to pressure difference , which is higher in the maternal arterial bed compared to the intervillous space, blood saturated with oxygen from the mouths of the spiral arteries is sent through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the dividing septa maternal blood flow through venous orifices. In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix among themselves.
The transfer of blood gases, nutrients , metabolic products and other substances from maternal blood to fetal and back is carried out at the moment of contact of the villi with the mother's blood through the placental barrier . It is formed by the outer epithelial layer of the villus, the stroma of the villus, and the wall of the blood capillary located inside each villus. Fetal blood flows through this capillary. Saturated in this way with oxygen, the blood of the fetus from the capillaries of the villi is collected into larger vessels, which eventually combine into vein of the umbilical cord , through which oxygenated blood flows to the fetus . Having given up oxygen and nutrients in the body of the fetus, blood, depleted in oxygen and rich in carbon dioxide, flows from the fetus through two umbilical arteries to the placenta , where these vessels divide radially in accordance with the number of cotyledons. As a result of further branching of the vessels inside the cotyledons, the fetal blood again enters the capillaries of the villi and is again saturated with oxygen, and the cycle repeats. Due to the passage through the placental barrier of blood gases and nutrients, the respiratory, nutritional and excretory functions of the placenta are realized. At the same time, oxygen enters the bloodstream of the fetus and carbon dioxide and other metabolic products of the fetus are excreted .
Saturated in this way with oxygen, the blood of the fetus from the capillaries of the villi is collected into larger vessels, which eventually combine into vein of the umbilical cord , through which oxygenated blood flows to the fetus . Having given up oxygen and nutrients in the body of the fetus, blood, depleted in oxygen and rich in carbon dioxide, flows from the fetus through two umbilical arteries to the placenta , where these vessels divide radially in accordance with the number of cotyledons. As a result of further branching of the vessels inside the cotyledons, the fetal blood again enters the capillaries of the villi and is again saturated with oxygen, and the cycle repeats. Due to the passage through the placental barrier of blood gases and nutrients, the respiratory, nutritional and excretory functions of the placenta are realized. At the same time, oxygen enters the bloodstream of the fetus and carbon dioxide and other metabolic products of the fetus are excreted .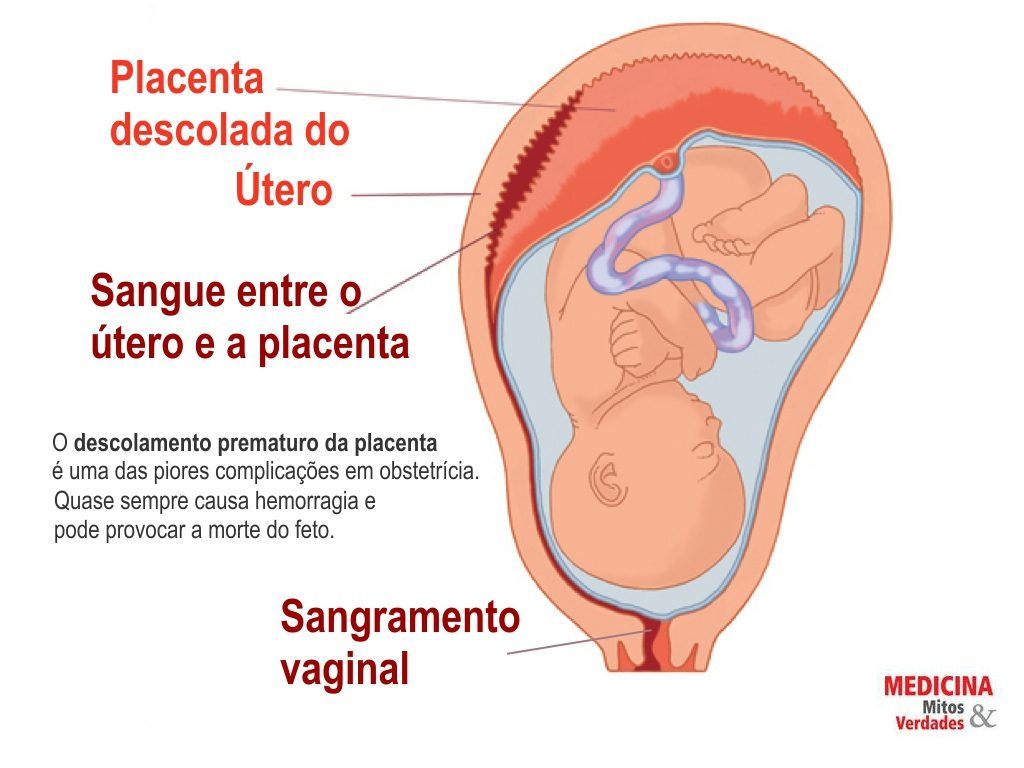 At the same time, proteins, lipids, carbohydrates, microelements, vitamins, enzymes and much more are transported towards the fetus.
