Baby delivery steps
Stages of labour | Te Whatu Ora
Labour has three stages:
- The first stage is when the neck of the womb (cervix) opens to 10cm dilated.
- The second stage is when the baby moves down through the vagina and is born.
- The third stage is when the placenta (afterbirth) is delivered.
The first stage of labour: dilation
Before labour starts, your cervix is long and firm. During the first hours of labour, the muscles of the uterus (womb) contract and help shorten and soften the cervix, so that it can dilate (open).
For first-time mothers, this stage can last from six to 36 hours.
During this time you might experience:
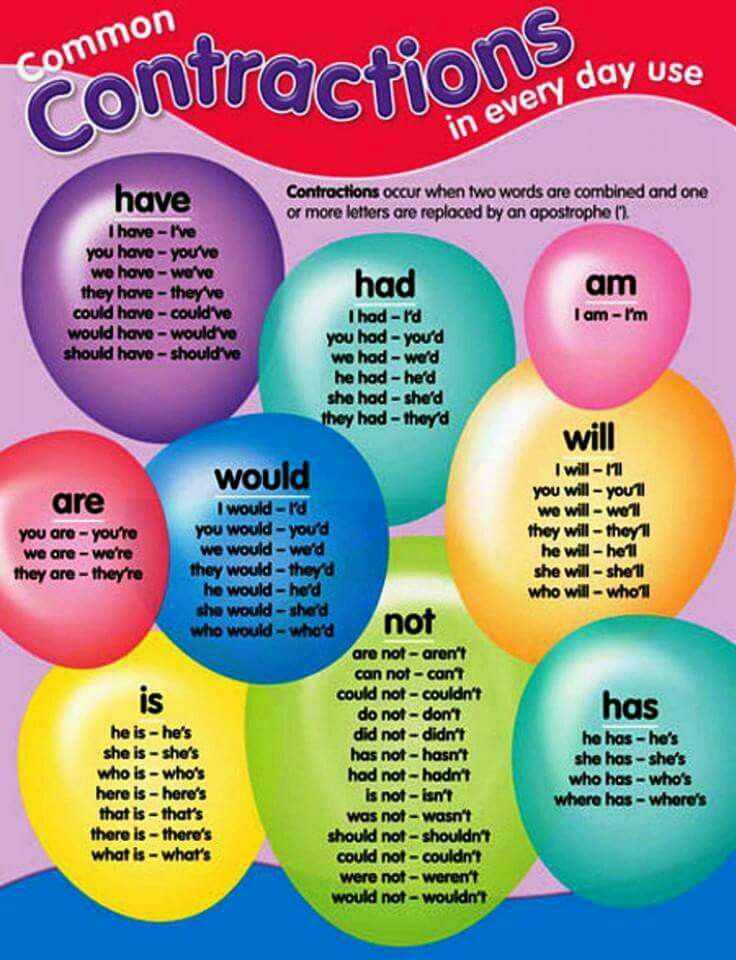
-
Contractions - some can be quite mild, like a period pain; others can be sharp and strong. Initially, the contractions will be short (between 30 to 40 seconds) and irregular. Once contractions are five minutes apart and a minute or more in length, labour is said to be 'established'.
- A 'show' - the discharge of a plug of mucus that can be thick and stringy or blood-tinged.
This may happen the day you go into labour, or up to a week before.
- 'Breaking of your waters' - this means the amniotic sac around your baby has ruptured.
Every labour is different. If you think you could be in labour, the first thing to do is relax and stay calm. The best place for early labour is at home.
When women who are planning to birth in a primary maternity unit or hospital stay at home until their labour is established, they are less likely to have interventions in their labour and are more likely to have a normal birth.
Keeping yourself comfortable and supporting your labour to establish while you're at home.
