Breastfeeding and hep c
Hepatitis B or C Infections | Breastfeeding
Mothers with Hepatitis B or C infections can breastfeed their infants.
Hepatitis B
Hepatitis B is a liver infection caused by the hepatitis B virus (HBV), which is transmitted by blood, semen or other body fluid from an infected person. A woman with hepatitis B can infect her infant with the virus during childbirth. All pregnant women pdf icon[PDF-864KB] are given a blood test for hepatitis B as part of their prenatal care or when they arrive at the hospital to give birth. CDC recommends that babies get the first dose of the hepatitis B vaccine before leaving the hospital or within the first 24 hours. Babies are usually given the second dose of the vaccine 1-2 months after the first dose, and the third dose by the time they are 18 months old.
Is it safe for a mother infected with hepatitis B virus (HBV) to breastfeed her infant?
Yes. All infants born to HBV-infected mothers should receive hepatitis B immune globulin (HBIG) and the first dose of hepatitis B vaccine within 12 hours of birth. The second dose of vaccine should be given at age 1–2 months, and the third dose at age 6 months. The infant should be tested after completion of the vaccine series, at age 9–12 months (generally at the next well-child visit), to determine if the vaccine worked and that the infant is not infected with HBV through exposure to the mother’s blood during the birth process. However, there is no need to delay breastfeeding until the infant is fully immunized. The risk of HBV mother-to-child transmission through breastfeeding is negligible if infants born to HBV-positive mothers receive the HBIG/HBV vaccine at birth.
Learn more about HBV infection.
Is it safe for the HBV-positive mother to breastfeed if her nipples are cracked and bleeding?
Data are insufficient to say yes or no. However, HBV is spread by infected blood. Therefore, if the HBV-positive mother’s nipples and/or surrounding areola are cracked and bleeding, she should stop nursing temporarily. To maintain her milk supply while not breastfeeding, she can express and discard her breast milk until her nipples are healed. Once her nipples are no longer cracked or bleeding, the HBV-positive mother may fully resume breastfeeding. Providers may need to refer mothers for lactation support to learn how to maintain milk production and how to supplement with pasteurized donor human milk or formula while temporarily not breastfeeding.
Once her nipples are no longer cracked or bleeding, the HBV-positive mother may fully resume breastfeeding. Providers may need to refer mothers for lactation support to learn how to maintain milk production and how to supplement with pasteurized donor human milk or formula while temporarily not breastfeeding.
Top of Page
Hepatitis C
Hepatitis C is a liver infection caused by the hepatitis C virus (HCV), which is transmitted by blood from an infected person. There is no vaccine for hepatitis C. The best way to prevent hepatitis C is by avoiding behaviors that can spread the disease, especially injecting drugs.
Is it safe for a mother infected with hepatitis C virus (HCV) to breastfeed her infant?
Yes. There is no documented evidence that breastfeeding spreads HCV. Therefore, having HCV-infection is not a contraindication to breastfeed.
Is it safe for the HCV-positive mother to breastfeed if her nipples are cracked and bleeding?
Data are insufficient to say yes or no. However, HCV is spread by infected blood. Therefore, if the HCV-positive mother’s nipples and/or surrounding areola are cracked and bleeding, she should stop nursing temporarily. To maintain her milk supply while not breastfeeding, she can express and discard her breast milk until her nipples are healed. Once her nipples are no longer cracked or bleeding, the HCV-positive mother may fully resume breastfeeding. Providers may need to refer mothers for lactation support to learn how to maintain milk production and how to supplement with donor human milk or formula while temporarily not breastfeeding.
However, HCV is spread by infected blood. Therefore, if the HCV-positive mother’s nipples and/or surrounding areola are cracked and bleeding, she should stop nursing temporarily. To maintain her milk supply while not breastfeeding, she can express and discard her breast milk until her nipples are healed. Once her nipples are no longer cracked or bleeding, the HCV-positive mother may fully resume breastfeeding. Providers may need to refer mothers for lactation support to learn how to maintain milk production and how to supplement with donor human milk or formula while temporarily not breastfeeding.
Visit CDC’s Viral Hepatitis C Frequently Asked Questions for additional information on HCV infection and pregnancy.
Breastfeeding and Hepatitis C: Is It Safe?
Written by Sharita Hanley
In this Article
- Is Breastfeeding Safe?
- What If I Have Cracked or Bleeding Nipples?