At the same time, proteins, lipids, carbohydrates, microelements, vitamins, enzymes and much more are transported towards the fetus.
Scheme of the placental barrier
1 - capillary endothelium of terminal villi
2 - villus capillary
3 - villus stroma
4 - epithelial cover of villi nine0007
The placenta performs an important protective (barrier function) through the placental barrier, which is selectively permeable in both directions. In the normal course of pregnancy, the permeability of the placental barrier increases up to 32-34 weeks of pregnancy, after which it decreases in a certain way. However, unfortunately, a fairly large number of drugs, nicotine, alcohol, narcotic substances, pesticides, other toxic chemicals, as well as a number of pathogens of infectious diseases penetrate the placental barrier relatively easily into the fetal circulation, which has an adverse effect on the fetus.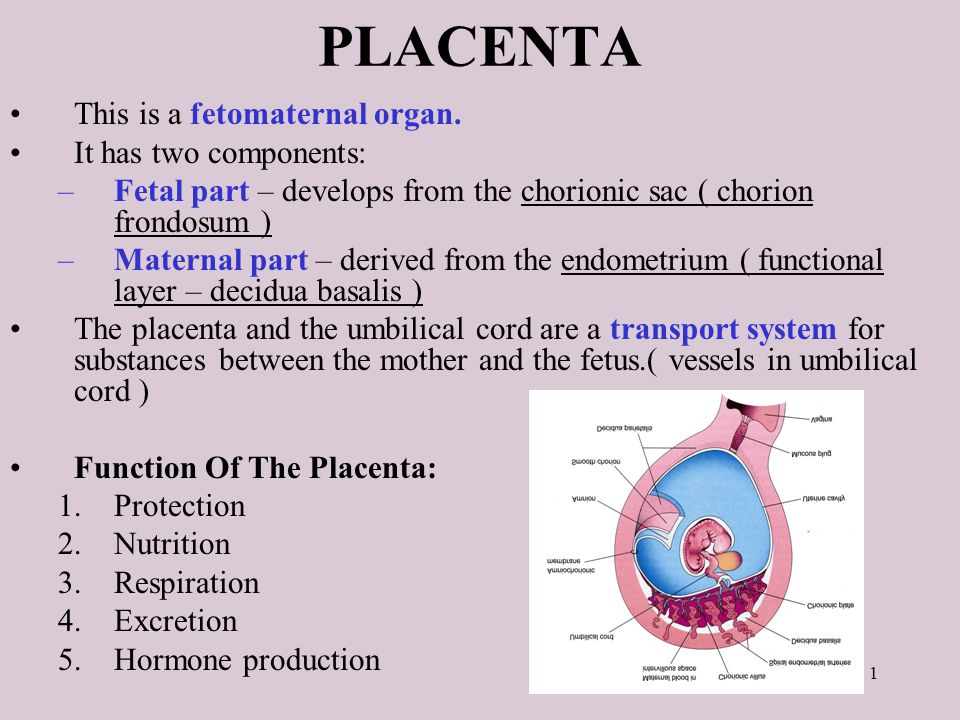 In addition, under the influence of pathogenic factors, the barrier function of the placenta is even more disturbed. nine0007
In addition, under the influence of pathogenic factors, the barrier function of the placenta is even more disturbed. nine0007
The placenta is anatomically and functionally related to the amnion (aqueous membrane) that surrounds the fetus. The amnion is a thin membrane that lines the surface of the placenta facing the fetus, passes to the umbilical cord and merges with the skin of the fetus at the umbilical ring. Amnion is actively involved in the exchange of amniotic fluid , in a number of metabolic processes, and also performs a protective function.