Click here for information on things to do and try and home, and how to look after yourself during early labour. [PDF, 1.1 MB]
[PDF, 1.1 MB]
When to ring your lead maternity carer (LMC) or our Labour & Birthing Suite (if you are giving birth at Auckland City Hospital):
- Your contractions are coming every five minutes, lasting longer than 50 seconds and have been getting stronger for at least two to three hours.
- You have severe or constant abdominal pain with a tight abdomen.
- Your water has broken and it is clear or has a tinge of pink. Put on a sanitary pad and check it after an hour. If it is wet, please ring us.
- Your water has broken and it is green or brown. Call us immediately - you will be advised to come into hospital.
- If there is a change in the pattern of your baby's movements..
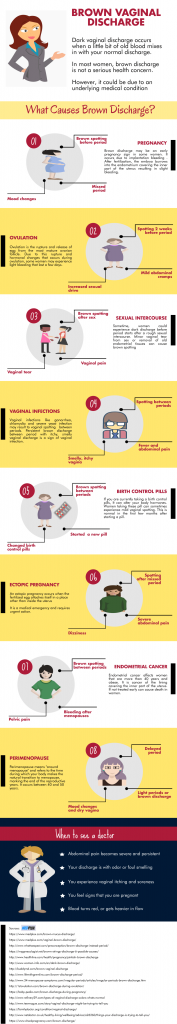
- You notice any vaginal bleeding - bright red vaginal bleeding is not normal.
Things to do and try at hospital:
- Try not to tense up during contractions. Your body is trying to release something, not tighten up.
- Find positions that feel comfortable.
 Walk the corridors slowly, lean on the walls, use the Swiss ball and La-Z-boy chairs. Try to stay off the bed, unless for a short rest.
Walk the corridors slowly, lean on the walls, use the Swiss ball and La-Z-boy chairs. Try to stay off the bed, unless for a short rest. - Water is great for relaxation and coping with contractions. If you don't have use of a pool, try the shower.
- Bring music and a player, if it relaxes or calms you.
- Bring an electric oil burner and use your aromatherapy oil.
- Continue to take refreshments and drink small amounts frequently.
- Phone calls are a distraction from your tasks of giving birth and looking after your new baby. Encourage family and friends to phone one designated person for updates.
The second stage of labour: your baby
The second stage of labour begins when the cervix is fully dilated (open) and the baby's head moves down out of the uterus and into the vagina (or birth canal). Your job at this stage is to push the baby through the birth canal, so you'll need focused determination and energy.
The birth of your baby may take 30 minutes to an hour or longer. This second stage could be further extended if you have an epidural.
This second stage could be further extended if you have an epidural.
A small number of women will require assistance with their births, either by forceps or ventouse (vacuum extraction). The obstetrician will choose which is best for your situation.
Find out more about your pain relief options and coping with labour.
The third stage of labour: the placenta
The final stage of labour is delivery of the placenta. There can happen in one of two ways listed below.
Your LMC can help you to decide which approach would be best for you, taking into considering your health, how your pregnancy has progressed and the type of labour and birth you experience.
1. Physiological management
Physiological third stage means waiting for your placenta to deliver spontaneously with your effort. This may take up to an hour following the birth; while you're waiting, skin-to-skin with your baby and a first breastfeed will be encouraged.
2. Active management
Active management involves injecting an ecbolic (contracting drug) into your leg as your baby's shoulders are born. The ecbolic speeds up placental separation and your uterus (womb) contracts down to reduce blood loss and ensure your womb remains contracted.
The ecbolic speeds up placental separation and your uterus (womb) contracts down to reduce blood loss and ensure your womb remains contracted.
Please read our leaflet on caring for your whenua [PDF, 1 MB] for more information.
Stages of labor and delivery, explained
Toward the end of pregnancy, it might be tempting to grab your hospital bag whenever you feel something new, thinking it’s an early sign of labor. There may even be a few false alarms – after all, your due date is only an estimate.
Whether labor begins on its own or you need an induction, it can be helpful to know what you may experience as your labor progresses toward delivering your baby, and when to head to the hospital or birth center.