- Do I Need to Test My Child for Hep C?
- How to Keep Your Baby Safe
New moms want to do all they can to protect their baby’s health. When you have hepatitis C, you may feel uncertain about the best ways to care for your newborn. Especially when it comes to a key decision: should you breastfeed your baby?
When you have hepatitis C, you may feel uncertain about the best ways to care for your newborn. Especially when it comes to a key decision: should you breastfeed your baby?
Is Breastfeeding Safe?
Yes, you can nurse your baby without worrying. HCV, the virus that causes hepatitis C, does not spread through breast milk. Studies also show that breastfed infants do not have higher rates of hepatitis C than formula-fed babies.
The virus spreads to others when blood from an infected person gets into the blood of someone who’s not infected. Babies can get the virus from their mothers during birth -- about 6 out of 100 infants born to moms with hepatitis C get infected. But research shows that breastfeeding doesn’t cause infections.
Other ways hepatitis C spreads include:
- Sharing needles or syringes
- Needlestick injuries, which can take place in health care settings
- Getting a tattoo or body piercing if tools are not cleaned properly
- Sexual contact with an infected person
- Sharing personal items that may have someone’s blood on it, like a razor or toothbrush
What If I Have Cracked or Bleeding Nipples?
It’s a common issue for nursing mothers. Research doesn’t directly say if it’s OK to continue breastfeeding or not. But experts say the safest bet is to stop until your nipples heal. To help prevent your milk from drying up, pump it and throw it away.
Research doesn’t directly say if it’s OK to continue breastfeeding or not. But experts say the safest bet is to stop until your nipples heal. To help prevent your milk from drying up, pump it and throw it away.
It’s also best to take a break from breastfeeding if:
- You have an infection like mastitis, or inflamed breast tissue
- Your breast is bruised or injured
- You notice cuts in your baby’s mouth
Feel free to start nursing again once you are symptom free.
Do I Need to Test My Child for Hep C?
If you have hepatitis C, your baby’s doctor will probably recommend testing for the virus when they are 18 months old.
There are a few tests they may use:
- Anti-HCV. This is the first test your child will get. It looks for antibodies to HCV, which tells you whether your child has been exposed to the virus. If the results are negative, your child does not have hep C. If they are positive, your baby will need more testing to see if they are currently infected.

- HCV-RNA. Your child will get this test if the anti-HCV results were positive. It looks for the virus in your child’s blood. Positive results mean your child has an active hepatitis C infection.
- Viral load test, which checks to see how much of the virus is in your child’s blood. If they’ve tested positive for HCV, doctors will use this test to see if treatment is working.
How to Keep Your Baby Safe
If your child has hepatitis C, there’s a 25% chance the virus clears up on its own. If it doesn’t, there are a few things you can do to protect their health. They should see their doctor often, have regular blood tests, and take any medicine the doctor prescribes. With the right treatment, hep C is curable. So work with your child’s doctor early on to fight the infection and help your little one avoid other health problems hep C can cause.
You can keep your baby safe by monitoring your health, too. Avoid alcohol and take the antiviral drugs your doctor prescribes. If you’re pregnant but not sure if you have hepatitis C, ask your doctor for an HCV test.
If you’re pregnant but not sure if you have hepatitis C, ask your doctor for an HCV test.
Hepatitis B and C - can I breastfeed?
Unfortunately, in our time, nursing mothers often worry about the question - is it possible to breastfeed their baby if they are carriers of hepatitis B or C viruses? Will the baby get infected through breast milk?
Only the attending physician can unambiguously answer this question, considering each specific individual case, and in our publication we will try to consider the most modern and reasonable points of view on this issue, making a small review of foreign and domestic literature.
First, let's consider the case when the mother is sick with hepatitis B . Hepatitis B virus (HBV) causes a systemic disease that affects the liver. The patient may not feel any symptoms at all, or may experience symptoms resembling a mild flu, but the disease can also develop and transient. The hepatitis B virus can be transmitted through contact with infected blood or other bodily fluids. Contact with infected mucous membranes during childbirth or during sexual contact is also a way of transmitting the virus.
Contact with infected mucous membranes during childbirth or during sexual contact is also a way of transmitting the virus.
Breast milk may contain hepatitis B surface antigen (HBsAg), and it has been suggested that breastfeeding is a route of possible entry of hepatitis B virus into infants.