Connects placenta and fetus umbilical cord , which is a cord-like formation. The umbilical cord contains two arteries and one vein . Two arteries in the umbilical cord carry oxygen-depleted blood from the fetus to the placenta. The vein of the umbilical cord carries oxygenated blood to the fetus. The vessels of the umbilical cord are surrounded by a gelatinous substance, which was called "wharton jelly" .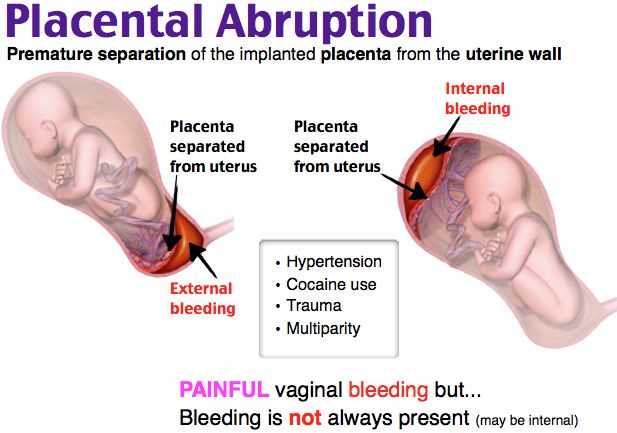 This substance provides the elasticity of the umbilical cord, protects the vessels and provides nutrition to the vascular wall. The umbilical cord may attach (most often) to the center of the placenta and less commonly to the side of the umbilical cord or to the membranes. The length of the umbilical cord in a full-term pregnancy is on average about 50 cm.
This substance provides the elasticity of the umbilical cord, protects the vessels and provides nutrition to the vascular wall. The umbilical cord may attach (most often) to the center of the placenta and less commonly to the side of the umbilical cord or to the membranes. The length of the umbilical cord in a full-term pregnancy is on average about 50 cm.
Placenta, membranes and umbilical cord together form placenta , which is expelled from the uterus after the birth of the child.
Ultrasound machine HM70A
Expert class at an affordable price. Single crystal sensors, full screen display, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a trolley.
Maternity hospital №7, Novosibirsk - What is the placenta? nine0001
Anna Valentinovna Yakimova, obstetrician-gynecologist, MD talks about the placenta and placental insufficiency.
Picture from the site http://s7ya7.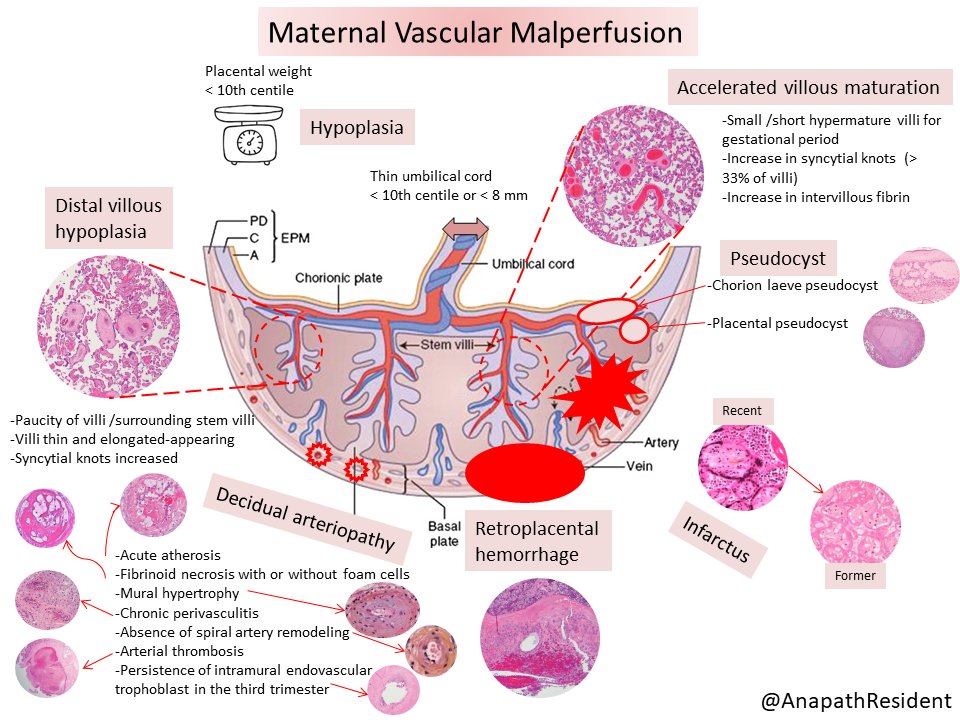 zdorovo-zivi.ru
zdorovo-zivi.ru
Placenta. The name of the organ comes from lat. placenta - cake, cake, pancake. This is an extra-embryonic organ, consisting of villi, thanks to which the fetus is nourished, respired, and waste products are removed from its blood. There are free and fixing (anchor) villi. The placenta is formed in the place where the embryo was implanted, arises as a result of the connection of the chorion - extraembryonic tissue with a thickened uterine mucosa (decidual tissue). Despite the fact that the blood of the mother and fetus does not mix, as they are separated by the placental barrier, the fetus receives all the necessary nutrients and oxygen from the mother's blood. In addition, the placenta produces hormones that ensure the preservation of pregnancy. The placenta has two surfaces. The surface that faces the fetus is called the fetal. It is covered with a smooth shell - the amnion, through which large vessels shine through. The one that is attached to the wall of the uterus is called maternal. nine0007