Below, we explain the three stages of labor and delivery for vaginal births. This includes what marks the start and end of each stage, how long each may last, how your body is likely to feel and more.
Click the links below to jump to each of the three stages of labor:
- The first stage of labor is usually the longest as your body gets ready for delivery.

- The second stage of labor is the process of delivering your baby after your cervix has fully dilated.
- The third stage of labor occurs after the baby is born and lasts until the placenta is delivered.
1. The first stage of labor
The first stage of labor is the preparation phase. For months, your body has been working to keep baby in. And now it’s time for your baby to come out.
Your body does this through contractions. Contractions help dilate (open) and efface (thin) the cervix, which is what connects your uterus to your vagina (birth canal).
What happens during the first stage of labor?
The first stage of labor is mainly distinguished by how dilated the cervix is and the characteristics of the contractions. Within this first stage, there are three phases: early, active and transition. If it’s your first time giving birth, the first stage of labor may take several days to complete. Here’s about how long each phase typically lasts:
- Early phase: Up to 24-48 hours
- Active phase: Up to about eight hours
- Transition phase: Up to about three hours
Early (latent) phase
In the latent phase, contractions start out mild and irregular, typically lasting for less than a minute. They’ll gradually become stronger and more frequent as your cervix dilates. During this phase, you may notice thick pink or red vaginal discharge – this is the mucus plug that helped keep bacteria from passing through the cervix during pregnancy.
They’ll gradually become stronger and more frequent as your cervix dilates. During this phase, you may notice thick pink or red vaginal discharge – this is the mucus plug that helped keep bacteria from passing through the cervix during pregnancy.
Active phase
You may have reached active labor once your contractions last for around a minute and have been occurring at least every 5 minutes for an hour (or ever 7 minutes if it’s not your first baby). This is when it’s time to call your provider or hospital, as you have been instructed. Other signs that it’s time to go to the hospital include:
- Your water breaks. This can feel like a sudden gush or a slow trickle from your vagina. It’s possible for your water to break before you reach active labor – call your care provider if it does.
- Intense contractions that you can’t walk or talk through.
- Bloody discharge that’s more watery than the mucus plug.
During active labor, you may also experience:
- Nausea or vomiting
- Leg cramps
- Pain and pressure in your lower back
Transition phase
The end of active labor is sometimes referred to as the transition to the second stage of labor. It’s when the cervix completely dilates to a full 10 centimeters, and is the shortest – but generally considered the hardest – part of labor. If this is your first time giving birth, transition may take up to a few hours, or it may progress quickly. Contractions will be the longest, strongest and most frequent so far.
It’s when the cervix completely dilates to a full 10 centimeters, and is the shortest – but generally considered the hardest – part of labor. If this is your first time giving birth, transition may take up to a few hours, or it may progress quickly. Contractions will be the longest, strongest and most frequent so far.
During the transition phase, you may also feel:
- Pressure in the lower back and rectum
- An urge to push (tell your care provider if you do, as they’ll want to make sure you’re fully dilated first)
Inducing labor
There are some cases where labor has to be started manually (induced). Labor induction may be recommended for reasons such as:
- Labor hasn’t started naturally around two weeks after the due date.
- Your water has broken but contractions haven’t started for several hours.
- There’s not enough amniotic fluid.
- You have an infection or other pregnancy complication.
Pain relief
If you choose to labor at a hospital or hospital-based birth center, you’ll likely have some flexibility around pain management once you reach active labor. If you’ve been unsure whether to try for an unmedicated birth or use an epidural, this may be when you make your final decision – only you will know how much pain relief you need.
If you’ve been unsure whether to try for an unmedicated birth or use an epidural, this may be when you make your final decision – only you will know how much pain relief you need.
Unmedicated methods like hydrotherapy and massage may work great for you, or you may choose medication like an epidural to provide a strong numbing sensation. Generally, you can expect to have a few different options for managing labor and delivery pains, but it can be helpful to research them ahead of time as you write your birth plan.