However, there is no evidence that breastfeeding increases the risk of transmission to the baby. [5,12]
Approximately 5 to 15 percent of pregnant women infected with the hepatitis B virus will pass the virus on to their babies before birth. But since the main contact of the baby with the virus occurs during or immediately before childbirth, immunoprophylaxis and vaccination in the early postpartum period have a high chance of preventing infection. This is why the hepatitis B vaccine is recommended for all newborns as part of the regular childhood vaccination schedule. [3]
Hepatitis B vaccine significantly reduces perinatal transmission and can completely eliminate the risk that a mother can infect her baby through breastfeeding. [5,12]
[5,12]
Infants born to mothers infected with hepatitis B who have already been exposed to maternal blood, amniotic fluid, and vaginal secretions at the time of birth may be breastfed. The newborn should receive immunoglobulin for hepatitis B serotherapy (HBIG) within 12 hours of birth, followed by three injections of hepatitis B vaccine: during the first week of life, at 1 month, and at 6 months.
All infants should be under pediatric supervision - including retesting for HBsAg to rule out chronic carriage. This protocol is successful in reducing the risk related to neonatal transmission of the virus during breastfeeding. In a group of 369 infants born to women with chronic hepatitis B, none of the breastfed infants were infected with the hepatitis B virus, but nine formula-fed infants were infected with it. [9]
Thus, breastfeeding does not increase infection rates among infants. Moreover, in areas with a high prevalence of the hepatitis B virus, not breastfeeding puts the baby at greater risk of the disease.
And even when hepatitis C virus was detected in breast milk, breastfed babies were not infected, and mothers with a positive test for hepatitis C virus RNA, according to the World Health Organization, should be advised to breastfeed. [11,12,15]
Hepatitis C virus (HCV), which is associated with later development of chronic liver disease, is now mainly acquired vertically in childhood. Perinatal transmission from mother to child is approximately 6 percent. The risk of transmission is associated with the presence of maternal HCV at birth and high maternal viral load [16].
Despite the presence of hepatitis C virus RNA in some breast milk samples, there is no evidence that breastfeeding confers a risk of hepatitis C infection [8,16] and there are no known cases of transmission of the virus from mother to infant through breast milk. [17] The overall proportion of maternal-infant transmission of hepatitis C among breastfed infants is the same as among formula-fed infants; and infected women should be allowed to breastfeed. [6,7,10]
An exception is a rare case of mothers in the acute period of hepatitis C acquired after childbirth, at a time when neutralizing antibodies are not yet present in her blood. [13]
It has been suggested that sore and cracked nipples during breastfeeding may be a risk of transmission of hepatitis C virus [4,14] but this theory is hypothetical and has not been well substantiated. A disturbing implication of this recommendation is that it implies a ban on breastfeeding if the mother has hepatitis C, while so many women have temporary nipple injury after childbirth. [3]
The National Strategy for Infant Feeding in the Russian Federation, published in 2008, also states that “Currently, the presence of hepatitis B and C in women is not a contraindication to breastfeeding, but feeding is carried out through special silicone pads.” [1]
And, in conclusion, we can consider the table of contraindications to breastfeeding, presented in the textbook on neonatology, Doctor of Medical Sciences, Professor, President of the Union of Pediatricians of St. Petersburg, Nikolai Pavlovich Shabalov:
Contraindications to breastfeeding (WHO training workshop Basic Newborn Care and Breastfeeding, 2002) [2]
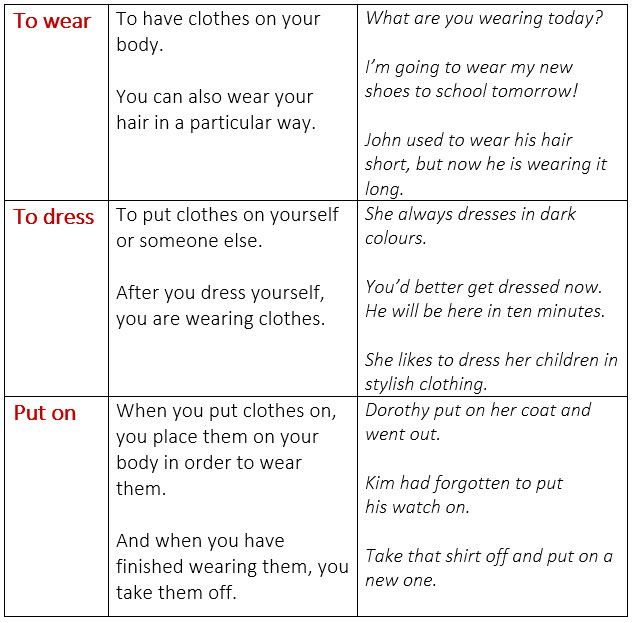
| Status | Breastfeeding(1) contraindicated | Breast milk (2) contraindicated | ||||||||||
| NO | YES | "?" | NO | YES | "?" | |||||||
| Temporary | Permanent | Temporarily | Permanent | |||||||||
| partially | fully | partially | fully | partially | fully | partially | fully | |||||
| Galactosemia (child) | x | x | ||||||||||
| Leucinosis ketonuria, maple syrup disease (child) | x(a) | x(a) | ||||||||||
| Phenylketonuria (child) | x(a) | x(a) | ||||||||||
| Herpetic stomatitis (child) | x | x | ||||||||||
| HIV/AIDS (child) | b | b | ||||||||||
| Maternal common non-severe infections | x | x | ||||||||||
| Chicken pox (maternal) | x(d) | x | ||||||||||
| Cytamegalovirus (maternal) | x | x | ||||||||||
| Gonorrhea (mother) | x(e) | x | ||||||||||
| Hepatitis A (maternal) | x | x | ||||||||||
| Hepatitis B (mother) | x(c) | x(c) | ||||||||||
| Herpes simplex (breast affection) | b | x | ||||||||||
| HIV/AIDS (mother) | b | b | ||||||||||
| Leprosy (mother) | x | x | ||||||||||
| Staphylococcus (mother) | x | x | ||||||||||
| Streptococcus (mother) | x(e) | x | ||||||||||
| Syphilis (mother) | x(e) | x | ||||||||||
| Taxoplasmosis (maternal) | x | x | ||||||||||
| Tuberculosis (maternal) | b | b | ||||||||||
| Mastitis (mother) | x | x | ||||||||||
| Breast abscess (mother) | g | b | ||||||||||
| Breast cancer | x(h) | x | ||||||||||
| Endometritis (maternal) | x | x | ||||||||||
| Urinary tract infections (maternal) | x | x | ||||||||||
"?" - conflicting opinions. (1) These tables apply only to biological mothers who are breastfeeding or expressing milk for their child. (2) Milk should be expressed regularly during the period of suspension of breastfeeding. (a) Monitor the level of the toxic metabolite in the child's blood. (b) Conflicting opinions, decisions are made on a case-by-case basis, literature should be reviewed. (c) If possible, give the newborn immunoglobulin and hepatitis B vaccine. (d) If the mother develops the disease within 6 days before or 2 days after delivery, then give the uninfected child specific anti-varicella immunoglobulin and give acyclovir, separate the child from the mother until her infection disappears. (e) 24 hours after the appearance of the therapeutic level of antibodies in the mother. (f) If there are lesions on the breast or nipple, they must be cleaned before feeding. (g) Feeding on an abscessed breast depends on the location of the abscess, the drainage incision, and whether the milk duct is affected. (h) In the interests of the health of the mother, breast-feeding may only be allowed after complete treatment has been completed.
Call a consultant Have questions? +7 (812) 956-3-954
References:
References:
- GU Scientific Center for Children's Health of the Russian Academy of Medical Sciences; AND I. Horse, State Research Institute of Nutrition RAMS . National strategy for feeding children in the first year of life in the Russian Federation. Natural feeding. PEDIATRIC PRACTICE, Baby food. March, 2008
- Shabalov N.P., Neonatology: Textbook. allowance: In 2 volumes / N.P. Shabalov. - T. I. - 3rd ed., Rev. and additional — M.: MEDpress-inform, 2004. — 608 p. : illus.
- Breastfeeding and Human Lactation (Jones and Bartlett Series in Breastfeeding/Human Lactation) by Jan Riordan Publishe r: Jones and Bartlett Publishers, 3rd Edition, 2004. Pages: 819.
- Buckhold KM., Who’s afraid of hepatitis C? Am J Nurs 100:26–31, 2000.
- De Martino, m.
Et al . Should hepatitis b surface antigen positivemothers breast feed? Archives of disease in childhood, 60: 972–974 (1985).
- Fischler B et al. Vertical transmission of hepatitis C virus infection. Scand J Infect Dis 28:353–56, 1996.