nine0007
The main structural unit of the placenta is cotelidone. Cotyledon of the placenta is conditionally comparable to a tree. Each cotyledon is formed by a stem villus, from which, like branches of a tree, villi of the second and third order extend, containing vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. Between the cotyledons there is a space - mejvirus, which on the maternal side is limited by partitions (septa) extending from the mucous membrane of the uterus. Most of the placental villi are freely immersed in the intervillous space (free villi) and are bathed in maternal blood. The spiral arteries, which are small branches of the arteries that supply the uterus, open into the intervillous space and supply oxygen-rich blood to the intervillous space. Due to the pressure difference, which is higher in the mother's arterial bed compared to the intervillous space, oxygenated blood from the mouths of the spiral arteries is directed through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the maternal circulation through the venous orifices through the separating septa.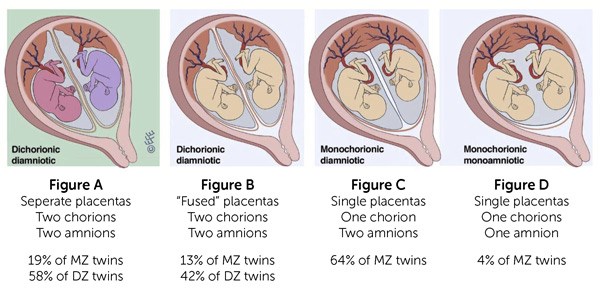 . In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix. Thus, the concept of the placental barrier appears: the blood of the mother of the fetus does not mix, because they are separated by the wall of the villus, loose connective tissue inside the villus and the wall of the vessel that is inside the villus, and in which the blood of the fetus circulates. nine0007
. In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix. Thus, the concept of the placental barrier appears: the blood of the mother of the fetus does not mix, because they are separated by the wall of the villus, loose connective tissue inside the villus and the wall of the vessel that is inside the villus, and in which the blood of the fetus circulates. nine0007
At the end of pregnancy, the placenta is a soft disk 15-18 cm in diameter, 2-4 cm thick in the central part, weighing about 500-600 g. their capillaries - 12 m2. The placenta, membranes, and umbilical cord together form the afterbirth, which is expelled from the uterus after the baby is born.