The second stage of labor
The second stage of labor begins once your cervix is fully dilated, and ends when your baby is born. It may take anywhere from a few minutes to a few hours. It’s possible that this stage could take longer if you find it harder to push from the numbness of an epidural, or if it’s your first time giving birth.
What happens during the second stage of labor?
The second stage of labor is all about pushing. Your doctor or midwife will guide you through how and when to push – you may be instructed to push when you feel the urge, or when you’re having a contraction. Contractions could remain as intense as they were at the end of stage one, but they may be a little less frequent.
Contractions could remain as intense as they were at the end of stage one, but they may be a little less frequent.
The third stage of labor
Once your baby has been born, you’re in the third stage of labor. This stage is considered complete once the placenta has been delivered, which generally happens within 30 minutes of childbirth.
What happens during the third stage of labor?
You’ll continue to have contractions, but they’ll be milder. These contractions will move the placenta out of your uterus, and over the next few days, help your uterus return to its normal size. If necessary, your care provider will remove any remaining tissue from your uterus.
The first hours of recovery
It’s finally time to meet, hold and celebrate your baby! Most babies are ready to breastfeed shortly after birth. Breastfeeding releases the hormone oxytocin, which encourages helpful, mild “post-birth” contractions and reduces bleeding. If your baby’s ready and you’re having trouble getting started, you can ask for help from a nurse or breastfeeding consultant. And if you or your baby don’t want to breastfeed, you’ll still get to hold them skin-to-skin to begin bonding unless your baby needs medical attention.
And if you or your baby don’t want to breastfeed, you’ll still get to hold them skin-to-skin to begin bonding unless your baby needs medical attention.
These first hours after birth mark the start of your recovery, and are sometimes referred to as the fourth stage of labor. During the rest of your hospital stay, your care team will monitor your blood pressure and other vital signs, and make sure you aren’t bleeding too much. They may also give you a shot of oxytocin and abdominal massages to promote contractions and control bleeding. You may find that you get chills or shakes during this stage, so ask for a blanket if you need one. If you had an epidural, the tube will be removed from your back, and if you had any small tears during delivery, you’ll be given local anesthetic and stitches.
And before you go home, you’ll receive plenty of tips for continuing your postpartum recovery and information about what to expect now that you’ve given birth.
What to know about the possibility of a C-section
Not every parent goes through all the stages of labor and delivery as they’re described above.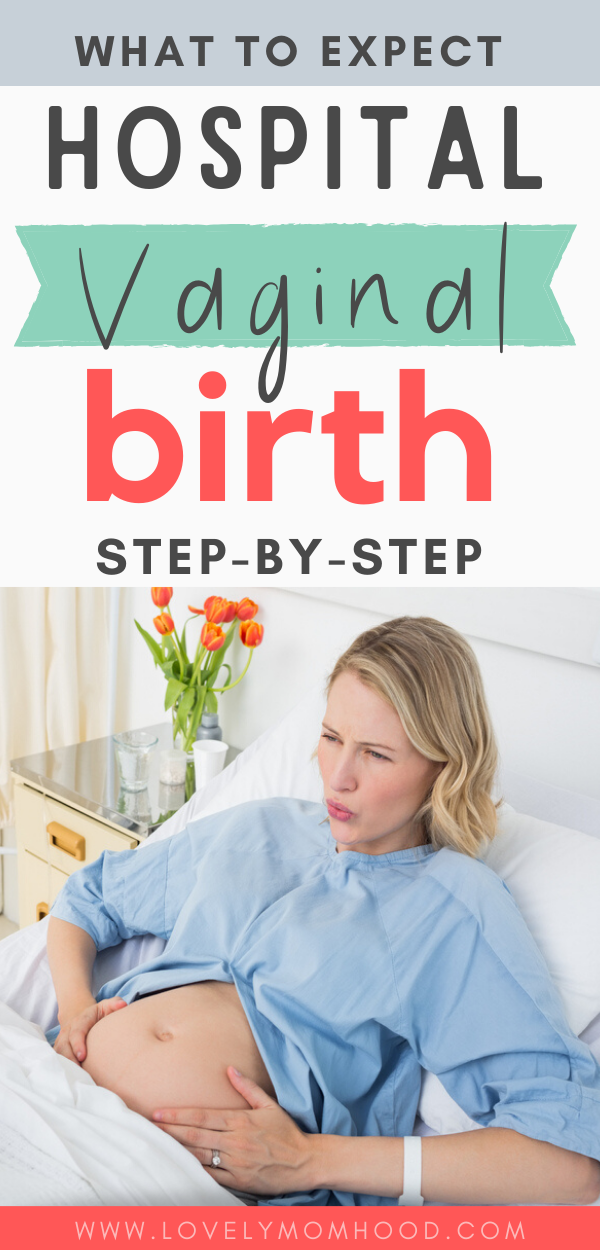 A cesarean delivery (C-section), which involves surgically delivering a baby through the abdomen, isn’t something many people think about as they approach their due date, unless it’s planned. However, C-sections account for up to 20-35% of births in the United States.