- Gibb DM et al . Mother-to-mother transmission of hepatitis C virus: evidence for preventable peripartum transmission. Lancet 356(9233):904–7, 2000.
- Hardikar W . Advances in pediatric gastroenterology and hepatology. J Gastroenterol Hepatol 17:476–81, 2002
- Hill JB et al. Risk of hepatitis B transmission in breast-fed infants of chronic hepatitis B carriers. Obstet and Gynecol 6:1049–52, 2002).
- Ho-Hsiung L et al. Absence of infection in breast-fed infants born to hepatitis C virus-infected mothers. J Pediatr 126:589–91, 1995.
- Kage, m. Et al. Hepatitis c virus RNA present in saliva but absent in breast-milk of the hepatitis c carrier mother.
Journal of gastroenterology and hepatology, 12: 518–521 (1997).
- Kim Fleischer Michaelsen, Lawrence Weaver, Francesco Branca and Aileen Robertson , Infant Feeding and Nutrition? and children? early age. Guidelines for the WHO European Region with a special focus on the republics of the former Soviet Union. WHO Regional Publications, European Series, No 87. World Health Organization, 2001 Updated reprint 2003.
- Polywka S et al. Low risk of vertical transmission of hepatitis C virus by breast milk. Clin Infect Dis 29:1327–29, 1999.
- Roberts EA, Yeung L. Maternal-infant transmission of hepatitis C virus. Hepatology 36: S106-13, 2002.
- Spencer, j.d. et al. T ransmission of hepatitis c virus to infants of human immunodeficiency virus-negative intravenous drug-using mothers: rate of infection and assessment of risk factors for transmission. Journal of viral hepatology, 4: 395–409 (1997).
- Tajiri H et al. Prospective study of mother-to-infant transmission of hepatitis C virus. Pediatr Infect Dis J 20:10–14, 2001
- Yeung LT, King SM, Roberts EA. Mother-to-infant transmission of hepatitis C virus. Hepatology 34:254–29, 2001
Alena Lukyanchuk Psychologist, lactation consultant, member of ILCA (The International Lactation Consultant Association)
Hepatitis and HBV - Milky HelpMilky Help
Category: Articles, Articles of GV consultants.
July 28 is World Hepatitis Day. According to the World Health Organization, 325 million people worldwide are infected with hepatitis B and C.
Hepatitis is an inflammation of the liver, most often caused by a viral infection. There are five main hepatitis viruses, called types A, B, C, D and E. However, some of them can become chronic and lead to severe liver disease.
Unfortunately, there is a chance of encountering hepatitis both before and during pregnancy and after childbirth. In such a situation, it is important to understand how safe it is to breastfeed, whether the mother will infect her child through breast milk.
Consider the possibility of breastfeeding 🤱🏻 with the most common types of this virus - hepatitis A, B and C.
🚨 Hepatitis A
Transmitted through water, food, dirty hands and household items. Often proceeds almost asymptomatically; but may be accompanied by symptoms similar to SARS, as well as an increase in the liver and spleen, nausea, vomiting, and intestinal disorders.
Although hepatitis A is not transmitted through breast milk, breastfeeding mothers may receive different advice regarding breastfeeding. Usually, breastfeeding can be continued, subject to good hygiene and the introduction of immunoglobulin against hepatitis A to the child. But in the case of a severe course of the disease, doctors may insist on the complete isolation of the mother from the child until she recovers.
🚨 Hepatitis B and C
Transmitted through blood and other bodily fluids. The insidiousness of hepatitis here is due to the fact that for a long time it can be asymptomatic and manifest itself only at a late stage, such as cirrhosis of the liver. Therefore, it is important to follow preventive measures (carefully monitor the sterility of instruments in medical offices, tattoo and nail salons, do not share personal hygiene items with other people, avoid promiscuity or use a condom), as well as get tested for hepatitis as soon as possible if contact with someone else's blood still occurred.
Despite this, breastfeeding with hepatitis B and C is safe 👌🏻, except for cases of cracks and other damage to the breast of a nursing mother, which can lead to contact of the baby with the mother's blood. In such situations, you should temporarily stop breastfeeding or feed the baby with expressed pasteurized milk.
According to the “National program for optimizing the feeding of children in the first year of life in the Russian Federation”, 2019 edition:
“For hepatitis B in women, breastfeeding is possible when vaccinated in combination with the introduction of a specific immunoglobulin after the birth of a child.