Normally, the placenta is attached to the uterine cavity on its anterior or posterior surface, sometimes in the fundus. If the placenta is attached in the lower part of the uterine cavity, close to the internal opening of the cervix - the internal pharynx, then its blood supply is often insufficient and the fetus may suffer from lack of oxygen and nutrients - a phenomenon called placental insufficiency occurs.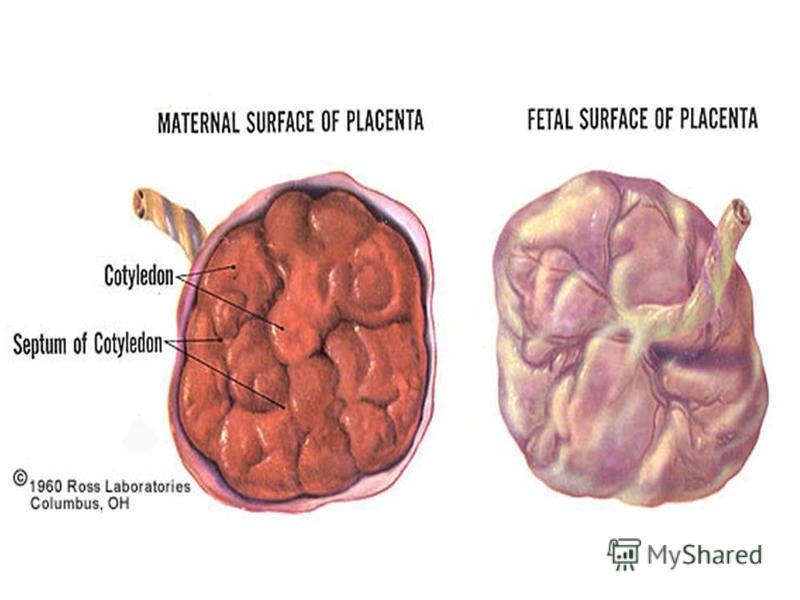 nine0007
nine0007
Placental insufficiency is a violation of all or some of the functions of the placenta, ultimately leading to oxygen starvation (hypoxia), fetal growth retardation or death and / or early termination of pregnancy.
Placental insufficiency may occur early in pregnancy due to abnormal formation of the placenta, for example, if the spiral arteries that supply the villi do not lose their ability to narrow their lumen in response to exposure to vasoconstrictor substances. It is possible that there is a violation of the development of blood vessels inside the villi, the vessels can form in the central part of the villus, and not close to its wall, then the transfer of nutrients from the mother's blood to the fetal blood and the flow of metabolic products back will be difficult. The process of development of the placenta (in particular, vascular formation) occurs to a greater extent in the first and second trimesters of pregnancy, ending at about 30-32 weeks. After this period, involutive processes predominate ("aging", immuring the villi with fibrinoid). Along with the processes of involution in the placenta during pregnancy, young villi develop, more often avascular, which, however, only partially compensate for the function of mature villi containing vessels that have “fallen out” of the circulation. nine0007
Along with the processes of involution in the placenta during pregnancy, young villi develop, more often avascular, which, however, only partially compensate for the function of mature villi containing vessels that have “fallen out” of the circulation. nine0007
In another scenario, placental insufficiency occurs at a later date, as a result of damage to the placenta in inflammatory processes, diabetes in a pregnant woman, or high blood pressure, when blood flow to the uterus is disturbed, which can also occur with increased maternal blood clotting . It is believed that it is the violation of the uteroplacental circulation that plays the main role in the formation of the intrauterine growth retardation syndrome. Before the advent of Doppler ultrasound research methods in obstetric practice, there were no non-invasive methods for studying blood flow in the mother-placenta-fetus system. To date, Doppler is the most preferred instrumental method that provides useful information in relation to the detection of blood flow disorders and the determination of pregnancy management tactics for placental insufficiency. If there are symptoms of placental insufficiency - a mismatch in the height of the uterine fundus, signs of a threat of early termination of pregnancy, rapid or slow fetal heart rate (normal: 120-160 beats per minute), an altered amount of amniotic fluid - it is necessary to conduct an ultrasound examination, Doppler blood flow in the vessels of the uterus, umbilical cord and fetus, and in the third trimester - cardiotocography. The earliest sign of placental dysfunction is a decrease in its production of hormones and proteins, therefore, in pregnant women with a known risk of placental dysfunction (for example, if she has a chronic inflammatory process or often / constantly increased blood pressure, etc.), you can examine the level placental lactogen, progesterone, unconjugated estriol in the blood. And on the basis of the data obtained, predict the further development of pregnancy and take preventive measures. nine0007