A cesarean delivery (C-section), which involves surgically delivering a baby through the abdomen, isn’t something many people think about as they approach their due date, unless it’s planned. However, C-sections account for up to 20-35% of births in the United States.
The most important thing to know is that a C-section is only recommended when it’s the best choice for you and your baby. One may be scheduled in advance if there’s a clear medical reason for doing so, but often the need for a C-section doesn’t arise until closer to, or during, labor. For example, one of the most common reasons for an unplanned C-section is stalled labor, in which the cervix stops opening despite continued contractions.
Start preparing for labor and delivery
Everybody’s big day is different. But if you’re reading this, you’re already doing two of the best things you can to get ready: learning and planning. In addition to becoming familiar with the process of giving birth, here are a few other tips:
- Take a class: Childbirth classes can teach you everything from tools for staying relaxed during labor to what to expect from different forms of pain relief, and more.

- Prepare a birth plan: Writing a birth plan to give to your care team will help them support your labor, delivery and postpartum care according to your preferences.
- Strengthen your pelvic floor: Your pelvic floor muscles are going to go through a lot during labor. Practicing Kegels (flexing the muscles that stop urination) and other exercises can help reduce your risk of pelvic floor dysfunction after birth.
Finally, talk with your care provider. Whether you’re working with a doctor or a midwife, they’ll be able to answer questions and walk you through anything you might be unsure about. Take advantage of their expertise – they want to help.
Talk to your care provider
Important to know - Health of a Petersburger
The total duration of childbirth and their course
The total duration of childbirth depends on many factors: age, physique and physical condition of the woman, her psychological mood, the speed of cervical dilatation, first pregnancy or repeated, the size of the child, the type of presentation and a number of other points.
Labor activity proceeds differently for all women, but the main periods of childbirth are clearly distinguished: 1st period - the period of contractions, the longest and most intense, 2nd period - the direct birth of a baby, 3rd period - the birth of the afterbirth (placenta).
First stage of labor (opening period)
As the name implies, during this period there is a gradual opening of the cervix as a result of regular contractions of the uterine muscles. Contractions occur with a decreasing interval, while they themselves become longer and more frequent.
The dilation period is the time elapsed from the onset of regular contractions until the cervix is fully dilated. During this period, the birth canal is prepared for the passage of the fetus through them with all the fetal formations.
Cervical dilatation occurs gradually: at first the cervix is smoothed out, then the pharynx opens up to 3-4 cm and at the end of the first stage of labor up to 10 cm. This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
The first stage of labor is the longest and consists of three phases:
1. Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is definitively flattened and opens about 4 cm.
2. Active phase (lasts 3-4 hours). Contractions become more intense, last at least 20 seconds, and the interval between them is reduced to 5-6 minutes. Normally, during the active phase, amniotic fluid is poured out, which contributes to a faster full disclosure of the uterine pharynx. By the end of the phase, the uterus opens by 8 cm. This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process. Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process. Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Second stage of labor (exile period)
The period of exile is the time from the moment of full opening of the pharynx until the birth of the fetus.
It is the second stage of childbirth that is their culmination, because for a short time (compared to contractions) the long-awaited birth of the baby takes place.
After the discharge of amniotic fluid, contractions temporarily stop. The volume of the uterine cavity decreases, the uterine cavity and vagina appear as a single birth canal. Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.
Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.
Pushing is a lot of physical work. During attempts, a woman experiences maximum physical stress (blood pressure rises, pulse and respiration become more frequent). During the attempts, the woman holds her breath, and in the intervals between them she rests and "gathers her strength for a new attempt."
In the process of one of the attempts, the head is born. Next, the shoulders are born (first the front, then the back) and the torso. Following the fetus, the posterior amniotic fluid is poured out with an admixture of cheese-like lubricant.
A woman in labor, having experienced severe fatigue, rests after hard work (pulse and respiration rate decrease).
Third stage of labor (postpartum period).
The afterbirth period is the time from the birth of the fetus to the birth of the placenta. During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
In the process of separation of the placenta from the walls of the uterus, the uteroplacental vessels are damaged, which is normally accompanied by blood loss in the amount of 100-200 ml, without adversely affecting the woman's condition. After the birth of the placenta, the uterus contracts sharply, becomes dense, which is necessary to stop bleeding in the area of the placental site; its bottom is in the middle between the womb and the navel.
During this period, the woman's pulse and respiration normalize. Her demeanor is calm. Chills can sometimes be observed (as a reaction to the transferred strong physical stress).
The third period is no longer as exciting and tense as the previous two. The child was born and the matter remains for the small - the separation of the placenta, or placenta. Nature provides for the resumption of contractions a few minutes after the birth of the baby, necessary for effective exfoliation from the uterus of tissues that nourished the fetus during pregnancy (placenta, membranes, umbilical cord).
Three periods of physiological labor - the natural end of a nine-month wait. Most likely, during the birth process itself, the woman in labor will not care what the period or phase of childbirth is now, but it is still desirable to know about them, at least for greater certainty before going to the hospital.
How to behave in childbirth? Learning to give birth quickly and with problems
Childbirth is a natural process laid down by nature. The whole sequence of events that take place during this period is predetermined, but by your actions you can either speed up the birth of a baby, or complicate his birth.
Childbirth is the final and most important stage of pregnancy. How you behave and how accurately and skillfully you follow the instructions of the obstetrician depends on how you will feel and how quickly your baby will be born. What does a newborn need to know? Let's try to answer the most important questions.
1. When is it time to go to the maternity hospital?
Childbirth is a natural result of hormonal changes that occur in your body during the final stages of pregnancy. The sagging belly and heaviness in its lower part and the lumbar region speak of the imminent denouement of the story. Periodically, weak contractions occur, the stomach tenses and pulls down, but these sensations quickly pass, the uterus relaxes again and becomes soft. Such contractions are harbingers of childbirth, but they are far from real labor activity.
The signal to call an ambulance should be sufficiently strong contractions that are repeated at regular intervals, the appearance of mucous secretions from the genital tract, slightly stained with blood, or the outflow of amniotic fluid.
2. First stage of childbirth: we breathe for two!
From the moment the contractions become regular, the first stage of labor begins, during which the strength, frequency and duration of uterine spasms increases and the cervix opens.
During spastic contraction of the uterine muscle fibers, the blood vessels that carry arterial blood to the placenta and fetus are compressed. The fetus begins to experience a lack of oxygen, and this involuntarily makes you breathe deeper. The reflex increase in the rate of contractions of your heart will ensure the delivery of oxygen to the child. Nature has provided that these processes take place regardless of your consciousness, but you should not completely rely on it.