If there are symptoms of placental insufficiency - a mismatch in the height of the uterine fundus, signs of a threat of early termination of pregnancy, rapid or slow fetal heart rate (normal: 120-160 beats per minute), an altered amount of amniotic fluid - it is necessary to conduct an ultrasound examination, Doppler blood flow in the vessels of the uterus, umbilical cord and fetus, and in the third trimester - cardiotocography. The earliest sign of placental dysfunction is a decrease in its production of hormones and proteins, therefore, in pregnant women with a known risk of placental dysfunction (for example, if she has a chronic inflammatory process or often / constantly increased blood pressure, etc.), you can examine the level placental lactogen, progesterone, unconjugated estriol in the blood. And on the basis of the data obtained, predict the further development of pregnancy and take preventive measures. nine0007
Can placental insufficiency be treated? The answer to this question is ambiguous.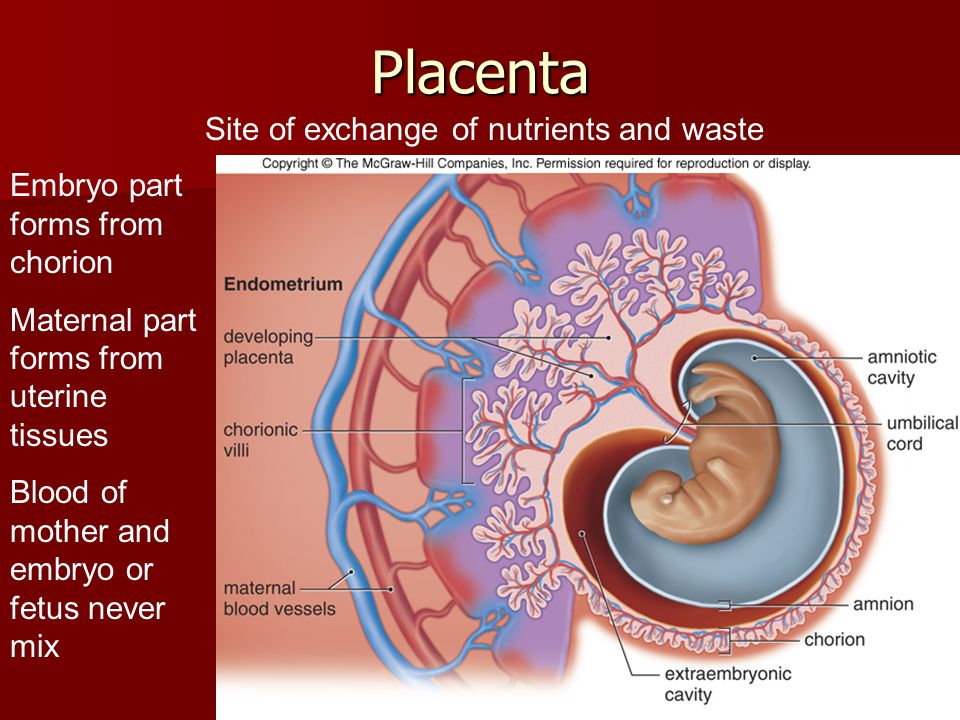 It is possible to influence the development of the placenta when it is incomplete, improving the conditions for development - by eliminating, for example, the inflammatory process, normalizing blood pressure, lowering the tone of the uterus, and normalizing blood clotting. You can influence the metabolism in the cells of the placenta - by doing this, for example, by introducing drugs into the body of a pregnant woman that help improve the utilization of glucose by cells. It is possible to influence the tone of the vessels, reduce the permeability of the wall and, in this way, the swelling of the tissues decreases and the penetration of oxygen into them improves. But we must understand that we do not cure placental insufficiency, we are only trying to influence the compensatory mechanisms that exist in the placenta, if this succeeds, the manifestations of placental insufficiency disappear. But more often, treatment is aimed at prolonging the pregnancy to the term of a viable fetus. nine0007
It is possible to influence the development of the placenta when it is incomplete, improving the conditions for development - by eliminating, for example, the inflammatory process, normalizing blood pressure, lowering the tone of the uterus, and normalizing blood clotting. You can influence the metabolism in the cells of the placenta - by doing this, for example, by introducing drugs into the body of a pregnant woman that help improve the utilization of glucose by cells. It is possible to influence the tone of the vessels, reduce the permeability of the wall and, in this way, the swelling of the tissues decreases and the penetration of oxygen into them improves. But we must understand that we do not cure placental insufficiency, we are only trying to influence the compensatory mechanisms that exist in the placenta, if this succeeds, the manifestations of placental insufficiency disappear. But more often, treatment is aimed at prolonging the pregnancy to the term of a viable fetus. nine0007
But if the signs of placental insufficiency increase, and the gestation period is more than 32 weeks, when even in a normal placenta it undergoes involution, the placenta initially developed incorrectly, and now it performs its functions worse, the fetus suffers, then it is useless to treat placental insufficiency, it is better to carry out early delivery and to nurse the newborn without the risk of intrauterine death, which is possible if the placenta depletes its reserves.