In the first stage of labor, during each contraction, you need to breathe calmly and deeply, trying not to hold your breath while inhaling. At the same time, the air should fill the upper sections of the lungs, as if raising the chest. You need to inhale through the nose, slowly and smoothly, exhale through the mouth, just as evenly.
You need to inhale through the nose, slowly and smoothly, exhale through the mouth, just as evenly.
3. Auto-training in the prenatal ward
To speed up the opening of the cervix, you need to walk more, but sitting is not recommended, while blood flow in the limbs is disturbed and venous blood stagnation occurs in the pelvis. From time to time it is useful to lie on your side, stroking your lower abdomen with both hands in the direction from the center to the sides, focusing on breathing and saying to yourself: "I am calm, I am in control of the situation, each contraction brings me closer to the birth of a baby."
4. To relieve pain
Acupressure of the lower back can help relieve pain. Find the outer corners of the sacral rhombus on your lower back and massage these points with clenched fists.
Monitor the frequency and duration of contractions and if they weaken or sharply increase, immediately inform your doctor. In case of severe pain, you can ask for an anesthetic, but you should remember that you should not take the medicine too often, this is fraught with narcotic depression of the newborn and a decrease in his adaptive abilities.
In case of severe pain, you can ask for an anesthetic, but you should remember that you should not take the medicine too often, this is fraught with narcotic depression of the newborn and a decrease in his adaptive abilities.
If dilatation of the cervix has caused reflex vomiting, rinse your mouth with water and then drink a few sips to replace the lost fluid. Do not drink a lot, this can provoke a recurrence of vomiting.
5. The maternity ward is not a place for tantrums
They say that difficult childbirth is a person's retribution for walking upright. Childbirth is actually a painful process, but the presence of reason allows us, representatives of the genus Homo sapiens, to control our emotions. Screaming, crying, tantrums and swearing have no place in the maternity ward. This creates a tense environment, interferes with the normal course of childbirth, complicates diagnostic and therapeutic measures, and ultimately affects their outcome.
6. Second stage of labor - pushing and expulsion of the fetus
After the baby's head slips through the dilated cervix and finds itself on the bottom of the pelvis, the pushing period of labor begins. At this time, there is a desire to push, as it usually happens during a bowel movement, but at the same time many times stronger. At first, the attempts are controllable, they can be "breathed", but by the beginning of the third stage of labor, the expulsion of the fetus, they become unbearable.
With the beginning of the straining period, you will be transferred to the delivery room. Having settled down on the delivery table, rest your feet on the special steps, firmly grasp the handrails and wait for the midwife's command.
While pushing, inhale deeply, close your mouth, tighten your lips tightly, pull the handrails of the birthing table towards you and direct all the energy of exhalation down, squeezing the fetus out of you. When the top of the baby appears from the genital slit, the midwife will ask you to ease your efforts. With gentle movements of her hands, she will first release the baby’s forehead, then his face and chin, after which she will ask you to push again. At the moment of the next attempt, the baby's shoulders and torso will be born. After the newborn is born, you can breathe freely and rest a little, but the birth is not over.
When the top of the baby appears from the genital slit, the midwife will ask you to ease your efforts. With gentle movements of her hands, she will first release the baby’s forehead, then his face and chin, after which she will ask you to push again. At the moment of the next attempt, the baby's shoulders and torso will be born. After the newborn is born, you can breathe freely and rest a little, but the birth is not over.
7. The third stage of labor and the final stage
The third stage of labor is the afterbirth period. At this time, weak contractions are observed, due to which the fetal membranes gradually exfoliate from the walls of the uterus.
About 10 minutes after your baby is born, your midwife will ask you to push again to deliver your afterbirth. The doctor will carefully examine it and make sure that all parts of the membranes have come out. After that, with the help of mirrors, he will examine the cervix and make sure that it is intact.